Abstract
The need for reliable access to hearing health care services is growing globally, particularly in developing countries and in remotely located, underserved regions in many parts of the developed world. Individuals with hearing loss in these areas are at a significant disadvantage due to the scarcity of local hearing health care professionals and the high cost of hearing aids. Current approaches to making hearing rehabilitation services more readily available to underserved populations include teleaudiology and the provision of amplification devices outside of the traditional provider-client relationship. Both strategies require access to such resources as dedicated equipment and/or specially trained staff. Another possible strategy is a self-fitting hearing aid, a personal amplification device that is equipped with an onboard tone generator to enable user-controlled, automated, in situ audiometry; an onboard prescription to determine the initial hearing aid settings; and a trainable algorithm to enable user-controlled fine-tuning. The device is thus assembled, fitted, and managed by the user without the need for audiological or computer support. This article details the self-fitting concept and its potential application in both developing and developed countries. Potential advantages and disadvantages of such a device are discussed, and considerations for further investigations into the concept are presented. Overall, the concept is considered technologically viable with the main challenges anticipated to be development of clear, simple user instructions and a delivery model that ensures reliable supplies of instant-fit ear tips and batteries.
Keywords: hearing aids, amplification, self-fitting, teleaudiology
Background
Of the 278 million people in the world with bilateral, moderate to profound hearing loss, two-thirds live in developing countries (WHO, 2004). Although there are no formally established criteria for the designation of countries as “developing,” the United Nations Conference on Trade and Development (UNCTAD) groups economically disadvantaged countries according to three categories, across which there is some overlap: least developed countries (LDC), small island developing states (SIDS), and land-locked developing countries (LLDC). Nations belonging to these categories are characterized by low per capita gross national income (GNI), high child mortality rates, low adult literacy rates, and political and economic instability (UN-OHRLLS, 2010). For the purposes of this article, we define a “developing country” as a nation that belongs to at least one of the above three categories. Based on this definition, such countries as Angola, Myanmar, and Haiti are considered developing countries.
Of those individuals in developing countries who have a permanent bilateral hearing loss of moderate degree or greater, approximately three-quarters have adult-onset hearing loss, the third leading cause of disability in the world (Smith, 2008). Most of the 186 million hearing-impaired people in developing countries could benefit from amplification, but current annual production and distribution of hearing aids is estimated to meet less than 3% of the need in this part of the world (WHO, 2004). One of the many barriers to accessing hearing aids in developing countries is cost. The World Health Organization (WHO) has established global guidelines for hearing aid affordability that vary according to each country’s per capita GNI, thus relating hearing aid expenditure to average household income. The WHO guidelines suggest that a single hearing aid should not exceed 3% of per capita GNI. For example, in a country with a per capita GNI of US$45,000, WHO guidelines stipulate that a hearing aid should cost approximately US$1,300, whereas in a developing country with a per capita GNI of US$550, the cost of the device should not exceed US$10 (Brouillette, 2008). Other researchers have stressed the requirement that devices for developing countries be made affordable to as many residents as possible (e.g., Bento & Penteado, 2010; Parving & Christensen, 2004).
Another barrier to hearing aid rehabilitation in developing countries is a deficit of skilled hearing health care professionals. In developing countries, the proportion of audiologists ranges from 1 per 500,000 to 1 per 6,250,000 people (Goulios & Patuzzi, 2008). Further, approximately 20% of the countries surveyed by Goulios and Patuzzi (2008), all of which had very low per capita GNI, reported having no audiologists at all. Currently, many developing countries receive hearing health care through local general practitioners and/or teachers of the deaf, as well as visiting aid agencies. However, many charitable organizations who visit developing countries do not leave behind a self-sustaining infrastructure. A case study reported in McPherson (2008) describes the occurrence of such a situation in The Gambia, an LDC in which an audiology clinic was established with the support of British and Scandinavian aid agencies. The clinic employed two trained staff members, both of whom subsequently left the area and caused the clinic’s closure after only a few years. Staff transience is a particular problem in the audiology field as there are more jobs than there are qualified people to fill them. Audiologists from developing countries, seeking to improve their own socioeconomic situation, will often migrate to fill positions in developed countries, thus creating chronic personnel shortages in their home country. Other contributors to the closure of the Gambian clinic included the high cost of purchasing equipment, a lack of local calibration and repair facilities, and the high cost of sending equipment overseas for these services (McPherson, 2008).
To address the significant shortage of clinical skills in developing countries, the viability of teleaudiology is being explored. Swanepoel et al. (2010) provides an excellent introduction to teleaudiology and the potential scope of its applications. Briefly, teleaudiology refers to the practice of audiology in which the clinician is situated remotely from the client and delivers services via information and communication technology, such as the telephone or internet. Teleaudiology has been successfully trialed for diagnostic testing (e.g., Choi et al., 2007; Krumm, Huffman, Dick, & Klich, 2008), hearing aid adjustment (e.g., Ferrari, 2006; Wesendahl, 2003), and counseling (e.g., Laplante-Levesque, Pichora-Fuller, & Gagne, 2006; Pearce, Ching, & Dillon, 2009). There is no doubt that technological advancement and the penetration of communication technologies into developing countries make teleaudiology a very viable strategy. Swanepoel et al. (2010), however, have pointed out that such potential complications as licensure, jurisdictional responsibility, certification, reimbursement, and quality control need to be addressed, as clinicians and clients could potentially be situated in different states or even in different countries. Further, the establishment of a teleaudiology network still requires resources, including specialized equipment and dedicated local staff to assist the client, obtain information, and/or to guide the process. The introduction of teleaudiology could also place undue burden on clinicians in developed countries, where staff shortages also exist, if they are tapped to provide remote services to clients in developing countries.
