Abstract
NAL-NL1, the first procedure from the National Acoustic Laboratories (NAL) for prescribing nonlinear gain, was a purely theoretically derived formula aimed at maximizing speech intelligibility for any input level of speech while keeping the overall loudness of speech at or below normal loudness. The formula was obtained through an optimization process in which speech intelligibility and loudness were predicted from selected models. Using updated models and applying some revisions to the derivation process, a theoretically derived NAL-NL2 formula was obtained in a similar way. Further adjustments, directed by empirical data collected in studies using NAL-NL1 as the baseline response, have been made to the theoretically derived formula. Specifically, empirical data have demonstrated that (a) female hearing aid users prefer lower overall gain than male users; (b) new hearing aid users with more than a mild hearing loss prefer increasingly less gain with increasing degree of hearing loss than experienced hearing aid users, and require up to 2 years to adapt to gain levels selected by experienced hearing aid users; (c) unilaterally and bilaterally fitted hearing aid users prefer overall gain levels that vary less than estimated by the bilateral correction factor; (d) adults prefer lower overall gain than children; and (e) people with severe/profound hearing loss prefer lower compression ratios than predicted when fitted with fast-acting compression. The literature and data leading to these conclusions are summarized and discussed in this article, and the procedure for implementing the adjustments to the theoretically derived NAL-NL2 formula is described.
Keywords: prescription, amplification, loudness, gender, age, experience, binaural loudness summation, NAL-NL2, NAL-NL1, hearing aid fitting
Introduction
The first prescription procedure developed by the National Acoustic Laboratories (NAL) for prescribing nonlinear gain (NAL-NL1) was introduced in 1999 (Byrne, Dillon, Katsch, Ching, & Keidser, 2001; Dillon, 1999). The prescription aims at maximizing speech intelligibility while ensuring that the overall loudness of speech does not exceed that perceived by normal-hearing listeners. The actual formula was derived through an optimization process that included modeling of effective speech intelligibility and loudness (Dillon, 2001). The speech intelligibility maximization rationale followed on from extensive research performed at NAL on linear prescription procedures that suggested that the best gain–frequency response for speech understanding was one that equalized, rather than normalized, loudness of speech bands (e.g., Byrne & Cotton, 1988; Byrne & Dillon, 1986). This was therefore different from a frequency-specific loudness normalization rationale, which at the time was more commonly used to fit nonlinear amplification (e.g., Cornelisse, Seewald, & Jamieson, 1995; Cox, 1995; Killion & Fikret-Pasa, 1993). When the NAL-NL1 formula was derived, the rationale of maximizing speech intelligibility for any input level was largely untested for nonlinear amplification. It was assumed that the close approximation of the NAL-NL1 prescription at medium input levels to the NAL-RP prescription (Byrne, Parkinson, & Newall, 1990) for linear gain was appropriate, but no other data were available to lend support to the final formula. Since the release of NAL-NL1, the preference for its prescribed gain-frequency response shape has been verified against a pure loudness normalization rationale (Keidser & Grant, 2001) and, therefore, the aim of speech intelligibility maximization was maintained in NAL-NL2. Consequently, as described in Dillon, Flax, Keidser, Ching, and Katsch (in press), the theoretical formula of NAL-NL2 is derived in a similar way to that of NAL-NL1. A speech intelligibility and loudness model is used in an optimization process in which the speech intelligibility model defines the gain-frequency response shape and the loudness rule prevents the optimization process from producing gain-frequency responses for different input levels of speech that produce the same output.
While it seemed intuitive to control loudness in such a way that the overall loudness of sounds was kept close to normal overall loudness for any input level of speech, there were, prior to introducing NAL-NL1, no data to support this principle. After NAL-NL1 was released, very early clinical reports suggested that many clients did not, in fact, tolerate the NAL-NL1 prescribed overall gain. In 2000, a retrospective survey of 39 audiologists across Australia, who had extensively used NAL-NL1, revealed that an estimated 61% of clients, on average, found the overall loudness of their hearing aids (HAs) “just right” immediately after fitting, while 33% reported the instruments made sounds too loud. Only 6% reported that sounds were too soft. At the follow-up appointment, after clients had had a few weeks to adapt to their fine-tuned instruments, the percentage of clients who seemed satisfied with the overall gain setting had increased to 71%, on average, while 21% still reported gain to be too high. The fact that nearly one in three people still had problems with their amplification being either too loud or too soft at the follow-up appointment was of concern. The survey did not provide information that could suggest the profile of clients who did not accept the prescribed gain, or if gain needed adjustment due to intolerance of low-frequency, high- frequency, or overall gain, or gain at low, medium, or high input levels. Consequently, several studies were initiated to obtain a better understanding of the factors that influenced loudness preferences.
At the same time, NAL-NL1 was used as the prescribed baseline response in many research projects, and many such studies have also provided valuable information about the gain preferred by hearing aid (HA) users in their everyday environments. Specifically, outcomes from a wide range of studies conducted over the past decade suggest that different populations prefer relatively different loudness to that prescribed on the basis of their hearing loss. Such empirical data have been taken into consideration when developing NAL-NL2, and adjustments have been made to the theoretically derived NAL-NL2 formula described in Dillon et al. (in press) to ensure that appropriate gain is prescribed to all HA users.
In this article, the empirical data directing the adjustment of the theoretical predictions that form the baseline for the NAL-NL2 formula is reviewed and discussed, and the resulting adjustments presented. Not all the empirical data provided strong evidence, and the article concludes by listing the areas in which further research is needed.
Overall Loudness Adjustments
At the end of the derivation process described in Dillon et al. (in press), it was found that the theoretically derived NAL-NL2 formula generally prescribed overall gain (averaged across the frequencies from 0.5 to 4.0 kHz) that was similar to the overall gain prescribed by NAL-NL1. As mentioned in the introduction, clinical anecdotes suggested that for at least one third of clients, the NAL-NL1-prescribed overall gain needed adjustments, mainly reduction. This was subsequently confirmed by studying the fitting results of 189 individuals who participated in different research projects at NAL between 2000 and 2006 (Keidser, Carter, Chalupper, & Dillon, 2007a; Keidser, Dillon, Dyrlund, Carter, & Hartley, 2007b; Keidser et al., 2005b; Keidser & Grant, 2001; Keidser, O’Brien, Carter, McLelland, & Yeend, 2008b). For all study participants, real-ear insertion gain (REIG) measurements of their preferred, or fine-tuned, response was available for a medium (65 dB) input level. From these measurements the preferred overall gain was obtained by averaging the gain values across 0.5, 1, 2, and 4 kHz. The preferred overall gain was then compared to the individually prescribed NAL-NL1 gain averaged across the same frequencies. When participants were bilaterally fitted, gain was further averaged across ears. This approach ignores interparticipant differences in gain variations to target at individual frequencies that may result from such factors as the specific receiver response characteristic, feedback, large vents, and individual gain preferences. The approach is deemed justifiable, nevertheless, as the study by Keidser et al. (2008b) specifically investigated gain preferences overall, and at low and at high frequencies in a population of 76 hearing-impaired listeners, and found that significant differences that applied to overall gain were not affected by individual preferences for more or less gain at specific frequency bands. Furthermore, open fittings that generally prevent amplified gain from being transmitted at frequencies below1.5 kHz were not included in this investigation.
Figure 1 shows the preferred overall gain for each individual, relative to the NAL-NL1 prescription, as a function of the average hearing threshold level (HTL) measured across 0.5, 1, 2, and 4 kHz (4FA HTL). If allowing for a variation of 3 dB in preferred gain, it would seem that the overall gain prescribed by NAL-NL1 was acceptable to only 50% of the study participants, while 45% preferred lower gain and 5% preferred higher gain. Thus these data confirm that for many clients, especially those with mild or moderate hearing loss, NAL-NL1 prescribed gain was too high. On average, the study participants preferred 3.2 dB less overall gain than prescribed, which is largely in agreement with the preferred gain deviation of 4.3 dB from the NAL-R prescription procedure found across various studies (Byrne & Cotton, 1988; Cox & Alexander, 1992; Convery, Keidser, & Dillon, 2005; Horwitz & Turner, 1997; Humes, Wilson, Barlow, & Garner, 2002) that have been discussed in Keidser and Dillon (2006). It is also in agreement with Boymans and Dreschler (2012) who found that a patient driven fine-tuning approach conducted in the laboratory resulted in 3.2 dB lower overall gain than the best match to the NAL-NL1 target achieved by audiologists. Consequently, the starting point for further loudness adjustments is the theoretical NAL-NL2 prescription less 3 dB overall gain.
