Abstract
Brugada syndrome is a genetically determined familial disease with autosomal dominant transmission and variable penetrance, conferring a predisposition to sudden cardiac death due to ventricular arrhythmias. The syndrome is characterized by a typical electrocardiographic pattern in the right precordial leads. This article will focus on the new electrocardiographic features recently agreed on by expert consensus helping to identify this infequent electrocardiographic pattern.
Keywords: Brugada syndrome, sudden death, ST-segment elevation, r' in lead V1.
INTRODUCTION
Brugada syndrome (BrS) [1] is a genetically determined familial disease with autosomal dominant transmission and variable penetrance. More than 70 genetic mutations related to sodium channels have been described, with the SCN5A gene involved in 20% of cases [2] BrS is highly prevalent in young men that die suddenly without apparent structural cardiac abnormalities, although the latter concept has recently been challenged [3]. Syncope or sudden death often occurs during rest or sleep, and is usually due to polymorphic ventricular tachycardia which leads to ventricular fibrillation.
Based on new data that have emerged since 2005, a group of experts on BrS has recently produced a consensus document outlining a number of new electrocardiographic (ECG) features to better identify the best ECG patterns (Br P) and allow its differential diagnosis from other ECG patterns which may also show ST elevation and/or r'-wave in leads V1-V2. The new consensus document, published in September 2012 [4] contains a series of interesting novelties which are described below, and that help to perform the differential diagnosis between BrS, with special emphasis in type-2 Br P, and healthy athletes, pectus excavatum, arrhythmogenic right ventricular dysplasia and incomplete right bundle branch block (RBBB).
TYPE-1 BRUGADA PATTERN – NEW DESCRIPTION DETAILS RECORDED IN THE RIGHT PRECORDIAL LEADS
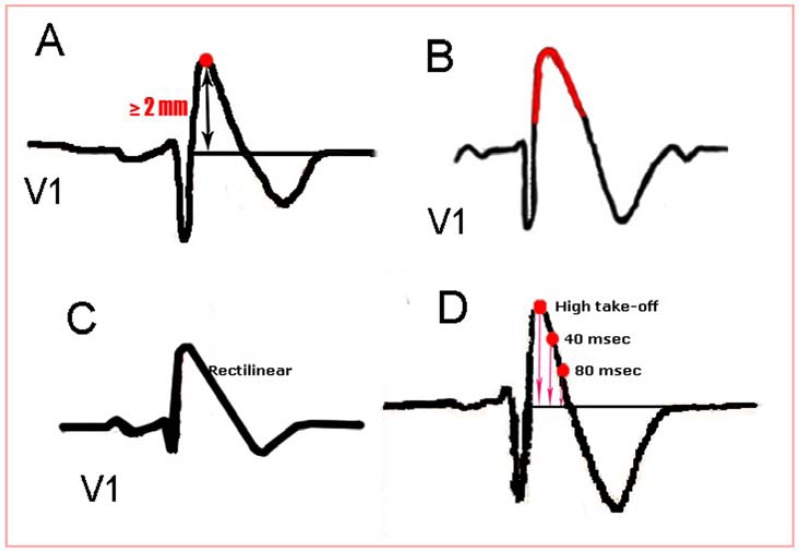
Type 1 Br P remains identical to that described in previous consensus documents [5-6], but with some new details that are helpful for its identification (Fig. 1):
Fig. (1).
(A) The high take-off (highest point) of QRS-ST is 2mm above the isoelectric line in most cases. (B) ST-segment morphology, as in previous consensus documents, is coved or concave, but (C) may occasionally be rectilinear. (D) ST-segment morphology shows progressive decline, so the high take-off of the QRS-ST is always higher than 40 ms later and this in turn is higher than after 80 ms.
• The high take-off or highest point of the QRS-ST is at least 2 mm high (Fig. 2A) in lead V1. In a few cases where this is less than 2 mm but greater than 1 mm [7], the pattern is only suggestive and not diagnostic of BrS.
Fig. (2).
(A) The J point may coincide with the highest point of the QRS-ST. (B) Postema found that the J point may appear after the highest point of the QRS-ST.