Even among individuals with hearing impairment in developed nations who have reliable access to hearing health care services, the majority do not acquire hearing aids. Only about one in five individuals with hearing impairment in the developed world have obtained hearing aids, a number that has not substantially changed in 30 years (Dillon, in press; Kochkin, 2005). The reasons for the low penetration rate are varied and include such factors as cost; the belief that existing devices do not perform well in noise; and the fact that the demand for audiological services, even in developed countries, can be greater than the ability of the profession to provide them (Swanepoel et al., 2010).
In addition, there are those hearing-impaired individuals who have reliable access to hearing health care services, but who wish to be in control of their own fitting process, without having to rely on an audiologist to program and adjust the settings of their hearing aids. A recent survey by Kochkin (2007) that focused on obstacles to obtaining a hearing aid listed the top five characteristics that would increase the likelihood that a currently unaided individual would seek out a hearing aid. Two of the five characteristics were lower cost and the ability to self-fit or self-adjust a hearing aid. Forty percent of those surveyed indicated that a discount of US$500 would encourage them to purchase hearing aids, whereas 19% reported that the ability to self-fit or self-adjust their hearing aids would increase the likelihood of a hearing aid purchase (Kochkin, 2007).
A Self-Fitting Hearing Aid
One possible solution for hearing-impaired individuals in both the developing and developed worlds is a “do-it-yourself” amplification device that can be fitted and managed entirely by the user, without the assistance of a hearing health care professional, the use of computer hardware, or access to a telephone or the internet. We refer to such a device as a “self-fitting” hearing aid. The concept of such a device is in the process of being evaluated at the National Acoustic Laboratories (NAL) in response to a growing global need for hearing health care services, particularly in developing nations and in remotely located, underserviced areas in developed countries.
The NAL vision of a self-fitting hearing aid is an amplification device that consists of a behind-the-ear (BTE) body and an instant-fit tip. The device contains a tone generator that may be activated either via an onboard button or with a remote control in order to start the process of an automated, in situ hearing threshold measurement. The same button is used by the hearing aid wearer to respond to the presented tones. An onboard prescriptive algorithm subsequently uses the measured thresholds as a basis for setting the hearing aid parameters (Figure 1). If the self-fitting hearing aid were equipped with a training algorithm and additional user controls, either on the device itself or on a remote control, the wearer would be able to further fine-tune the device in his or her everyday listening environments (Dillon et al., 2006). Briefly, we envision a training algorithm that concurrently collects and combines information about the acoustic characteristics of the user’s current environment and the user-selected settings in that environment. Over time, as sufficient data are accumulated, the hearing aid begins to anticipate the user’s preferred setting in a given listening environment and adjusts the hearing aid accordingly.
Figure 1.
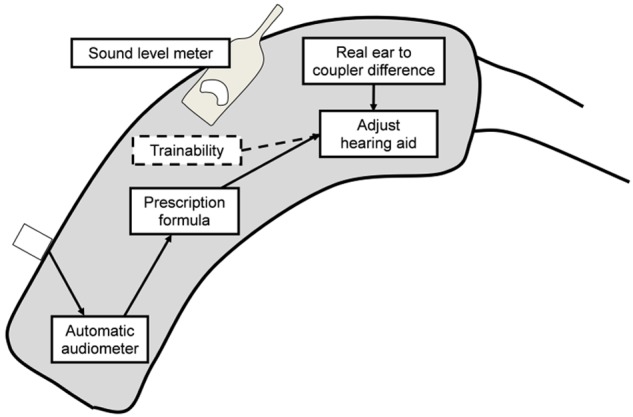
A model of the components of a self-fitting hearing aid
The concept of a self-fitting hearing aid is not new. In 1984, Köpke, Wiener, Maas, Eggert, and Götze patented the idea of a digital hearing aid that could present the user with internally generated tones in order to measure the user’s hearing thresholds, and then apply a transfer function to produce the prescribed hearing aid settings. This method of determining hearing aid settings very much describes the general concept of a self-fitting hearing aid. However, as far as we know, a device designed according to these principles has not yet been realized.
Whereas technological constraints may have prevented Köpke et al. and others of that era from realizing the kind of self-fitting hearing aid described in Figure 1, the prospect of producing a device that incorporates fully automated procedures for audiometric testing and hearing aid fitting is now very real. For example, many hearing aids are now equipped with tone generators (e.g. Intricon (2011), Widex, Siemens, and many others). These tone generators are primarily used to indicate changes to the volume level and program and as a low-battery indicator, although Widex (2011) makes use of this feature to provide harmonic tones that are designed to assist the user with relaxation and tinnitus relief (Kuk, Peeters, & Lau, 2010). The greater power and sophistication of digital hearing aid chipsets further make it feasible for the device to host a complex transfer function or prescriptive formula, and/or a training algorithm.
There are issues, however, that remain to be addressed before a self-fitting hearing aid is launched, some of which are explored and discussed in this issue of Trends in Amplification. For example, a factor that has yet to be investigated is the proportion of potential users who will be able to find an environment that is quiet enough for valid threshold measurements to be obtained. It may be possible for the device’s instructions to advise the user to move into a room or area in which no other sounds can be heard. Alternatively, the hearing aid microphone could be used to measure the ambient noise level, with a warning sound produced by the onboard tone generator whenever the masked thresholds are not better than the estimated masked threshold in that noise spectrum. The reliability and validity of in situ audiometric thresholds as measured with different styles of instant-fit tips are further discussed in Keidser et al. (2011) in this issue.
Commercial Alternatives
Currently, there are commercially available hearing aids that may be purchased and adjusted without visiting a hearing health care professional. Several of these devices could be considered “self-fitting” in that the wearer is in control of the fitting procedure. Additionally, a group of low-cost devices, produced specifically for the developing world, are currently available. Table 1 shows an overview of currently available hearing instruments that are distributed via nontraditional channels. The hearing aids summarized in the table can be broadly divided into two categories: (a) user-programmable devices, and (b) devices aimed specifically at clients in developing countries.