Figure 1.
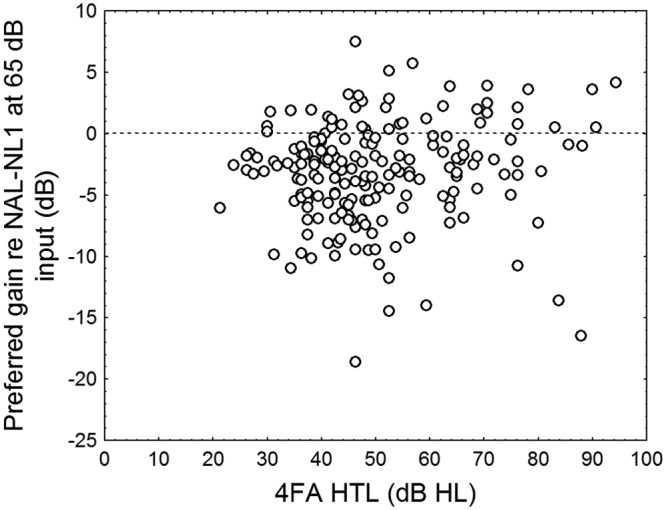
The preferred overall gain, measured across 0.5, 1, 2, and 4 kHz, relative to NAL-NL1 prescribed overall gain as a function of the degree of hearing loss for 189 adult hearing aid users participating in one of five different research studies
Further information that was available for all our research study participants in Figure 1 included degree of hearing loss (4FA HTL in dB HL), slope of audiogram (dB), age (years), gender (female/male), experience with amplification (inexperienced/experienced), and aid configuration (unilateral/bilateral). These parameters were used as independent variables in a forward stepwise multiple regression analysis to determine whether there was a model that could predict the preferred gain deviation from the NAL-NL1 prescription better than by chance. Data from five outliers who produced variations that exceeded three times the standard deviation of residuals were excluded from the analysis. They were the 5 study participants who selected more than 13 dB less gain than preferred (cf. Figure 1). A significant model (F6, 175 = 10.0, p < .0000001) that included all six parameters and explained 25% of the variance was found. The regression coefficients, partial correlations, coefficient of determination, and significance level are shown for each parameter in Table 1. According to this model, the least gain relative to that prescribed was preferred by younger, inexperienced, unilaterally fitted females with mild, flat hearing loss. Overall, gender, aid configuration, and experience with amplification contributed most to the model. These three parameters direct the amount of gain prescribed by NAL-NL2 and are presented and discussed further below.
Table 1.
The Parameters of the Model Predicting Preferred Gain Deviation From the NAL-NL1 Prescription and Their Regression Coefficients (β and B), Partial Correlations, Coefficient of Determination (R-squared), and Significance Level (p level)
| Parameter | β | B | Partial correlation | Semipartial correlation | R-squared | p level |
|---|---|---|---|---|---|---|
| Gender (F/M) | 0.22 | 1.68 | 0.22 | 0.20 | 0.22 | 0.0028 |
| Aid configuration (U/B) | 0.23 | 1.91 | 0.26 | 0.23 | 0.03 | 0.0006 |
| Aid experience (N/E) | 0.20 | 1.49 | 0.20 | 0.18 | 0.19 | 0.0067 |
| 4FA HTL (dB HL) | 0.15 | 0.04 | 0.15 | 0.13 | 0.22 | 0.0448 |
| Age (years) | 0.10 | 0.03 | 0.11 | 0.10 | 0.07 | 0.1439 |
| Slope (dB) | 0.09 | 0.02 | 0.09 | 0.08 | 0.27 | 0.2200 |
Note: F = female; M = male; U = Unilateral; B = Bilateral; N = no experience; E = experience.
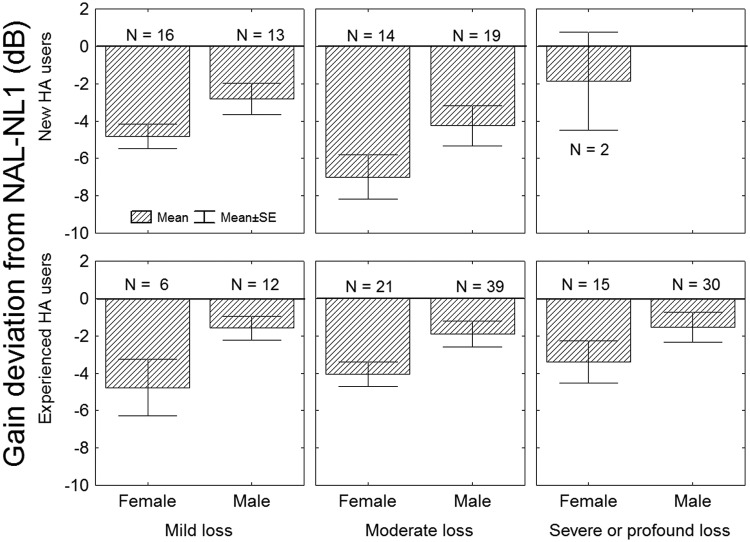
Gender Effect
Gender was one of the stronger predictor of the selected gain deviation from the NAL-NL1prescription. On average, female HA users preferred 2.4 dB less gain than male HA users, a difference that according to a t test is highly statistically significant (t = −4.09, p = .00006). As can be seen in Figure 2, this significant difference appears to be consistent across degree of hearing loss and experience with amplification. The classification of hearing loss into mild, moderate, and severe/profound is determined by the 4FA HTL being less than or equal to 40 dB HL, between 40 and 60 dB HL, and greater than 60 dB HL, respectively.
Figure 2.
The average preferred overall gain, measured across 0.5, 1, 2, and 4 kHz, relative to NAL-NL1 prescribed overall gain, for 189 hearing aid users participating in one of five different research studies, shown by gender, degree of hearing loss, and hearing aid experience
Note: Bars show plus and minus one standard error.
Cox, Alexander, Taylor, and Grey (1997) cite two studies reporting that female listeners with normal hearing rate a particular level significantly louder than normally hearing male listeners in loudness scaling tests using narrow-band stimuli (Kiessling, Steffens, & Wagner, 1993; Nielsen, 1995). In both studies the difference between loudness functions was about 6 dB. According to Kiessling et al. (1993), the gender effect observed in their study was in agreement with data from Hellbrück (1983). Supporting these findings are data by Rogers, Harkrider, Burchfield, and Nabelek (2003), who also found that male listeners with normal hearing selected, on average, significantly higher most comfortable levels (MCL) when listening to speech than did female listeners, with a difference of approximately 6 dB. Rogers et al. (2003) further speculated that the generally lower MCL measured in females is partly explained by the female cochlea being more sensitive to acoustic stimulation as demonstrated in various studies on otoacoustic emissions. Cox and colleagues found a trend in the same direction of about 3 dB in their normative data obtained for a new loudness test, but the gender effect was not statistically significant. Likewise, Ventry, Woods, Rubin, and Hill (1971) and Hochberg (1975) reported that female listeners with normal hearing chose lower MCLs than male listeners. In Ventry et al. (1971), this difference applied when listening to pure tones (9.3 dB) and noise (2.3 dB), but not when listening to speech (0.2 dB). In Hochberg (1975), the stimulus was speech and the difference in preferred level was 3.3 dB. However, in none of these cases was the gender effect significant. Bentler and Cooley (2001), who examined the threshold of discomfort data obtained on 710 ears (103 with normal hearing and 607 with impaired hearing) across five studies, did not find gender to be a predictive variable of measured discomfort levels. Overall, it would seem that, at least around the comfortable loudness level, females prefer to listen to softer levels than males. Although not all findings were statistically significant, it was felt that there was sufficient support to justify the introduction of a gender effect into NAL-NL2. Based on the data in Figure 2, the overall gain is increased by 1 dB for males and reduced by 1 dB for females (relative to the corrected NAL-NL2 prescribed overall gain) whenever gender of the client is specified. This gain adjustment is independent of frequency and input level.