• ST-segment morphology is described as concave (coved) (Fig. 1B) with respect to baseline but may be, in a few cases, rectilinear (Fig. 1C), followed in either case by negative symmetrical T-wave.
• ST-segment morphology shows progressive decline, so the high take-off of the QRS-ST is always higher than 40 msec later and this in turn is higher than after 80 msec. (Fig. 1D).
• ST-segment descent after the QRS peak is slow (less than 0.4 mV at 40 ms) [7] in contrast to that observed in patients with RBBB where the descent is more pronounced.
• The ratio between the peak height of QRS-ST/peak of ST-segment after 80 ms is greater than 1 in BrS and less than 1 in athletes according to the Corrado index [8]. This author considers that the J point coincides with the peak of QRS-ST. However this is not necessarily true in all cases (Fig. 2) [9-10]. Nevertheless this index is still valid for differential diagnosis.
• The duration of the QRS in leads V1-V2 is greater than in the middle and left precordial leads, although this is sometimes difficult to determine (“Mismatch concept”).
• Type-1 Br P may be seen in a single lead, V1 or V2, but never exclusively in V3 [11].
• Complete RBBB and type-1 Br P are characterized by the presence of positive terminal deflections of the QRS and negative T-waves in leads V1-V2, respectively. However, unlike in BrS, ST-segment in RBBB is not elevated and is accompanied by an S-wave in leads I and V6, with a wider QRS (≥ 120 ms). By contrast, in BrS there is no wide S-wave in left precordial leads.
TYPE-2 BRUGADA PATTERN
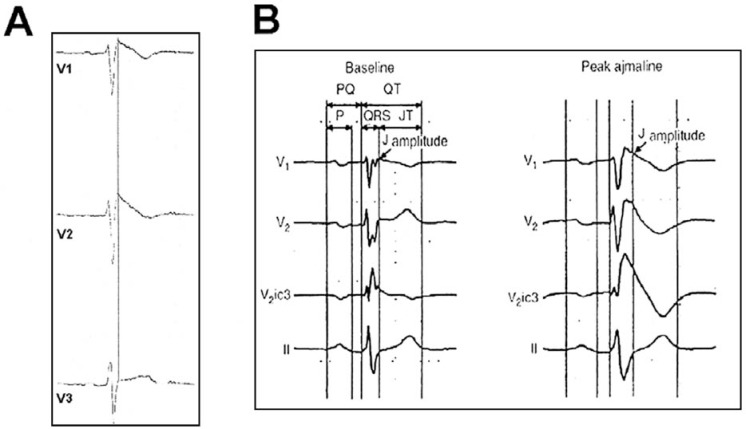
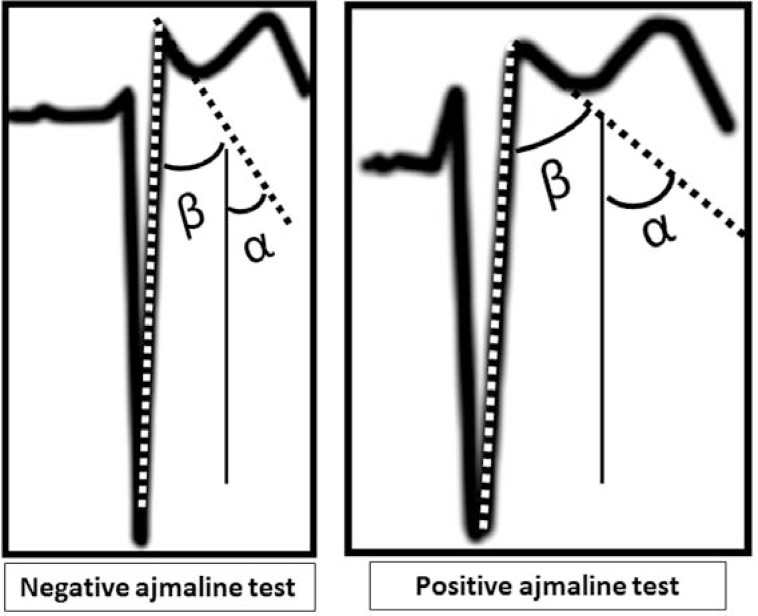
Given the minimal morphological differences between types-2 and 3 Br P as described in previous consensus documents [5-6] and the lack of impact on prognosis and risk stratification, the new type-2 ECG pattern definition includes both the old types-2 and 3 patterns (Figs. 3, 4):
Fig. (3).
