Abstract
A self-fitting hearing aid, designed to be assembled and programmed without audiological or computer support, could bring amplification to millions of people in developing countries, who remain unaided due to the lack of a local, professional, audiological infrastructure. The ability to assemble and insert a hearing aid is fundamental to the successful use of a self-fitting device. In this study, the management of such tasks was investigated. Eighty older, urban-dwelling, hearing-impaired adults in a developed country were asked to follow a set of written, illustrated instructions to assemble two slim-fit behind-the-ear hearing aids. Participants were allowed to access assistance with the task from an accompanying partner. A range of personal and audiometric variables was measured through the use of structured questionnaires and standardized tests of health literacy, cognitive function, and manual dexterity. The results showed that 99% of participants were able to complete the hearing aid assembly task, either on their own or with assistance. Health literacy, or the ability to read and understand health-related text, and gender most strongly influenced participants’ ability to complete the assembly task independently and accurately. Higher levels of health literacy were associated with an increased likelihood of independent and successful task completion. Male participants were more likely to complete the task on their own, while female participants were more likely to assemble the device without errors. The results of this study will inform future work regarding development of educational material for the self-fitting hearing aid as well as candidacy for such a device.
Keywords: hearing aids, hearing aid management, self-fitting, amplification, health literacy, cognition
Introduction
Hearing aid management refers to the physical activities users must perform to successfully handle, wear, and maintain their amplification devices. These activities include, but are not limited to, inserting the earmold or hearing aid shell into the ear canal, locating and operating the onboard control(s), removing the device from the ear, changing the battery, and cleaning accumulations of debris from the sound bore (Dillon, 2001; Ward, Gowers, & Morgan, 1979). To perform these activities, the successful hearing aid user requires a sufficient degree of tactile sensitivity, manual dexterity, cognitive function, and visual acuity (Erber, 2003).
The influence of tactile sensitivity and manual dexterity on hearing aid management skills is well - established in the audiology literature. In a study of the effect of different hearing aid and earmold styles on physical handling ability in the elderly, Stephens and Meredith (1991) compared the participants’ scores on a standardized measure of tactile sensitivity to the time they took to successfully insert an earmold into their ear and place the hearing aid body behind the pinna. They found that those participants who had less tactile sensitivity took significantly longer to accomplish the insertion task. The time taken to correctly insert the battery into the hearing aid was considered by these researchers to be a test of “manipulative skills,” and this result was found to correlate significantly with the time participants took to successfully insert an in-the-ear (ITE) hearing aid. In addition, participants who were unable to insert their own hearing aids in a single attempt were found to have significantly poorer tactile sensitivity than those participants who completed this activity on the first try. Similarly, Kumar, Hickey, and Shaw (2000) investigated the relationship between manual dexterity, as measured by the Purdue Pegboard Test (Tiffin & Asher, 1948), and self-reported hearing aid satisfaction among elderly hearing aid users. A significant positive correlation between these two variables was reported, with good manual dexterity linked to higher levels of hearing aid satisfaction. In a study of factors that influence an individual’s decision to return a hearing aid to the audiologist, Jacobson, Newman, Sandridge, and McCaslin (2002) found that rejection of amplification was significantly associated with manual dexterity problems. Those clients who returned their hearing aids to the audiologist shortly after the fitting demonstrated greater problems with manual dexterity than did those who retained their devices.
Anecdotal reports from clinical audiologists suggest that good management skills are fundamental to regular and successful hearing aid use, an assertion that is amply supported by the literature. In a telephone survey of primarily older (> 60 years of age) adults who had been fitted with their first set of hearing aids 3 months prior, Hickson, Hamilton, and Orange (1986) found a significant correlation between hours of daily aid use and physical handling ability, with poor management skills associated with few to no hours of daily use. Similarly, Brooks (1985) reported that the most commonly cited reason for nonuse of hearing aids, which was mentioned by more than 25% of the study participants, was the inability to correctly insert the earmold. Poor management skills were shown by Kapteyn (1977) and Sorri, Luotonen, and Laitakari (1984) to lead to user reports of dissatisfaction with hearing aid performance. Interestingly, participants in the Sorri et al. (1984) study reported equal levels of satisfaction with the amount and quality of instruction they received from the audiologist at their fitting appointment, regardless of whether they were successful hearing aid users or had discontinued aid use due to handling difficulties.
Several studies have investigated the effect of hearing aid style on management ability. Stephens and Meredith (1991) found that hearing aid users over the age of 75 years who had already been identified as experiencing management difficulties were significantly better able to manage behind-the-ear (BTE) hearing aids when the helix lock was removed from their skeleton earmolds. A follow-up study revealed that a BTE with this kind of modified earmold was also significantly easier for participants to handle than was an ITE, even though the participants who were randomly assigned the ITE style performed significantly better on a test of dexterity that required them to assemble a combination of nuts, bolts, and spacers (Meredith & Stephens, 1993).
Although a few studies have found no direct relationship between age and/or gender and successful hearing aid use (e.g., Hickson et al., 1986; Mulrow, Tuley, & Aguilar, 1992), many studies have shown that management difficulties are significantly more likely to be experienced by female hearing aid users and those over 75 years of age. For example, Ward et al. (1979) directed a group of first-time hearing aid users to perform such management activities as operating the volume control and changing the battery. Difficulties were demonstrated by varying numbers of participants for all seven tasks studied, primarily using the volume control wheel, inserting the earmold, and changing the battery, and these were significantly more common among the older female participants. Similar findings have been reported by Brooks (1985), Upfold, May, and Battaglia (1990), Stephens and Meredith (1991), and Meredith and Stephens (1993).
The extent to which hearing aid management may improve or decline over time is not clear. Upfold et al. (1990) observed the manipulation skills of a group of elderly hearing aid users immediately after their initial fitting and again after a period of several weeks. They found that even for those study participants who were successful in carrying out management tasks at the initial appointment, these skills tended to decline over the following weeks. Conversely, Henrichsen, Noring, Lindemann, Christensen, and Parving (1991) found that there was no significant difference in the proportion of handling difficulties experienced at 6 months postfitting relative to those encountered 4 years postfitting. However, few participants in the Henrichsen et al. study demonstrated any handling difficulties at all. One reason for their findings may be due to the fact that nonusers were not included in Henrichsen et al.’s retrospective study and that by 6 months postfitting, individuals with significant management difficulties may have already ceased wearing their hearing aids.
The majority of hearing aid management studies were conducted in the 1980s and 1990s, and thus predate the widespread use of personal computers and cellular telephones. While it may be argued that conversance with such technology is likely to lead to improved hearing aid management, this does not seem to be the case. Anecdotal evidence from clinical audiologists suggests that the nature of clients’ complaints and difficulties have not changed substantially over the last decade and that the introduction of new hearing aid technologies brings with it a host of associated management difficulties. The miniaturization of hearing aids, while appealing from a cosmetic point of view, can present problems due to smaller batteries and ever-shrinking (while at the same time more sophisticated) controls. Similarly, a report in Griffing (2009) states that many older adults experience problems with insertion and retention of the dome or ear tip on receiver-in-canal (RIC) devices, which is expected given their smaller size relative to a standard BTE and earmold combination.
