Abstract
The influence of client–clinician interactions has not been emphasized in hearing health care, despite the extensive evidence of the impact of the provider–patient interaction on health outcomes. The purpose of this study was to identify factors in the client–clinician interaction that may influence hearing aid adoption. Thirteen adults who had received a hearing aid recommendation within the previous 3 months and 10 audiologists participated in a study to generate, sort, and rate the importance of factors in client–clinician interaction that may influence the hearing aid purchase decision. A concept mapping approach was used to define meaningful clusters of factors. Quantitative analysis and qualitative interpretation of the statements resulted in eight concepts. The concepts in order of their importance are (a) Ensuring client comfort, (b) Understanding and meeting client needs, (c) Client-centered traits and actions, (d) Acknowledging client as an individual, (e) Imposing undue pressure and discomfort, (f) Conveying device information by clinician, (g) Supporting choices and shared decision making, and (h) Factors in client readiness. Two overarching themes of client-centered interaction and client empowerment were identified. Results highlight the influence of the client–clinician interaction in hearing aid adoption and suggest the possibility of improving hearing aid adoption by empowering clients through a client-centered interaction.
Keywords: hearing aid adoption, client–clinician interaction, client-centered care, concept mapping
There are many reported factors related to the low adoption rate of hearing aids. Among the factors that influence hearing aid adoption are (a) assumption that hearing loss is a part of the normal aging process (Humphrey, Herbst, & Faurqi, 1981), (b) attitudes toward hearing loss and hearing aids (Brooks & Hallam, 1998), (c) stigma attached to hearing loss and hearing aids (Biggs, 1997; Erler & Garstecki, 2002), (d) hearing sensitivity (Garstecki & Erler, 1998; Humphrey et al., 1981; Swan & Gatehouse, 1990), (e) perceived seriousness of the hearing impairment (Duijvestijn et al., 2003; Swan & Gatehouse, 1990; van den Brink, Wit, Kempen, & van Heuvelen, 1996), (f) quality and cost of the hearing aids; and need for an acclimatization period (Lee & Lotz, 1998).
Amplification is the most common intervention recommended for persons with hearing problems (Chisolm et al., 2007). A challenge for hearing health care professionals has been to raise the adoption rate of hearing aids. In spite of the advancement in hearing aid technology over the past 20 years the number of individuals who own hearing aids relative to the number of people with hearing loss is still low. Communication can be improved in 90% of people with hearing loss through properly fitted hearing aids (World Health Organization, 2006); however, only 20% of people who could benefit from amplification actually own hearing aids (National Institute on Deafness and Other Communication Disabilities, 2008). Half of individuals with hearing-related complaints seek professional help (Humphrey et al., 1981). New hearing aid users comprise 38.8% of all users (Kochkin, 2005). These statistics suggest that a large proportion of individuals who seek hearing health care and may be potential hearing aid candidates do not follow through with hearing aid recommendations.
Despite reports that hearing care professionals can influence hearing aid uptake (Kochkin, 2009), research on hearing aid uptake has focused primarily on satisfaction with, and the limitations of the hearing instruments themselves rather than on the client–clinician interactions that lead to hearing aid acquisition per se (Wong, Hickson, & McPherson, 2003). The top three factors that have been identified as influencing first-time hearing aid owners’ hearing aid purchase decision are (a) the individual’s perception that his or her hearing loss has worsened, (b) the influence of the family members, and (c) the audiologist (Kochkin, 2009). The extent to which, and the process of how, audiologists affect hearing aid adoption have not been studied. A recent MarkeTrack survey investigated the impact of the hearing health care professional on hearing aid user success (Kochkin et al., 2010). Clients rated the attributes of hearing health care professionals including knowledge, professionalism, empathy, creation of realistic expectations, explained care and maintenance of hearing aids, and quality of service during and after the fitting process. The hearing health care professional and the fitting process were correlated with hearing aid user success. Client’s beliefs or desires, in combination with what hearing health care professionals tell their clients, regardless of what the professionals actually do, even before the provision of hearing aids, may influence the client’s perception of the outcome (Abrams, Chisolm, & Saunders, 2005). The quality of the clinical encounter, including such factors as treatment expectations and clinicians’ expertise, is an important factor considered by potential clients of hearing services (Milhinch & Doyle, 1990).
The impact of the physician–patient interaction on medical practice outcomes has been extensively studied in the medical field (Bensing, 1991; Dasinger, Krause, Thompson, Brand, & Rudolph, 2001; Dibbelt, Schaidhammer, Fleischer, & Greitemann, 2009; Griffin et al., 2004; Stewart et al., 1999). Physician–patient communication is referred to as the most important aspect of health care (Silverman, Kurtz, Draper, & Kurtz, 1998) and influences the physiological, behavioral, and subjective measures of health status (Kaplan, Greenfield, & Ware, 1989). Perceived quality of the physician–patient interaction correlates with long-term treatment results in rehabilitation (Dibbelt et al., 2009). However there is a lack of empirical evidence regarding the influence of the client–clinician interaction on hearing aid uptake (Vestergaard Knudsen, Öberg, Nielsen, Naylor, & Kramer, 2010).
According to contemporary psychology, the interaction between an individual and his or her situation can determine the individual’s behavior (Magnusson, 1976). If we can establish how a new situation is typically interpreted by individuals or groups of individuals and their disposition to behave in this kind of situation, we can predict behavior in a new situation (Magnusson, 1976). Therefore if we know how a novel encounter such as the hearing aid adoption process is interpreted by clients and clinicians, we may be able to foresee how the client–clinician interaction may influence clients’ hearing aid purchase decisions and to understand how clinicians interact with a new hearing aid client. Insights into the client–clinician interaction can help us identify factors that may influence clients’ inclination toward the uptake of hearing aids and may lead to suggestions on how to improve the interaction. The purpose of this research was to investigate clients’ and clinicians’ views of factors in the client–clinician interactions that may influence first time hearing aid candidates in their hearing aid purchase decision. The specific goals of this research was to (a) identify factors in initial client–clinician interactions that may influence the hearing aid purchase decision in first time hearing aid candidates, (b) develop a conceptual framework for the identified factors, and (c) investigate the importance of these factors to clients and clinicians.
Method
Participants
The views of both persons with hearing loss (clients) and hearing health care professionals (clinicians) were sought. The client group included persons between 45 and 85 years of age (Mean = 70.84) with an acquired sensorineural hearing loss and who had received a hearing aid recommendation within the 3 months prior to the study, regardless of whether a hearing aid was acquired. Thirteen clients were recruited and participated in some components of the study. Two of the clients were recruited through their clinicians and 11 were recruited directly through advertisements in a local newspaper. The client group demographic is summarized in Table 1.
Table 1.
Description of the Client Participants, Their Hearing Status, and Hearing Aid Ownership
| Sex | Age | Hearing aid | HF Ave-RE | HF Ave-LE | |
|---|---|---|---|---|---|
| Client 1 | M | 70 | No | 51 | 56 |
| Client 2 | F | 70 | Yes | 43 | 38 |
| Client 3 | M | 70 | No | 38 | 55 |
| Client 4 | F | 74 | No | 48 | 53 |
| Client 5 | M | 78 | Yes | 21 | 30 |
| Client 6 | F | 69 | Yes | 41 | 33 |
| Client 7 | F | 48 | Yes | 53 | 43 |
| Client 8 | F | 77 | Yes | 53 | 36 |
| Client 9 | M | 81 | Yes | 36 | 50 |
| Client 10 | M | 74 | No | 46 | 53 |
| Client 11 | F | 80 | Yes | 63 | 43 |
| Client 12 | F | 67 | No | 35 | NR |
| Client 13 | F | 63 | Yes | 48 | 55 |
Note: HF Ave is the mean air conduction threshold in dB HL in 1, 2, and 4 KHz.