The α and β angles described by Chevalier for RBBB and BrS.
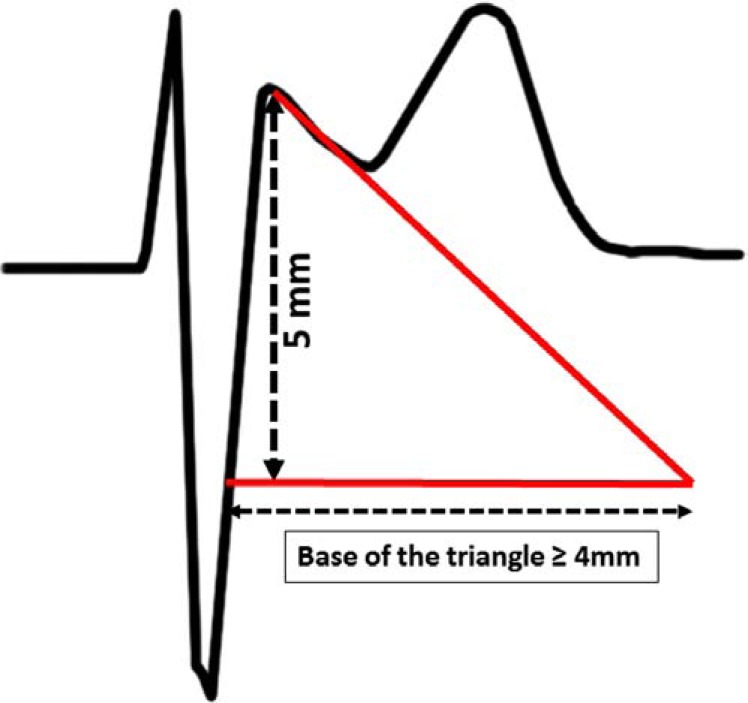
Fig. (4).
The base of the triangle longer than 4 mm in BrS is also useful to distinguish between the two BrS and healthy athletes.
• In type-2 Br P, a true r’-wave can be identified in leads V1-V2 at a height of 0.2 mV followed by ST-segment elevation ≥ 0.5 mm with respect to the isoelectric line, followed by T-wave usually in lead V2 with saddle back morphology. T-wave morphology in lead V1 is variable.
The consensus document also elaborates on differences in the r'-wave seen in the ECG of patients with BrS as compared to those with incomplete RBBB, healthy athletes, arrhythmogenic right ventricular dysplasia and pectus excavatum:
• In BrS the r’-wave is broad, rounded and generally of low voltage, with a slow descent. In contrast, that of incomplete RBBB is pointed. The QRS duration in leads V1-V2 is the same as in lead V6 in incomplete RBBB, as occurs in athletes who may also present with this pattern, whereas in type- 2 Br P usually is longer in leads V1-V2 (Fig. 4) although often is difficult to determine.
• There are a couple of new measurements which may also help to quantify the difference in the r’-wave morphology:
The alpha (α> 50°, Sensitivity 71% and Specificity 79%) and beta angles (β> 58°, Sensitivity 79 %, Specificity 83%) described by Chevallier [12] are greater in BrS than in incomplete RBBB (Fig. 3).
The duration of the base of the triangle, of the r’-wave at 5mm of the high take-off ≥ 4mm is a good criterion for Br.S [13] and is much shorter in healthy athletes with incomplete RBBB (Fig. 4).
OTHER TYPE-1 AND TYPE-2 ECG CRITERIA
The consensus group has also identified other electrocardiographic alterations that may be observed in BrS:
- Long QT in the right precordial leads [14].
