Abstract
The traditional approach to the ECG diagnosis of left ventricular hypertrophy (LVH) is focused on the best estimation of left ventricular mass (LVM) i.e. finding ECG criteria that agree with LVM as detected by imaging. However, it has been consistently reported that the magnitude of agreement is rather low as reflected in the low sensitivity of ECG criteria. As a result, the majority of cases with true anatomical LVH could be misclassified by using ECG criteria of LVH. Despite this limitation, it has been reported that the ECG criteria for LVH provide independent information on the cardiovascular risk even after adjusting for LVM. Understanding possible reasons for the frequent discrepancy between common ECG LVH criteria and LVH by echo or MRI would help understanding the genesis of ECG changes that occur as a consequence of increased LV mass.
Keywords: Electrocardiography, left ventricular hypertrophy, electrical remodeling.
INTRODUCTION
In the 21st century, the role of electrocardiography in the assessment of left ventricular hypertrophy will move beyond the imprecise estimation of left ventricular mass to decoding its primary information - the electrical properties of hypertrophied myocardium. Future research must shift its focus from the correlation between anatomical parameters (weight, mass) and ECG parameters to research leading to an understanding of the discrepancies between the anatomical and electrical characteristics, the electrical origins of the changes in P waves, QRS complex, ST segment, and T waves, and the means by which these changes predict adverse clinical outcomes.
The accumulated evidence on electrical remodeling and its role in producing arrhythmias should be our model. We must link the electrical events accompanying hypertrophy to the underlying electrical events, and, in turn to the adverse effects seen with hypertension and other disease states leading to hypertrophy. As this evidence is evaluated, it should lead to a more precise utilization of the ECG in patient management, including the monitoring of response to drugs and other treatments. In support of this, we must improve the technical quality of the ECG recording, use modeling and simulation technology, and expand the graphical presentation of the electrical properties of myocardium.
Predicting the future role of the ECG in the diagnosis and management of patients whose disease manifests itself primarily as cardiac enlargement is a difficult challenge. Other imaging methods are increasingly seen as providing more accurate and more complete information. Even electrocardiologists are reconsidering its place, e.g.:“...The introduction of new noninvasive technology, in particular the echocardiogram with Doppler, allows viewing image of the the beating heart in 2 and 3 dimensions and follow the intracardiac blood flow. This development has diminished the role of the ECG in the assessment of hypertrophy and dilatation of cardiac chambers and in sizing myocardial infarction..Therefore, the ECG is no longer needed to establish the diagnosis and follow the management of patients with congenital and acquired structural diseases of the myocardiu, cardiac valves, great vessels, and pericardium..” [1].
The electrocardiographic (ECG) diagnostics of left ventricular hypertrophy (LVH) currently is based primarily on the QRS voltage criteria. However, increased QRS voltage in the setting of actual anatomical left ventricular hypertrophy (LVH) is not a consistent finding, as reflected in a wide range of both sensitivities and specificities of ECG criteria for LVH [2, 3]. Nevertheless, ECG criteria for LVH have been shown to be a strong independent predictor of cardiovascular morbidity and mortality in patients with essential hypertension and in the general population [4, 5].
QRS complex patterns in LVH patients cover a broad spectrum: increased QRS voltage, prolonged QRS duration, left axis deviation, and LAFB and LBBB-like patterns, as well as pseudo-normal QRS patterns. In general, the resultant QRS voltage is determined by interplay of spatial and non-spatial determinants [6]. The interpretation of the ECG in LVH focuses on the spatial determinants, while tending to neglect the modified electrical properties of the myocardium. Traditionally, discrepancies between LVM and QRS voltage are perceived as a limitation of ECG in LVH diagnosis.
Currently it seems that the terms left ventricular enlargement, left ventricular hypertrophy and increase in left ventricular mass are used somewhat interchangeably, it is therefore important to start with the definition of left ventricular hypertrophy. While it may seem self evident that this term refers to an increase in the mass of the left ventricle, some would not agree. Some would insist that the term be limited to an increase in mass in response to a disease state, thereby excluding the physiologic increase in mass which accompanies physical training or pregnancy. Some would prefer the term left ventricular enlargement, considering it to be a more inclusive term, skirting the pathologic/non-pathologic issue. Of more concern to the readers of this paper are those who consider “LVH” to be an electrocardiographic term, referring to an electrocardiogram which meets certain criteria which have been found in individuals with an increased heart mass. While few would consider this a valid definition for the term, it is frequently used in ECG reports: “This ECG shows LVH”. This use of the term is probably used carelessly, or out of a desire to shorten the more accurate “This ECG shows electrical abnormalities which meet the Cornell Criteria for the ECG diagnosis of left ventricular hypertrophy”. To clarify the use of the term in this paper, we consider left ventricular hypertrophy to be an increase in the anatomic mass of the left ventricle, whether physiologic or pathologic, and it is interchangeable with left ventricular enlargement. We do NOT believe that it should include the constellation of electrical abnormalities often seen with anatomic LVH, a point which we will defend in the paper.