Table 1.
An overview of currently available hearing aids that are distributed through nontraditional channels
| Company | Website | Device characteristics | Price per device | User requirements |
|---|---|---|---|---|
| America Hears (2011) | http://www.americahears.com | digital; both custom and stock size products available | US$899-1,299 | computer, internet access, telephone, audiogram (optional: Virtual Office programming software, Freedom programming interface, and cables for self-programming; impressions for custom earmolds or shells) |
| Australia Hears (2011) | http://www.australiahears.com.au | digital; stock size products only | US$990-1,250 | computer, internet access (optional: audiogram; IHearYou programming software, AHPro3 programming interface, and cables for self-programming) |
| DIY Hearing Aids (2011) | http://www.diyhearingaids.com | digital; both custom and stock size products available | US$995-1,195 (optional: telecoil US$125, directional microphone US$125, custom earmold US$110) | computer, internet access, telephone, audiogram (optional: Virtual Technician programming software, eMini Tec programming interface, and cables for self-programming; impressions for custom earmolds or shells) |
| Godisa (2011) | http://www.godisa.org | digital; custom product only | unknown, but reportedly low cost | audiogram, impressions (optional: 2 cc coupler or real-ear measurement equipment) |
| HearSource (2011) | http://www.hearsource.com | digital; both custom and stock size products available | US$995 (optional: telecoil US$99, directional microphone US$99, custom earmold US$99) | computer, internet access, telephone, audiogram (optional: Virtual Technician programming software, eMini Tec programming interface, and cables for self-programming; impressions for custom earmolds or shells) |
| Solar Ear (2011) | http://www.solarear.com.br/solar | digital and analog; both custom and stock size products available | US$165-300; prices for some models unavailable | audiogram (optional: impressions for custom earmolds, 2 cc coupler or real-ear measurement equipment) |
User-Programmable Hearing Aids
The user-programmable devices, which include those sold by such companies as Australia Hears, America Hears, Hear Source, and DIY Hearing Aids, are digital hearing aids with such features as multichannel compression, adaptive feedback cancellation, and noise reduction and speech enhancement algorithms. Cost per device averages US$1,000, which is comparable to a low-cost traditionally fitted hearing aid.
In order to program and adjust the devices, a previous audiogram, a computer, internet access, fitting software, and/or a hardware interface between the computer and the hearing aids are required. The American companies (America Hears, Hear Source, and DIY Hearing Aids) require that the hearing aid candidate first contact a representative of the company for a telephone consultation. In order to comply with Food and Drug Administration (FDA) requirements, the candidate is required to submit an audiogram, a medical history and waiver form, and a Health Insurance Portability and Accountability Act (HIPAA) privacy policy form. America Hears runs an audiology center at which free hearing tests are offered; candidates who do not live near the center are advised to obtain a hearing test from a local audiologist. Hear Source and DIY Hearing Aids do not maintain brick-and-mortar hearing centers. Following the receipt of the necessary paperwork, the most appropriate hearing aid model is then chosen in consultation with the company representative. If a device requiring a custom earmold or shell is selected, the user must have ear impressions taken locally so the company can send them to the manufacturer. Ear impressions are not offered by any of the American companies discussed here. Hear Source and DIY Hearing Aids additionally offer a telephone appointment with a “coach” who can guide the user through the fine-tuning process and provide technical support. Due to the difference in Australian laws governing the provision of health-related products, Australian hearing aid candidates can order devices from Australia Hears with or without an audiogram. All devices purchased from these companies are delivered to the user preprogrammed. For those users who wish to undertake self-adjustments, fitting software, an interface box, and programming cables may be ordered in conjunction with the hearing aids. DIY Hearing Aids, America Hears, and Australia Hears charge an additional fee for these items.
The fitting software tends to be complex and sophisticated, resembling the fitting software used clinically by audiologists. For example, the fitting software offered by both Hear Source and DIY Hearing Aids includes an overall gain control with a 32 dB range, a 12-channel “equalizer” that allows gain adjustments at discrete frequencies from 0.2 kHz to 7.2 kHz, the ability to alter the compression threshold in four channels, a maximum power output (MPO) control, a slider to set the level of noise reduction, a toggle switch to activate or disable a feedback cancellation algorithm, and a choice of four microphone modes or input types (omnidirectional microphone, directional microphone, telecoil, direct audio input). Users can choose to implement any combination of these features in two programs. In the software, the hearing aid settings may be viewed as a gain curve or as an input/output function. Short tutorial videos that explain how to use many of the software functions are freely available on both websites and can also be found on YouTube. Both the software and the tutorials use such “clinical” vocabulary as frequency, intensity, decibel, and steady-state noise, which cannot be expected to be readily understood by the general population. In contrast, the IHearYou software offered by Australia Hears tends to be aimed more at troubleshooting problems that the user is experiencing in specific listening situations. For example, one screen asks the user to evaluate the quality of speech in background noise from a list of descriptors that include “clear,” “hollow or echoing,” and “muffled or dull.” On selecting an answer, the software presumably implements the corresponding changes to the gain/frequency response, compression parameters, and/or noise reduction algorithm.
Devices for Developing Countries
Devices geared to the developing world are currently produced and sold by Godisa and Solar Ear. Godisa is a charitable organization based in Botswana that produces and distributes several models of low-cost BTE hearing aids and a solar-powered battery recharger that is designed to accept a range of battery sizes (Brouillette, 2008; Godisa, 2011). Similarly, Solar Ear, located in Brazil, manufactures and distributes a range of analog and digital hearing aids, a solar-powered battery charger, and low-cost, long-life rechargeable hearing aid batteries (Solar Ear, 2011). The three digital hearing aid models offered by Solar Ear, which include two BTEs and one receiver-in-canal (RIC) device, feature two-channel wide dynamic range compression (WDRC) and a low-battery warning. The two BTE hearing aids, both for individuals with severe to profound hearing loss, also have telecoils, volume controls, and trimpots that allow alteration of MPO and high- and low-frequency gain. Specific information about Godisa devices could not be obtained as emails to the organization went unanswered. As of the date of the publication of this article, their website is no longer online.