The inclusion criteria for the clinicians included hearing health care professionals (audiologists and hearing instrument specialists/hearing aid dispensers) from a variety of clinical settings who prescribed and dispensed hearing aids. An invitation to participate in the study was mailed and emailed to clinicians who were within 1 hr driving distance from the research center. Hearing instrument specialists did not respond to the letter of invitation. Participants in the clinician group consisted of 10 audiologists who participated in some parts of the study. Clinician participants were from university clinics (n = 2), owners and employees of sole ownership settings (n = 5), and those who worked in private practice chains (n = 3). There were 3 male and 7 female clinicians. Three of the clinicians had less than 5 years experience, 3 had 5 to 10, and 4 had more than 10 years of clinical experience.
Procedures
Concept mapping (Kane & Trochim, 2007; Trochim & Kane, 2005) was used to develop a two dimensional concept map of factors in client–clinician interactions that were perceived by participants to influence hearing aid adoption. Concept mapping allows a group of participants to voice their ideas, give objective meanings to their ideas, and then represent the ideas in a visual map (Trochim, 1989). Concept mapping is also a good fit when the goal of the research is the assessment of the quality of health care, planning, or evaluation of health care services (Trochim & Kane, 2005). Concept mapping has been widely used in health care contexts, including the development of long-term care report cards, development of conceptual frameworks for complex constructs such as quality of care, and development of guidelines for public health management of lower prevalence chronic conditions (Elbeck & Fecteau, 1990; Groenwoud, van Exel, Berg, Huijsman, 2008; van der Waal, Casparie, & Lako, 1996; Wheeler, Anderson, Boddie-Willis, Price, & Kane, 2005).
Ethics approval for the study was granted by the University of Western Ontario Ethics Review Board. Group sessions took place at the National Centre for Audiology at the University of Western Ontario, London, Ontario. The first author facilitated the group sessions and was assisted by an audiologist cofacilitator. Both facilitators had experience in interviewing and conducting group adult aural rehabilitation sessions. The four steps of concept mapping, (a) brainstorming, (b) sorting and rating, (c) data analysis, and (d) interpretation, were followed to collect and analyze the data.
Brainstorming
Seven audiologists and 12 clients participated in group brainstorming sessions at the National Centre for Audiology. There were four brainstorming sessions, two for client groups and two for clinician groups. In these sessions, participants were asked to think about the period of time between when a person decides to book an appointment with a hearing care professional and the time when a hearing aid is recommended. Participants were asked to, “Generate statements that describe factors in the client–clinician interaction that influence the hearing aid purchase decision.” The statements were displayed on a large screen for participants to see as they were created. The statements generated in the four brainstorming sessions were compiled. To ensure that participants had a clear, understandable, and relevant list of ideas that were not redundant and to have a manageable number of statements for the next task, the research team reviewed all the items to eliminate redundant ideas. The statements were edited for clarity and to ensure they were syntactically similar for both groups. The resulting set of statements served as the core content for the sorting and rating tasks.
Sorting and Rating of the Statements
Ten audiologists and 11 clients completed an individual unstructured sort of the statements. The client group completed the sorting and rating tasks in two sessions held at the National Centre for Audiology. The sorting and rating material and instructions were mailed to the participants in the clinician group and completed tasks were returned by mail. Statements were numbered and each statement was printed on a separate card. Participants were asked to sort the cards into piles based on how similar in meaning they were to one another and in a way that made sense to them. To complete the sorting task, participants were provided the following instructions: (a) there is no right or wrong way to group the statements, (b) they should create at least 5 piles, (c) a statement could be put in its own pile if it is unrelated to the other statements or if it stands alone as a unique idea, and (d) they should not have a “Miscellaneous” or “Other” pile. Participants were given a form to record the statements in each pile and asked to provide a title that captured the content of the pile.
For the rating task, participants were given the list of statements and asked to rate the relative importance of each statement on a client’s decision to purchase hearing aids using a 5-point Likert-type scale (1 = minimally important, 2 = somewhat important, 3 = moderately important, 4 = very important, 5 = extremely important).
Multidimensional Scaling (MDS) and Hierarchical Cluster Analysis
Data were entered into the Concept Systems software (2011) and nonmetric MDS analysis (Davison, 1983) was conducted using the sort data. A symmetric N × N binary similarity matrix, where N was the number of statements, was generated for each participant and the individual matrices were added together to produce a total similarity matrix. The total similarity matrix indicates how many participants paired the same two statements into the same group. The total similarity matrix was then transformed into a matrix of distances between the items, which was used to create the point map. Each point on the map represents a brainstormed statement. The statements that were grouped together more often by participants are closer together in the two dimensional space than statements that were grouped together less frequently. Hierarchical cluster analysis grouped individual statements on the point map into clusters of statements that reflect similar concepts (Kane & Trochim, 2007).
The importance rating data was transformed into a matrix with 5 importance categories. The rating data were averaged across all participants, each item, and each cluster. The importance ratings were averaged twice, first across all participants and a second time across all items in a cluster. As a result, even slight importance rating differences between clusters may be considered meaningful (Trochim, 1989). The strength of the MDS was tested by computing a stress index. The stress index indicates the goodness of fit of the two dimensional configuration to the combined sort data. A lower stress value indicates a better fit between the concept map and similarity matrix. For concept mapping studies a stress value lower than 0.35 is recommended (Kane & Trochim, 2007; Trochim, 1993). A split-half reliability measure was also conducted for this study. Participants’ sorting data were randomly assigned to two subgroups. Separate similarity matrices were computed for each subgroup and were correlated. Reliability is affected by the number of participants. Split half reliability is based on the calculation of only half of the total number of participants; as a result it does not reflect the correlational value for the entire sample. This issue was corrected by applying the Spearman–Brown Prophecy Formula to the split half correlation (Trochim, 1993).
Interpretation
Three audiologists and 4 clients participated in the interpretation of the maps. Separate group sessions were held for each participant group. The goal of these sessions was to present the results to participants, describe how they have contributed to the results, and label the clusters in a meaningful way. Participants were asked to review the statements in each cluster and create a word or a short phrase that described the group of statements as a cluster. The number of clusters that were presented to participants for interpretation was decided by the research team (Kane & Trochim, 2007). The maximum number of cluster solutions was decided based on two factors: (a) the number of clusters that were expected to be interpretable for the context under the investigation and (b) the average number of piles sorted by participants. The research team reviewed the statements and the labels that were created by participants for each cluster. The research team generated a short description for each cluster and labels were finalized so that the titles represented the overall concept and the majority of the statements in that cluster.