Experience Effect
Experience also contributed to the prediction of preferred gain deviation from the NAL-NL1 prescription in the 189 fitting results shown in Figure 1. On average, new HA users preferred 2.2 dB less gain than experienced HA users, a difference that was significant according to a t test (t = 3.48, p = .0006). A closer look at Figure 2 reveals that experience seems to have a greater effect on people with moderate hearing loss than on people with mild hearing loss. A proportion of the 189 fitting results reviewed above stems from a study that directly investigated the effect of experience on preferred overall gain (Keidser et al., 2008b). For that study, 50 new clients and 26 return clients who had worn amplification for at least 3 years were recruited. They were all fitted with Siemens Music Pro instruments: a digital, three-memory, two-channel compression device equipped with a volume control. Each participant was fitted with three programs, where possible, consisting of the NAL-NL1-prescribed response (all participants), NAL-NL1 with a low-frequency cut (32 participants), and NAL-NL1 with a high-frequency cut (all participants). The participants were encouraged to experiment with the different programs and volume control settings in their everyday environments. One, 4, and 13 months postfitting, new HA users returned to the clinic to have the REIG of their preferred program and volume control setting for general listening in the field (excluding very loud listening conditions) recorded. For experienced HA users, the preferred response was only recorded 1 month postfitting and this measure served as a reference. The study found that on average, new HA users preferred 2.7 dB less gain than experienced HA users, a difference that was not statistically significant. When dividing study participants into two groups depending on their 4FA HTL, it was found that when the 4FA HTL ≤ 43 dB HL, there was no significant difference between gain preferred by new and experienced HA users after 1 month of adaptation to the new device. Furthermore, there was no significant change in gain preferred over time by new HA users with a milder hearing loss (Figure 3). However, new HA users with a 4FA HTL > 43 dB HL preferred progressively less overall gain than prescribed as the degree of hearing loss increased (about − 1dB gain per 3 dB of hearing loss). On average, they preferred significantly less gain (6 dB) than experienced HA users with a 4FA HTL > 43 dB HL. It was also found that among the new HA users with higher degree of hearing loss, a significant gain adaptation took place but was not completed after 13 months of HA usage (cf. Figure 3). These significant differences applied to overall gain and were not affected by individual preferences for more or less gain, relative to that prescribed, at low or high frequencies.
Figure 3.
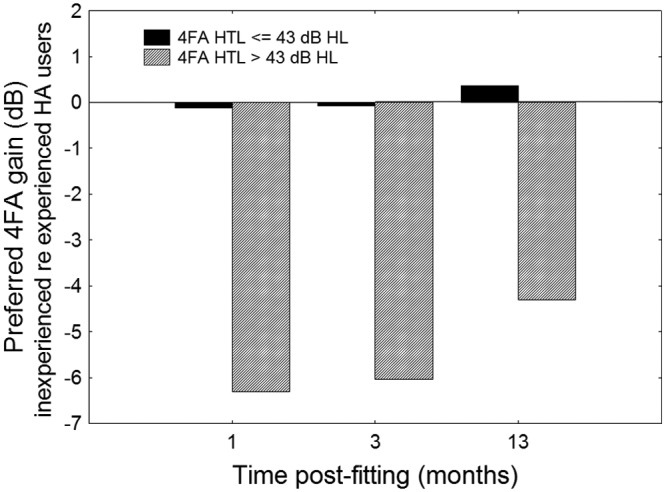
The difference in average overall gain relative to NAL-NL1 prescribed overall gain, measured across 0.5, 1, 2, and 4 kHz, preferred by new hearing aid users 1, 4, and 13 months after fitting and users with more than 3 years of hearing aid experience
Note: The full and hatched bars show data for participants with a mild and a moderate or greater degree of hearing loss, respectively.
The findings in Keidser et al. (2008b) is not directly in conflict with Convery et al. (2005), who concluded, based on an extensive literature review, that there was no support for using gain adaptation with new HA users, or Smeds et al. (2006), who found no significant difference in preferred overall loudness between new and experienced HA users when listening through HAs. Specifically, the review suggested that new HA users, on average, preferred 2 dB less gain than experienced HA users, but that the difference was not statistically significant and was independent of the time, up to 12 months, at which gain preferences were measured postfitting. None of the studies reviewed by Convery et al. (2005) controlled for the effect of degree of hearing loss, and in many investigations experience was defined as at least 1 year’s use of amplification, a time frame that data from Keidser et al. (2008b) suggest is not sufficient. In Smeds et al. (2006), the new HA users had quite mild hearing loss, with an average 4FA HTL of about 35 dB HL. They were therefore likely to accept gain levels similar to those accepted by their experienced counterparts.
Clients presenting with more than a mild hearing loss are likely to have had unaided hearing loss for longer and thus have become more accustomed to a quieter world before seeking rehabilitation with HAs. Therefore, it seems reasonable that only this population may initially find the prescribed gain overwhelming while slowly adapting to appropriately prescribed gain levels over time. Based on this background, an experience effect has been introduced with NAL-NL2 for those with a 4FA HTL exceeding 40 dB HL that will be implemented if a client is categorized as a “new” user. Figure 4 shows the hearing loss dependent gain reduction applied to new hearing aid users that is derived from the data presented in Keidser et al. (2008b). Note that because the data set collected in Keidser et al. (2008b) did not include HA users with a 4FA HTL exceeding 55 dB HL, the suggested gain reduction for new HA users is only progressive to a 4FA HTL of 60 dB HL, after which it becomes constant. The uniform gain reduction selected for higher degrees of hearing loss is partly due to lack of evidence that gain reduction should be progressive beyond this point and partly due to a reluctance to further reduce overall gain for those who most need it. In fact, for experienced HA users with a greater degree of hearing loss, there is no adjustment made to the theoretical NAL-NL2 formula (cf. Figure 4), as there is no evidence to suggest that gain should be reduced for this population. This approach was partly confirmed in a recent study (Convery & Keidser, 2011), in which experienced HA users with severe or profound hearing loss generally presented with overall gain slightly higher than that prescribed by NAL-RP (Byrne et al., 1990), which is very close to that prescribed by NAL-NL1 for medium input levels and hence that prescribed by the theoretically derived NAL-NL2 formula. The hearing loss dependent gain adjustments related to experience are independent of frequency and input level.
Figure 4.
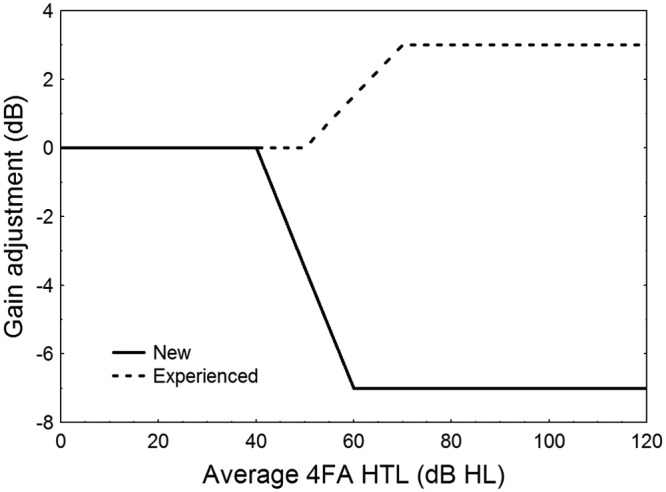
The implemented gain adjustment in NAL-NL2 as a function of degree of hearing loss for level of experience
In the study by Keidser et al. (2008b), it was noted that there was no significant correlation between the overall gain preferences of experienced HA users and experience with amplification beyond 3 years. Consequently, that study concluded that the time course of gain adaptation for new HA users was between 13 and 36 months. Of the 17 new HA users from the Keidser et al. (2008b) study who presented a 4FA HTL between 44 and 55 dB HL, 11 agreed to continue to have their gain preferences monitored every 6 months until they had worn their HA(s) for 36 months. At each appointment, the participants’ hearing threshold was also tested at 0.5, 1, 2, and 4 kHz. Over the 36 months, the participants showed an average decrease in 4FA HTL of 3 dB that mostly occurred over the last 12 months. This change in threshold was taken into account when deriving the (higher) target gain that the new HA users were expected to adapt to over time and that is shown by the broken line in Figure 5. Figure 5 further shows at each measurement point the average gain deviation values selected by the 11 participants. The dotted line shows two times the standard error of the target gain. At 24 months, the average preferred gain by the new HA users falls within the 95% confidence interval of the expected gain variation for experienced HA users, meaning that there is no longer a significant difference in overall gain preferred by the two groups. The observed average gain adaptation at 24 months was 3.2 dB, but increased to 4.0 dB if excluding 1 participant who was the only one to systematically reduce gain over time. There is a noticeable reduction in preferred gain from 30 to 36 months that is mainly due to 2 participants who suddenly reduced their preferred gain by about 4.0 dB. Up until their 36-month appointment, these 2 participants showed gain preferences that were consistent with the overall trend, and no cause other than random fluctuation has been found to explain the change. Overall, this data suggest that gain adaptation may occur gradually over the first two years of HA usage in new HA users with higher degrees of hearing loss.