As a secondary goal of these organizations is to provide meaningful employment for individuals who are deaf, these devices are assembled by members of the local deaf community. The technology is basic and adjustments to the devices’ settings, which may be made to achieve a match to a prescriptive target or to the user’s preferred level, are effected via screwdriver-adjustable trimpots. The method of device distribution is not clear, but it is likely that Godisa and Solar Ear hearing aids are fitted by local health personnel and/or audiologists associated with visiting aid agencies. None of these devices are designed to be self-adjusted by the wearer.
Other Nontraditional Hearing Aids
Figure 2 shows the two categories described above, as well as two other related device categories: (a) over-the-internet (OTI) hearing aids and (b) personal amplifiers. Although all currently available user-programmable hearing aids fall under the rubric of OTI devices, not all OTI devices are user programmable. The majority of OTI hearing aids are preprogrammed by the manufacturer or distributor according to a user-supplied audiogram before being dispensed by mail. As these devices require an audiogram for programming, the hearing aid candidate still needs to visit a hearing health care professional to obtain a hearing test. Personal amplifiers, some of which are available OTI, are similar to hearing aids in that they provide some degree of amplification. However, any adjustments that may be made to their gain/output are not frequency-specific, and thus these devices cannot be matched to the user’s individual audiometric thresholds. Their manufacture and sale are often not controlled by government regulatory bodies, and as such, do not meet sufficient quality and safety standards to be marketed as hearing aids or medical devices. Callaway and Punch (2008) subjected 11 low- and mid-range over-the-counter (OTC) hearing devices, all of which are available OTI, to a battery of electroacoustic tests. These tests included measurements of full-on gain, total harmonic distortion, equivalent input noise (EIN), frequency range, battery life, and the presence of high-frequency peaks. The suitability of each device for three audiometric configurations relative to the National Acoustic Laboratories-Revised (NAL-R; Byrne & Dillon, 1986) prescriptive formula was also investigated. The results showed that the low-range devices were inadequate, with high levels of EIN, little to no high-frequency gain, peaky frequency responses, and high battery drain displayed by some or all of the devices. The potential for these devices to damage users’ residual hearing due to the high output levels measured in the low-range devices was also highlighted by the authors.
Figure 2.
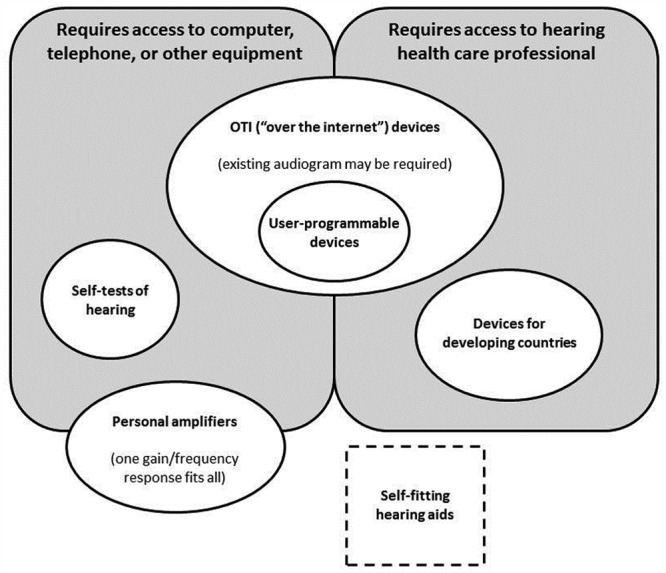
Unlike a self-fitting hearing aid, which is designed to be entirely self-contained, all currently available nontraditional hearing aids and self-tests of hearing require either additional equipment and/or access to a hearing health care professional
The fifth and final category shown in Figure 2 encompasses self-tests of hearing. Currently, all self-tests of hearing are computer-, telephone-, and/or questionnaire-based. None of these test methods provides the person being tested with reliable, frequency-specific thresholds to which a validated prescriptive algorithm can be applied to yield hearing aid settings. There are currently no self-tests of hearing available in a hearing aid or other wearable device that does not require the attachment of an additional programming unit (e.g., Ludvigsen & Topholm, 1997), or a computer.
The self-fitting hearing aid concept under investigation at NAL is designed to incorporate aspects of three categories described in Figure 2 into a single device: (a) a self-test of the user’s hearing, (b) user programmability, and (c) suitability for developing countries. Consequently, the self-fitting hearing aid concept currently being explored at NAL aims to be a unique solution that can be fitted and managed entirely by the user, without the need for access to a hearing health care professional or additional equipment.
Potential Advantages and Disadvantages
As with any new invention, there are both possible benefits and drawbacks to the introduction of a self-fitting hearing aid into the market. An anticipated advantage of a self-fitting hearing aid is the expected lower financial cost. As discussed earlier in this article, the price of a hearing aid in a developing country is often prohibitively expensive relative to average household income (Brouillette, 2008). In the case of a self-fitting hearing aid, the lack of need for a professional hearing health care provider, as well as the reduced need for travel to and from the clinic, is likely to represent a significant cost savings for the user. This advantage could also be attractive to hearing aid candidates in developed countries.