Results
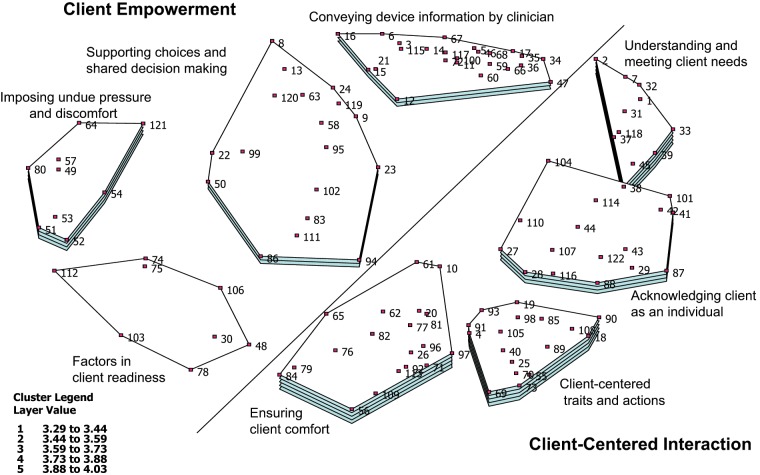
Hierarchical cluster analysis of the point map yielded an eight-cluster solution (Figure 1). The eight factors in the client–clinician interaction that influence the hearing aid purchase decision in order of their average importance are (a) Ensuring client comfort, (b) Understanding and meeting client needs, (c) Client-centered traits and actions, (d) Acknowledging client as an individual, (e) Imposing undue pressure and discomfort, (f) Conveying device information by clinician, (g) Supporting choices and shared decision making, and (h) Factors in client readiness. The average importance ratings for the clusters ranged from 3.29 for factors in client readiness (the least important) to 4.03 for ensuring client comfort (the most important). The eight concepts, a short description of each concept, and examples of statements in each concept are summarized in Table 2. The complete list of statements in each concept can be found in the appendix.
Figure 1.
Concept map depicting eight clusters with layers indicating average importance ratings for the cluster
Note: Each dot and the number adjacent to the dot represent a brainstormed statement.
Table 2.
Eight Clusters in Client–Clinician Interactions That Influence Hearing Aid Adoption, a Short Description for Each Concept and Examples of Statements in Each Cluster
| Concept | Description | Sample statements |
|---|---|---|
| Ensuring client comfort | Client comfort in different dimensions including physical and psychological | The client feels that the clinician is sincere in his or her intentions. (96) The amount of time spent with the client. (62) The client doesn’t feel pressured. (65) The physical environment is comfortable and welcoming. (84) |
| Understanding and meeting client needs | Assessing the client as an individual and explaining the assessment results and how they relate to each individual client’s communication needs | The clinician asks what situations are difficult for the client. (37) The clinician relates the assessment results to the difficulty they are having. (33) The clinician considers the client’s lifestyle and/or work requirements. (45) The client is shown the hearing test results on a graph and the results are compared to normal hearing. (1) |
| Client-centered traits and actions | Traits and actions of a clinician who would likely foster client-centered approach to interaction | The client feels the clinician cares about him or her. (98) The client feels that all his or her questions have been answered. (93) The client’s rapport with the clinician. (91) The client and clinician communicate easily. (85) |
| Acknowledging client as an individual | Recognizing each client’s individuality in hearing aid adoption | The client feels his or her concerns have been heard and validated. (116) The clinician values what is important to the client. (88) The clinician provides an opportunity for the client to express his or her concerns. (122) The clinician is able to explain things to the client at appropriate level. (101) |
| Imposing undue pressure and discomfort | Factors negatively influencing hearing aid adoption such as pressure | The client feels rushed and as if on an assembly line. (51) The client feels some pressure to purchase. (53) The client has the impression audiologist is “up-selling.” (57) The client is given too many choices. (121) |
| Conveying device information by clinician | Emphasis on information transfer from the clinician to the client | The clinician explains why a particular hearing aid is recommended. (60) The client can hear what a hearing aid sounds like. (100) The clinician explains why a hearing aid needs to be adjusted by the clinician. (34) The clinician explains that background noise may be a problem. (35) |
| Supporting choices and shared decision making | Supporting client’s choices regarding hearing aid and empowering the client with shared decision making | The client feels that he or she is a part of the process. (94) The client has control over the hearing aid settings. (23) The client has freedom to make some of the decisions with respect to the hearing aid. (95) The client is given time to think about the hearing aid purchase. (50) |
| Factors in client readiness | Internal and external factors that influence client’s attitude and readiness in pursuing hearing aids | The client accepts there is a need for hearing aids. (106) The clinician has been involved in another family member’s care. (78) The client is referred by a friend. (103) The client’s experience with friends or family who have hearing aids. (75) |
The statements and concepts were reviewed by the research team to identify overarching themes in the map. Two overarching themes were identified that correspond with specific areas in the concept map. To illustrate the overarching themes the research team divided the map into two areas by drawing a diagonal line across the map (Figure 1). The area on the right of the diagonal line associates with an overarching theme of client-centered interaction and on the left with client empowerment. The clusters on the right of the diagonal line have higher average importance ratings than the clusters on the left. The average importance rating for clusters in the client-centered interaction theme was 3.93 compared to 3.56 for the client empowerment theme.
A stress index of 0.26 was computed for the sorting task, which indicates a very good fit of the concept map to the similarity matrix (Trochim, 1993). The split-half correlation for the sorting task was 0.606. The Spearman–Brown correction was applied to the split-half correlation and resulted in a reliability estimate of 0.97 suggesting high consistency between the two groups in how they sorted the data (Trochim, 1993).
Discussion
This study explored factors in client–clinician interactions that are reported by clients and clinicians to influence hearing aid purchase decisions in persons who have received their first hearing aid recommendation. The findings revealed eight key constructs in the client–clinician interaction. Two major themes were identified from the client–clinician interaction model: client-centered interaction and client empowerment. Although elements of client-centered interaction are evident in all concepts in the map, the content of the four clusters located left to the line correspond more closely to the theme of client empowerment theme.
The cluster supporting choices and shared decision making has a central location on the map. The statements in this cluster have been frequently sorted with statements in other clusters. The central location of this cluster suggests a conceptual centrality, meaning that this concept correlates with both identified themes. Shared decision making has been identified as a key element in client empowerment and client centeredness (Mead & Bower, 2000).
Some of the factors influencing a person’s decision to purchase hearing aids that were indentified in this study have been previously reported in the hearing aid uptake literature. Statements in the ensuring client comfort cluster such as “the client has trust in the facility that the clinician works in” (Item 79) agree with findings in previous studies that suggest that clients’ opinions about hearing aid clinics influence rehabilitation decisions (Laplante-Lévesque, Hickson, & Worrall, 2010a). The providers’ expertise (Milhinch & Doyle, 1990), hearing aid dealer practices (Franks & Beckmann, 1985), and imperfections in the hearing aid delivery system (Garstecki, 1996) have also been shown to influence hearing aid uptake. In the current study the clusters, ensuring client comfort and imposing undue pressure and discomfort show similar findings, for example “the client’s perception of the clinician’s expertise” (Item 97), “the client feels that the clinician is sincere in his or her intentions” (Item 96), and “the client has the impression audiologist is ‘up-selling’” (Item 57). Deceptive practices of the hearing aid dealer and use of high pressure tactics have been shown to contribute to the rejection of hearing aids (Franks & Beckmann, 1985). This is in line with the concept imposing undo pressure and discomfort. The statements in this cluster also suggest that pressuring a client, who is in the process of hearing aid adoption, to purchase a device that is not affordable or is beyond the client’s need may negatively influence the person’s hearing aid purchase decision.