- Conduction disorders (longer PR and HV intervals and wider QRS complexes), which occur more frequently in carriers of SCN5A gene mutations [15], as well as in symptomatic patients [16].
- The presence of atrial fibrillation (AF) or other supraventricular arrhythmias [17]. It has even been shown [18] that up to 5% of lone AF may also present a Br P. Additionally, new onset AF may be the first clinical manifestation of latent BrS
- The presence of an early repolarization pattern in inferior leads [19].
- The presence of fragmented QRS complexes [20].
- T-wave alternans, which may be observed after administration of sodium channel blockers [21].
DIFFERENTIAL DIAGNOSIS WITH OTHER ENTITIES
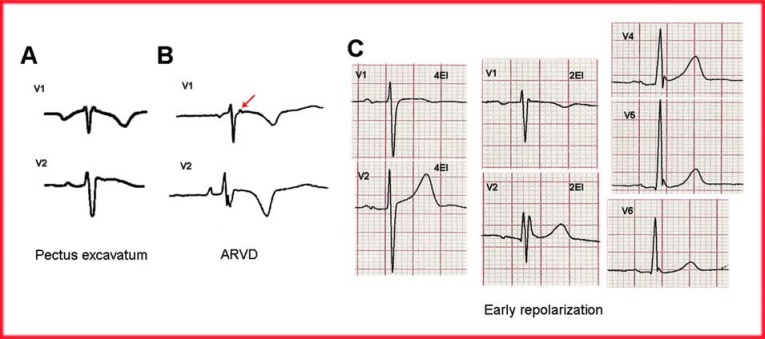
Differential diagnosis between Br P and other entities with ST-segment elevation may be difficult (Fig. 5), even for expert cardiologists. Other clinical entities whose ECG morphologies could be misdiagnosed as BrS are: Pectus excavatun, ARVD and early repolarization. Here we provide some quick clues to keep in mind:
Fig. (5).
(A) The ECG pattern of Pectus excavatum (22) depicting a negative P-wave in lead V1 (electrodes in adequate position). The r'-wave in lead V1 is narrow, followed by a slight ST-segment elevation. (B) In ARVD, the ECG pattern is quite different from that of BrS. The presence of an epsilon wave (arrow), atypical RBBB and negative T-waves beyond lead V3 helps in distinguishing between these two entities. (C) The ECG of patients with early repolarization usually presents J point and ST-segment elevation in the middle and left precordial leads. However, if leads V1-V2 electrodes are placed in a non-standard position (2nd intercostal space), rSr’ morphology is observed.
1. Isolated RBBB
The r’-wave is followed by ST-segment depression below the isoelectric line and the r’-wave is narrow.
2. Healthy Athletes
The ECG of healthy athletes depicts a fast r’-wave. The ST-segment is usually not elevated in lead V1 with a Corrado index is ≤1 (see above).
3. Pectus Excavatum
The ECG pattern found in pectus excavatum [22] usually presents with a negative P-wave in lead V1 despite adequate position of the precordial electrodes. The r'-wave in this lead is narrow, followed by a slight ST-segment elevation and the T-wave may be negative or positive/negative in lead V1 and positive in lead V2 (Fig. 5A). Some cases have been considered as Brugada phenocopies (see below).
4. Arrhythmogenic Right Ventricular Dysplasia (ARVD)
The ECG pattern of ARVD in leads V1-V2 is generally quite different from that observed in BrS [23]. In ARVD, atypical RBBB morphologies have been described with r’-wave plateau in lead V1 and the ST-segment usually not elevated. Occasionally, patients with BrS may depict an epsilon-like wave in lead V2 leading to confusion.
In ARVD, T-wave inversion in the precordial leads (V1 to V3-V5) is almost the rule. Although positive late potentials can also be found in BrS, the prevalence is much higher in ARVD [24] (Fig. 5B).
5. Early Repolarization Pattern (ERP)
The ECG pattern of ERP is a common variant, usually benign but recently associated with sudden death in selected cases [25]. It is characterized by a J point elevation which manifests as slurring or notching at the QRS-ST junction followed by an upward concave ST-segment in at least two consecutive leads. It may be recorded in the inferior and/or middle-left precordial leads but not in the right precordial leads. It is therefore, very different from the Br P, but both entities can coexist [26].