Before considering the future role of the ECG, it is logical that we start with a review of its perceived role in the recent past, i.e. the beginning of the 21st century. The 2009 statement of the AHA/ACCF/HRS [7] on cardiac chamber hypertrophy serves as a convenient and appropriate starting point. In considering left ventricular enlargement, this document provides a list of 36 criteria which were considered useful for its detection, divided into five groups:
Limb lead voltage;
Precordial lead voltage;
Combination of limb and precordial voltage;
Combination of voltage and non-voltage
Combined criteria with left anterior fascicular block and bundle-branch block.
The majority of these criteria, in all groups, are based on increased voltage in defined leads, and the reflection of the major spatial changes of the cardiac electric field associated with LVH – its shift to the left, posteriorly and upward. The combined voltage and non-voltage criteria also include QRS duration, and the Romhilt-Estes score utilizes more QRS parameters than voltage alone (left axis deviation, intrinsicoid deflection) and also includes changes in the ST-T segment and P wave [8].
While that consensus statement is primarily concerned with the sensitivity and specificity of various criteria in predicting the presence of anatomically validated hypertrophy, it does refer to more recent information about reversal of hypertrophy with therapy and the possible value of the ECG to assist the clinician in preventing or delaying adverse outcomes. Nevertheless, the large number and variety of ECG criteria for a seemingly simple clinical parameter, increased size of the left ventricle, is noteworthy, especially in view of the fact that the list is a result of expert consensus, and all of the criteria are evidence based.
The number of ECG criteria for LVH implies that no single or explicit ECG pattern is predictive of an increase in left ventricular mass, and that there are a variety of yet unexplained associations between the ECG and the anatomic entity of increased left ventricular mass. The consensus statement seems to reflect this state of affairs, in that it recommends no single criterion, but recommends that the ECG reader specify the one used in the interpretation, and that other modifying factors, such as gender, race, and body habitus be included when these factors are validated.
Pewsner’s meta-analysis [9] of the value of the ECG in the diagnosis of LVH in hypertension provides a useful summary of information on this topic at the turn of the century. The most common ECG criteria (Sokolow-Lyon index [10], Cornell voltage [11], Cornell voltage-duration product [12], Gubner [13], Romhilt-Estes 4 and 5 points [8]) were compared with respect to sensitivity and specificity. The most striking finding was the large spread in reported sensitivity (0 to 68%) and specificity (53 to 100%). Median sensitivity and specificity were equally wide, and the more recent and more sophisticated indices did not out-perform the Sokolow-Lyon index, which was developed in 1949. The correct identification of true positive and true negative cases of LVH is unsatisfactory. It is obvious that the ECG has failed in its important assignment of detection of the increased left ventricular mass.
Kannel and others [14, 15] have documented that some of the same criteria used in the detection of left ventricular enlargement are also independent risk factors, in both the general population and in hypertensive patients, for cardiovascular disease and early death. It should be emphasized that this risk is independent from increased left ventricular mass measured by echocardiography [16, 17]. This attention grabbing risk of a purely electrical phenomena predicting increased cardiovascular risk is seldom mentioned in lists of general cardiovascular risk factors, neither among modifiable nor non-modifiable risk factors.
In summary, at the turn of 21st century, the role of the ECG in managing patients with LV enlargement is centered around the hypothesis that left ventricular enlargement is the only important evidence of target organ damage, and is the principal signal for action by the clinician to increase treatment and tighten management. However, in spite of its poor performance in detection of increased LV mass, the ECG has continued to be used, largely because of its wide availability and relatively low cost. Other LVH diagnostic methods (echocardiography and magnetic resonance imaging), with an established superior performance of sensitivity and specificity, are utilized increasingly as a means of evaluating ventricular mass. This has caused some to question the future utility of the ECG as a clinical tool.