Figure 5.
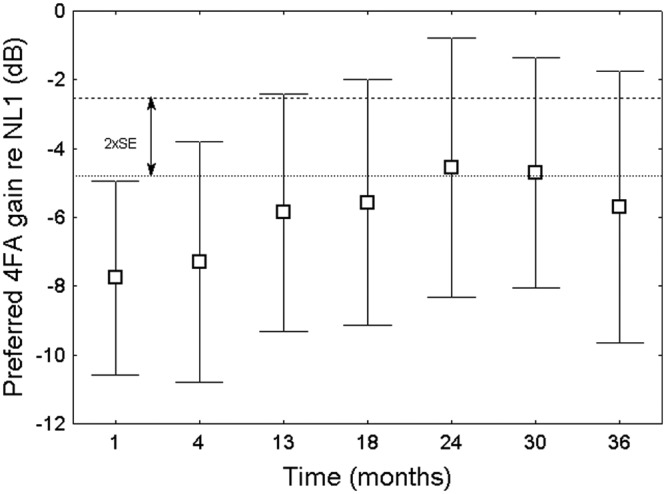
The mean preferred gain deviation from the NAL-NL1 prescription over time
Note: The bars show the 95% confidence bands. The broken line shows the average gain to which the participants were expected to adapt (taking a general shift in threshold into account) and the dotted line shows two times the standard error (SE) of that value.
The limited data on adaptation time in new users support speculations by Keidser et al. (2008b) that adjustment to higher gain takes between 13 and 36 months and also supports speculations by Palmer, Nelson, and Lindley (1998) that neural plasticity in the auditory system is likely to happen when the hearing loss is substantial. On average, the participants did not adapt fully to the target gain. Possible reasons for the shortfall include the small number of participants, the fact that the subgroup consisted mainly of HA users whose gain preferences were at the lower end of the range of observed gain preferences, and that the lower limit of an acceptable range of volume control settings had been reached. The last suggestion implies that gain closer to 100% gain adaptation may be accepted by the HA users if gain was automatically and incrementally increased over the first 24 months of HA usage. In terms of implementing gradual gain increases over this period of time, it is technically feasible to incorporate a feature that enables slow and automatic gain increases in hearing instruments (e.g., Robinson & Verberne, 2003; Schum & Beck, 2006). Assuming that new users would seek higher overall gain levels over time, trainability (Dillon et al., 2006; Zakis, McDermott, & Dillon, 2007) is another feature available to adjust to gain adaptation. However, where these features are not available, and the client is unable to manage a volume control, it would be the responsibility of the hearing service provider to ensure that gain is gradually increased for new HA users with a moderate or greater degree of hearing loss over the first two years of HA usage.
Bilateral Corrections
Aid configuration was one of the significant parameters contributing to the model explaining the overall gain preferred by 189 research participants. According to a t test for independent samples, those who were unilaterally fitted preferred significantly less gain by 2 dB than those who were bilaterally fitted (t = 3.58, p = .0004). Bilateral corrections were introduced in NAL-NL1 and thus it is assumed (but cannot be confirmed) that those who were unilaterally fitted were, on average, fitted with relatively higher gain than those who were bilaterally fitted. In NAL-NL1, more loudness summation was assumed for higher than lower input levels. For an input level of 65 dB SPL, the difference in prescribed gain between unilaterally and bilaterally fitted HA users was just more than 5 dB, when a symmetrical hearing loss is assumed, a compensation which our data suggest may be slightly too large.
The bilateral correction introduced in NAL-NL1 was based on a literature review (summarized in Dillon, 2001) that suggests that in normal ears, binaural summation of loudness increases from about 3 dB near threshold to 6 to 10 dB at comfortable and high sound pressure levels. Limited data available for hearing-impaired listeners suggested that binaural loudness summation in hearing-impaired ears was similar or perhaps slightly less than in normal ears (Dermody & Byrne, 1975; Hall & Harvey, 1985; Hawkins, Prosek, Walden, & Montgomery, 1987). Consequently, NAL-NL1 prescribed 3 dB more gain for a unilateral fit relative to a bilateral fit for input levels below 40 dB SPL, with a linear increase in the bilateral gain correction with increasing input level up to 8 dB at 90 dB SPL and above. The level-dependency means that unilaterally fitted people are prescribed higher compression ratios (CR) than those who are bilaterally fitted.
More recent studies confirm that binaural loudness summation changes with level in normal ears, and suggest that it is greatest (10 dB) at medium input levels around 60 dB SPL (e.g., Marozeau & Florentine, 2009; Whilby, Florentine, Wagner, & Marozeau, 2006). The same studies showed that binaural loudness summation is less in impaired than in normal ears, a finding that presumably in part is due to the steeper loudness growth functions typically measured for hearing-impaired listeners. A study by Epstein and Florentine (2009) has further demonstrated that binaural loudness summation is less when listening to a visible live talker than when listening to recorded speech and tones presented through loudspeakers or over headphones, conditions that previous data are based on. Taken together, recent studies support the suggestion of the above data that the bilateral compensation in NAL-NL1 was too large. Consequently, the bilateral correction factor has been reduced in NAL-NL2 to provide 2 dB more gain for a unilateral than a bilateral fitting for input levels below 40 dB SPL and to linearly increase gain for increasing input levels up to 6 dB at 90 dB SPL and above (Figure 6). That is, for a 65 dB SPL input, the correction factor is reduced to 4 dB. These correction factors apply to a perfectly symmetrical hearing loss. The gain difference between unilateral and bilateral fittings decreases as the asymmetry between ears increases up to 50 dB, when no correction is deemed necessary (Tobias, 1963; Tonning, 1971). How the difference in gain (dG) between unilateral and bilateral fittings relates to the degree of asymmetry is shown in Equation 1 where AC is the air conduction threshold and L the input level.
Figure 6.
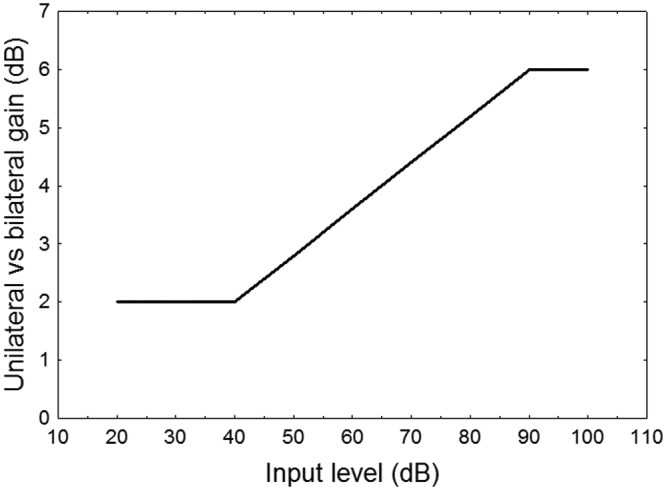
The difference in gain applied by NAL-NL2 to a unilateral and bilateral hearing loss when the asymmetry between ears is 0 dB
| (1) |
It should be noted that the correction factors make up the best estimate from average data as individual differences in binaural loudness summation among the hearing-impaired listeners were evident in both Whilby et al. (2006) and Marozeau and Florentine (2009).