The ensuring client comfort concept has expanded previous findings by introducing the issue of client comfort in the actual interaction with items such as “the client is comfortable asking clinician questions” (Item 81), “the client feels comfortable calling clinician with questions” (Item 20), and “the client feels comfortable answering clinician’s questions” (Item 82).
The concept, factors in client readiness, converges with findings of several studies that investigated the influence of a person’s attitude and acceptance of hearing loss on hearing aid uptake. van den Brink et al. (1996) found that a person’s attitude influences hearing aid uptake. Garstecki and Erler (1998) and Humes, Wilson, and Humes (2003) showed a positive relationship between acceptance of hearing loss and hearing aid uptake. The results of this study also support those of Laplante-Lévesque et al. (2010a) that suggest other people’s experiences can influence rehabilitation decisions. In the current study, previous experiences of the individual, a friend, or family member were reported to influence the hearing aid purchase decision.
Conveying device information by clinician is a concept that is introduced to hearing health care literature for the first time by this study. This concept highlights the perceived need for the clinician to provide comprehensive information to the client during the hearing aid adoption process. This includes information regarding hearing aid selection and fitting including hearing aid styles, brands, features, as well as how a specific device would be selected for the individual client. It also includes financial information such as cost, warranty, and return policy. These results underscore previous findings that physicians often underestimate the amount of information their patients want (Guadagnoli & Ward, 1998). Due to the extent of the information pertaining to selection of an appropriate hearing device, even if all the information is presented to the client, many people cannot recall all the information, especially if the information is offered only once. This has been documented in diabetes care and education where patients found the information, which was often presented on only one occasion, overwhelming (Wikblad, 1991). Diabetic patients preferred information given at the beginning of the process to be at a minimum but acceptable level and that information be given continually throughout the process (Wikblad, 1991). The conveying device information concept also underscores the issue of shared decision making. The client’s preference for more information and the desire for a more active role in the decision-making process have been linked together in the health care literature (Cassileth, Zupkis, Sutton-Smith, & March, 1980; Sutherland, Llewellyn-Thomas, Lockwood, Tritchler, & Till, 1989). In a model of shared intervention decision making developed by Laplante-Lévesque, Hickson, and Worrall (2010b), “Being Informed,” which is described as receiving information about intervention options and obtaining unbiased recommendations, is one of the steps in the decision-making process. The proximity of the conveying device information concept and supporting choices and shared decision-making cluster on the concept map indicates that the content of these two clusters have often been placed together by participants and are conceptually close. The cluster, supporting choices and shared decision making implies that clients are not just recipients of professional decisions and recommendations but they are also part of the decision-making process. This necessitates a client-centered interaction in which the client is given sufficient information to empower him or her to make choices. Client-centered care has also been suggested as the preferred approach in client–clinician encounters when rehabilitation decisions are made (Laplante-Lévesque et al., 2010a).
Client-Centered Interaction
The concept map of the client–clinician interaction shares similar components with the client-centered care or patient-centered care approach described in the literature. In this article the term client-centered care is used for both client-centered and patient-centered care. Law and Mills (1998) found several common components in six client-centered frameworks. Provision of information; physical comfort; person-centered communication; facilitation of client participation; flexible, individualized service delivery, which were common to all six models were also identified in the concept map of the client–clinician interaction in the current study. To interpret the findings of this study, two client-centered models, one described by Stewart (2003) and the other by Law, Baptiste, and Mills (1995), are used. The elements of Stewart’s (2003) client-centered care that are similar to the findings in this study are exploring both disease and illness experience, understanding the whole person, finding common ground, and enhancing the client–clinician relationship. In addition, the findings share concepts of client involvement in decision making and partnership within the client-centered care model as described by Law et al. (1995).
Client-centered care is a holistic approach to care in which the objective and subjective aspects of ill health are combined (Stewart, 2003). The health care professional conceptualizes both the disease and the illness. According to Law, Polatajko, Baptiste, and Townsend (1997), client-centered care is an enabling process that focuses on the client. The health care professional is a facilitator who enables the client to generate and implement solutions to their problems. Two clusters, understanding and meeting client needs and acknowledging client as an individual underline the perceived importance of a holistic approach to the assessment process, enabling the client to evaluate and become aware of their communication difficulties. In a client-centered approach to care, disease is an objective problem of the structure or function of the body organs and systems, while illness is the subjective experience of the patient of their problem (Stewart, 2003). Examples of statements that correspond with using a holistic approach to care are “the clinician asks what situations are difficult for the client” (Item 37), “the clinician relates the assessment results to difficulties the client is having” (Item 33), and “the clinician considers the client’s lifestyle and/or work requirements” (Item 45). Items such as “the clinician helps the client to explore his or her communication importance” and “the clinician helps the client to be more aware and assess his or her problems” support the role of the clinician as a facilitator who enables the client to identify his or her specific communication difficulties.
Another component of client-centered care is determining common ground between the client and the health care professional (Stewart, 1995). Finding common ground can be achieved by defining the problem, setting goals for treatment and/or management, and defining the role of the health care professional and the client within the interaction (Stewart, 2003). Examples of statements that correspond to finding common ground are “the clinician provides enough information about hearing loss” (Item 2) and “the clinician explains the reason why the client needs hearing aids” (Item 31). In client-centered care agreement on what is wrong helps the treatment/management plan to be more acceptable (Stewart, 2003). “Providing an opportunity for the client to express his or her concerns” (Item 122), and “explaining things to the client at appropriate level” (Item 101) can help to define the problem and set goals for rehabilitation. Hearing aid adoption is influenced by perceived activity limitation and/or participation restriction due to hearing difficulties (Duijvestijn et al., 2003; Swan & Gatehouse, 1990; van den Brink et al., 1996). Hearing impaired individuals who are less aware of or overlook their communication problems are less likely to adopt hearing aids (Helvik, Wennberg, Jacobsen, & Hallberg, 2008; Humes et al., 2003). Thus “helping the client to explore his or her communication importance and to be more aware and assess his or her problems” (Items 41 & 42) may facilitate the hearing aid adoption, while focusing on the hearing loss and the audiogram as in the biomedical model may not necessarily result in the acceptance of the hearing loss and understanding its link to the client’s communication difficulties.
The client–clinician relationship is the foundation of client-centered care; however clients frequently report that audiologists do not seem to understand their difficulties (Glass & Elliot, 1992). The client-centered traits and actions and ensuring client comfort clusters relate to the client–clinician relationship component of the client-centered care. These concepts reveal the importance of the client–clinician relationship. For example, “the client should feel all his or her questions have been answered” (Item 93), “the clinician can be reached easily by phone” (Item 19), and “the client should feel the clinician has patience with the client during the whole process” (Item 113).
In client-centered care, the power and control between the health care professional and the client are shared. This partnership is unique to each client, as they exercise different degrees of control in different dimensions (Stewart, 2003). The Supporting choices and shared decision making cluster supports the client’s partnership in the hearing aid adoption process, for example, “the client feels he or she is allowed to make choices” (Item 83) and “the client feels that he or she is a part of the process” (Item 94).