OTHER CONSIDERATIONS TO REMEMBER
Other ECG aspects were briefly discussed in the last consensus paper and deserve a comment in this review:
1) The concept of Brugada phenocopy has been recently introduced [27-29], and refers to an ECG pattern with Br P morphology that disappears after resolution of its precipitants. Patients with Brugada phenocopy must undergo a sodium blocker pharmacological provocation test and genetic testing in order to rule out true BrS. The latter is desirable but not mandatory, as genetic testing is only positive in 20-25% of true BrS. For detailed information on Brugada Phenocopies, please visit www.brugadaphenocopy.com
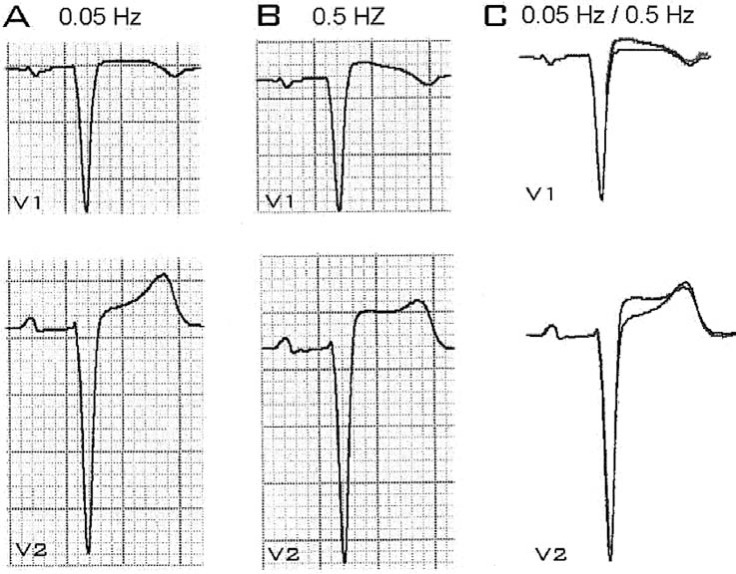
2) The new consensus document also describes certain technical details of ECG acquisition which can affect the recording. Improper use of the high-pass filter can distort the ST-segment and final portion of the T-wave, producing a Brugada phenocopy (Fig. 5) [28-29].
3) As in the previous consensus documents, changes produced by non-standard placement of electrodes were discussed, including the utility of high precordial lead placement to properly diagnose BrS (Fig. 6). A recent study [30] using MRI established that the exact location of the electrodes on the right ventricle outflow tract correlated with the most profound Br P changes. The authors indicate that the outflow tract is better recorded at the third intercostal space in the sternal and left parasternal positions.
Fig. (6).
Leads V1-V2 recordings performed with (A) standard 0.05 Hz filter and (B) non-standard filter (0.5Hz), showing how the use of a non-standard filter distorts the ST-segment producing a Brugada phenocopy. (C) On superimposing the two images, the degree of distortion is clearly seen.
CONCLUSION
This manuscript reviews the new tools developed to help health care providers in the differential diagnosis of BrS. The ECG remains the most essential diagnostic tool to suspect this infrequent but devastating condition.