While there are no currently available studies that directly examine the effects of visual acuity and/or cognitive function on hearing aid management skills, it is generally accepted that impaired cognitive function, particularly that associated with aging, influences the ability of the hearing aid user to appropriately adjust onboard controls (Kricos, 2006) and to understand and/or remember instructions for using and caring for a hearing aid (Erber, 2003). Similarly, many hearing aid users with poor functional vision reportedly experience difficulties in managing their devices (Erber, 2003).
To address these issues and their effect on hearing aid management, it has been suggested that audiologists employ specific techniques, such as simple diagrams and clear language, when instructing clients in the use of new devices (Erber, 2003; Maurer & Schow, 1996). These techniques are drawn from the field of health literacy, an area that researchers in audiology are increasingly beginning to explore. Health literacy refers to the “degree to which individuals have the capacity to obtain, process, and understand the basic health information . . . needed to make appropriate health decisions” (Ratzan & Parker, 2000, p. 32) and is considered an important contributor to positive health outcomes. A correlation between low levels of health literacy and poor compliance with health or medical treatment has been demonstrated in a number of studies (e.g., Schillinger et al., 2002; Williams, Baker, Parker, & Nurss, 1998), and a range of strategies for improving compliance among less health-literate individuals has been developed. These strategies include creating printed health care materials that are written at a third- to sixth-grade reading level, numbering step-by-step instructions, and pairing text with images to reinforce the message (Doak, Doak, & Root, 1996; Osborne, 2005). Further information about the importance of health literacy considerations in an audiological context may be found in Caposecco, Hickson, and Meyer (2011).
The primary objective of this study was to investigate the management of the assembly task associated with a self-fitting hearing aid among urban-dwelling older adults with a hearing loss in a developed country. The rationale of the investigation was to identify and correct any procedural difficulties encountered by this population prior to the introduction of the self-fitting concept to a developing country. Specifically, this study aimed to determine the proportion of hearing-impaired individuals who are able to follow a set of illustrated, written instructions to successfully select and assemble an instant-fit tip, tube, and hearing aid body; insert a battery; and insert the device into the ear, with or without assistance from an attendant partner or friend. The relationship between successful completion of the task and a range of personal, demographic, and hearing variables was also investigated.
Method
Participants
Eighty participants, 28 female and 52 male, completed the study. Participants ranged in age from 45 to 90 years, with a median age of 73 years (SD = 11 years). Participants were selected for inclusion in the study if they were between 45 and 90 years of age and had a measurable hearing loss in at least one ear, which we defined as a four-frequency average (4FA; average of pure tone thresholds at 0.5, 1, 2, and 4 kHz) greater than 25 dB HL. On average, the group rated their unaided hearing as fair, with a mean of 14 years of amplification experience among the 62 participants who currently wear or have previously worn hearing aids.
Forty participants were recruited from the National Acoustic Laboratories’ (NAL) participant database. As the NAL database is primarily made up of older individuals with previous amplification experience (individuals on the database have a median age of 73 years and 70% of them currently wear hearing aids), recruitment of the remaining participants focused on individuals between the ages of 45 and 60 and people without prior hearing aid experience. Participants on the younger side of our age range were desirable to ensure a reasonable distribution with respect to parameters that are associated with hearing aid management difficulties, such as manual dexterity. Additionally, individuals without prior hearing aid experience were targeted as we anticipate that initially it will be primarily new users who will access a self-fitting hearing aid. To that end, 40 participants were drawn from employees of local businesses and residents of local low-care retirement villages.
Participants were required to have a partner, friend, or relative available to attend the study appointment with them. The age of the partners ranged from 18 to 92 years, with a median age of 71 years (SD = 16 years). Nineteen partners were male and 61 were female. Forty-five participants lived in the same dwelling as their partner, while 34 did not.
The treatment of participants in this study was approved by the Australian Hearing Ethics Committee and conformed in all respects to the Australian government’s National Statement on Ethical Conduct in Human Research.
Procedure
All study tasks were completed in a single appointment. Prior to the appointment, a consent form and a questionnaire were mailed to each participant with a request to bring the completed documents to the study appointment. The questionnaire, which was designed specifically for this study, elicited information about the participant’s age, gender, level of formal education, current work status, occupation, socioeconomic status (SES), general literacy, health literacy, physical health, visual acuity, hearing status, and previous hearing aid experience (Appendix A in Convery, Keidser, & Hartley, 2011).
At the study appointment, the questionnaire was reviewed by the experimenter to ensure all items had been completed and there were no ambiguous responses. For those participants who were aided, information about the make, model, and style of the hearing aid(s) was recorded. A short questionnaire that asked for the age and gender of the participant’s study partner, as well as his or her relationship to the participant and whether or not the pair resided in the same dwelling, was administered.
A hearing screening was completed for those participants for whom we did not have an audiogram on file. The purpose of the screening was to confirm, rather than quantify, the hearing loss. An Interacoustics AD17TA portable audiometer was used to present two 25 dB HL pure tones to each ear via TDH-39 headphones at 0.5, 1, 2, and 4 kHz. Participants were enrolled in the study if, at a minimum, they failed to detect one presentation of the tone at one frequency in one ear.
Participants were given a red and a blue cloth bag, each containing a set of hearing aid components for the right and left ears, respectively. Participants were instructed to assemble both hearing aids and were allowed to select which ear they assembled first. Each bag contained three pieces of slim tubing in three lengths, three open dome tips in three sizes, one Siemens Pure hearing aid body, and one size 312 battery (Figure 1). The bags were accompanied by two spiral-bound instruction booklets, one for the right ear and one for the left ear, that outlined a step-by-step procedure for assembling the hearing aid from the parts provided, inserting the assembled device into the ear, troubleshooting the physical fit, and pressing an onboard button to generate a tone. The instructions were written at a reading level of grade 3.5, typeset in a large font, and were illustrated with black-and-white line drawings. Further details about the development of the instruction booklets may be found in Caposecco et al. (2011).
Figure 1.

Components of the self-fitting hearing aid prototype for the left ear that were provided to the participants
Note: Clockwise from top: tubes of three lengths, domes of three sizes, a size-312 battery, and the hearing aid body.
Partners were available to assist participants with the assembly task. However, participants were instructed to attempt each step in the instruction booklet prior to soliciting help from their partner, and partners were told not to offer assistance unless requested by the participant. The experimenter observed the procedure and did not answer any questions or provide assistance. Experimenter intervention in the assembly task was reserved for cases in which the participant and/or partner engaged in unsafe behavior (e.g., attempting to eat the battery), but this did not occur. The verbal instructions that were given to the participant prior to task commencement are found in Appendix B.