Client Empowerment
Empowerment is a complex experience of personal change, which can be facilitated by adopting a client-centered approach to care (Aujoulat, d’Hoore, & Deccache, 2007). There are interpersonal and intrapersonal dimensions to the client empowerment process. In the interpersonal dimension, empowerment is an interactive process, which is seen from the point of view of the client–clinician interaction. In an interactive view, empowerment is the process of communication and education where the knowledge and power are shared (Aujoulat et al., 2007), while in an intrapersonal view empowerment is a personal process in which the power is created within the person (Aujoulat et al., 2007). The three clusters conveying device information by clinician, supporting choices and shared decision making, and imposing undo pressure and discomfort align with the interpersonal dimension of client empowerment. The factors in client readinesscluster supports the intrapersonal view of empowerment. From an interpersonal view to empowerment it is the clinician’s responsibility to empower the client by conveying device information, supporting the client’s choices, not pressuring the client to purchase hearing aids or a specific hearing aid, and allowing the client to be involved in decision making. In an intrapersonal dimension, the client should be ready to pursue hearing aids. The factors in client readinesscluster supports the intrapersonal view to empowerment with statements such as “the client accepts there is a need for hearing aids” (Item 106) and “the client has a positive attitude” (Item 48). The four concepts that describe client empowerment, view empowerment as a combination of both an interactive and a personal process as described by McWilliam et al. (1997) in which the power is not simply given by the clinician, nor is it solely created within the client, but empowerment is facilitated by the client–clinician relationship.
Implementing the Themes Into Practice
The overall themes in the concept map of the client–clinician interaction emphasize the empowerment of the clients within the interaction. Although client-centered interaction and client empowerment necessitate partnership and client involvement in the process, most of the generated statements in this study were unidirectional; that is, the statements were directed toward the clinicians. This was in spite of the equal power and opportunity given to both clients and clinicians during the data collection. This finding highlights the historical dominance of the biomedical model in audiology. Participants’ views on the role of clients and clinicians reflected the clinician as the expert and the client as the passive recipient of information and recommendations. Shifting the paradigm of care from a biomedical to client-centered care model is not easy. Many factors contribute to the difficulty implementing client-centered care, one of which is changing the way both clients and clinicians traditionally interact with one another (Ponte et al., 2003).
From the clients’ position, their unfamiliarity with hearing health care and the novelty of the context may account for some of the unidirectional statements generated in this study. Participants in the client group were all individuals who had their first hearing aid recommendation 3 months prior to the study and had limited knowledge of what the hearing aid adoption process entailed. Participation is a developmental process and taking an active role is improved by information, development of personal expertise, and the relationship with health care professional (Say, Murtagh, & Thomson, 2006). This finding emphasizes the importance of knowledge translation including educating consumers on hearing loss and hearing aid–related issues. Prospective hearing aid candidates may also benefit from educational material and group aural rehabilitation participation prior to hearing aid acquisition (Garstecki, 1990; Saunders, Lewis, & Forsline, 2009). Findings of this study offer preliminary guidelines for dispensing clinicians. It is important for clinicians to consider the novelty of the encounter for clients who are seeing a hearing health care professional for the first time. To establish client-centered interaction, both the clinicians and the clients need to be mindful of their role in the process and understand the partnership (Shaw, McWilliam, Sumsion, & MacKinnon, 2007). Clinicians can facilitate the involvement of the clients by creating a comfortable space and place for clients, communicating necessary information, and being aware of the amount of information that each individual can retain in one session. Provision of information, as expressed by participants in this study, is a common element in many client-centered frameworks (Law & Mills, 1998). The novelty of the interaction and an overwhelming amount of information and the manner in which it is conveyed may become a barrier to the active participation of clients in the hearing aid adoption process.
Another explanation for the unidirectionality of the statements may be a result of the client’s experience in previous interactions. An individual’s previous experience with health care professionals may influence a client’s desire or expectation about their level of involvement in the decision-making process (Adams, Smith, & Ruffin, 2001). An active role in the interaction with their health care provider may not be a meaningful option for clients who have no knowledge or expectation of anything other than a passive role (Kenny, Quine, Shiell, & Cameron, 1999). In contrast, clients will be more likely to take a more active role if they feel their clinician is willing to involve them in the decision-making process (Adams et al., 2001).
Both clients and clinicians directed the statements toward clinicians. Our results indicate that clinicians recognize the importance of client-centered practice and client empowerment; however, they saw themselves as the key actor in the process. Studies in chronic illness have found discrepancies between health care professionals’ explicit intentions and their behavior (Freeman & Loewe, 2000; Paterson, 2001). The unidirectionality of the statements disregards one of the most important steps in the client-centered care, which is client–clinician partnership (Sumsion, 1999).
A client-centered approach improves client’s adherence and health outcomes (Robinson, Callister, Berry, & Dearing, 2008). Although a causal relationship between the factors identified in this study and hearing aid adoption has not been established, these factors may be used as a guideline to inform a client-centered approach to improve clients’ adherence to hearing aid recommendations. Further research can investigate if a casual relationship exists between the identified factors and hearing aid purchase decisions. Concept mapping was a useful approach to engage multiple stake holders with different powers in the research. The participatory nature of this method allowed ideas from a diverse group to be collected into clusters and to create a concept map that describes the groups’ perception of the factors influencing the hearing aid purchase decision. Participants in this study were recruited from within 1 hr driving distance of the research site and the majority of the clinicians in the study were graduates from a single audiology program. It would be beneficial to investigate whether the same concepts emerge from a wider sample of clients and clinicians.
The findings highlight the importance of putting the client-centered care approach at the center of practice and entering into a dialogue on what client-centeredness means in audiology and how it can be enacted in actual practice. Understanding the elements of a client-centered interaction facilitates its implementation into practice. Based on the findings of this study, an outline of the key constructs of client-centered practice in audiology and their implications for practice and research is warranted.
This research has explored the client–clinician interaction in the initial visits of first time hearing aid candidates. Future research should explore how interactions change in the course of continuing clinical care and how they influence hearing aid use. A current study in progress at the National Centre for Audiology compares the clients’ and clinicians’ importance ratings of the factors identified in this study. The goal of the comparison is to investigate the differences between the two groups in how they rate the importance of the identified factors. Further work is also underway to compare the importance ratings with clients and clinicians in nationwide study.
Acknowledgments
The authors gratefully acknowledge the Ontario Research Fund, Unitron, the Ontario Neurotrauma Foundation, the Canada Foundation for Innovation, and Michael Huffman (Concept System Inc.) for their support.
Appendix
Appendix.