If trainability is an incorporated feature in the self-fitting device, the ability of the user to undertake the fine-tuning process in response to real-world listening situations could be an advantage. Hearing aid fittings and subsequent fine-tuning adjustments are traditionally conducted in a quiet room with a single sound source and little to no background noise, an acoustic environment that differs markedly to the average user’s everyday listening situations. Although it is important to ensure that the hearing aid operates appropriately in this kind of “best case” environment, users may not necessarily find the initial setting preferable as they step out of the clinic and into a busy street. To rectify this problem, some proprietary fitting software packages include a comprehensive library of sounds, accompanied by still pictures or virtual scenes, that replicate everyday listening situations (e.g., Howes & Olson, 2006; Meskan & Robinson, 2000). At present, however, there are limitations to the degree to which an acoustic environment can be accurately reproduced, especially when constrained by the limited number of loudspeakers typically found in an audiology clinic (Guastavino, Katz, Polack, Levitin, & Dubois, 2005). Additionally, the unique range of the user’s most commonly encountered listening situations may not be adequately represented among the sound library. In contrast, a self-fitting hearing aid would allow users to fine-tune and personalize their settings in response to their own individual listening environments.
A further anticipated advantage of a self-fitting and/or trainable hearing aid is the increased feeling of psychological ownership that such a device is expected to confer on the user. The concept of psychological ownership refers to the internalized feelings of possession we have toward other entities or “targets,” which may include objects, ideas, or even other people. Individuals incorporate ownership targets into their own self-identity, using them to help define who they are (Pierce, Kostova, & Dirks, 2003). Although psychological ownership has not been widely researched in relation to health care, Karnilowicz (2010) argues that the concept can usefully be extended to include chronic health conditions and their associated treatments. For example, an individual may feel a sense of ownership toward his or her hearing loss and hearing aids, and therefore that they constitute part of his or her identity.
Psychological ownership and self-identity are intrinsically bound up with the notion of control. Pierce et al. (2003) state that the strength of psychological ownership (and, hence, the extent to which it is integrated into the individual’s self-identity) is strongly influenced by the degree of control the individual is able to exercise over his or her ownership targets. In the context of current research into management of chronic health conditions, this is very much in line with the wealth of studies demonstrating that the role of the patient as an active collaborator in, rather than the passive recipient of, the treatment of his or her own chronic health condition leads to improved adherence and better outcomes (e.g., Gardetto, 2011; Kralik, Koch, Price, & Howard, 2004; Mayor, 2006).
Control over one’s ownership targets is influenced by a range of factors, the most important of which is self-creation (Pierce et al., 2003). That is, individuals will experience a greater sense of ownership of, and control over, something they invest in creating themselves. This will arguably be the case for users of a self-fitting hearing aid, as unlike a hearing aid fitted by a professional, the device requires a substantial investment of effort and time by the end user. This advantage may apply more to users in developed countries who are able to choose a self-fitting hearing aid from a range of hearing health care options, as opposed to those in the developing world whose choices are limited or nonexistent.
Depending on one’s perspective, the fact that a self-fitting hearing aid does not require direct input from a hearing health care professional may be seen either as an advantage or a disadvantage. From the point of view of some end users, this freedom may be viewed as an advantage. Elberling and Hansen (1999) have suggested that three conditions must be met in order for a traditional hearing aid to be successfully fine-tuned: (a) a clear description of the problem by the user, (b) correct interpretation of the problem by the hearing health care professional, and (c) the translation of the problem into appropriate changes to the hearing aid’s electroacoustic characteristics. Even if only one of these conditions is not fulfilled, the fine-tuning process is unlikely to yield the preferred response. Although key words associated with specific auditory percepts have been identified (Nelson, 2001) and flow charts have been developed to aid the hearing health care professional in interpreting a client’s complaints (Kuk, 1999), the second and third conditions remain difficult to meet in all cases. A self-fitting hearing aid, however, allows users to act directly on and experiment with their own settings, without relying on their ability to translate perceptions into words or a professional’s ability to translate words into adjustments.
A potential disadvantage of a self-fitting hearing aid is the risk of an audiologically inappropriate fitting. Identifying the presence of a conductive or mixed hearing loss is a critical step prior to hearing aid fitting, as many pathologies of the outer or middle ear can be treated medically or should be investigated prior to fitting with amplification (Silman & Silverman, 1997). In the lead-up to a traditional hearing aid fitting, such contraindications are often able to be discerned through a combination of otoscopy and audiometry. For example, impacted wax in the ear canal can be detected with an otoscope, whereas air- and bone-conduction thresholds on the audiogram will distinguish between sensorineural and conductive sites of lesion. In the case of the self-fitting hearing aid, however, otoscopy cannot be performed, as a person cannot easily look into one’s own ear canal. Such other contraindications to a hearing aid fitting as a sudden or rapidly progressing hearing loss, otalgia, a physical malformation of the ear, or active infection may also, if overlooked, result in poor fitting outcomes for the user. Other issues that may arise after the fitting include the selection of inappropriately high levels of gain and output, which may lead to temporary or permanent threshold shift, particularly among users with severe and profound hearing loss (Macrae, 1991). The safety of a self-fitting hearing aid will depend on how well the device can identify the presence of conductive and asymmetrical hearing losses, and how accurately it is able to measure hearing thresholds and to prescribe an appropriate gain/frequency response, compression parameters, and MPO. Such issues require further investigation.
The threat that the self-fitting hearing aid could pose to the livelihood of hearing health care professionals depends, in developed countries, on the extent to which the device is taken up by existing hearing aid users versus individuals who are currently unaided. If the former situation occurs, then the impact on the profession will depend on the overall supply and demand for audiological services. It is important to recognize, however, that many people will continue to need considerable assistance from clinicians for diagnosis, motivational counseling, and/or instructional counseling in device usage and listening tactics. Although the candidacy criteria for a self-fitting hearing aid are unknown at present, infants, young children, and individuals with cognitive and/or fine motor difficulties are examples of groups who are unlikely to be suitable candidates for a self-fitting device. Such populations will continue to require direct clinical interaction with a hearing health care professional.
