Abstract
Background
Peroral endoscopic myotomy (POEM) has been recently introduced in clinical practice for the treatment of achalasia. The endoluminal functional lumen imaging probe (EndoFLIP) system) uses impedance planimetry for the real-time measurement of the diameter of the oesophago-gastric junction.
Objective
The aim of this study is to prospectively evaluate the effect of POEM on the oesophago-gastric junction using EndoFLIP.
Methods
All the patients who underwent POEM in a single centre between April and July 2013 were enrolled in the study. EndoFLIP was used intraoperatively, immediately before and after POEM. During follow-up patients underwent oesophagogastroduodenoscopy, oesophageal pH monitoring and manometry. Clinical outcomes were compared with the diameter of the oesophago-gastric junction after POEM.
Results
In total, 23 patients (12 males, mean age 51.7 years) were enrolled, and 21 underwent POEM successfully. Preoperative mean basal lower oesophageal sphincter pressure was 42.1 mmHg (±17.6). Before POEM, the mean oesophago-gastric junction diameter and cross-sectional area were 6.3 mm (±1.8) and 32.9 mm2 (±23.1), respectively. After treatment, the mean diameter and cross-sectional area of the oesophago-gastric junction were 11.3 mm (±1.7 SD) and 102.38 mm2 (±28.2 SD), respectively. No complications occurred during a mean follow-up of 5 months. Median post-operative Eckardt score was 1. Three patients (14.3%) referred heartburn. Follow-up studies revealed gastro-oesophageal reflux disease (GORD) in 57.1% of patients and oesophagitis in 33.3%. No correlations were observed between the diameter of oesophago-gastric junction after POEM and symptoms relief, GORD incidence and lower oesophageal sphincter pressure.
Conclusions
The diameter of oesophago-gastric junction substantially increases after POEM. EndoFLIP is a reliable method for the intraoperative evaluation of oesophago-gastric junction diameter. However, the real usefulness of this technology after POEM remains controversial.
Keywords: Achalasia, peroral endoscopic myotomy, EndoFLIP, oesophago-gastric junction, oesophageal manometry, oesophagus, endoscopy
Background and aims
Achalasia is a rare oesophageal disease characterized by the absence of efficacious peristalsis of the oesophageal body and impaired relaxation of the lower oesophageal sphincter (LOS) in response to swallowing.1,2 Achalasia is caused by the progressive degeneration of the neurons of the myenteric Auerbach plexus. Degeneration is irreversible, and all the available treatments – medical, endoscopic and surgical – aim to relieve the symptoms of achalasia (dysphagia, regurgitation, chest pain and weight loss) by reducing the basal and swallow-induced residual LOS pressure.1,2
The classic surgical treatment of achalasia is Heller myotomy associated with an anti-reflux wrap.1,2 The disruption of the muscular fibres of the LOS by using endoscopic pneumatic dilation with large-calibre balloons offers excellent short-term results, with a minimal complication rate and invasiveness.1,2 Despite the excellent results at 2-year follow-up,3 the benefits of balloon dilations seem to vanish with time, especially in young patients.4,5
More recently, peroral endoscopic myotomy (POEM) has been introduced in clinical practice as an endoscopic alternative to surgical myotomy.6 POEM may theoretically offer the same long-term benefits of surgical myotomy, with the minimal invasiveness of an endoscopic transoral procedure. POEM is gaining international consensus, although few data on long-term follow-up are available.7
The efficacy of any therapeutic intervention for achalasia is usually measured by evaluation of symptoms, appearance of oesophago-gastric junction (OGJ) at oesophagogastroduodenoscopy (OGD), timed oesophagograms, and oesophageal manometry.
The EndoFLIP (Endoluminal Functional Lumen Imaging Probe) System is a new technology that provides real-time measurements of the diameter of OGJ and of its cross-sectional area8,9 through a specific catheter with a balloon attached at the distal end, using specific algorithms and impedance planimetry. EndoFLIP may allow the immediate evaluation of the effects of any therapeutic interventions on the LOS and OGJ, including anti-reflux procedures.10,11 and treatment of achalasia.12–14 However, few studies have evaluated the possible benefits of the use of EndoFLIP during POEM.11,15,16
The aim of this prospective observational study is to report on the effects of POEM on the OGJ and LOS, as evaluated with EndoFLIP immediately after myotomy, and to compare clinical outcomes, manometry findings and gastro-oesophageal reflux disease (GORD) incidence during follow-up with the post-operative diameter of the OGJ.