Eight Clusters and Statements in Each Cluster
| Understanding and meeting client needs |
|---|
| 37—The clinician asks what situations are difficult for the client. |
| 31—The clinician explains the reason why the client needs hearing aids. |
| 33—The clinician relates the assessment results to the difficulty they are having. |
| 39—The clinician explains the test or procedure that she or he is doing. |
| 32—The clinician explains what the audiogram means in terms of how a hearing aid will help. |
| 45—The clinician considers the client’s life style and/or work requirements. |
| 2—The clinician provides enough information about hearing loss. |
| 7—The clinician explains hearing test results thoroughly. |
| 118—The clinician can simplify the technical terms and technology by explaining in layman’s terms. |
| 1—The client is shown the hearing test results on a graph and the results are compared to normal hearing. |
| 38—The clinician sends a report to the client. |
| Acknowledging client as an individual |
| 27—There is consistency in information obtained from different clinicians. |
| 122—The clinician provides an opportunity for the client to express his or her concerns. |
| 88—The clinician values what is important to the client. |
| 116—The client feels his or her concerns have been heard and validated. |
| 29—The clinician explains throughout testing to build trust. |
| 87—The clinician is confident in conveying information. |
| 44—The clinician realizes everyone has different needs. |
| 101—The clinician is able to explain things to the client at appropriate level. |
| 43—The clinician realizes everyone is different. |
| 107—The clinician makes the transition very easy. |
| 114—The clinician assures a follow-up appointment. |
| 42—The clinician helps the client to explore his or her communication importance. |
| 41—The clinician helps the client to be more aware and assess his or her problems. |
| 110—The clinician is able to accommodate individuals with special needs. |
| 28—Information is posted about the profession, degrees, and credentials in layman’s terms. |
| 104—The clinician doesn’t overwhelm the client with too much technology at first. |
| Conveying device information by clinician |
| 60—The clinician explains why a particular hearing aid is recommended. |
| 5—The clinician provides enough information about hearing aids. |
| 47—The clinician relates the hearing aid technology to the client’s lifestyle or listening needs. |
| 21—The client is offered different styles and choices of hearing aids. |
| 46—The clinician explains different styles of hearing aids and earmolds and what they will do for the client. |
| 59—The clinician explains why a particular size or style of hearing aid may not be suitable. |
| 115—The clinician assures the client that the hearing aids can be returned. |
| 66—The clinician explains the pros and cons of each hearing aid. |
| 14—The clinician explains the client’s rights (such as the mandatory 30-day trial period). |
| 35—The clinician explains that background noise may be a problem. |
| 36—The clinician explains all the features of the hearing aid. |
| 3—The clinician shows pictures of hearing aids. |
| 68—The clinician explains how long the hearing aids are expected to last. |
| 17—The clinician provides an information sheet about the care of hearing aids. |
| 16—The clinician has knowledge of funding sources to access that the client is not aware of. |
| 11—The clinician provides a demonstration of sample hearing aids. |
| 117—The client experiences what a hearing aid feels like on his or her ear. |
| 67—The clinician discusses the hearing aid warranty. |
| 34—The clinician explains why a hearing aid needs to be adjusted by the clinician. |
| 15—A trial period longer than 30 days is available. |
| 100—The client can hear what a hearing aid sounds like. |
| 72—The clinician provides pamphlets with information for different hearing aids. |
| 6—The clinician provides information about other programs of care (e.g., aural rehabilitation programs). |
| 12—The client is given a web site so that he or she can do research at home. |
| Client-centered traits and actions |
| 40—The clinician is upfront and honest. |
| 4—The client feels the clinician is knowledgeable. |
| 89—The clinician’s level of expertise. |
| 18—The clinician is thorough. |
| 93—The client feels that all his or her questions have been answered. |
| 55—The clinician is pleasant. |
| 85—The client and clinician communicate easily. |
| 70—The clinician meets the client’s expectations for professionalism. |
| 73—The clinician does not appear hurried. |
| 108—The same clinician is seen from start to finish. |
| 90—The clinician shows empathy toward the client. |
| 91—The client’s rapport with the clinician. |
| 69—The clinician projects a professional appearance. |
| 98—The client feels the clinician cares about him or her. |
| 19—The clinician can be reached easily by phone. |
| 25—The clinician is down to earth. |
| 105—The clinician and client’s personalities are compatible. |
| Ensuring client comfort |
| 77—The client has trust in the clinician. |
| 71—The client has confidence in the clinician. |
| 97—The client’s perception of the clinician’s expertise. |
| 10—The client feels that the testing is thorough and accurate. |
| 76—How much the client believes what the clinician is saying. |
| 92—The client’s feeling of the clinician’s competence. |
| 61—The clinician provides sufficient time in the appointment to explain recommendations. |
| 96—The client feels that the clinician is sincere in his or her intentions. |
| 65—The client doesn’t feel pressured. |
| 113—The client feels the clinician has patience with the client during the whole process. |
| 81—The client is comfortable asking the clinician questions. |
| 56—Office staff is professional. |
| 62—The amount of time spent with the client. |
| 20—The client feels comfortable calling clinician on the phone with questions. |
| 79—The client has trust in the facility that the clinician works in. |
| 82—The client is comfortable answering the clinician’s questions. |
| 109—The client is taken on time for the appointment. |
| 84—The physical environment is comfortable and welcoming. |
| 26—The clinician sits and chats. |
| Supporting choices and shared decision making |
| 102—The recommendation is based on a medical decision and not on a sale. |
| 9—The client is given sufficient information to empower him or her to make choices. |
| 86—The clinician’s response to the client’s expressed financial constraints. |
| 95—The client has freedom to make some of the decisions with respect to the hearing aid. |
| 58—The clinician accepts client’s decision to purchase one versus two hearing aids. |
| 83—The client feels he or she is allowed to make choices. |
| 94—The client feels that he or she is a part of the process. |
| 50—The client is given time to think about the hearing aid purchase. |
| 8—The clinician provides information about outside funding agencies and potential eligibility. |
| 119—The clinician is willing to accommodate the client’s desire for a certain feature or model. |
| 13—The clinician provides three different price levels from which to choose. |
| 22—The client has the opportunity to get a second opinion. |
| 24—The client has the opportunity to try a different hearing aid. |
| 99—The client feels the decision is not final. |
| 23—The client has control over the hearing aid settings. |
| 120—The clinician prescribes a hearing aid from client’s preferred company. |
| 111—A family member is included in the appointment. |
| 63—The clinician provides information and options about other locations where the hearing aids can be purchased. |
| Factors in client readiness |
| 106—The client accepts there is a need for hearing aids. |
| 74—The client’s readiness to pursue hearing aids. |
| 48—The client has a positive attitude. |
| 75—The client’s experience with friends or family who have hearing aids. |
| 30—The client is referred by his or her physician. |
| 78—The clinician has been involved in another family member’s care. |
| 112—The client has had a bad experience with another clinician. |
| 103—The client is referred by a friend. |
| Imposing undue pressure and discomfort |
| 53—The client feels some pressure to purchase. |
| 54—The client has difficulty understanding the clinician during testing. |
| 51—The client feels rushed and as if on an assembly line. |
| 80—The client feels that the clinician is prescribing hearing aids that exceed the client’s needs. |
| 57—The client has the impression audiologist is “up-selling.” |
| 64—The client feels that the clinician is prescribing hearing aids beyond client’s price range. |
| 52—The client has concerns with the relationship between the clinic where test is done and where he or she is referred to purchase the hearing aid. |
| 49—The clinician pushes certain hearing aids. |
| 121—The client is given too many choices. |
Footnotes
Authors’ Note: Portions of this article were presented at the American Academy of Audiology Convention, April 8, 2011, Chicago, IL, and at the Sixth International Adult Aural Rehabilitation Conference, May 23, 2011, St. Pete Beach, FL.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Grants: Ontario Research Fund; Unitron; Canada Foundation for Innovation; Ontario Neurotrauma Foundation; Ontario Graduate Scholarships in Science and Technology.