Practical issues that may present a challenge include finding a suitable instant-fit ear tip and ensuring a reliable battery supply to users of the self-fitting hearing aid. Instant-fit tips (and even custom-made earmolds) have a shorter lifespan than the amplification devices to which they are attached. Although extra tips could be provided with the self-fitting hearing aid, a long-term solution is needed that will allow users in remote and developing parts of the world to access affordable replacement tips. A similar problem exists for batteries. Rechargeable and solar-powered batteries are an obvious solution, and are currently being produced by such organizations as Solar Ear. However, even these products have a limited lifespan. Electrically powered battery chargers would not suit populations living without electricity, while solar-powered devices would be impractical for those dwelling in areas with little daylight for several months of the year. If the self-fitting hearing aid is to be realized, a carefully thought-out distribution model is required to ensure that those who obtain the device can continue to use it. In developing countries, it is also critical that those individuals with severe hearing loss, for whom instant-fit tips may not be suitable due to their high gain requirements, are catered for through the provision of suitable custom earmolds.
Considerations for Future Investigations
As pointed out earlier in this article, the self-fitting hearing aid concept relies on the capability of the device to achieve reliable and valid in situ thresholds using an automated procedure that is fully administered by the hearing aid user. Several studies have demonstrated that automated audiometry is as reliable and valid as manual audiometry (e.g., Margolis, Glasberg, Creeke, & Moore, 2010; Ho, Hildreth, & Lindsey, 2009), and a recent study also proved the reliability and validity of in situ audiometry, provided that transducer-specific real-ear-to-dial difference (REDD) values are applied to the threshold measurements to compensate for low-frequency leakage (O’Brien, Keidser, Yeend, Hartley, & Dillon, 2010). These studies are reviewed in more detail in an accompanying article (Keidser et al., in press), which also addresses such issues as the detection of asymmetry and conductive loss, two possible contraindications to a conventional hearing aid fitting. To our knowledge, there exists no hearing aid with an onboard tone generator that can be activated by the user to complete an audiometric test. When a device with such a feature becomes available, the ability of a layperson to follow and understand a set of instructions to complete automated audiometry, and the reliability and validity of the resulting measurements, will need to be verified. Such research could include investigations into the levels of ambient noise in the environments that users of the device typically select for performing audiometric testing.
Unless it is possible to design a one-size-fits-all device, a candidate for the self-fitting hearing aid will likely need to assemble several hearing aid components prior to performing automated in situ audiometry. Specifically, we expect that the user will need to select appropriate tube and instant-fit tip sizes from a range of different sizes, connect them to the body of a hearing aid, insert a battery into the assembled device, and learn how to insert the aid into the ear. In a conventional hearing aid fitting, such tasks are left to the hearing aid provider, who also has experience in determining whether the aid fits well in the person’s ear. Again, a successful outcome here is likely to depend on the instructions provided. This aspect has been explored in a group of older, urban-dwelling, hearing-impaired adults living in a developed country (Australia), and the results are presented in an accompanying article (Convery et al., 2011b). The study found that health literacy, or the ability to read and understand health-related text, was an important predictor of the outcome, with participants who had a higher level of health literacy better able to complete the tasks accurately and independently. This result clearly points toward the importance of supplying simple instructions with the self-fitting hearing aid. Another accompanying article in this issue (Caposecco et al., 2011) explains how health literacy differs from general literacy, and presents and discusses the steps involved in developing written health care material using best practice design principles. The steps are further illustrated through the development of the instructions for assembling and inserting a hearing aid that were used in the Convery et al. (2011b) study. From these investigations, it becomes clear that future studies must focus on devising clear instructions for how to assemble, self-fit, and fine-tune the hearing aid.
We believe that the primary market for the self-fitting hearing aid should be developing countries that lack an audiological infrastructure. Therefore, when developing instructions for use of the device, the high rate of illiteracy in such areas should be considered and the efficacy of the instructions verified in the target population. More information about the disadvantages currently faced by hearing-impaired people living in developing countries and how innovative technology could make a difference in these areas are discussed in an accompanying article by McPherson (in press). In this article, McPherson highlights the lack of research into how to match amplification technology with the need in developing countries for affordable and appropriate devices.
Perception of the self-fitting concept has been gauged among urban-dwelling, hearing-impaired adults in a developed country (Convery et al., 2011a). Overall, perception of the concept among this population sample was positive. Interestingly, although self-adjustment, convenience, and independence were the most cited advantages, the most cited disadvantage was a personal preference for professional guidance. This outcome was measured in a population that has a choice of hearing health care services, and is not likely to be directly applicable to hearing-impaired individuals in a developing country. It would therefore be beneficial to survey residents of a developing country to determine whether the self-fitting hearing aid is an appropriate and desirable solution, or whether this population would prefer an investment in building local centers at which hearing services are provided, either by trained professionals or through the use of teleaudiology.
Before a self-fitting hearing aid could be made available in either developing or developed countries, a thorough evaluation must be performed to establish that the outcome of using a self-fitting hearing aid is at least as good as the outcome achieved with a professional hearing aid fitting. On a somewhat related topic, Wong (in press) looks at the current research on three elements related to a self-fitting hearing aid and reviews them using evidence-based principles: the performance of in situ threshold measurements, the ability of hearing aid users to reliably select their preferred responses in different listening environments and associated outcomes, and the ability of older adults to assemble and use a hearing aid. None of these research questions were answered with high quality evidence and some specific questions have yet to be addressed, suggesting that there is scope for more investigations in all three areas.