THE FUTURE
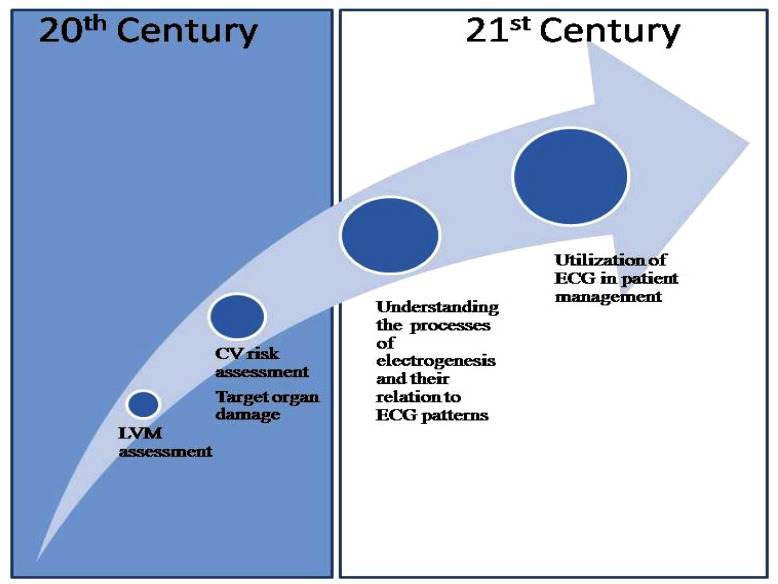
The most obvious lesson from the past is that we must look beyond the diagnosis of increased ventricular mass as the main objective of the ECG (Fig. 1). Most of our research time and effort has been expended in the largely unsuccessful attempt to improve the sensitivity and specificity of the ECG to detect increased LV mass by correcting for sex, race, ethnicity and other possible confounders. The fact that increased mass is important cannot be seriously questioned. Increased mass from echocardiogram does predict mortality independent of the electrocardiogram. What is then the role of ECG?
Fig. (1).
In the 21st century, the role of electrocardiography in assessment of left ventricular hypertrophy will move beyond the estimation of left ventricular mass and risk assessment to a deeper understanding of electrogenesis and electrical remodeling and its relation to ECG patterns.
BASIC UNDERSTANDING OF ELECTRICAL REMODELING WITH HYPERTROPHY
The major challenge for the future is to fill in the major gaps in our information and knowledge base:
How do the large number of patients with demonstrated ventricular enlargement who have no ECG abnormalities differ from those who do?
What is the underlying mechanism that produces the electrical remodeling seen with left ventricular enlargement?
What is the time course of electrical remodeling and corresponding ECG patterns during the evolution of ventricular enlargement?
How do these electrical changes relate to the adverse outcomes accompanying them?
How do the variety of ECG patterns (increased amplitude, axis deviation, ST-T changes, P wave changes, etc.) seen with hypertrophy relate to myocardial function and to adverse outcomes?
Do the various ECG patterns differ in their correlation with increased ventricular mass and increased mortality and morbidity?
How is the effect of cardioactive /antihypertensive drugs reflected in the variety of ECG patterns in left ventricular enlargement?
NEW GUIDANCE IN THE MANAGEMENT OF PATIENTS AND RISK ASSESSMENT:
Answering these questions may enable us to direct our primary attention to the expanded use of the ECG as an indicator of success or failure in the management of patients with ventricular hypertrophy, and in particular, those with hypertension. Though we have a number of very good therapeutic interventions for this prevalent and serious disease, we are still using intermittently measured level of blood pressure as the major clinical indicator of success or failure of therapy. Although there is accumulated detailed knowledge on the effect of cardioactive and antihypertensive drugs at the level of receptors or ion channels, this knowledge is not linked to our understanding of the effect of these drugs on impulse creation and propagation, and how this relates to the interpretation of ECG patterns.