Age Effect
Among the adult population (> 20 years) whose data are illustrated in Figure 1, age also contributed to the model that predicted the preferred gain relative to the NAL-NL1 prescription. However, the correlation between the two factors, suggesting that younger people preferred the greatest gain reduction, is very weak (r = .13) and not significant (p = .08). Furthermore, among the older adults (> 60 years) with an acquired hearing loss, who made up the largest proportion of the test participants (~90%), age is confounded with the degree of hearing loss that gets significantly more severe as the person grows older. Consequently, an effect of age in adults would need to be investigated in a more controlled study.
Other data, however, suggest that children prefer higher overall gain levels than adults. In a collaborative study between NAL and the University of Western Ontario in Canada, the NAL-NL1 and Desired Sensation Level Input-Output (DSL[i/o]) version 4.1 (Cornelisse et al., 1995) prescriptions were compared by 48 children across the two sites (Ching, Scollie, Dillon, & Seewald, 2010). Prior to testing the children, the study protocol was evaluated at NAL using 11 hearing-impaired adults. Although the two prescription procedures differ in both the prescribed frequency response slope and overall gain, the main difference in the fittings achieved was in overall gain, with the DSL[i/o] fitting rationale providing, on average, 7 dB more gain than the NAL-NL1 prescription for a medium input level to the children. Among the adults, DSL[i/o] was found to be significantly louder than NAL-NL1 in a loudness rating test. After a brief evaluation in the field, 1 adult showed a small preference for DSL[i/o] over NAL-NL1, while 7 had a strong overall preference for NAL-NL1 over DSL[i/o]. Following a period of acclimatization, the children showed no significant difference in their loudness ratings between the prescription procedures (Scollie et al., 2010b). In the field, more children (24) preferred DSL[i/o] than preferred NAL-NL1 (17; Scollie et al., 2010a). Taken together with the data in Figure 1, these findings suggest that children may prefer higher overall gain levels than adults.
It was hypothesized that the apparent difference in preference for overall gain by children and adults may be related to when the hearing loss was acquired rather than age. During one study conducted at NAL, part of which is presented in Keidser et al. (2007b), 43 adults with severe or profound hearing loss were fitted with the same device according to the NAL-RP prescription and with CRs prescribed by the manufacturer. Of these test participants, 15 had a congenital hearing loss and 28 had an acquired hearing loss. For each participant, the gain values were extracted at 0.25, 0.5, 1, 2, 3, and 4 kHz from the REIG curve obtained for a 70 dB SPL input of the fine-tuned response. The average gain across these six frequencies was compared to the prescribed gain at the same frequencies. The difference in the gain deviation from the NAL-RP prescription selected by the two groups of participants was 0.61 dB. According to a t test, this difference was not statistically significant (t = 0.53; p = .6). Based on these data sets, NAL-NL2 distinguishes between children and adults, using the entered year of birth, and prescribes 5 dB more gain for a 65 dB input level for children than for adults. That is, relative to the theoretically derived NAL-NL2 formula, the overall prescribed gain for children is increased by 2 dB for an input level of 65 dB SPL. The findings also suggest that at some point in time people with congenital hearing loss will want the overall gain reduced. Presumably the gain reduction should be implemented gradually, but it is currently unknown when to commence gain reduction and over which period it should take place.
Compression
Up to this point the data analyzed and discussed have mainly concerned gain preferences for a 65 dB input level. Only the bilateral correction factor is known to depend on input level and, consequently, unilaterally fitted people will be prescribed a higher CR than bilaterally fitted people. The effect of gender and experience is assumed to apply to all input levels, but what effect may age have on gain preferences at high and low input levels?
Age Effect on Preferred Gain at High and Low Input Levels
Scollie et al. (2010a) reported that most children preferred DSL[i/o] for listening to soft speech and NAL-NL1 for listening in loud, noisy environments. For children, an increase in gain is more likely to lead to greater speech intelligibility at low input levels where speech may be limited by audibility and is less likely to cause a noise-induced hearing loss if introduced at low than at high input levels. Therefore, it seemed desirable for the children to increase gain relative to the NAL-NL1 prescription more at low than at medium input levels and not at all at high input levels, an approach that called for a higher CR for children than prescribed by NAL-NL1. Coincidentally, independent data also suggested that a higher CR than that prescribed by NAL-NL1 was preferred by adults, at least by those with mild and moderate hearing loss. In two studies, test participants were fitted with a research device that frequently logged information about the intensity of the environment and the volume control setting while used in the field (Smeds et al., 2006; Zakis et al., 2007). The baseline response in both studies was the NAL-NL1 prescription. The logged data confirmed all previous findings that adult HA users reduce gain relative to the NAL-NL1 prescription for a 65 dB SPL input level. These two studies further demonstrated that relatively more gain reduction (1.5 dB, on average) was preferred for higher intensity levels around 80 dB SPL, whereas relatively less gain reduction (1 dB, on average) was preferred for lower intensity levels around 50 dB SPL. As described in Dillon et al. (in press), higher CRs are prescribed by the theoretically derived NAL-NL2 formula as a result of an update to the speech intelligibility model.
Compression Limit for Fast-Acting Compression
One of the advantages of nonlinear amplification is that it can make a wide range of input levels available within a narrower range of hearing and, for many people with an elevated threshold, compression is necessary to make even all speech sounds audible. The smaller the dynamic range of hearing is at a given frequency, the higher a CR would be needed to make all speech sounds audible. However, applying compression to the rapidly fluctuating speech signal causes some level of distortion to both the spectral and temporal cues (e.g., Bustamante & Braida, 1987; Moore, 1990; Plomp, 1988), and several studies suggest that for people with mild or moderate hearing loss such distortions have a deleterious effect on speech discrimination, or diminish ratings of sound quality and preference, when using CRs much greater than 3:1 in conjunction with fast time constants and multiple channels (Keidser et al., 2005a; Neuman, Bakke, Mackersie, Hellman, & Levitt, 1998; Plomp, 1994; Verschuure, Prinsen, Dreschler, 1994). Therefore, a compromise between audibility and acceptable sound quality and optimum speech understanding seems inevitable.
From the optimized data produced for NAL-NL2 (Dillon et al., in press), it was apparent that without some constraints, the prescribed CR would in some cases be well in excess of 3:1 even for a person with a moderate degree of hearing loss. To date, most research on the effect of compression on speech has been conducted using fast attack and release times to respond to rapid changes in input level. However, Neuman et al. (1998) did observe that when using a CR of 3:1, the rating of clarity, pleasantness, and overall impression increased, while background noise was rated less noisy, with increasing release time (up to 1000 ms). It would therefore seem that when longer time constants are used, such that compression acts more like an automatic volume control, higher CR could be used to provide audibility of a wider range of sounds without compromising speech intelligibility and listening comfort. The discrepancy between CRs accepted for fast and slow acting compression would most likely be largest for people with more severe and profound hearing loss who display very narrow dynamic ranges of hearing. Although based on limited data, it was decided to introduce a limit to the CR for fast-acting compressors.
The maximum values introduced for fast-acting compression are shown in Figure 7. It can be seen that the maximum CR values are within 3:1 across all frequencies and degrees of hearing loss. It may be noted that lower CRs are chosen for profound hearing loss relative to moderate and severe hearing loss, especially across the lower frequencies. This was guided by data collected by Keidser et al. (2007b), which suggest that people with profound hearing loss prefer amplification in the low frequencies to be more linear than is preferred by people with moderately severe hearing loss. The data were based on a field evaluation of different combinations of the CRs (1:1, 1.8:1, and 3:1) implemented in the low and high frequencies, as outlined in Table 2, by 21 experienced HA users with moderately severe or profound hearing loss. The compression schemes were implemented in a fast-acting device (5 msec attack and 70-120 msec release) and compared pair-wise in the field for 3 weeks each using an adaptive procedure. According to this procedure, all participants first compared the four schemes combining the CRs of 1:1 and 3:1at low (LF) and high (HF) frequencies [LF CR; HF CR]; that is, [1:1, 1:1], [1:1, 3:1], [3:1, 1:1], and [3:1, 3:1]. Thereafter, each individual compared their preferred combination of 1:1 and 3:1 with combinations including 1.8:1 compression. For example, if the winning combination of the first round was [1:1, 3:1], then this scheme was compared with schemes [1:1, 1.8:1], [1.8:1, 1.8:1], and [1.8:1, 3:1]. During each field test, participants filled in structured diaries about their experiences and at the end of each field test they completed an exit interview during which a forced choice of preference for either of the two schemes was made. The losing scheme exited the trial while the winning scheme was compared with a yet untested scheme.