Methods
All the patients who underwent POEM in a single tertiary referral centre between April 2013 and July 2013 were enrolled in the study. POEM was offered to patients with a confirmed diagnosis of achalasia and an Eckardt score greater than 3. Diagnostic workup for achalasia, included, as usual, high-resolution manometry, timed barium oesophagograms, and OGD.
POEM technique
POEM was performed by two endoscopists (GC and PF) according to the technique previously described by Inoue et al.6 The mucosa of the oesophagus was lifted with a 10% glycerol solution, and incised approximately 10–13 cm above the OGJ. A triangle-tip knife (TT-knife, Olympus Co., Tokyo, Japan) was used to create a tunnel into the oesophageal submucosa, extended for 3 cm beyond the OGJ. After submucosal dissection, myotomy was performed, and included preferably the circular bundles of the muscularis propria of the oesophagus and cardia. The mucosal defect was closed with endoscopic clips.
EndoFLIP system and catheter
The EndoFLIP® System technology uses impedance planimetry to characterize the geometry of cross-sectional measurement areas. Impedance planimetry uses AC voltage measurements made between pairs of electrodes to estimate the extent of the diameter of the medium (a conductive fluid) at the mid-point between those electrodes. If the conductive medium is contained in a flexible balloon and an array of voltage electrodes used, the shape of the balloon can be reproduced based on the voltage readings. This is the basis of the EndoFLIP imaging technique.8,9
The EndoFLIP EF-825 catheter was used for the study. This catheter has attached at the distal end a soft balloon, with 16 electrodes, spacing 5 mm each other, providing an 8 cm-long image field, for volume-controlled measurements. No pressure sensors are embedded in this catheter.
The probe has a very soft and flexible tip, and can be easily pushed through the cardia before and after POEM. The position of the catheter can be checked using an endoscope alongside the probe. The measurement of the diameters and cross-sectional areas does not require any collaboration by the patient (swallowing, breathing …), and thus EndoFLIP can be used during the operation under general anaesthesia.
EndoFLIP measurements were performed on the same day, immediately before and after the POEM procedure. The balloon was inflated with 30 ml of balanced saline solution, and pulled back into the OGJ to a point where the OGJ was observed to be located centrally within the balloon. The narrowest cross-sectional area identified the LOS and the OGJ, and was used as reference diameter.
Still images of the EndoFLIP measurements were acquired and stored for comparisons, before and after the POEM.
Management after POEM and follow-up
Patients resumed oral feeding 1 or 2 days after POEM and were discharged. Follow-up visits for assessment of symptoms were performed 30 days after the procedure. At 3-month and/or 6-month follow-up patients underwent evaluation of symptoms, oesophageal high-resolution manometry and pH monitoring.
Data analysis and statistics
Demographics, preoperative and procedural data, results of the EndoFLIP measurements and follow-up data were recorded into a prospectively collected database on Microsoft Excel, encrypted and stored.
The data collected before and after POEM were compared. Data are presented as mean ± standard deviation when parametric and as median (range) when nonparametric. ANOVA test was used to compare mean diameter of OGJ after POEM to clinical outcomes (Eckardt score, GORD at oesophageal pH monitoring, oesophagitis and GORD symptoms). Pearson’s test was used to assess the correlations between OGJ diameter after POEM, basal LOS pressure and 4sIRP. A p-value of 0.05 was considered as statistically significant.
Results
During the study periods 23 consecutive patients (12 males, mean age 51.7 years) underwent POEM and EndoFLIP, and were enrolled in the study. Median Eckardt score before POEM was 8 (range 5–12). Thirteen patients had a type I achalasia at high-resolution manometry; 10 a type-II. Preoperative mean basal LOS pressure was 42.1 mmHg (±17.6 SD) and mean 4sIRP was 28.5 mmHg (±15.5 SD) (Table 1).
Table 1.