While the participants (and partners, if applicable) worked through the assembly task, the experimenter evaluated their performance. The time taken for the participants to complete each of the nine steps, including any assistance rendered by their partners, was measured with a stopwatch and recorded on a worksheet. At the completion of each step, the experimenter assigned a numerical rating to the participants’ performance. Accurate, independent completion of the step was given a rating of 3, while a rating of 2 was assigned to participants who received assistance from their partners on that step. A rating of 1 was given if the participant made one or more errors on the step, and a rating of 0 indicated that the participant did not attempt or complete the step. Note that the ratings should be thought of as discrete categories, rather than points on an interval scale. Two experimenters conducted the study, each of whom tested approximately half the participant group. A third experimenter, who was not otherwise involved in data collection for this study, observed several appointments to ensure uniformity in the rating and evaluation procedure.
Following the assembly task, the Montreal Cognitive Assessment (MoCA; Nasreddine et al., 2004) was administered. The MoCA is a brief, pen-and-paper test that assesses cognitive performance in the domains of visuospatial and executive function, memory, attention, language, abstraction, delayed recall, and orientation. The MoCA has been validated on an elderly population and has been shown to be more sensitive than the more widely used Mini-Mental State Examination (MMSE; Folstein, Folstein, & McHugh, 1975) in distinguishing between normal cognitive aging and mild cognitive impairment (Olson, Chhanabhai, & McKenzie, 2008). The maximum score that can be obtained on the MoCA is 30, with scores ≥ 26 indicating normal cognitive function and scores < 26 suggestive of varying degrees of cognitive impairment.
The participants’ manual dexterity was assessed with the Grooved Pegboard Test (GPT; Trites, 1977), which requires the participant to place small metal pegs into a square 25-hole board as quickly as possible. Both the pegs and the holes are keyhole-shaped, and each hole is angled slightly differently, requiring the participant to draw on fine motor skills to correctly orient each peg. Participants completed the test twice, first with their dominant hand and then with their nondominant hand. The score of this test is the time, expressed in seconds, taken to complete the peg insertion task.
The Short Test of Functional Health Literacy in Adults (S-TOFHLA; Parker, Baker, Williams, & Nurss, 1995) was administered to measure the participants’ health literacy. The S-TOFHLA is an exercise in which the test-taker is presented with several paragraphs of health-related text from which one or two words are missing from each sentence. The task is to fill in each blank with the correct word, which is selected from a list of four choices. The S-TOFHLA is a cloze exercise, a type of assessment that requires the ability to understand context and vocabulary to correctly identify the missing words. A version of the S-TOFHLA that had been modified to reflect Australian language and culture was used in this study (Buchbinder, Hall, & Youd, 2006). The maximum obtainable score on the S-TOFHLA is 36, with a score of ≥ 23 indicating adequate health literacy, a score between 17 and 22 indicating marginal health literacy, and a score of < 16 indicating inadequate health literacy.
The study appointment was approximately 1.5 hr in length and both participants and their partners were paid a small cash gratuity for their time.
Data Management
Responses to items on the demographic questionnaire that employed a scale were assigned numerical values. Responses to items targeting general literacy, self-assessed health literacy, general health, visual acuity, and self-assessed hearing status were assigned values that increased with a greater degree of perceived disability or handicap. For example, a response of excellent was assigned a value of 1, while a response of very poor was assigned a value of 5. For the questions relating to education and daily hearing aid use, the opposite was true, with responses of higher rank attracting a higher numerical value.
To make the occupation data fit more easily into this paradigm, the occupations listed on the demographic questionnaire were grouped to yield five categories. Category 1 includes laborer and machinery operator/driver, category 2 includes sales worker and technician/trade worker, and category 3 includes community/personal worker and clerical/administrative worker. Categories 4 and 5 represent manager and professional, respectively.
The decile ranking assigned to the participant’s home suburb by the Australian Bureau of Statistics’ Socio-Economic Indexes for Areas (SEIFA) was used as an indicator of SES. Decile rankings can range from 1 to 10 and are a measure of economic advantage and disadvantage relative to other areas of Australia. A decile ranking of 1 indicates that the area is the most disadvantaged relative to areas in the other deciles. Both the median and modal decile rankings for our participant group were 10, with 79% of participants living in suburbs that are classified as the most socioeconomically advantaged areas in Australia. Due to the extremely skewed distribution in our participant sample, SES was eliminated as an independent variable in all subsequent analyses.
Self-assessments of participants’ visual acuity were elicited through three questions on the demographic questionnaire that asked about general eyesight as well as degree of difficulty experienced while reading and while performing such tasks as cooking or sewing. Spearman’s rho showed that the participants’ responses to these questions were significantly correlated (ρ = .44-.70, p < .05). The three questions all used very similar 5-point rating scales, so individual participant responses were averaged to yield a single visual acuity rating.
While audiograms were not measured in this study, threshold data were available from past studies for 54 participants. Spearman’s rho showed a moderate but significant correlation between participants’ audiometric thresholds and self-assessment of their unaided hearing (ρ = .53, p < .05). This is in line with the findings of Salonen, Johansson, Karjalainen, Vahlberg, and Isoaho (2011), who reported a significant relationship between objectively measured and self-assessed degree of hearing loss. Consequently, self-reported hearing status is used as the parameter for degree of hearing loss in subsequent analyses.
The two manual dexterity scores yielded by the GPT for the dominant and nondominant hands were highly correlated (r = .73, p < .0001). The scores were therefore averaged for each participant to produce a single value.
Results
Participant Profile
Table 1 lists the mean or median value, standard deviation, and range of the independent variables measured on each of the 80 study participants. Both the median and modal education level was TAFE1 or trade qualification, with 30% of the participant group reporting it as their highest level of formal education. Participants reported an average of 11 years of amplification experience, while 18 of the 80 participants had not worn hearing aids at all prior to their entry into the study. If the unaided participants are excluded, the mean number of years of hearing aid experience increases to 14. A variety of hearing aid styles, including traditional BTEs, slim-fit BTEs, ITEs, and in-the-canal (ITC) devices, were represented among the aided participants. Median daily hearing aid use was between 4 and 8 hr although 39% of participants reported wearing their hearing aid(s) for more than 8 hr per day. Forty-one percent of the study group reported that their unaided hearing was fair on a scale that ranged from very poor to excellent. Across the visual measures, the median rating was 1.3, which corresponded to a point between the excellent and good categories.
Table 1.
Mean or Median Value, Standard Deviation, and Range of the Independent Variables Measured on Each Participant
| Mean/median | Standard deviation | Range | |
|---|---|---|---|
| Age (years) | 73 | 10.9 | 45-90 |
| Education level | 3 (TAFE/trade qualification) | 1.3 | 1-6 |
| Occupation | 4 (Manager/professional) | 1.3 | 1-5 |
| Hearing aid experience (years) | 11 | 12.9 | 0-60 |
| Daily aid use | 4 (Between 4 and 8 hr/day) | 2.1 | 0-5 |
| Hearing | 3 (Fair) | 0.8 | 2-5 |
| Vision | 1.3 (Good to excellent) | 0.6 | 1-4.3 |
| GPT | 100.9 | 37.6 | 57.5-241.5 |
| MoCA | 26.1 | 3.1 | 15-30 |
| S-TOFHLA | 33.8 | 4.6 | 3-36 |
Note: TAFE = Technical and Further Education; GPT = Grooved Pegboard Test; MoCA = Montreal Cognitive Assessment; S-TOFHLA = Short Test of Functional Health Literacy in Adults.