Figure 7.
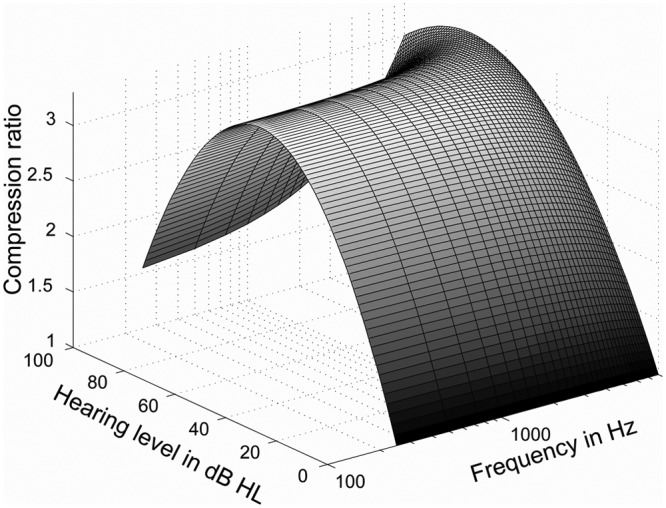
The maximum compression ratios accepted with fast-acting compression in NAL-NL2 as a function of degree of hearing loss and frequency
Table 2.
The Compression Schemes Trialed in an Adaptive Fashion in Keidser et al. (2007)
| Scheme | CR LF | CR HF | First round (all) | Second round (example, individual) |
|---|---|---|---|---|
| 1 | 1:1 | 1:1 | X | |
| 2 | 1:1 | 1.8:1 | X | |
| 3 | 1:1 | 3:1 | X | X |
| 4 | 1.8:1 | 1:1 | ||
| 5 | 1.8:1 | 1.8:1 | X | |
| 6 | 1.8:1 | 3:1 | X | |
| 7 | 3:1 | 1:1 | X | |
| 8 | 3:1 | 1.8:1 | ||
| 9 | 3:1 | 3:1 | X |
Note: CR = Compression ratio; LF = low frequencies (≤ 1 kHz); HF = high frequencies (≥2 kHz).
The data from this study suggested a nonlinear relationship between the preferred CR at the low frequencies and the degree of low-frequency hearing loss, where the optimum CR increases when the low-frequency HTL (LF HTL) increases from moderate to severe after which the optimum CR decreases to reach linear for a profound hearing loss. Specifically, 5 participants with an average LF HTL of 75 dB HL and above all chose linear amplification in the low-frequency band, presumably because higher CRs distort temporal and prosodic cues in the speech signal on which this population heavily relies, while another 5 participants, all with an average LF HTL around 70 dB HL preferred 1.8:1 compression. Participants with lower LF HTL randomly chose either 1:1 or 1.8:1 compression, suggesting that the optimum CR for them was somewhere between these two discrete values. Higher CRs were generally preferred in the high frequencies; see Keidser et al. (2007b) for further details.
To avoid inadvertently high CRs to be prescribed by the NAL-NL2 formula for fast-acting compressors, the optimized data were filtered through a function based on the CR limits outlined in Figure 7. Whenever the CR arising from the speech intelligibility optimization calculations exceeded the CR limits, the gains prescribed by the optimizer were adjusted as follows: no change was made to the gains prescribed for speech at an overall input level of 65 dB SPL, the gains for lower input levels were decreased relative to the gains resulting from the optimizer, by just the amount needed to ensure that the appropriate CR limit was not exceeded, and the gains for higher input levels were increased to achieve the same aim. These adjusted gains were then used to train the neural network on which the final prescription formula is based, as described in Dillon et al (in press). Training was performed separately using the adjusted gains to derive a formula appropriate to fast compression and using the unadjusted gains to derive a formula appropriate to slow compression, resulting in two different formulas for the two types of compression. Note that the difference in prescribed CR with these two formulas is negligible for people with mild and moderate hearing loss.
Evaluation and Future Research
All the loudness adjustments introduced in this article are based on average data although interparticipant differences exist as is evident throughout the presentation. This is, however, in agreement with the general principle that prescription procedures provide a baseline response that is assumed to be appropriate for the average listener and from which fine-tuning to individual preferences can be made. A comparison of NAL-NL2 with other generic prescription procedures, including NAL-NL1, in terms of impact on loudness and speech intelligibility is presented by Johnson and Dillon (2011). This investigation confirms, that relative to NAL-NL1, lower overall loudness that is also well below normal overall loudness is achieved with NAL-NL2. According to this investigation, NAL-NL2 prescribed gain generally appears more similar to that prescribed by DSLm[i/o] (Scollie et al., 2005) than that of CAMEQ2-HF (Moore, Glasberg, & Stone, 2010).
The final NAL-NL2 prescription procedure has yet to be formally evaluated in a clinical study. It is our experience, however, from a couple of research studies, which have used the NAL-NL2 prescription as baseline response, that less fine-tuning is required than when NAL-NL1 was used. This would suggest that NAL-NL2 makes a better general starting point. As demonstrated in recent studies, starting from an appropriately prescribed baseline response is important as self-adjustments, or training of hearing aids, are biased by the starting point (Dreschler, Keidser, Convery, & Dillon, 2008; Keidsser, Convery, & Dillon, 2008a; Mueller, Hornsby, & Weber, 2008), which means that audiologist-driven fine-tuning probably is too. Because hearing aids are more likely to be equipped with a volume than a tone control, verifying the prescribed gain-frequency response shape, which results primarily from the speech intelligibility modeling in the optimization process described in Dillon et al. (in press), should have highest priority in future evaluation studies. Nevertheless, not all devices offer a volume control and not all users are able or inclined to use onboard controls, and hence further verification of the various overall gain adjustments, introduced to the theoretically derived NAL-NL2 prescription and described in this article, would also be desirable.
Of the various parameters that affected overall gain preference, gender resulted in the smallest variation of 2 dB, which may appear insignificant taking into account the accuracy with which target generally is reached. It should be noted though that various studies have found differences in loudness perception between normally hearing males and females of up to 6 dB, and, therefore, a systematic investigation into the effect of gender on overall gain preference among HA users would be beneficial. Such an investigation could further include a study on the interactive effect of gender and age, as it is currently unknown if gender has an effect on gain preferences among children. The other effects introduced are more substantial and it would be of interest to specifically verify the real-life validity of the bilateral correction factor, which primarily stems from data measured under headphones on normal-hearing listeners using less ecologically valid stimuli, which also ignore real-life factors such as visual cues, distance, and reverberation (e.g., Florentine & Epstein, 2011). Stronger evidence for gain preferences among HA users with severe or profound hearing loss is also called for.
Other factors that should be more thoroughly investigated in the future include the time course of adaptation to fully prescribed gain levels among new users with higher degree of hearing loss. Such a study would be very valuable as it could result in better agreement among proprietary adaptation managers and encourage manufacturers to implement a feature in hearing devices that automatically applies increased gain over time for new users. A similarly important question to answer is at what time overall gain should be reduced for children, or young adults. This question may be less of an issue for people who start to wear HAs at a young age, because they will presumably prefer and be able to select lower gain levels at some point in time, or gradually over time. However, it would be useful to know how much gain to prescribe to a person who acquires a hearing loss as a young adult. Finally, there may be other audiological, psychophysical, or cognitive factors that affect HA users’ preference for overall gain and that have not been captured in this review.