Baseline characteristics of enrolled patients, results of the intra-operative evaluation of OGJ during POEM, and clinical outcomes at follow-up, including also GORD and LOS pressure
| Number of patients enrolled (successfully treated) | 23 (21) |
| Mean age (years) | 51.7 |
| Males | 12 |
| Basal LOS pressure (mean ± SD) | 42.1 mmHg ± 17.6 |
| 4sIRP (mean ± SD) | 28.5 mmHg ± 15.5 |
| Eckardt score (median [range]) | 8 (5–12) |
| Pre-operative OGJ diameter [mean (±SD)] (using a balloon inflated with 30 ml of saline solution) | 6.3 mm ± 1.8 |
| Post-operative OGJ diameter | 11.3 mm ± 1.7 |
| Pre-operative OGJ cross-sectional area [mean (±SD)] (using a balloon inflated with 30 ml of saline solution) | 32.9 mm2 ± 23.1 |
| Post-operative OGJ cross-sectional area | 102.38 mm2 ± 28.2 |
| Mean follow-up (range) | 5 months (3–6 months) |
| Post-operative basal LOS pressure (mean ± SD) | 23.5 mmHg ± 11 |
| Post-operative 4sIRP (mean + SD) | 10.3 mmHg ± 4.2 |
| Post-operative Eckardt score (median [range]) | 1.0 (0–3) |
| GORD at oesophageal pH monitoring (n/%) | 12 (57.1%) |
| Reflux oesophagitis (n/%) | 7 (33.3%) |
| GORD symptoms (heartburn) (n/%) | 3 (14.3%) |
The procedures were completed successfully in 21 of 23 patients. In two patients – one with a history of breast cancer and mediastinal irradiation and another one with a sigmoid oesophagus and a very long history of dysphagia – mucosal lifting failed and POEM procedures were aborted. The patients underwent pneumatic dilation using a 30 mm balloon. EndoFLIP was successfully performed in all the cases. The day after the procedure the patients underwent OGD and oesophageal Gastrografin® study, demonstrating no complications, and the patients were fed with a soft diet. Patients were discharged an average 3 days after the procedure.
EndoFLIP measurements
Baseline EndoFLIP data are available for all the patients. Before POEM, the OGJ diameter and cross-sectional area – as measured with EndoFLIP and a balloon inflated with 30 ml of saline solution – were on average 6.3 mm (±1.8 SD) and 32.9 mm2 (±23.1 SD), respectively.
After treatment, the mean diameter and cross-sectional area of the OGJ substantially increased to 11.3 mm (±1.7 SD) and 102.38 mm2 (±28.2 SD), respectively (Table 1).
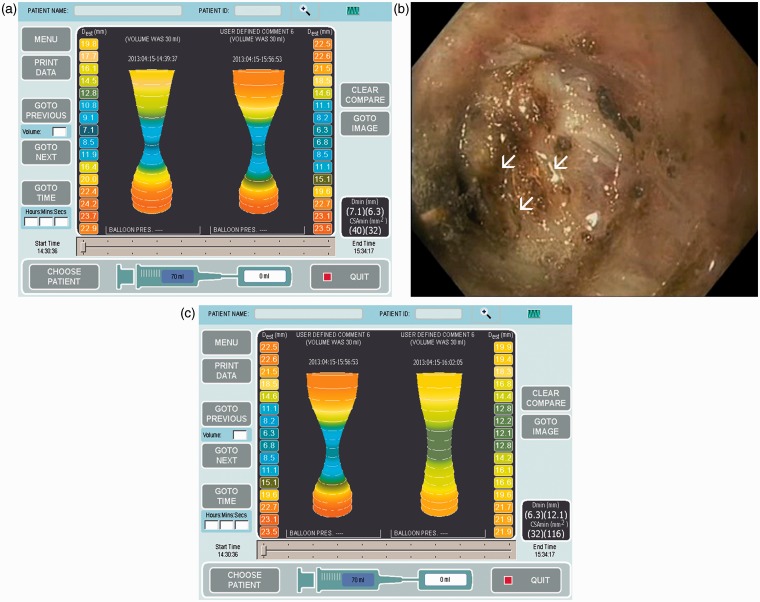
In one patient, after the initial myotomy, the diameter of the OGJ was not substantially wider compared with the preoperative results (6.3 mm vs. 7.1 mm, respectively). The mucosal incision had not yet been closed with the clips. The endoscope was thus reinserted in the submucosal tunnel, and some more bundles of the LOS were cut using electrocoagulation. At the final measurement using EndoFLIP, the mean diameter of LOS at 30 ml was now 12.7 mm (Figure 1).