Summary
This article introduced the concept of a “do-it-yourself” amplification device that requires no access to further instrumentation and that can be managed, fitted, and fine-tuned entirely by the user, either independently or with the assistance of another layperson. Such a device would offer people who live in developing countries and in geographically remote areas increased access to hearing rehabilitation. We further argue that a proportion of hearing-impaired people who already have reliable access to audiological services, but who wish to play a greater role in the fitting and fine-tuning process, could also benefit from the availability of such a device. The anticipated advantages of a self-fitting hearing aid include the expected lower cost of such a device, the ability to fine-tune the device’s settings in response to real-world listening situations, an increased sense of psychological ownership, and the freedom from dependence on a hearing health care professional, while the possible disadvantages include the risk of an audiologically inappropriate fitting, the risk of aid-induced hearing loss if excessively high gain and output levels are selected, and the high level of cognitive functioning that is likely to be required to carry out the self-fitting procedure. The distribution model of a self-fitting hearing aid, with a particular focus on the supply of replacement instant-fit tips and batteries, presents a challenge that must be carefully addressed.
Footnotes
Authors’ Note: Portions of this article were presented at the 30th International Congress of Audiology in São Paulo, Brazil, April 2010.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed the receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for this study was provided by the HEARing Cooperative Research Centre, Melbourne, Australia.
References
- America Hears. (2011). Programming and adjustment options. Retrieved from http://www.americahears.com/Products/VirtualOffice.shtml
- Australia Hears. (2011). Our hearing aid prices and accessories. Retrieved from https://www.australiahears.com.au/Online-Store.aspx
- Bento R., Penteado S. (2010). Designing of a digital behind-the-ear hearing aid to meet the World Health Organization requirements. Trends in Amplification, 14, 64-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouillette R. (2008). Rehabilitation of hearing loss: challenges and opportunities in developing countries. In McPherson B., Brouillette R. (Eds.), Audiology in developing countries (pp. 141-154). New York, NY: Nova Science [Google Scholar]
- Byrne D., Dillon H. (1986). The National Acoustic Laboratories’ new procedure for selecting the gain and frequency response of a hearing aid. Ear and Hearing, 7, 257-265 [DOI] [PubMed] [Google Scholar]
- Callaway S. L., Punch J. L. (2008). An electroacoustic analysis of over-the-counter hearing aids. American Journal of Audiology, 17, 14-24 [DOI] [PubMed] [Google Scholar]
- Caposecco A., Hickson L., Meyer C. (2011). Assembly and insertion of a self-fitting hearing aid: Design of effective instruction materials. Trends in Amplification, 15 (4), 184-195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J., Lee H., Park C., Oh S., Park K. (2007). PC based tele-audiometry. Telemedicine and eHealth, 13(5), 501-508 [DOI] [PubMed] [Google Scholar]
- Convery E., Keidser G., Hartley L. (2011a). Perception of a self-fitting hearing aid among urban-dwelling hearing-impaired adults in a developed country. Trends in Amplification, 15 (4), 175-183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Convery E., Keidser G., Hartley L., Caposecco A., Hickson L., Meyer C. (2011b). Management of Hearing Aid Assembly by Urban-Dwelling Hearing-Impaired Adults in a Developed Country: Implications for a Self-Fitting Hearing Aid. Trends in Amplification, 15(4), 196-208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon H. (in press). Hearing aids (2nd ed.). Sydney, Australia: Boomerang Press [Google Scholar]
- Dillon H., Zakis J. A., McDermott H., Keidser G., Dreschler W., Convery E. (2006). The trainable hearing aid: what will it do for clients and clinicians? Hearing Journal, 59, 30-36 [Google Scholar]
- DIY Hearing Aids. (2011). Hearing aid product list and order page. Retrieved from http://www.diyhearingaids.com/digital-hearing-aid-products
- Elberling C., Hansen K. V. (1999). Hearing instruments: interaction with user preference. In Rasmussen A. N., Osterhammel P. A., Andersen T., Poulsen T. (Eds.), Auditory models and non-linear hearing instruments. Proceedings of the18th Danavox Symposium (pp 341-357). Copenhagen, Denmark: Holmens Trykkeri [Google Scholar]
- Ferrari D. V. (2005). Remote programming and verification as a mean to improve quality of hearing and fitting. In Rasmussen A. N., Poulsen T., Andersen T., Larsen C. B. (Eds.) Hearing aid fitting. Proceedings of the 21st Danavox Symposium (pp 531-543). Aalborg, Denmark: Centertryk [Google Scholar]
- Gardetto N. J. (2011). Self-management in heart failure: Where have we been and where should we go? Journal of Multidisciplinary Healthcare, 4, 39-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godisa. (2011). About Godisa: Technologies for the developing world. Retrieved from http://www.godisa.org/about.html
- Goulios H., Patuzzi R. (2008). Education and practice of audiology internationally: Affordable and sustainable education models for developing countries. In McPherson B., Brouillette R. (Eds.), Audiology in developing countries (pp. 51-74). New York, NY: Nova Science [Google Scholar]
- Guastavino C., Katz B. F. G., Polack J. D., Levitin D. J., Dubois D. (2005). Ecological validity of soundscape reproduction. Acustica, 91, 333-341 [Google Scholar]
- HearSource. (2011). Hearing aid programming. Retrieved from http://www.hearsource.com/hearing_aid_software.html
- Ho A. T. P., Hildreth A. J., Lindsey L. (2009). Computer-based audiometry versus manual audiometry. Otology & Neurotology, 30, 876-883 [DOI] [PubMed] [Google Scholar]