References
- Abrams H., Chisolm T., Saunders G. (2005). Measuring hearing aid outcomes—Not as easy it seems. Journal of Rehabilitation Research and Development, 42, 157-168 [DOI] [PubMed] [Google Scholar]
- Adams R. J., Smith B. J., Ruffin R. E. (2001). Patient preferences for autonomy in decision making in asthma management. British Medical Journal, 56(2), 126-132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aujoulat I., d’Hoore W., Deccache A. (2007). Patient empowerment in theory and practice: Polysemy or cacophony? Patient Education and Counseling, 66(1), 13-20 [DOI] [PubMed] [Google Scholar]
- Bensing J. (1991). Doctor–patient communication and the quality of care. Social Science & Medicine, 32, 1301-1310 [DOI] [PubMed] [Google Scholar]
- Biggs S. (1997). Choosing not to be old? Masks, bodies and identity management in later life. Ageing and Society, 17, 553-570 [Google Scholar]
- Brooks D. N., Hallam R. S. (1998). Attitudes to hearing difficulty and hearing aids and the outcome of audiological rehabilitation. British Journal of Audiology, 32, 217-226 [DOI] [PubMed] [Google Scholar]
- Cassileth B. R., Zupkis R. V., Sutton-Smith K., March V. (1980). Information and participation preferences among cancer patients. Annals of Internal Medicine, 92, 832-836 [DOI] [PubMed] [Google Scholar]
- Chisolm T. H., Johnson C. E., Danhauer J. L., Portz L. J. P, Abrams H. B., Lesner S., . . . Newman C. W. (2007). A systematic review of health-related quality of life and hearing aids: Final report of the American academy of audiology task force on the health-related quality of life benefits of amplification in adults. Journal of the American Academy of Audiology, 18, 151-183 [DOI] [PubMed] [Google Scholar]
- Concept Systems Incorporated. (2011). The Concept System. (Version 4). Ithaca, NY: Concept Systems Incorporated; Retrieved from http://www.conceptsystems.com. [Google Scholar]
- Dasinger L. K., Krause N., Thompson P. J., Brand R. J., Rudolph L. (2001). Doctor proactive communication, return-to-work recommendation, and duration of disability after a workers’ compensation low back injury. Journal of Occupational and Environmental Medicine, 43, 515-525 [DOI] [PubMed] [Google Scholar]
- Davison M. L. (1983). Multidimensional scaling. New York, NY: Wiley [Google Scholar]
- Dibbelt S., Schaidhammer M., Fleischer C., Greitemann B. (2009). Patient-doctor interaction in rehabilitation: The relationship between perceived interaction quality and long-term treatment results. Patient Education and Counseling, 76, 328-335 [DOI] [PubMed] [Google Scholar]
- Duijvestijn J. A., Anteunis L. J., Hoek C. J., Van Den Brink R. H., Chenault M. N., Manni J. J. (2003). Help-seeking behaviour of hearing-impaired persons aged 55 years; effect of complaints, significant others and hearing aid image. Acta Oto-Laryngologica, 123, 846-850 [DOI] [PubMed] [Google Scholar]
- Elbeck M., Fecteau G. (1990). Improving the validity of measures of patient satisfaction with psychiatric care and treatment. Hospital and Community Psychiatry, 41, 998-1001 [DOI] [PubMed] [Google Scholar]
- Erler S. F., Garstecki D. C. (2002). Hearing loss-and hearing aid-related stigma: Perceptions of women with age-normal hearing. American Journal of Audiology, 11(2), 83-91 [DOI] [PubMed] [Google Scholar]
- Franks J. R., Beckmann N. J. (1985). Rejection of hearing aids: Attitudes of a geriatric sample. Ear and Hearing, 6, 161-166 [DOI] [PubMed] [Google Scholar]
- Freeman J., Loewe R. (2000). Barriers to communication about diabetes mellitus. Journal of Family Practice, 49, 507-512 [PubMed] [Google Scholar]
- Garstecki D. C. (1990). Hearing health knowledge in aging adults. Journal of the Academy of Rehabilitative Audiology, 23, 79-88 [Google Scholar]
- Garstecki D. C. (1996). Older adults: Hearing handicap and hearing aid management. American Journal of Audiology, 5(3), 25-34 [Google Scholar]
- Garstecki D. C., Erler S. F. (1998). Hearing loss, control, and demographic factors influencing hearing aid use among older adults. Journal of Speech, Language, and Hearing Research: JSLHR, 41, 527-537 [DOI] [PubMed] [Google Scholar]
- Groenwoud A., van Exel N., Berg M., Huijsman R. (2008). Building quality report cards for geriatric care in the Netherlands: Using concept mapping to identify the appropriate “Building Blocks” from the consumer’s perspective, The Gerontologist, 48(1), 79-92 [DOI] [PubMed] [Google Scholar]
- Glass L., Elliot H. (1992). The professionals told me what it was, but that’s not enough. SHHH Journal, 13, 26-28 [Google Scholar]
- Griffin S. J., Kinmonth A. L., Veltman M. W. M., Gillard S., Grant J., Stewart M. (2004). Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: A systematic review of trials. Annals of Family Medicine, 2, 595-608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guadagnoli E., Ward P. (1998). Patient participation in decision-making. Social Science & Medicine, 47, 329-339 [DOI] [PubMed] [Google Scholar]
- Helvik A. S., Wennberg S., Jacobsen G., Hallberg L. R. M. (2008). Why do some individuals with objectively verified hearing loss reject hearing aids? Audiological Medicine, 6, 141-148 [Google Scholar]
- Humes L. E., Wilson D. L., Humes A. C. (2003). Examination of differences between successful and unsuccessful elderly hearing aid candidates matched for age, hearing loss and gender: Evaluación de las diferencias entre los candidatos exitosos y no exitosos de edad mayor, al uso de auxiliar auditivo por edad, grado de hipoacusia y sexo. International Journal of Audiology, 42, 432-441 [DOI] [PubMed] [Google Scholar]
- Humphrey C., Herbst K. G., Faurqi S. (1981). Some characteristics of the hearing-impaired elderly who do not present themselves for rehabilitation. British Journal of Audiology, 15(1), 25-30 [DOI] [PubMed] [Google Scholar]
- Kane M., Trochim W. M. (2007). Concept mapping for planning and evaluation. Thousand Oaks, CA: SAGE [Google Scholar]
- Kaplan S. H., Greenfield S., Ware J. E., Jr. (1989). Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Medical Care, 27(Suppl. 3), S110-S127 [DOI] [PubMed] [Google Scholar]
- Kenny P., Quine S., Shiell A., Cameron S. (1999). Participation in treatment decision making by women with early stage breast cancer. Health Expectations, 2, 159-168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochkin S. (2005). MarkeTrak VII: Hearing loss population tops 31 million people. Hearing Review, 12(7), 16-29 [Google Scholar]
- Kochkin S. (2009). MarkeTrak VIII: 25-year trends in the hearing health market. Hearing Review, 16(10), 12-31 [Google Scholar]
- Kochkin S., Beck D. L., Christensen L. A., Compton-Conley C., Fligor B. J., Kricos P. B., . . . Turner R. G. (2010). MarkeTrak VIII: The impact of the hearing healthcare professional on hearing aid user success. Hearing Review, 17(4), 12-34 [Google Scholar]