Figure 1.
Evaluation of the oesophago-gastrioc junction (OGJ) using EndoFLIP, before and after Peroral endoscopic myotomy (POEM).
a) The diameter of the OGJ did dot substantially changed before POEM (7.1 mm, on the left side of the picture) and after POEM (6.3 mm, on the right side of the picture); b) the endoscope was reinserted into the submucosal tunnel, and some additional bundles at the level of the lower oesophageal sphincter (arrows) were cut; c) the EndoFLIP real-time evaluation, demonstrate a satisfactory enlargement of the OGJ (12.1 mm, right side of the picture).
Follow-up
Mean follow-up after POEM was 5 months (range 3–6 months). No complications occurred in the study population. Post-operative median Eckardt score was 1 (range 0–3). Three patients (14.3%) referred heartburn at follow-up. However, oesophageal pH monitoring revealed GORD in 12 patients (57.1%), and oesophagitis was found in seven patients (33.3%). After POEM, average basal LOS pressure was 23.5 mmHg (±11) and 4sIRP 10.3 mmHg (±4.2) (Table 1).
Four patients had an OGJ diameter less than 10 mm after POEM, but three of them had GORD at oesophageal pH monitoring. At univariate analysis, no statistically significant correlations were observed between the post-operative EndoFLIP measurement of the OGJ, and Eckardt score, GORD at oesophageal pH monitoring, reflux oesophagitis, and symptoms of GORD at follow-up visit (Table 2).
Table 2.
Correlation between OGJ diameter after POEM with clinical outcomes and GORD
| # patients | Diameter OGJ (mean ± SD) | p-value | ||
|---|---|---|---|---|
| Dysphagia relief | ECK = 0 | 9 | 11.689 ± 1.822 | 0.432 |
| ECK > 0 | 12 | 11.067 ± 1.707 | ||
| GORD at pH-metry | GERD | 12 | 11.325 ± 1.658 | 0.981 |
| No GERD | 9 | 11.344 ± 1.949 | ||
| Oesophagitis | Oesophagitis | 7 | 11.943 ± 0.616 | 0.267 |
| No oesophagitis | 14 | 11.029 ± 2.046 | ||
| GORD symptoms | Heartburn | 3 | 12.100 ± 0.721 | 0.424 |
| No heartburn | 18 | 11.206 ± 1.839 |
ECK: Eckardt Score; GORD: Gastro-oesophageal reflux disease.
No significant correlations were observed between the OGJ diameter after POEM and post-operative basal LOS pressure (R = 0.08; p = 0.755) and 4sIRP (R =−0.28; p = 0.259).
Discussion
POEM is now considered effective and safe for the treatment of oesophageal achalasia.6,7,17–24
Previous studies demonstrated that the long-term benefits of surgical and endoscopic treatment of achalasia are directly related with the reduction of the basal LOS pressure.4,5 Recurrences of dysphagia have been observed more frequently in case of LOS pressure ≥10 mmHg.5 Unfortunately, oesophageal manometry cannot be performed during POEM, with the patients under anaesthesia, and any evaluation of the effects of myotomy on LOS pressure and oesophageal emptying should be performed post-operatively.
Some authors have demonstrated that the distensibility of the OGJ can substantially affect oesophageal emptying, and this parameter could correlate with the efficacy of the procedure and, possibly, with adverse events (including GORD).13,16
Currently during POEM, the effects and completeness of myotomy can be only assessed subjectively and empirically, by evaluating the appearance of myotomy at OGD and by passing the endoscope through the cardia, trying to appreciate any resistance to the transit. In order to have a complete myotomy at the level of the LOS, submucosal dissection and myotomy are usually extended for 2–3 cm beyond the cardias on the gastric wall.6,25 However, again endoscopic measurements are subjective and imprecise, and may be affected by many biases.