The manual dexterity test produced a mean score of 101 s across the two hands (SD = 37.6 s). Norms for this test vary considerably depending on scoring method and population. However, it should be noted that our participant group, on average, completed the GPT more slowly and demonstrated more performance variation than did the age-matched reference group listed in the test’s user manual. The mean MoCA score among our participant group was 26, with a range of 15 to 30 and a standard deviation of 3.15. The mean S-TOFHLA score obtained by our participants was 34 and ranged from 3 to 36, with a standard deviation of 4.61.
Variable Reduction and Classification
A Spearman’s rho rank order correlation analysis was then conducted on gender and the 10 independent variables listed in Table 1: age, level of education, occupation, self-reported hearing status, hearing aid experience, daily hearing aid use, self-reported visual acuity, manual dexterity, cognitive function, and health literacy. An initial analysis revealed a strong correlation between all the performance tests and visual acuity, a result that was influenced by the data of one participant who performed well below average on these tests. Data for this participant was subsequently excluded from the factor analysis, as he was considered to be an outlier within the participant group.
From the new analysis on 79 data points, medium to strong significant correlations were found for three pairs of variables. Age and manual dexterity were significantly correlated (r = .71, p < .05), suggesting that younger participants were likely to have a greater degree of manual dexterity. The correlation between education level and occupation (r = .60, p < .05) suggests that participants with higher levels of formal education were more likely to work or have worked in professional and/or managerial jobs. Hearing aid experience and daily hearing aid use were also significantly correlated (r = .71, p < .05), suggesting that the more hearing aid experience participants had, the greater the number of hours they used their hearing aids per day. For the purpose of further analyses, age, occupation, and hearing aid experience were chosen as representative parameters as they were considered either easier to obtain (for example, asking for an individual’s age versus subjecting him or her to an assessment of manual dexterity) and/or less susceptible to variation over time (for example, determining the number of years an individual has worn hearing aids versus asking him or her to accurately recall the pattern of daily aid use over a long period of time). Gender, self-reported visual acuity, cognitive function, and health literacy were also selected as independent parameters for use in further analyses.
Hearing Aid Assembly Task
For the purpose of the data analysis, the hearing aid assembly task was divided into five steps: tube selection, dome selection, parts assembly, insertion into the ear, and button press. The parts assembly step encompasses attaching the dome to the tube, attaching the tube to the hearing aid body, and inserting the battery.
As shown in Table 2, participants took between 2.0 and 34.5 min to complete the entire task for the first hearing aid, with a mean assembly time of 7.5 min (SD. = 4.9 min). Participants took between 1.5 and 15.7 min to assemble the second hearing aid, with a mean assembly time of 3.9 min (SD = 2.5 min). According to a paired t test, the time taken to assemble the second hearing aid was significantly shorter, t(158) = 5.7, p < .0000001.
Table 2.
Mean Assembly Time, in Minutes, and Standard Deviations for the Five Major Steps of the Hearing Aid Assembly Task for Both Ears
| First ear | Second ear | |
|---|---|---|
| Tube selection | 1.1 (0.7) | 0.5 (0.4) |
| Dome selection | 0.6 (1.0) | 0.3 (0.2) |
| Assembly of parts | 2.6 (1.5) | 1.6 (1.1) |
| Insertion into ear | 2.1 (1.6) | 1.1 (0.9) |
| Button press | 0.5 (0.7) | 0.3 (0.5) |
| Total time | 7.5 (4.9) | 3.9 (2.5) |
Note: Assembly of parts includes attaching the dome to the tube, attaching the tube to the hearing aid body, and inserting the battery. The total time also includes the extra time taken by participants for troubleshooting.
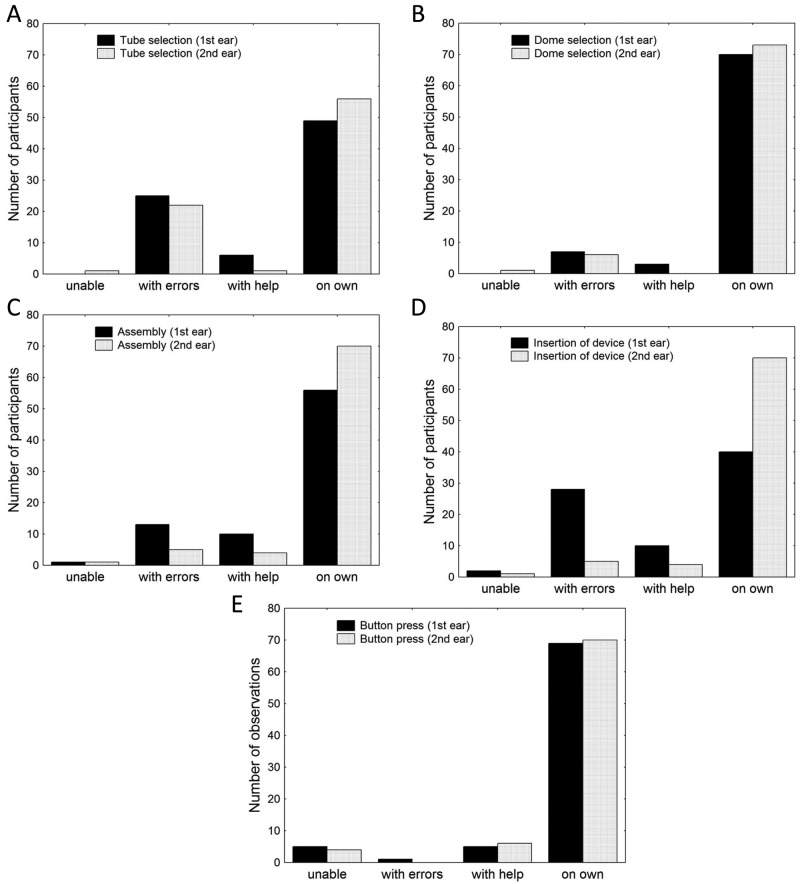
As the participants progressed through each step in the assembly procedure, they were also assigned a rating that reflected how accurately they performed the step (that is, whether they correctly followed the instructions) and whether or not they requested help on the step from their partner. On the basis of these ratings, participants were grouped into four categories: (a) did not complete the step, (b) completed the step with errors (re: the instructions), (c) completed the step with assistance, and (d) completed the step on their own. Figure 2 shows the number of participants in each group for both the first and second assembly tasks. The majority of participants were able to complete each step on their own and without errors, although a proportion of participants made errors in selecting the correct tube length and in inserting the first assembled device into the ear.
Figure 2.
Number of participants classified as unable to perform the task, able to perform task with errors, able to perform task with help, and able to perform task with assistance for (a) tube selection, (b) dome selection, (c) device assembly, (d) device insertion, and (e) button press steps in the hearing aid assembly task
Note: Ratings are shown for both the first and second task attempts.