ACKNOWLEDGEMENTS
Declared none.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Brugada P, Brugada J. Right bundle branch block. persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391–96. doi: 10.1016/0735-1097(92)90253-j. [DOI] [PubMed] [Google Scholar]
- 2.Probst V, Wilde AA, Barc J , et al. SCN5A mutations and the role of genetic background in the pathophysiology of Brugada syndrome. Circ Cardiovasc Genet. 2009;2:552–7. doi: 10.1161/CIRCGENETICS.109.853374. [DOI] [PubMed] [Google Scholar]
- 3.Frustaci A, Russo MA, Chimenti C. Structural myocardial abnormalities in asymptomatic family members with Brugada syndrome and SCN5A gene mutation. Eur Heart J. 2009;30:1763. doi: 10.1093/eurheartj/ehp148. [DOI] [PubMed] [Google Scholar]
- 4.Bayés de Luna A, Brugada J, Baranchuk Aetal. Current electrocardiographic criteria for diagnosis of Brugada pattern a consensus report. J Electrocardiol. 2012;45:433–42. doi: 10.1016/j.jelectrocard.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Wilde AA, Antzelevitch C, Borggrefe Metal. Study Group on the Molecular Basis of Arrhythmias of the European Society of Cardiology. Proposed diagnostic criteria for the Brugada syndrome consensus report. Circulation. 2002;106:2514–9. doi: 10.1161/01.cir.0000034169.45752.4a. [DOI] [PubMed] [Google Scholar]
- 6.Antzelevitch C, Brugada P, Borggrefe Metal. Brugada syndrome report of the second consensus conference. Heart Rhythm. 2005;2:429–40. doi: 10.1016/j.hrthm.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 7.Nishizaki M, Sugi K, Izumida Netal. Classification and assessment of computerized diagnostic criteria for Brugada-type electrocardiograms. Heart Rhythm. 2010;7:1660–6. doi: 10.1016/j.hrthm.2010.06.035. [DOI] [PubMed] [Google Scholar]
- 8.Corrado D, Pelliccia A, Heidbuchel H, et al. Section of Sports Cardiology European Association of Cardiovascular Prevention and Rehabilitation Working Group of Myocardial and Pericardial Disease European Society of Cardiology. Recommendations for interpretation of 12-lead electrocardio gram in the athlete. Eur Heart J. 2010;31:243–59. doi: 10.1093/eurheartj/ehp473. [DOI] [PubMed] [Google Scholar]
- 9.Postema PG, van Dessel PF, Kors JAetal. Local depolarization abnormalities are the dominant pathophysiologic mechanism for type 1 electrocardiogram in Brugada syndrome a study of electrocardiograms vectorcardiograms and body surface potential maps during ajmaline provocation. J Am Coll Cardiol. 2010;55:789–97. doi: 10.1016/j.jacc.2009.11.033. [DOI] [PubMed] [Google Scholar]
- 10.Bayés de Luna A, Garcia Niebla J, Goldwasser D. The ECG differential diagnosis of Brugada pattern and athletes. Eur Heart J. 2010 [Google Scholar]
- 11.Richter S, Sarkozy A, Paparella Getal. Number of electrocardiogram leads displaying the diagnostic coved-type pattern in Brugada syndrome A diagnostic consensus criterion to be revised. Eur Heart J. 2010;31:1357–64. doi: 10.1093/eurheartj/ehq049. [DOI] [PubMed] [Google Scholar]
- 12.Chevallier S, Forclaz A, Tenkorang J , et al. New electrocardiographic criteria for discriminating between Brugada types 2 and 3 patterns and incomplete right bundle branch block. J Am Coll Cardiol. 2011;58:2290–8. doi: 10.1016/j.jacc.2011.08.039. [DOI] [PubMed] [Google Scholar]
- 13.Serra-Autonell G, Goldwasser D, Brugada J , et al. Differential diagnosis of type 2 Brugada pattern and incomplete right bundle branch block in athletes. Eur Heart J. 2012;33(suppl):P3393. [Google Scholar]
- 14.Pitzalis MV, Anaclerio M, Iacoviello M. QT interval prolongation in right precordial leads in Brugada syndrome. J Am Coll Cardiol. 2003;42:1632–7. doi: 10.1016/j.jacc.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Smits JP, Eckardt L, Probs LV. Genotype-phenotype relationship in Brugada syndrome: ECG features differentiate SCN5A from non-SCN5A related patients. J Am Coll Cardiol. 2002;40:350–56. doi: 10.1016/s0735-1097(02)01962-9. [DOI] [PubMed] [Google Scholar]