EndoFLIP allows a real-time measurement of the diameter of the oesophagus and of the OGJ.8,9,15 The possibility to measure the diameter of the OGJ before and after the POEM can be particularly useful to drive therapy and reveal cases of incomplete myotomy, before the closure of the entry of submucosal tunnel with clips. In one of our cases, even though the myotomy seemed complete at the end of the procedure, EndoFLIP did not reveal any substantial change of the diameter of the OGJ, with the balloon inflated at 30 ml. The mucosal incision had not yet been closed. Hence, the endoscope was inserted again into the submucosal tunnel, and some additional muscular bundles were cut at the level of the OGJ, with a substantial improvement of the final diameter of the OGJ.
In contrast to other studies,8,9,11,13,15,16,26–28 the EndoFLIP probe used in this study (EF-825) does not measure pressure, and consequently actual distensibility of the OGJ was not assessed during the study. Evidence from achalasia patients studied with EndoFLIP in seminal series by Rohof et al.13 and Pandolfino et al.27 supports using distensibility index rather than pressure or cross-sectional area to predict treatment outcomes. In the series by Pandolfino et al.,27 the OGJ distensibility index was greatest in the control subjects and smallest in the untreated patients. Furthermore, patients with a good treatment response had a significantly greater OGJ distensibility index than untreated patients or patients with a poor treatment response.
Similar results were published by Rohof et al.,13 where OGJ distensibility was significantly reduced in untreated patients compared with controls. OGJ distensibility also correlated with oesophageal emptying and symptoms, and was significantly higher in patients successfully treated compared with those with residual symptoms after treatment (Eckardt score >3).
However, in the present series EndoFLIP was used more to drive therapy than for predicting success from POEM. Even though it is extremely important in predicting the outcomes of the procedure, ‘distensibility’ (by meaning of a direct function of pressure – mm2/mmHg) can be less useful during the operation, since surgeon and endoscopists want to set the lumen size and not compliance of OGJ. Thus, the ‘diameter of GEJ or its cross-sectional area are more intuitive parameters, and probably more valuable during the procedure.
POEM is different from the Heller-Dor procedure. It is not possible to narrow and restrict the OGJ opening (with an anti-reflux wrap) after myotomy. The myotomy itself cannot be really targeted: myotomy can be complete or incomplete; it can include or not the longitudinal bundles. However, endoscopists cannot cut the inner circular bundles ‘a little bit more’ or ‘a little bit less’. Adjusting to myotomy up to a certain OGJ distensibility index is a fascinating idea, but impractical. In our experience EndoFLIP simply represented an objective, quantitative, controlled way to evaluate whether or not the myotomy was complete.
Furthermore, measuring the diameter that the OGJ opens out to with 30 ml in the balloon gives us a different measure of distensibility: how much the OGJ opens for a given volume in the balloon; 30 ml simulates a bolus pressure of around 10–15 mmHg, probably similar to what happens during physiological swallowing.
However, we recognize that the lack of distensibility data in the present series does not permit to us to completely assess the prognostic value of EndoFLIP, and to properly compare the outcomes of this study with those of previously published series, and consequently represent a significant bias.
One of the most common adverse events after POEM is GORD.7,23 In our series 57.1% of patients had a positive oesophageal pH monitoring, and 33.3% reflux oesophagitis. Nevertheless, only 14.3% had GORD symptoms requiring daily medications. In contrast to surgical Heller myotomy, an anti-reflux procedure is not performed after POEM, leading to an increased incidence of GORD. Incidence of GORD is very variable in published series, from 5–46%.7,23 A wider opening of the OGJ, as seen with the EndoFLIP system, may theoretically favour GORD.8 No correlations between the post-operative OGJ diameter and the incidence of GORD, reflux oesophagitis, and heartburn were observed in the present study. No other studies have correlated GORD incidence with the OGJ diameter after POEM.
However, in a study by Kwiatek et al.8 that compared patients with GORD vs. controls, cross-sectional area (and as a consequence the OGJ diameter) was not significantly different in the two groups of patients, at any level of balloon filling, whereas pressure within the EndoFLIP bas during distension was significantly different at 20 ml, 30 ml and 40 ml filling. A very poor correlation between the endoscopic and EndoFLIP estimates of OGJ distensibility was also observed in the study.