Participants were subsequently classified into six categories according to their overall performance on the hearing aid assembly task. As illustrated in Figure 3, participants were grouped according to whether they completed all assembly steps correctly on their own (Group 1), completed all steps correctly with help (Group 2), completed all steps on their own with a single error (Group 3), completed all steps on their own with more than one error (Group 4), required help to complete the steps and made errors (Group 5), or were unable to complete the task (Group 6). Twenty percent of the participant group were able to complete the hearing aid assembly task for both ears without errors and without requiring assistance from their partners. Those participants who assembled the hearing aids on their own but made one or more errors made up 50% of the group. Five percent made no errors but required help to complete the task, while 24% both needed assistance and made mistakes on at least one step. One participant was unable to complete the task at all, even with the assistance of her partner.
Figure 3.
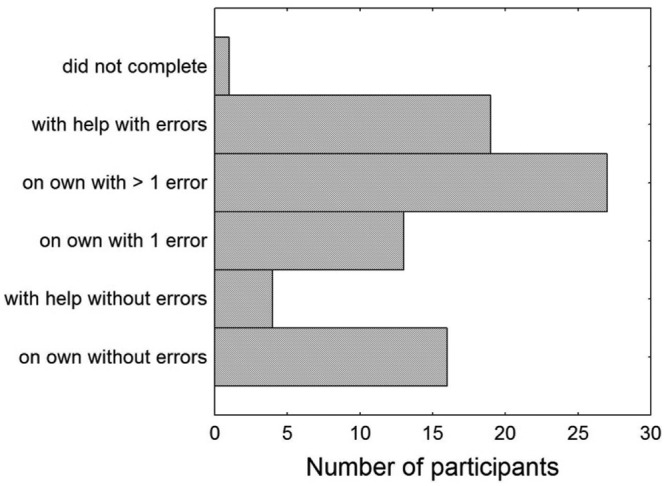
Classification of participants according to performance accuracy and need for assistance on the hearing aid assembly task
Two discriminant analyses were then conducted using the forward stepwise method. Two participants were excluded from the data set: the participant who was unable to complete the hearing aid assembly task and a participant who did not obtain a valid score on the MoCA and was thus automatically excluded by the statistical analysis software. The first discriminant analysis was conducted to determine the influence of the seven independent variables on whether or not the participant required assistance to complete the hearing aid assembly task. The discriminant analysis produced a significant model, F(3, 74) = 6.1; p < .0009, that included three parameters: gender, health literacy, and cognitive function. When combined, these three parameters correctly classified 74% of the participants as either able or unable to complete the hearing aid assembly task on their own. The model suggested that the participants who assembled the hearing aid without assistance were more likely to be male and to have higher levels of health literacy and cognitive function. Based on the standardized coefficients (β values), p levels, and tolerance (1 − R2) values of each variable (Table 3), gender contributed the most to the model, followed by health literacy.
Table 3.
The Three Independent Variables in the Model That Correctly Classified 74% of the Study Participants as Either Able or Unable to Complete the Hearing Aid Assembly Task on Their Own
| Parameter | β | p values | Tolerance |
|---|---|---|---|
| Gender | −.86 | .0008 | 0.97 |
| Health literacy | −.82 | .009 | 0.68 |
| Cognitive function | .36 | .25 | 0.69 |
Note: The weight of each predictor’s contribution to the model (standardized β coefficients), significance levels (p), and the proportion of the variance that is attributable to each predictor (tolerance) are shown.
A second discriminant analysis was conducted to determine the influence of the seven independent variables identified in the factor analysis on whether or not the participants who completed the task on their own were able to complete the hearing aid assembly task without errors. Participants who had received help with one or more steps of the assembly task and had made errors on one or more steps (Group 5) were excluded from the analysis, as it could not be definitively determined whether it was the participant or his or her partner who was responsible for the error(s).
The discriminant analysis produced a significant model, F(4, 55) = 7.5; p < .0001, that included four parameters: gender, health literacy, age, and hearing aid experience. When combined, these four parameters correctly classified 80% of the participants as having completed the hearing aid assembly task either with or without errors. The model suggested that the participants who made no errors were more likely to be female, to have higher levels of health literacy, to be older, and to have less prior experience with hearing aids. The final two predictors appear counterintuitive; however, these parameters contributed the least to the model, and the difference between the mean values for these parameters of each group was small. Participants who were able to complete the assembly task without errors had a mean age of 71.2 years and an average of 9.5 years of previous hearing aid experience, while those who made errors in the assembly process had a mean age of 70.8 years and had worn hearing aids for an average of 11.8 years prior to entering the study.
Based on the standardized coefficients (β values), p levels, and tolerance values of each variable (Table 4), the model assigned greater weight to gender and health literacy than to the other two parameters. Indeed, when the discriminant analysis was repeated with only gender and health literacy as independent variables, the same percentage of participants (80%) was correctly assigned to the two groups.
Table 4.
The Four Independent Variables in the Model That Correctly Classified 80% of the Study Participants as Either Able or Unable to Complete the Hearing Aid Assembly Task Without Errors
| Parameter | β | p values | Tolerance |
|---|---|---|---|
| Gender | −.89 | .00004 | 0.96 |
| Health literacy | .49 | .04 | 0.85 |
| Age | .37 | .14 | 0.84 |
| Hearing aid experience | −.25 | .27 | 0.97 |
Note: The weight of each predictor’s contribution to the model (standardized β coefficients), significance levels (p), and the proportion of the variance that is attributable to each predictor (tolerance) are shown.
Discussion
Overall, 79 out of 80 participants were able to complete the assembly and insertion tasks associated with the self-fitting hearing aid, either independently or with assistance from their partners. When the individual steps in the assembly process are examined separately, between 70% and 88% of participants were able to independently select the correct dome size, assemble the hearing aid, or press the onboard button when completing the task for the first ear (Figures 2b, 2c, and 2e). The percentage of participants who successfully completed these steps increased to between 88% and 91% when they assembled the second hearing aid. It is possible that these high success rates were due in part to the relatively high proportion of experienced hearing aid users, particularly among those participants above 60 years of age, who took part in this study.
With respect to the remaining steps, it appears that participants experienced greater difficulty with tube selection and device insertion than with any other component of the assembly task. As shown in Figures 2a and 2d, the percentage of participants who completed these steps during the first assembly task without errors or assistance was 61% and 50%, respectively. Tube selection was the first step in the hearing assembly procedure. Participants were provided with tubes in three lengths: short, medium, and long. According to the instruction booklet, participants were advised to first arrange the tubes in size order on the table and then to select the medium-length tube. Later in the booklet, in the troubleshooting section, participants were given the opportunity to change the tube length if the medium size did not fit their ear. A number of participants commented that they could not tell the difference between the different lengths, particularly between the medium and long tubes, and thus were forced to select one at random to continue with the task. The line drawing in the instruction booklet suggested that there were greater length differences between the three tubes than there were in real life, even though the short and long tubes differ in length by only 1 cm. Many participants had difficulty discerning this difference, particularly as each tube is curved in two places in different directions. When arranging the tubes on the table, some participants did not line them up in a uniform direction, which made it even more difficult to distinguish the different lengths. Based on verbal comments that were made while completing this step, it was clear that participants correctly understood that the medium-length tube was required. However, if they were unable to judge which tube was the medium one, the step was performed incorrectly. The success rate for tube selection increased to 70% on the second attempt, but this was still lower than the success rates for the other steps.