- 16.Benito B, Brugada J, Brugada R, Brugada P. Síndrome de Brugada. Rev Esp Card. 2009;62:1297–315. doi: 10.1016/s1885-5857(09)73357-2. [DOI] [PubMed] [Google Scholar]
- 17.Schimpf R, Giustetto C, Eckardt L , et al. Prevalence of supraventricular tachyarrhythmias in a cohort of patients with Brugada syndrome. Ann Noninvasive Electrocardiol. 2008;13:266–9. doi: 10.1111/j.1542-474X.2008.00230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pappone C, Radinovic A, Manguso F , et al. New-onset atrial fibrillation as first clinical manifestation of latent Brugada syndrome: prevalence and clinical significance. Eur Heart J. 2009;30:2985–92. doi: 10.1093/eurheartj/ehp326. [DOI] [PubMed] [Google Scholar]
- 19.Sarkozy A, Cherchia G, Paparella G , et al. Inferior and lateral ECG repolarization abnormalities in Brugada syndrome. Circ Arrhythmic Electrophysiol. 2009;2:154–61. doi: 10.1161/CIRCEP.108.795153. [DOI] [PubMed] [Google Scholar]
- 20.Morita H, Kusano KF, Miura D , et al. Fragmented QRS as a marker of conduction abnormality and a predictor of prognosis of Brugada syndrome. Circulation . 008b;118:1697–704. doi: 10.1161/CIRCULATIONAHA.108.770917. [DOI] [PubMed] [Google Scholar]
- 21.Tada T, Kusano KF, Nagase S. The relationship between the magnitude of T wave alternans and the amplitude of the T wave in Brugada syndrome. J Cardiovasc Electrophysiol. 2008;19:56–61. doi: 10.1111/j.1540-8167.2007.00967.x. [DOI] [PubMed] [Google Scholar]
- 22.Karaoka H. Electrocardiographic patterns of the Brugada syndrome in two young patients with pectus excavatum. J Electrocardiol. 2002;35:169–71. doi: 10.1054/jelc.2002.32336. [DOI] [PubMed] [Google Scholar]
- 23.Marcus FI, McKenna WJ, Sherrill D , et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia. Proposed modification of the Task Force Criteria. Circulation. 2010;121:1533–41. doi: 10.1161/CIRCULATIONAHA.108.840827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yodogawa K, Morita N, Kobayashi Y , et al. A new approach for the comparison of conduction abnormality between arrhythmogenic right ventricular cardiomyopa-thy/dysplasia and Brugada syndrome. Ann Noninvasive Electrocardiol. 2011;16:263–9. doi: 10.1111/j.1542-474X.2011.00441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haïssaguerre M, Derval N, Sacher F , et al. Sudden cardiac arrest associated with early repolarization. N Eng J Med. 2008;358:2016–23. doi: 10.1056/NEJMoa071968. [DOI] [PubMed] [Google Scholar]
- 26.McIntyre W, Perez Riera A, Femenia F, Baranchuk A. Coexisting early repolarization pattern and Brugada syndromes recognition of potentially overlapping entities. J Electrocardiol. 2012;45:195–98. doi: 10.1016/j.jelectrocard.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 27.Baranchuk A, Nguyen T, Ryu MH , et al. Brugada Phenocopy: New Terminology and Proposed Classification. Ann Noninvasive Electrocardiol. 2012;17:299–314. doi: 10.1111/j.1542-474X.2012.00525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.García-Niebla J, Serra-Autonell G, Bayés de Luna A. Brugada syndrome electrocardiographic pattern as a result of improper application of a high pass filter. Am J Cardiol. 2012;110:318–20. doi: 10.1016/j.amjcard.2012.04.038. [DOI] [PubMed] [Google Scholar]
- 29.Anselm DD, Baranchuk A. Brugada Phenocopy: Redefinition and Updated Classification. Am J Cardiol. 2012;111:453. doi: 10.1016/j.amjcard.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 30.Veltman C, Papavassilu T, Konrad M , et al. Insights into the location of type 1 ECG in patients into the location of type 1 ECG in patients with Brugada syndrome: correlations of ECG and CV magnetic resonance imaging. Heart Rhythm. 2012;9:414–21. doi: 10.1016/j.hrthm.2011.10.032. [DOI] [PubMed] [Google Scholar]