The optimal diameter of OGJ after POEM is still unknown. In a study by Rieder et al.15 the diameter of the OGJ varied from 5.3 mm (range 5.1–5.4 mm) pre-operatively to 9.1 mm (6.2–11.6 mm; p = 0.04) after POEM, with a 30 ml inflated balloon. At the same time, the cross-sectional area increased from 22.0 mm2 (20–32 mm2) to 71.5 mm2 (30–106 mm2, p = 0.06) at a lower median intra-balloon pressure (pre: 29.4 vs. post: 23.7 mmHg), which clearly indicates immediate post-operatively increased OGJ distensibility. In the same study EndoFLIP was tried also on four healthy volunteers, who had a OGJ median diameter of 9.2 mm (7.7–10.7 mm) when the bag was filled with 30 ml. The corresponding cross-sectional area was 64.1 mm2 (44.3–90.9 mm2), with a median intra-bag pressure of 23.2 mmHg (9.6–41.8 mmHg). In a study by Verlaan et al.16 in 10 patients, the median distensibility at 30 ml varied from 1.0 mm2/mmHg (IQR 0.8–1.5) before treatment to 2.9 mm2/mmHg after treatment (1.3–19.6) (p = 0.08).
In the present study the OGJ diameter and cross-sectional area went from 6.3 mm (±1.8 SD) and 32.9 mm2 (±23.1 SD), pre-operatively to 11.3 mm (±1.7 SD) and 102.38 mm2 (±28.2 SD) after POEM. However, it is still unknown what the correct OGJ diameter should be to allow a quick oesophageal emptying, avoiding at the same time the GORD that affected 60% of patients from the series by Verlaan et al.16 and 57.1% of our patients. Furthermore, the effects of POEM on the diameter of the OGJ are often unpredictable, and not really controllable.
EndoFLIP system is a safe and effective technology for the evaluation of the effects of myotomy on the OGJ and LOS. However, additional studies with follow-up are necessary to evaluate the true utility of this system during POEM.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1. Campos GM, Vittinghoff E, Rabl C, et al. Endoscopic and surgical treatments for achalasia: A systematic review and meta-analysis. Ann Surg 2009; 249: 45–57. [DOI] [PubMed] [Google Scholar]
- 2. Cheatham JG, Wong RK. Current approach to the treatment of achalasia. Curr Gastroenterol Rep 2011; 13: 219–225. [DOI] [PubMed] [Google Scholar]
- 3. Boeckxstaens GE, Annese V, des Varannes SB, et al. Pneumatic dilation versus laparoscopic Heller's myotomy for idiopathic achalasia. N Engl J Med 2011; 364: 1807–1816. [DOI] [PubMed] [Google Scholar]
- 4. Hulselmans M, Vanuytsel T, Degreef T, et al. Long-term outcome of pneumatic dilation in the treatment of achalasia. Clin Gastroenterol Hepatol 2010; 8: 30–35. [DOI] [PubMed] [Google Scholar]
- 5. Eckardt VF, Gockel I, Bernhard G. Pneumatic dilation for achalasia: Late results of a prospective follow up investigation. Gut 2004; 53: 629–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010; 42: 265–271. [DOI] [PubMed] [Google Scholar]
- 7. Stavropoulos SN, Modayil RJ, Friedel D, et al. The International Per Oral Endoscopic Myotomy Survey (IPOEMS): A snapshot of the global POEM experience. Surg Endosc 2013; 27: 3322–3338. [DOI] [PubMed] [Google Scholar]
- 8. Kwiatek MA, Pandolfino JE, Hirano I, et al. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc 2010; 72: 272–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McMahon BP, Frokjaer JB, Kunwald P, et al. The functional lumen imaging probe (FLIP) for evaluation of the esophagogastric junction. Am J Physiol Gastrointest Liver Physiol 2007; 292: G377–G384. [DOI] [PubMed] [Google Scholar]
- 10. Hoppo T, McMahon BP, Witteman BP, et al. Functional lumen imaging probe to assess geometric changes in the esophagogastric junction following endolumenal fundoplication. J Gastrointest Surg 2011; 15: 1112–1120. [DOI] [PubMed] [Google Scholar]