Since the tubes themselves cannot be shortened or lengthened to make them easier to distinguish, one solution to this issue may be to clearly label the tubes and/or their packaging. Although the tubes used in our study were standard tubes that are widely used with traditional slim-fit BTE hearing aids and thus are already labeled with numbers, these numbers are intended for use by audiologists and technicians and are too small for the average hearing aid user to see. Indeed, not one participant noticed the presence of these numbers. The instructions and accompanying diagram could also be improved to make the process for comparing the tube lengths easier to understand.
Insertion of the device into the ear was another step that caused problems for a large number of participants, although there was an improvement in the success rate on this step from 50% on the first attempt to 88% on the second attempt. A small number of errors on this step are the result of participants placing the dome portion of the hearing aid into the ear canal incorrectly. The remaining proportion of errors can be traced to incorrect placement of the concha lock (or anchor, as it was called in the instruction booklet). Many participants ignored it entirely, leaving it sticking out, while the ones who did attempt to put the anchor into their concha did not do so fully, causing it to unfurl out of their ear.
There are several possible reasons for the low rate of success on this step. First, of the numerous line drawings in the instruction booklet, the illustration of concha lock placement was probably the most ambiguous. From the picture alone, it is not immediately obvious exactly how the anchor should lie along the bottom of the concha. It was also observed that some participants did not understand the accompanying text (“Press the anchor into the bowl at the bottom of your ear”). The wording of this step was one of the most difficult parts of developing the instruction booklet, as the use of an uncommon anatomical word like “concha” had to be avoided. However, the substitution of the word “bowl” confused some participants, who did not understand to which part of the ear the instructions were referring.
A second possible explanation for participants’ difficulty with this step may have been their unfamiliarity with this component of a hearing aid. Only 19% of participants entered the study wearing slim-fit BTE hearing aids and, of these, only half had concha locks on their own devices. Third, as several participants pointed out, it is difficult to confirm correct placement of the anchor by following the next step in the instruction booklet (“The hearing aid should look like this in your ear”), as no mirror was made available to the participants. Even participants who may have had the ability to self-correct an incorrect anchor placement were not able to do so, as they could not see that they had made an error in the first place. Use of a mirror, removal of the anchor, and/or clearer instructions on this step may yield better fitting outcomes.
Participants were given the opportunity to troubleshoot the physical fit of the assembled hearing aid following the insertion step. The booklet instructed participants to check if they were experiencing a list of fit problems (e.g., “The hearing aid is falling off your ear”) and offered advice on what to do to fix them (e.g., “Try a shorter tube”). When assembling the first device, 14% of the participants skipped the troubleshooting step, while 51% of participants did not troubleshoot during the second assembly attempt. A snug, comfortable fit is a prerequisite for the successful and continued use of any hearing aid. Evaluating and troubleshooting physical fit issues are, in the case of traditional hearing aids, the domain of the trained hearing health care professional. However, for a self-fitting hearing aid, these tasks become the responsibility of the user. It is therefore critical that users of a self-fitting hearing aid learn how to accurately assess the fit of their devices and to modify them accordingly. One way this may be accomplished is to provide specific, practical criteria against which users can evaluate the fit and comfort of their devices. For example, instead of instructing users to check whether or not “The hearing aid is falling off your ear,” it might be clearer for the instructions to say the following: “Move your head from side to side. Bend forward and reach toward your feet. Does the hearing aid fall off your ear when you do these things? If so, choose a shorter tube.” It is also possible that physical fit issues may not become apparent until after the user has worn the hearing aid for some time. If this is the case, it may be worthwhile to include follow-up instructions and/or a separate troubleshooting guide that the user can refer to both during and several days or weeks after the initial assembly and fitting.
One participant in the group was unable to complete the full hearing aid assembly task. She correctly selected the appropriate dome and tube and was able to put these two parts together on her own, but was unsuccessful in attaching the dome/tube combination to the hearing aid body. She requested help from her partner, but the partner refused to assist, saying that the study tasks were “inappropriate for elderly people” and “too confusing.” As the participant could go no further in assembling the hearing aid on her own, the task was therefore terminated. Although this participant had no prior experience with hearing aids, her performance on other relevant measures, such as the MoCA and the S-TOFHLA, was no different to the other nonusers who were successfully able to complete the assembly task. It is likely, therefore, that this participant would have been successful in assembling the device if a more supportive partner had been available to assist.
A second participant performed well below average on the MoCA, S-TOFHLA, and GPT. He was, however, able to assemble both hearing aids, albeit with assistance from his partner on most steps. In light of this participant’s cognitive difficulties, which were apparent even when speaking informally with him, it is unlikely that he would be a successful, independent user of a self-fitting hearing aid. However, if an assistant were willing and able to take over the assembly and management tasks, it is possible that he would be a candidate for such a device.
As mentioned in the introduction, many studies have found that while hearing aid management difficulties tend to increase with age, such difficulties are more prevalent among female hearing aid users over the age of 75 (e.g., Stephens & Meredith, 1991; Ward et al., 1979). In the Ward et al. (1979) study, participants were asked to perform several of the same hearing aid manipulation tasks that we required of our participants, such as inserting a battery into a hearing aid and placing the device into the ear. However, participants in this and other similar management studies were assessed on their own, while our participants were allowed to request assistance with these tasks from a partner. When we looked at factors that influenced whether or not our participants could complete the hearing aid assembly task on their own, we found that gender was a strong predictor of this. Specifically, we found that male participants were more likely to assemble and insert the hearing aid on their own than were the female participants. However, when assembly accuracy was examined, we found that it was the female participants who were more likely to complete the task correctly. A related finding is that our female participants were more likely than the male participants to request assistance from their partners. Fifty percent of female participants asked for help, whereas only 17% of male participants did so. Requests for assistance were not influenced by the gender of the partner; relatively similar proportions of female (28%) and male (32%) partners became involved in the assembly task. Our results suggest that the role of the partner is therefore an important one. For segments of the population who have been repeatedly identified as experiencing the greatest difficulty with hearing aid management, such as women over the age of 75, the involvement of an assistant may mean the difference between an unsuccessful hearing aid user and a successful one. The majority of the female participants in the current study, however, and likely those in the management studies conducted in the 1980s and 1990s, were older women who did not work outside the home or did so only for a limited period of time many years ago. It is possible, therefore, that the gender effect we observed in this study may become less significant over time, as increasing numbers of women with careers enter the aging population and technology becomes more common in the lives of older adults.