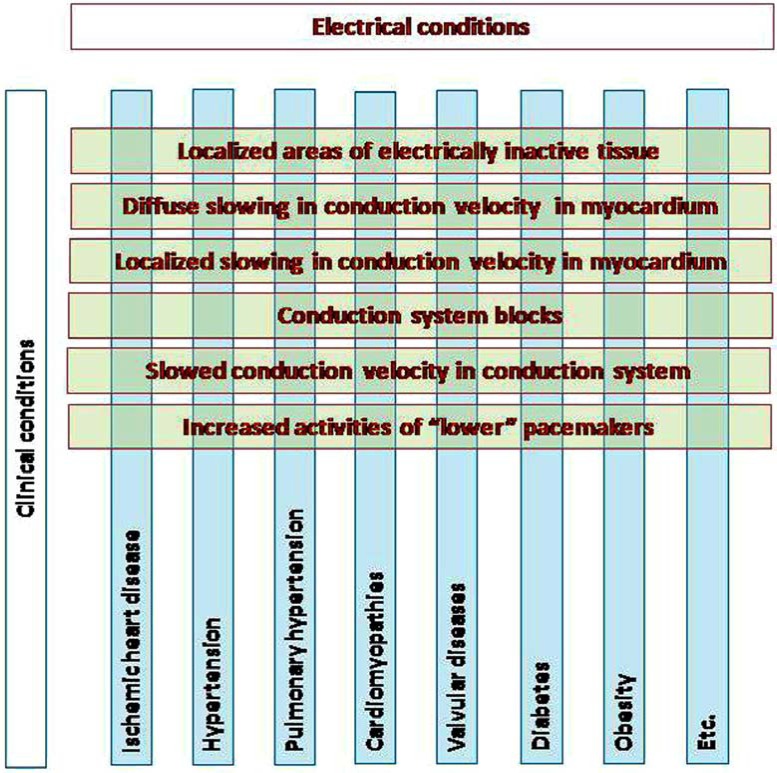
Similarly, another challenge is to understand the implications of the negative prognostic and predictive ability of the ECG (i.e., its use in cardiovascular risk assessment) and its value in preventive programs and in management of patients at risk. In this context, it is clear that there should be a change in our terminology used for changes in electrical properties associated with left ventricular enlargement. As shown in (Fig. 2), we must use terminology consistent with the information provided by ECG – i.e. electrical terminology rather than anatomic or clinical terminology.
Fig. (2).
Electrocardiography must use terminology consistent with the information it provides – information on impulse generation and propagation. The same alterations of electrical properties can be present with different clinical situations. Moreover, the clinical conditions are not “pure”. We deal with co-morbidities in the clinical practice. This is a major challenge for electrocardiography in the 21st century in general, and for the diagnosis of left ventricular hypertrophy in particular.
IMPROVED TECHNICAL QUALITY IN THE RECORDING OF AND PROCESSING THE ECG, GRAPHICAL PRESENTATION, MODELING AND MULTIMODAL IMAGING
The classical 12- lead ECG using the hexaxial coordinate system and precordial leads provides an unnecessarily complex and redundant concept for understanding the relation between individual ECG curves and the heart, and the enlarged left ventricle in particular. Orthogonal lead systems and new 2D and 3D graphical presentations of the electrical events in the myocardium – i.e. impulse generation and propagation – will go beyond the “classical” scalar electrocardiograms. New methods of interpretation of the shape, planarity and complexity of the vector loops may provide the needed links [18]. In the case of LVH, the simultaneous recording of the ECG with signals from other comparable images of ECG signals and other diagnostic techniques will provide a more complete and complex view of the relationships between structural and functional characteristics of the hypertrophied ventricle, and thus contribute to answering many of the above mentioned questions.
In conclusion, in the 20th century the ECG was not very successful in its traditionally assigned role – the estimation of increased left ventricular mass. On the other hand, evidence of the association between a variety of ECG changes seen with LVH and prognosis provides powerful evidence of the independent and unique information provided by ECG, and should provoke the interest of researchers, clinicians and epidemiologists alike.
The ultimate role of any diagnostic method in cardiology is to meet the needs of the physician in diagnosing and managing cardiac patients. It is highly likely that we have already harvested the low lying fruit in ECG diagnosis over the past century of its use. ECG is the only diagnostic method recording the electrical activity of the heart. The electrical impulses precede/ trigger myocardial contractions. Creation and propagation of electrical impulses and contraction are two linked but distinguishable processes; therefore the idea about replacing ECG by methods providing anatomical, structural and/ or hemodynamic information is not rational.
It is a paradox that the introduction of imaging methods, such as echocardiography or cardiac magnetic resonance (CMR) imaging, into clinical evaluation of LVH has presented a challenge for electrocardiography. The specific roles of these individual methods can now be explicitly defined, and each of these imaging methods can be used for more appropriate estimation of mass, volume and pattern of LVH, structure and movements of the myocardium, and hemodynamic events. The ECG can and should now focus on its specific and unique information – electrogenesis (impulse generation and impulse propagation), diagnosis of the electrical status of the myocardium, and in risk assessment and monitoring of the effect of therapy. It should be noted that this information is complementary to the information provided by other imaging methods. The apparent limitation/disadvantage of ECG may prove to be its principal advantage.