Summary
Empirical data collected during the past decade suggest that different populations prefer different overall gain relative to that prescribed by NAL-NL1, which for all HA users aimed at keeping the overall loudness of speech at any input level at or below normal overall loudness. These data have been reviewed, and the adjustments made to NAL-NL2 as a result have been outlined. Specifically, for a 65 dB input level, NAL-NL2 prescribes 3 dB less overall gain than NAL-NL1 for adults with mild or moderate hearing loss and 2 dB more overall gain for children. Relative to this adjustment, specification of gender results in further prescription of 1 dB less gain for females and 1 dB more gain for males. New users with a 4FA hearing loss greater than 40 dB HL will have gain increasingly reduced by up to 7 dB for an average hearing loss of 60 dB HL and above. The new users are expected to gradually adapt to gain levels prescribed to experienced HA users with a similar degree of hearing loss over a period of 2 years. The gradual adaptation is managed either by an algorithm built into the hearing instrument, where available; by using a trainable feature; or manually by the clinician. Finally, the bilateral correction factor has been revised such that unilaterally fitted HA users are prescribed increasingly higher gain, from 2 dB at a 40 dB input level to 6 dB for an input level of 90 dB SPL, relative to bilaterally fitted HA users with symmetrical hearing loss. It is further noted that empirical data support the use of different CRs for NAL-NL2 relative to NAL-NL1 and for different compressor speed for those with high degree of hearing loss.
Acknowledgments
The authors would like to thank the many audiologists who were involved in data collection, especially Lisa Hartley, David Hartley, Ingrid Yeend, Margot McLelland, and Heidi Limareff, and the many volunteers who participated in the various and sometimes lengthy studies. We are also grateful to Siemens, GN ReSound, and the Oticon Foundation who sponsored some of the studies referred to in this article.
Footnotes
Authors’ Note: Part of this article has been presented at the International Hearing Aid Research Conference, Lake Tahoe, August 2010; the International Conference on Adult Hearing Screening, Cernobbio, June 2010; the Audiology Australia XIX National Conference, Sydney, May 2010; the Canadian Academy of Audiology, Toronto, October 2009; the National Hearing Care Audiology Team Conference, Hobart, October 2009; the IX Connexx Pro Workshop, Nyborg Strand, August 2009; the 53rd International Congress of Hearing Aid Acousticians, Leipzig, October 2008; the New Zealand Audiological Society 32nd Annual Conference, Christchurch, July 2008; the Audiology Australia XVIII National Conference, Canberra, May 2008; AudiologyNOW 2008, Charlotte NC, April 2008; the Australian College of Audiology, Adelaide, September 2007; Phonak’s Hearing Care for Adults conference, Chicago, November 2006.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The development of NAL-NL2 was financially supported by the HEARing CRC established and supported under the Australian Government’s Cooperative Research Centres Program.
References
- Bentler R. A., Cooley L. J. (2001). An examination of several characteristics that affect the prediction of OSPL90 in hearing aids. Ear and Hearing, 22(1), 58-64 [DOI] [PubMed] [Google Scholar]
- Boymans M., Dreschler W. A. (2012). Audiologists-driven versus patient-driven fine tuning of hearing instruments. Trends in Amplification, 16(1), 49-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bustamante D., Braida L. (1987). Multichannel compression limiting for hearing-impaired listeners. Journal of Rehabilitation Research and Development, 24, 149-160 [PubMed] [Google Scholar]
- Byrne D., Cotton S. (1988). Evaluation of the National Acoustic Laboratories’ new hearing aid selection procedure. Journal of Speech and Hearing Research, 31, 178-186 [DOI] [PubMed] [Google Scholar]
- Byrne D., Dillon H. (1986). The National Acoustic Laboratories’ (NAL) new procedure for selecting the gain and frequency response of a hearing aid. Ear and Hearing, 7, 257-265 [DOI] [PubMed] [Google Scholar]
- Byrne D., Dillon H., Katsch R., Ching T., Keidser G. (2001). The NAL-NL1 procedure for fitting non-linear hearing aids: characteristics and comparisons with other procedures. Journal of the American Academy of Audiology, 12(1), 37-51 [PubMed] [Google Scholar]
- Byrne D., Parkinson A., Newall P. (1990). Hearing aid gain and frequency response requirements for the severely/profoundly hearing-impaired. Ear and Hearing, 11(1), 40-49 [DOI] [PubMed] [Google Scholar]
- Ching T., Scollie S., Dillon H., Seewald R. (2010). A cross-over, double-blind comparison of the NAL-NL1and the DSL v4.1 prescriptions for children with mild to moderately severe hearing loss. International Journal of Audiology, 49(S1), S4-S15 [DOI] [PubMed] [Google Scholar]
- Convery E., Keidser G. (2011). Transitioning hearing aid users with severe and profound loss to a new gain/frequency response: Benefit, perception, and acceptance. Journal of the American Academy of Audiology, 22, 168-180 [DOI] [PubMed] [Google Scholar]
- Convery E., Keidser G., Dillon H. (2005). A review: Does amplification experience have an effect on preferred gain over time? Australian & New Zealand Journal of Audiology, 27(1), 18-32 [Google Scholar]
- Cornelisse L. E., Seewald R. C., Jamieson D. G. (1995). The input/output formula: A theoretical approach to the fitting of personal amplification devices. Journal of the Acoustical Society of America, 97, 1854-1864 [DOI] [PubMed] [Google Scholar]
- Cox R. (1995). Using loudness data for hearing aid selection: The IHAFF approach. Hearing Journal, 48(2), 39-44 [Google Scholar]
- Cox R. M., Alexander G. C. (1992). Maturation of hearing aid benefit: objective and subjective measurements. Ear and Hearing, 13(3), 131-141 [DOI] [PubMed] [Google Scholar]
- Cox R. M., Alexander G. C., Taylor I. M., Grey G. A. (1997). The Contour Test of Loudness Perception. Ear and Hearing, 18, 388-400 [DOI] [PubMed] [Google Scholar]
- Dermody P., Byrne D. (1975). Loudness summation with binaural hearing aids. Scandinavian Audiology, 4(1), 23-28 [Google Scholar]
- Dillon H. (1999). NAL-NL1: A new procedure for fitting non-linear hearing aids. Hearing Journal, 52(4), 10-16 [Google Scholar]
- Dillon H. (Ed.). (2001). Hearing aids (pp. 255-256, 380). Sydney, Australia: Boomerang Press [Google Scholar]
- Dillon H., Flax M., Keidser G., Ching T., Katsch R. (in press). Derivation of the NAL-NL2 procedure. Trends in Amplification. [Google Scholar]
- Dillon H., Zakis J., McDermott H., Keidser G., Dreschler W., Convery E. (2006). The trainable hearing aid: What will it do for clients and clinicians? Hearing Journal, 59, 30-36 [Google Scholar]
- Dreschler W. A., Keidser G., Convery E., Dillon H. (2008). Client-based adjustments of hearing-aid gain: the effect of different control configurations. Ear and Hearing, 29, 214-227 [DOI] [PubMed] [Google Scholar]
- Epstein M., Florentine M. (2009). Binaural loudness summation for speech and tones presented via earphones and loudspeakers. Ear and Hearing, 30, 234-237 [DOI] [PubMed] [Google Scholar]
- Florentine M., Epstein M. (2011). Measures of the ecological loudness of speech. In Dau T., Jepsen M. L., Poulsen T., Dalsgaard J. C. (Eds.), Speech perception and auditory disorders (pp. 89-94). Denmark: Centretryk [Google Scholar]
- Hall J. W., Harvey A. D. (1985). Diotic loudness summation in normal and impaired hearing. Journal of Speech and Hearing Research, 28, 445-448 [DOI] [PubMed] [Google Scholar]
- Hawkins D. B., Prosek R. A., Walden B. E., Montgomery A. A. (1987). Binaural loudness summation in the hearing impaired. Journal of Speech and Hearing Research, 30, 37-43 [DOI] [PubMed] [Google Scholar]