Health literacy emerged as a significant predictor in our analyses, both of whether participants required assistance to assemble the hearing aid prototype and whether they could complete the assembly task without errors. The higher the health literacy level, the more likely the participant was to be able to assemble the device on his or her own and to do so correctly. Health literacy is a factor that is often overlooked in the field of audiology, although research indicates that higher levels of health literacy are linked to more successful health outcomes (e.g., Schillinger et al., 2002; Williams et al., 1998). Audiological clients, particularly those being fitted with hearing aids for the first time, are typically faced with a great deal of new, highly technical information that is presented to them in a short span of time. Although the majority of clients accessing audiology services are older adults, printed instructional materials that accompany hearing aids often use a sophisticated vocabulary unsuited to the layperson (e.g., telecoil, transmitter, Bluetooth) and are printed in small font sizes against a low-contrast background. Supplementary information provided by the audiologist is often given orally, and the message may not be correctly received due to the client’s hearing loss, a health literacy level that is at odds with the information being presented, or other factors.
Health literacy also correlates with SES, a fact that may have affected the results of our study. Not only did our participant group comprise individuals from a highly developed part of the world, but our participants, on average, tended to belong to the highest SES stratum in the country. Including participants from a range of socioeconomic backgrounds with, presumably, a range of health literacy levels may have allowed us to observe a wider variety of errors in participants’ interpretation and understanding of the assembly instructions.
The finding in this study that health literacy so strongly influences an individual’s ability to independently and accurately manage a novel amplification device is an important one, as unlike gender, this is an aspect of audiological service delivery that hearing health care professionals and the hearing aid industry can control. In accordance with evidence-based health literacy principles, such strategies as larger fonts, pictogram illustrations, and lay vocabulary can and should be used to improve accessibility to information for a wider range of hearing aid users. The effect of health literacy will also be an important consideration when the self-fitting hearing aid is introduced in developing countries, as health literacy levels tend to be lower compared to those in the developed world (Kickbusch, 2001; Nutbeam & Kickbusch, 2000).
Although a significant statistical model was obtained with our data set, our conclusions should still be interpreted with caution as some variables, such as health literacy and gender, displayed a skewed distribution. The model should ideally be verified in another population, preferably one in which the independent variables are distributed more normally. As the self-fitting hearing aid is designed primarily for individuals with hearing loss in the developing world, this study should be repeated in a developing country to identify and evaluate potential management issues among the device’s target population.
Summary
User management of the assembly tasks associated with a self-fitting hearing aid among older hearing-impaired adults was investigated in this study. Eighty participants, who were drawn from an urban area in a developed country, followed a set of illustrated, written instructions at a grade level of 3.5 to assemble a hearing aid, with the option to request assistance with the task from an accompanying partner. The influence of a range of personal and audiometric characteristics was examined through structured questionnaires and standardized assessments of health literacy, cognitive performance, and manual dexterity.
The results of the study indicated that 79 out of 80 participants were successfully able to assemble the study hearing aids, insert the devices into the ear, and press an onboard button, either on their own or with the assistance of a partner. Twenty-five percent of these participants completed the assembly task without errors, while the remaining 75% made mistakes that were primarily related to selecting the correct tube length and positioning the anchor in the concha. Changes to both the design of the device and to the instructions could reduce or eliminate these errors.
Health literacy significantly influenced participants’ ability to manage the assembly task on their own as well as their ability to complete the task without errors. This suggests that the reading level at which the instructions are presented is likely to underpin the success of the self-fitting hearing aid. Gender was another significant factor, with male participants more likely to complete the assembly task on their own and female participants more likely to assemble the hearing aids without errors. The importance of the assistant’s role in successful hearing aid management was highlighted with the finding that female participants were three times as likely as male participants to seek assistance with the assembly task. While the participants in our study were successful overall with the hearing aid assembly task, ultimately, management and feasibility of the self-fitting hearing aid should be verified among hearing aid candidates in a developing country.
Appendix A
Demographic Questionnaire
Date of Birth:
Gender: Female/Male
What is the highest level of formal education you have completed? Less than high school (year or grade ____)/high school/TAFE or trade qualification/ bachelor’s degree (e.g., BA, BSc)/postgraduate diploma/postgraduate degree (e.g., master’s degree, PhD)
What is your current employment status? Employed full-time/employed part-time/house duties/retired/student/unemployed
Which category2 best describes your occupation now, or your main occupation when you were working? Community or personal worker/clerical or administrative worker/laborer/machinery operator or driver/manager/professional/sales worker/technician or trade worker
How would you rate your English reading skills? Excellent/good/moderate/fair/poor
How confident are you at filling out medical forms by yourself? Extremely/quite a bit/somewhat/a little bit/not at all
How would you rate your general health? Excellent/good/fair/poor/very poor
How would you rate your eyesight (with glasses or contact lenses, if you wear them)? Excellent/good/fair/poor/very poor
How much difficulty do you have reading ordinary print in newspapers (with glasses or contact lenses, if you wear them)? No difficulty at all/a little difficulty/moderate difficulty/extreme difficulty/stopped reading the newspaper because of my eyesight/no interest in reading the newspaper
How much difficulty do you have doing work or hobbies that require you to see well up close, such as cooking, sewing, or fixing things around the house (with glasses or contact lenses, if you wear them)? No difficulty at all/a little difficulty/moderate difficulty/extreme difficulty/stopped doing close work because of my eyesight/no interest in doing close work
How would you rate your hearing? Excellent/good/fair/poor/very poor
Have you ever been fitted with hearing aid(s)? Yes/No (go to question 18)
When did you first receive hearing aid(s)?
Were you first fitted with one or two hearing aid(s)?
Do you currently wear hearing aid(s)? Yes/No (go to question 18)
When did you receive your current hearing aid(s)?
Do you usually wear both, one, or neither of your hearing aid(s)?
On an average day, how many hours do you wear your hearing aid(s)? None/less than 1 hr per day/between 1 and 4 hr per day/between 4 and 8 hr per day/more than 8 hr per day
Please answer this question only if you have never been fitted with, or do not currently wear, hearing aids. Have you ever handled a hearing aid (e.g., assisted a friend or family member with their hearing aid)? Yes/No
Appendix B
Prior to beginning the assembly task, the experimenter read the following instructions to the participant and his or her partner:
The cloth bag in front of you contains all the parts you will need to build a hearing aid. Please follow the instructions in this booklet to put the parts together. You can ask your partner for help, but you must try each step in the assembly task on your own first before you can ask for help. You are the only one who can ask for help—your partner cannot decide to help you. I cannot help either of you with the task or answer any questions. Please try to pretend that you and your partner are alone and that I am not in the room with you. Do you have any questions before you start?
TAFE stands for Technical And Further Education and refers to an Australia-wide network of postsecondary institutions that provide vocational education and training.
Categories were taken from the Australian Bureau of Statistics census form.
Footnotes
Authors’ Note: Portions of this article were presented at the First International Conference on Cognitive Hearing Science in Linköping, Sweden, June 2011 and at the 10th European Federation of Audiology Societies Congress in Warsaw, Poland, June 2011. The hearing aids used in this study were provided by Siemens Audiologische Technik, Erlangen, Germany.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for this study was provided by the HEARing Cooperative Research Centre, Melbourne, Australia.