- Laplante-Lévesque A., Hickson L., Worrall L. (2010a). Factors influencing rehabilitation decisions of adults with acquired hearing impairment. International Journal of Audiology, 49, 497-507 [DOI] [PubMed] [Google Scholar]
- Laplante-Lévesque A., Hickson L., Worrall L. (2010b). A qualitative study of shared decision making in rehabilitative audiology. Journal of the Academy of Rehabilitative Audiology, XLIII, 27-43 [Google Scholar]
- Law M., Baptiste S., Mills J. (1995). Client-centered practice: What does it mean and does it make a difference? Canadian Journal of Occupational Therapy, 62, 250-257 [DOI] [PubMed] [Google Scholar]
- Law M., Mills J. (1998). Client-centered occupational therapy. In Law M. (Ed.), Client-centered occupational therapy (pp. 1-18). Thorofare, NJ: Slack [Google Scholar]
- Law M., Polatajko H., Baptiste S., Townsend E. (1997). Core concepts of occupational therapy. In Canadian Association of Occupational Therapists (Eds.). Enabling occupation: An occupational therapy perspective (pp. 29-56). Ottawa, Ontario, Canada: CAOT [Google Scholar]
- Lee K., Lotz P. (1998). Noise and silence in the hearing instrument industry (CISTEMA Working Paper, No. 98-1). Copenhagen, Denmark: Copenhagen Business School [Google Scholar]
- Magnusson D. (1976). The person and the situation in an interactional model of behavior. Scandinavian Journal of Psychology, 17, 253-271 [Google Scholar]
- McWilliam C. L., Stewart M., Brown J. B., McNair S., Desai K., Patterson M. L., . . . Pittman B. J. (1997). Creating empowering meaning: An interactive process of promoting health with chronically ill older Canadians. Health Promotion International, 12(2), 111-123 [Google Scholar]
- Mead N., Bower P. (2000). Patient-centeredness: A conceptual framework and review of the empirical literature. Social Science & Medicine, 51, 1087-1110 [DOI] [PubMed] [Google Scholar]
- Milhinch J.C., Doyle J. (1990). Client’s decision-making choosing a hearing healthcare service. Australian Journal of Audiology, 12, 45-53 [Google Scholar]
- National Institute on Deafness and other Communication Disorders. (2008). Statistics about hearing, balance, ear infections, and deafness. Retrieved from http://www.nidcd.nih.gov/funding/programs/09HHC/Pages/summary.aspx
- Paterson B. (2001). Myth of empowerment in chronic illness. Journal of Advanced Nursing, 34, 574-581 [DOI] [PubMed] [Google Scholar]
- Ponte P. R., Conlin G., Conway J. B., Grant S., Medeiros C., Nies J., . . . Conley K. (2003). Making patient-centered care come alive: Achieving full integration of the patient’s perspective. Journal of Nursing Administration, 33(2), 82-90 [DOI] [PubMed] [Google Scholar]
- Robinson J. H., Callister L. C., Berry J. A., Dearing K. A. (2008). Patient-centered care and adherence: Definitions and applications to improve outcomes. Journal of the American Academy of Nurse Practitioners, 20, 600-607 [DOI] [PubMed] [Google Scholar]
- Saunders G. H., Lewis M. S., Forsline A. (2009). Expectations, prefitting counseling, and hearing aid outcome. Journal of the American Academy of Audiology, 20, 320-334 [DOI] [PubMed] [Google Scholar]
- Say R., Murtagh M., Thomson R. (2006). Patients’ preference for involvement in medical decision making: A narrative review. Patient Education and Counseling, 60(2), 102-114 [DOI] [PubMed] [Google Scholar]
- Shaw L., McWilliam C., Sumsion T., MacKinnon J. (2007). Optimizing environments for consumer participation and self-direction in finding employment. OTJR Occupation Participation and Health, 27(2), 59-70 [Google Scholar]
- Silverman J., Kurtz S. M., Draper J., Kurtz S. M. (1998). Skills for communicating with patients. Abingdon, UK: Radcliffe Medical Press [Google Scholar]
- Stewart M. (1995). Effective physician-patient communication and health outcomes: A review. Canadian Medical Association Journal, 152, 1423-1433 [PMC free article] [PubMed] [Google Scholar]
- Stewart M. (2003). Patient-centered medicine: Transforming the clinical method (2nd ed.). Abingdon, UK: Radcliffe Medical Press [Google Scholar]
- Stewart M., Brown J. B., Boon H., Galajda J., Meredith L., Sangster M. (1999). Evidence on patient-doctor communication. Cancer Prevention & Control, 3(1), 25-30 [PubMed] [Google Scholar]
- Sumsion T. (Ed.). (1999). Client-centered practice in occupational therapy: A guide to implementation. Edinburgh, UK: Churchill Livingston [Google Scholar]
- Sutherland H. J., Llewellyn-Thomas H., Lockwood G., Tritchler D., Till J. (1989). Cancer patients: Their desire for information and participation in treatment decisions. Journal of the Royal Society of Medicine, 82, 260-263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan I. R., Gatehouse S. (1990). Factors influencing consultation for management of hearing disability. British Journal of Audiology, 24, 155-160 [DOI] [PubMed] [Google Scholar]
- Trochim W. (1989). An introduction to concept mapping for planning and evaluation. Evaluation and Program Planning, 12(1), 1-16 [Google Scholar]
- Trochim W. (1993, November 6). Reliability of concept mapping. Paper presented at the annual meeting of the American Evaluation Association, Dallas, TX [Google Scholar]
- Trochim W., Kane M. (2005). Concept mapping: An introduction to structured conceptualization in health care. International Journal for Quality in Health Care, 17, 187-191 [DOI] [PubMed] [Google Scholar]
- van den Brink R. H., Wit H. P., Kempen G. I., van Heuvelen M. J. (1996). Attitude and help-seeking for hearing impairment. British Journal of Audiology, 30, 313-324 [DOI] [PubMed] [Google Scholar]
- van der Waal M. A. E, Casparie A. F., Lako C. J. (1996). Quality of care: A comparison of preferences between medical specialists and patients with chronic diseases. Social science & medicine, 42, 643-649 [DOI] [PubMed] [Google Scholar]
- Vestergaard Knudsen L., Öberg M., Nielsen C., Naylor G., Kramer S. E. (2010). Factors influencing help seeking, hearing aid uptake, hearing aid use and satisfaction with hearing aids: A review of the literature. Trends in Amplification, 14, 127-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler F. C., Anderson L. A., Boddie-Willis C., Price P. H., Kane M. (2005). The role of state public health agencies in addressing less prevalent chronic conditions. Preventing Chronic Disease, 2(3), A12. [PMC free article] [PubMed] [Google Scholar]
- Wikblad K. F. (1991). Patient perspectives of diabetes care and education. Journal of Advanced Nursing, 16, 837-844 [DOI] [PubMed] [Google Scholar]
- Wong L. L. N., Hickson L., McPherson B. (2003). Hearing aid satisfaction: What does research from the past 20 years say? Trends in Amplification, 7, 117-161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2006). Deafness and hearing impairment. Retrieved from http://www.who.int/features/factfiles/deafness/08_en.html