- 11. Perretta S, Dallemagne B, McMahon B, et al. Video. Improving functional esophageal surgery with a “smart” bougie: Endoflip. Surg Endosc 2011; 25: 3109–3109. [DOI] [PubMed] [Google Scholar]
- 12. O'Dea J, Siersema PD. Esophageal dilation with integrated balloon imaging: Initial evaluation in a porcine model. Therap Adv Gastroenterol 2013; 6: 109–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rohof WO, Hirsch DP, Kessing BF, et al. Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology 2012; 143: 328–335. [DOI] [PubMed] [Google Scholar]
- 14. Massey BT. EndoFLIP assessment of achalasia therapy: Interpreting the distensibility data is a bit of a stretch. Gastroenterology 2013; 144: e17–e18. [DOI] [PubMed] [Google Scholar]
- 15. Rieder E, Swanstrom LL, Perretta S, et al. Intraoperative assessment of esophagogastric junction distensibility during per oral endoscopic myotomy (POEM) for esophageal motility disorders. Surg Endosc 2013; 27: 400–405. [DOI] [PubMed] [Google Scholar]
- 16. Verlaan T, Rohof WO, Bredenoord AJ, et al. Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc 2013; 78: 39–44. [DOI] [PubMed] [Google Scholar]
- 17. Chiu PW, Wu JC, Teoh AY, et al. Peroral endoscopic myotomy for treatment of achalasia: From bench to bedside (with video). Gastrointest Endosc 2013; 77: 29–38. [DOI] [PubMed] [Google Scholar]
- 18. Costamagna G, Marchese M, Familiari P, et al. Peroral endoscopic myotomy (POEM) for oesophageal achalasia: Preliminary results in humans. Dig Liver Dis 2012; 44: 827–832. [DOI] [PubMed] [Google Scholar]
- 19. Lee BH, Shim KY, Hong SJ, et al. Peroral endoscopic myotomy for treatment of achalasia: Initial results of a Korean study. Clin Endosc 2013; 46: 161–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Minami H, Isomoto H, Yamaguchi N, et al. Peroral endoscopic myotomy for esophageal achalasia: Clinical impact of 28 cases. Dig Endosc 2013; 26: 43–51. [DOI] [PubMed] [Google Scholar]
- 21. Swanstrom LL, Rieder E, Dunst CM. A stepwise approach and early clinical experience in peroral endoscopic myotomy for the treatment of achalasia and esophageal motility disorders. J Am Coll Surg 2011; 213: 751–756. [DOI] [PubMed] [Google Scholar]
- 22. von Renteln D, Inoue H, Minami H, et al. Peroral endoscopic myotomy for the treatment of achalasia: A prospective single center study. Am J Gastroenterol 2012; 107: 411–417. [DOI] [PubMed] [Google Scholar]
- 23. von Renteln D, Fuchs KH, Fockens P, et al. Peroral endoscopic myotomy for the treatment of achalasia: An international prospective multicenter study. Gastroenterology 2013; 145: 309–311. [DOI] [PubMed] [Google Scholar]
- 24. Zhou PH, Yao L, Zhang YQ, et al. PerOral Endoscopic Myotomy (POEM) for esophageal achalasia: 205 cases report. Gastrointest Endosc 2012; 75: AB132–AB133. [Google Scholar]
- 25. Inoue H, Tianle KM, Ikeda H, et al. Peroral endoscopic myotomy for esophageal achalasia: Technique, indication, and outcomes. Thorac Surg Clin 2011; 21: 519–525. [DOI] [PubMed] [Google Scholar]
- 26. Perretta S, Dallemagne B, Donatelli G, et al. Transoral endoscopic esophageal myotomy based on esophageal function testing in a survival porcine model. Gastrointest Endosc 2011; 73: 111–116. [DOI] [PubMed] [Google Scholar]
- 27. Pandolfino JE, de RA, Nicodeme F, et al. Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP) in achalasia patients. Neurogastroenterol Motil 2013; 25: 496–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Teitelbaum EN, Boris L, Arafat FO, et al. Comparison of esophagogastric junction distensibility changes during POEM and Heller myotomy using intraoperative FLIP. Surg Endosc 2013; 27: 4547–4555. [DOI] [PubMed] [Google Scholar]