References
- Brooks D. N. (1985). Factors relating to the under-use of postaural hearing aids. British Journal of Audiology, 19, 211-217 [DOI] [PubMed] [Google Scholar]
- Buchbinder R., Hall S., Youd J. M. (2006). Functional health literacy of patients with rheumatoid arthritis attending a community-based rheumatology practice. Journal of Rheumatology, 33, 879-886 [PubMed] [Google Scholar]
- Caposecco A., Hickson L., Meyer C. (2011). Assembly and insertion of a self-fitting hearing aid: Design of effective instruction materials. Trends in Amplification, 15(4), 184-195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Convery E., Keidser G., Hartley L. (2011). Perception of a self-fitting hearing aid among urban-dwelling hearing-impaired adults in a developed country. Trends in Amplification, 15(4), 175-183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon H. (2001). Hearing aids. Sydney, Australia: Boomerang Press [Google Scholar]
- Doak C. C., Doak L. G., Root J. H. (1996). Teaching patients with low literacy skills. Philadelphia, PA: J. B. Lippincott [Google Scholar]
- Erber N. P. (2003). Use of hearing aids by older people: Influence of non-auditory factors (vision, manual dexterity). International Journal of Audiology, 42(2), S21-S25 [PubMed] [Google Scholar]
- Folstein M. F., Folstein S. E., McHugh P. R. (1975). “Mini-Mental State”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189-198 [DOI] [PubMed] [Google Scholar]
- Griffing T. (2009). Crafting protocols: Selection and fitting issues for older adults. Hearing Review, 16(13), 18-19 [Google Scholar]
- Henrichsen J., Noring E., Lindemann L., Christensen B., Parving A. (1991). The use and benefit of in-the-ear hearing aids. Scandinavian Audiology, 20, 55-59 [DOI] [PubMed] [Google Scholar]
- Hickson L., Hamilton L., Orange S. P. (1986). Factors associated with hearing aid use. Australian Journal of Audiology, 8(2), 37-41 [Google Scholar]
- Jacobson G. P., Newman C. W., Sandridge S. A., McCaslin D. L. (2002). Using the Hearing Aid Selection Profile to identify factors in hearing aid returns. Hearing Journal, 55(2), 30-33 [Google Scholar]
- Kapteyn T. S. (1977). Satisfaction with fitted hearing aids. I. An analysis of rather technical information. Scandinavian Audiology, 6, 147-156 [DOI] [PubMed] [Google Scholar]
- Kickbusch I. S. (2001). Health literacy: Addressing the health and education divide. Health Promotion International, 16, 289-297 [DOI] [PubMed] [Google Scholar]
- Kricos P. B. (2006). Audiologic management of older adults with hearing loss and compromised cognitive/psychoacoustic auditory processing capabilities. Trends in Amplification, 10(1), 1-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar M., Hickey S., Shaw S. (2000). Manual dexterity and successful hearing aid use. Journal of Laryngology and Otology, 114, 593-597 [DOI] [PubMed] [Google Scholar]
- Maurer J., Schow R. L. (1996). Audiologic rehabilitation for elderly adults: Assessment and management. In Schow R. L., Nerbonne M. A. (Eds.), Introduction to audiologic rehabilitation (pp. 413-454). Boston, MA: Allyn & Bacon [Google Scholar]
- Meredith R., Stephens D. (1993). In-the-ear and behind-the-ear hearing aids in the elderly. Scandinavian Audiology, 22, 211-216 [DOI] [PubMed] [Google Scholar]
- Mulrow C. D., Tuley M. R., Aguilar C. (1992). Correlates of successful hearing aid use in older adults. Ear and Hearing, 13(2), 108-113 [DOI] [PubMed] [Google Scholar]
- Nasreddine Z. S., Chertkow H., Phillips N., Whitehead V., Collin I., Cummings J. L. (2004). The Montreal Cognitive Assessment (MoCA): A brief cognitive screening tool for detection of mild cognitive impairment. Neurology, 62(7, S5), A132. [DOI] [PubMed] [Google Scholar]
- Nutbeam D., Kickbusch I. (2000). Advancing health literacy: A global challenge for the 21st century. Health Promotion International, 15, 183-184 [Google Scholar]
- Olson R. A., Chhanabhai T., McKenzie M. (2008). Feasibility study of the Montreal Cognitive Assessment (MoCA) in patients with brain metastases. Supportive Care in Cancer, 16, 1273-1278 [DOI] [PubMed] [Google Scholar]
- Osborne H. (2005). Health literacy from A to Z. Boston, MA: Jones and Bartlett [Google Scholar]
- Parker R. M., Baker D. W., Williams M. V., Nurss J. R. (1995). The test of functional health literacy in adults: A new instrument for measuring patients’ literacy skills. Journal of General Internal Medicine, 10, 537-541 [DOI] [PubMed] [Google Scholar]
- Ratzan S. C., Parker R. M. (2000). Introduction. In Selden C. R., Zorn M., Ratzan S. C., Parker R. M. (Eds.), National library of medicine current bibliographies in medicine: Health literacy. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services [Google Scholar]
- Salonen J., Johansson R., Karjalainen S., Vahlberg T., Isoaho R. (2011). Relationship between self-reported hearing and measured hearing impairment in an elderly population in Finland. International Journal of Audiology, 50, 297-302 [DOI] [PubMed] [Google Scholar]
- Schillinger D., Wang F., Grumbach K., Daher C., Palacios J., Diaz-Sullivan G., Bindman A. B. (2002). Association of health literacy with diabetes outcomes. Journal of the American Medical Association, 288, 475-482 [DOI] [PubMed] [Google Scholar]
- Sorri M., Luotonen M., Laitakari K. (1984). Use and non-use of hearing aids. British Journal of Audiology, 18, 169-172 [DOI] [PubMed] [Google Scholar]
- Stephens S. D. G., Meredith R. (1991). Physical handling of hearing aids by the elderly. Acta Otolaryngologica Supplement, 476, 281-285 [DOI] [PubMed] [Google Scholar]
- Tiffin J., Asher E. J. (1948). The Purdue Pegboard: Norms and studies of reliability and validity. Journal of Applied Psychology, 32, 234-247 [DOI] [PubMed] [Google Scholar]
- Trites R. L. (1977). Neuropsychological test manual. Ottawa, ON, Canada: Royal Ottawa Hospital [Google Scholar]
- Upfold L. J., May A. E., Battaglia J. A. (1990). Hearing aid manipulation skills in an elderly population: A comparison of ITE, BTE, and ITC aids. British Journal of Audiology, 24, 311-318 [DOI] [PubMed] [Google Scholar]
- Ward P. R., Gowers J. I., Morgan D. C. (1979). Problems with handling the BE10 Series hearing aids among elderly people. British Journal of Audiology, 13, 31-36 [DOI] [PubMed] [Google Scholar]
- Williams M. V., Baker D. W., Parker R. M., Nurss J. R. (1998). Relationship of functional health literacy to patients’ knowledge of their chronic disease: A study of patients with hypertension and diabetes. Archives of Internal Medicine, 158, 166-172 [DOI] [PubMed] [Google Scholar]