- Howes C., Olson L. (2006). The role of virtual reality in hearing instrument fittings. Hearing Review, 13(5), 60-63 [Google Scholar]
- Intricon. (2011). The all-new Overtus™. Retrieved from http://intricon.com/products/hearing-health/digital-amplifiers/overtus/
- Karnilowicz B. (2011). Identity and psychological ownership in chronic illness and disease state. European Journal of Cancer Care, 20, 276-282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keidser G., Dillon H., Zhou D., O’Brien A., Carter L., Yeend I., Hartley L. (in press). Expected reliability and validity of thresholds measured automated and in situ. Trends in Amplification
- Kochkin S. (2005). MarkeTrak VII: Consumer satisfaction with hearing instruments in the digital age. Hearing Journal, 58, 30-43 [Google Scholar]
- Kochkin S. (2007). MarkeTrak VII: Obstacles to adult non-user adoption of hearing aids. Hearing Journal, 60, 24-51 [Google Scholar]
- Köpke W., Wiener P., Maas R., Eggert A., Götze G. W. (1984). Digital hearing aid and method. U.S. Patent No. 4,471,171 September 11, 1984
- Kralik D., Koch T., Price K., Howard N. (2004). Chronic illness self-management: taking action to create order. Journal of Clinical Nursing, 13, 259-267 [DOI] [PubMed] [Google Scholar]
- Krumm M., Huffman T., Dick K., Klich R. (2008). Telemedicine for audiology screening of infants. Journal of Telemedicine and Telecare, 14, 102-104 [DOI] [PubMed] [Google Scholar]
- Kuk F. K. (1999). How flow charts can help you troubleshoot hearing aid problems. Hearing Journal, 52, 46, 48,-49, 52 [Google Scholar]
- Kuk F., Peeters H., Lau C. (2010). The efficacy of fractal music employed in hearing aids for tinnitus management. Hearing Review, 17(10), 32-42 [Google Scholar]
- Laplante-Levesque A., Pichora-Fuller K. M., Gagne J. P. (2006). Providing an internet-based audiological counselling programme to new hearing aid users: A qualitative study. International Journal of Audiology, 45, 697-706 [DOI] [PubMed] [Google Scholar]
- Ludvigsen C., Topholm J. (1997). Fitting a wide range compression hearing instrument using real ear threshold data: a new strategy. High Performance Hearing Solutions, 2, 37-39 [Google Scholar]
- Macrae J. (1991). Prediction of deterioration in hearing due to hearing aid use. Journal of Speech and Hearing Research, 34, 661-670 [DOI] [PubMed] [Google Scholar]
- Margolis R. H., Glasberg B. R., Creeke S., Moore B. C. J. (2010). AMTAS®: Automated method for testing auditory sensitivity: Validation studies. International Journal of Audiology, 49(3), 185-194 [DOI] [PubMed] [Google Scholar]
- Mayor V. (2006). Long-term conditions. 3: Being an expert patient. British Journal of Community Nursing, 11, 59-63 [DOI] [PubMed] [Google Scholar]
- McPherson B. (2008). Audiology: a developing country context. In McPherson B., Brouillette R. (Eds.), Audiology in developing countries (pp. 5-20). New York, NY: Nova Science [Google Scholar]
- McPherson B. (2011). Innovative technology in hearing instruments: Matching needs in the developing world. Trends in Amplification, 15(4), 209-1214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meskan M. E., Robinson J. L. (2000). A patient-focused approach to fitting hearing instruments. Hearing Review, 7(12), 52-55 [Google Scholar]
- Nelson J. A. (2001). Fine tuning multi-channel compression hearing instruments. Hearing Review, 8, 30, 32,, 34,-35, 58 [Google Scholar]
- O’Brien A., Keidser G., Yeend I., Hartley L., Dillon H. (2010). Validity and reliability of in situ air conduction thresholds measured through hearing aids coupled to closed and open instant-fit tips. International Journal of Audiology, 49, 868-876 [DOI] [PubMed] [Google Scholar]
- Parving A., Christensen B. (2004). Clinical trial of a low-cost, solar-powered hearing aid. Acta Oto-Laryngologica, 124, 416-429 [DOI] [PubMed] [Google Scholar]
- Pearce W., Ching T. Y. C., Dillon H. (2009). A pilot investigation into the provision of hearing services using tele-audiology to remote areas. Australian and New Zealand Journal of Audiology, 31(2), 96-100 [Google Scholar]
- Pierce J. L., Kostova T., Dirks K. T. (2003). The state of psychological ownership: Integrating and extending a century of research. Review of General Psychology, 7, 84-107 [Google Scholar]
- Silman S., Silverman C. A. (1997). Auditory diagnosis: Principles and applications. San Diego, CA: Singular [Google Scholar]
- Smith A. W. (2008). Demographics of hearing loss in developing countries. In McPherson B., Brouillette R. (Eds.), Audiology in developing countries (pp. 21-50). New York, NY: Nova Science [Google Scholar]
- Solar Ear. (2011). Welcome to solar ear: The problem, the solution, the impact. Retrieved from http://www.solarear.com.br/solar/
- Swanepoel D., Clark J. L., Koekemoer D., Hall J. W., Krumm M., Ferrari D., McPherson B., Olusanya B., Mars M., Barajas J. (2010). Telehealth in audiology: The need and potential to reach underserved communities. International Journal of Audiology, 49, 195-202 [DOI] [PubMed] [Google Scholar]
- United Nations Office of the High Representative for the Least Developed Countries, Landlocked Developing Countries, and the Small Island Developing States. (2011). About LDCs, LLDCs, and SIDS. Retrieved from http://www.unohrlls.org/
- Wesendahl T. (2003). Hearing aid fitting: Application of telemedicine in audiology. International Tinnitus Journal, 9(1), 56-58 [PubMed] [Google Scholar]
- Widex. (2011). Mind440 key features. Retrieved from http://www.widex.pro/en/products/series/clear440/
- Wong L. L. N. (2011). Evidence on self-fitting hearing aids. Trends in Amplification, 15(4), 215-225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2004). Guidelines for hearing aids and services for developing countries (2nd ed.). Geneva, Switzerland: World Health Organization; Retrieved from www.who.int/pbd/deafness/en/hearing_aid_guide_en.pdf [Google Scholar]