- Hellbrück J. (1983). Geschlechtsspezifische Unterschiede in der Lautstärkeempfindung—Resalität oder Artefakt? Psychologie, 30, 387-399 [PubMed] [Google Scholar]
- Hochberg I. (1975). Most comfortable listening for the loudness and intelligibility of speech. Audiology, 14(1), 27-33 [DOI] [PubMed] [Google Scholar]
- Horwitz A. R., Turner C. W. (1997). The time course of hearing aid benefit. Ear and Hearing, 18(1), 1-11 [DOI] [PubMed] [Google Scholar]
- Humes L. E., Wilson D. L., Barlow N. N., Garner C. (2002). Changes in hearing-aid benefit following 1 or 2 years of hearing-aid use by older adults. Journal of Speech, Language and Hearing Research, 45, 772-782 [DOI] [PubMed] [Google Scholar]
- Johnson E. E., Dillon H. (2011). A Comparison of Gain for Adults from Generic Hearing Aid Prescriptive Methods: Impacts on Predicted Loudness, Frequency Bandwidth, and Speech Intelligibility. Journal of the American Academy of Audiology, 22, 441-459 [DOI] [PubMed] [Google Scholar]
- Keidser G., Brew C., Brewer S., Dillon H., Grant F., Storey L. (2005a). The preferred response slopes and two-channel compression ratios in twenty listening conditions by hearing-impaired and normal-hearing listeners and their relationship to the acoustic input. International Journal of Audiology, 44, 656-670 [DOI] [PubMed] [Google Scholar]
- Keidser G., Carter L., Chalupper J., Dillon H. (2007a). Effect of low-frequency gain and venting effects on the benefit derived from directionality and noise reduction in hearing aids. International Journal of Audiology, 46, 554-568 [DOI] [PubMed] [Google Scholar]
- Keidser G., Convery E., Dillon H. (2008a). The effect of the baseline response on self-adjustments of hearing aid gain. Journal of the Acoustical Society of America, 124, 1668-1681 [DOI] [PubMed] [Google Scholar]
- Keidser G., Dillon H. (2006). What’s new in prescriptive fittings Down Under? In Palmer C. V., Seewald R. (Eds.), Hearing care for adults 2006 (pp.133-142). Stafa, Switzerland: Phonak AG [Google Scholar]
- Keidser G., Dillon H., Dyrlund O., Carter L., Hartley D. (2007b). Preferred compression ratios in the low and high frequencies by the moderately severe to severe-profound population. Journal of the American Academy of Audiology, 18(1), 17-33 [DOI] [PubMed] [Google Scholar]
- Keidser G., Grant F. (2001). comparing loudness normalization (IHAFF) with speech intelligibility maximization (NAL-NL1) when implemented in a two-channel device. Ear and Hearing, 22, 501-515 [DOI] [PubMed] [Google Scholar]
- Keidser G., Limareff H., Simmons S., Gul C., Hayes Z., Sawers C., Korchek K. (2005b). Clinical evaluation of Australian Hearing’s guidelines for fitting multiple memory hearing aids. Australian & New Zealand Journal of Audiology, 27(1), 51-68 [Google Scholar]
- Keidser G., O’Brien A., Carter L., McLelland M., Yeend I. (2008b). Variation in preferred gain with experience for hearing aid users. International Journal of Audiology, 47, 621-635 [DOI] [PubMed] [Google Scholar]
- Kiessling J., Steffens T., Wagner I. (1993). [On the clinical applicability of loudness scaling]. Audiologische Akustik, 32, 100-115 [Google Scholar]
- Killion M., Fikret-Pasa S. (1993). The 2 types of sensorineural hearing loss. Loudness and intelligibility considerations. Hearing Journal, 46(11), 31-34 [Google Scholar]
- Marozeau J., Florentine M. (2009). Testing the binaural equal-loudness-ratio hypothesis with hearing-impaired listeners. Journal of the Acoustical Society of America, 126, 310-317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore B. C. J. (1990). How much do we gain by gain control in hearing aids? Acta Otolaryngology, 469(Suppl.), 250-256 [PubMed] [Google Scholar]
- Moore B. C. J., Glasberg B. R., Stone M. A. (2010). Development of a new method for deriving initial fitting for hearing aids with multichannel compression: CAMEQ2-HF. International Journal of Audiology, 49, 216-227 [DOI] [PubMed] [Google Scholar]
- Mueller H. G., Hornsby B. W. Y., Weber J. E. (2008). Using trainable hearing aids to examine real-world preferred gain. Journal of the American Academy of Audiology, 19, 758-773 [DOI] [PubMed] [Google Scholar]
- Neuman A. C., Bakke M. H., Mackersie C., Hellman S., Levitt H. (1998). The effect of compression ratio and release time on the categorical rating of sound quality. Journal of the Acoustical Society of America, 103, 2273-2281 [DOI] [PubMed] [Google Scholar]
- Nielsen J. R. (1995). Loudness scaling: Influence from some experimental parameters (Report No. 65; The Acoustics Laboratory, Technical University of Denmark). Copenhagen, Denmark: Technical University of Denmark [Google Scholar]
- Palmer C. V., Nelson C. T., Lindley G. A.(1998). The functionally and physiologically plastic adult auditory system. Journal of the Acoustical Society of America, 103, 1705-1721 [DOI] [PubMed] [Google Scholar]
- Plomp R. (1988). The negative effect of amplitude compression in multichannel hearing aids in the light of the modulation-transfer function. Journal of the Acoustical Society of America, 83, 2322-2327 [DOI] [PubMed] [Google Scholar]
- Plomp R. (1994). Noise, amplification, and compression: considerations of three main issues in hearing aid design. Ear and Hearing, 15, 2-12 [PubMed] [Google Scholar]
- Robinson J., Verberne J. (2003). Satisfy: Slow adaptation to ideal settings for you. Beltone, pp 1-4 [Google Scholar]
- Rogers D. S., Harkrider A. W., Burchfield S. B., Nabelek A. K. (2003). The influence of listener’s gender on the acceptance of background noise. Journal of the American Academy of Audiology, 14, 372-82 [PubMed] [Google Scholar]
- Schum D. J., Beck D. L. (2006). Meta Controls and advanced technology amplification. News from Oticon, pp 1-8 [Google Scholar]
- Scollie S. D., Ching T., Seewald R., Dillon H., Britton L., Steinberg J., Corcoran J. (2010a). Evaluation of the NAL-NL1 and DSL v4.1 prescriptions for children: Preference in real world use. International Journal of Audiology, 49(S1), S49-S63 [DOI] [PubMed] [Google Scholar]
- Scollie S. D., Ching T., Seewald R., Dillon H., Britton L., Steinberg J., King A. K. (2010b). Children’s speech perception and loudness ratings when fitted with hearing aids using the DSL v.4.1 and the NAL-NL1 prescriptions. International Journal of Audiology, 49(S1), S26-S34 [DOI] [PubMed] [Google Scholar]
- Scollie S., Seewald R., Cornelisse L., Moodie S., Bagatto M., Laurnagaray D., Plumford J. (2005). The desired sensation level multistage input/output algorithm. Trends in Amplification, 9, 159-197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smeds K., Keidser G., Zakis J., Dillon H., Leijon A., Grant F., Brew C. (2006). Preferred overall loudness. II: Listening through hearing aids in field and laboratory tests. International Journal of Audiology, 45(1), 12-25 [DOI] [PubMed] [Google Scholar]
- Tobias J. V. (1963). Application of a “relative” procedure to a problem in binaural-beat perception. Journal of the Acoustical Society of America, 35, 1442-1447 [Google Scholar]
- Tonning F. M. (1971). Directional audiometry III. Acta Otolaryngol, 72, 404-412 [DOI] [PubMed] [Google Scholar]
- Ventry I. M., Woods R. W., Rubin M., Hill W. (1971). Most comfortable loudness for pure tones, noise, and speech. Journal of the Acoustical Society of America, 49, 1805-1813 [DOI] [PubMed] [Google Scholar]
- Verschuure H., Prinsen T. T., Dreschler W. A. (1994). The effects of syllabic compression and frequency shaping on speech intelligibility in hearing impaired people. Ear and Hearing, 15(1), 13-21 [DOI] [PubMed] [Google Scholar]
- Whilby S., Florentine M., Wagner E., Marozeau J. (2006). Monaural and binaural loudness of 5- and 200- ms tones in normal and impaired hearing. Journal of the Acoustical Society of America, 119, 3931-3939 [DOI] [PubMed] [Google Scholar]
- Zakis J. A., McDermott H. J., Dillon H. (2007). The design and evaluation of a hearing aid with trainable amplification parameters. Ear and Hearing, 28, 812-830 [DOI] [PubMed] [Google Scholar]