During recent years, significant knowledge of the active and passive electrical properties of hypertrophied myocardium has been summarized, especially in relation to arrhythmias going deeply into subcellular structures and processes. The term “electrical remodeling” has been introduced, comprising complex changes in active and passive electrical properties of myocardium, including cardiac microstructure, ion channels, energy metabolism, and gene expression. Building on this knowledge, the diagnostic role of ECG in left ventricular enlargement will go beyond the imprecise estimation of left ventricular mass [19, 20]. The future role of ECG in LVH will focus on the specific unique information in the electric field of the heart, and will bring clinical indicators for diagnosing and managing the early signs of heart failure and an arrhythmogenic substrate.
ACKNOWLEDGEMENTS
Partly supported by the grant ITMS 26240220072, Structural Funds, Slovak Republic.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Surawicz B. How to increase the accuracy of electrocardiogram’s interpretation and stimulate the interest of interpreters?. J Electrocardiol. 2010;43:19–3. doi: 10.1016/j.jelectrocard.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Pewsner D, Jüni P, Egger M, Battaglia M, Sundström J, Bachmann LM. Accuracy of electrocardiography in diagnosis of left ventricular hypertrophy in arterial hyper-tension: systematic review. BMJ. 2007;335(7622):711–719. doi: 10.1136/bmj.39276.636354.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hancock EW, Deal BJ, Mirvis DM , et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part V: electrocardiogram changes associated with cardiac chamber hypertrophy: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee. Council on Clinical Cardilogy the American College of Cardiology Foundation, and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am CollCardiol . 2009;53(11):992–1002. doi: 10.1016/j.jacc.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 4.Kannel WB, Gordon T, Castelli WP, Margolis JR. Electrocardiographic left ventricular hypertrophy and risk of coronary heart disease: the Framingham Study. Ann Intern Med. 1970;72:813– 22. doi: 10.7326/0003-4819-72-6-813. [DOI] [PubMed] [Google Scholar]
- 5.Rautaharju PM, LaCroix AZ, Savage DD , et al. Electrocardiographic estimate of left ventricular mass versus radiographic cardiac size and the risk of cardiovascular disease mortality in the epidemiological follow-up study of the first National Health and Nutrition Examination Survey. Am J Cardiol. 1988;62:59–66. doi: 10.1016/0002-9149(88)91365-3. [DOI] [PubMed] [Google Scholar]
- 6.Bayley RH, editor. New York: Paul B. Hoeber; 1958. Biophysical principles of electrocardiography. [Google Scholar]
- 7.Hancock EW, Deal BJ, Mirvis DM , et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part V: electrocardiogram changes associated with cardiac chamber hypertrophy: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee. Council on Clinical Cardilogy the American College of Cardiology Foundation, and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol . 2009; 53:992. doi: 10.1016/j.jacc.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 8.Romhilt D, Estes E. Point-score system for the ECG diag-nosis of left ventricular hypertrophy. Am Heart J. 1968;75:752–8. doi: 10.1016/0002-8703(68)90035-5. [DOI] [PubMed] [Google Scholar]
- 9.Pewsner D, Jüni P, Egger M, Battaglia M, Sundström J, Bachmann LM. Accuracy of electrocardiography in diagnosis of left ventricular hypertrophy in arterial hyper-tension: systematic review. BMJ. 2007;6:335. doi: 10.1136/bmj.39276.636354.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sokolow M, Lyon TP. The ventricular complex in left ventricular hypertrophy as obtained by unipolar and limb leads. Am Heart J. 1949;37:161–6. doi: 10.1016/0002-8703(49)90562-1. [DOI] [PubMed] [Google Scholar]
- 11.Casale P, Devereux R, Kligfield P , et al. Electrocardio-graphic detection of left ventricular hypertrophy: development and prospective validation of improved criteria. J Am Coll Cardiol. 1985;6:572–80. doi: 10.1016/s0735-1097(85)80115-7. [DOI] [PubMed] [Google Scholar]
- 12.Okin PM, Roman MJ, Devereux RB, Kligfield P. Electrocardiographic identification of increased left ventricular mass by simple voltage-duration products. J Am Coll Cardiol. 1995;25:417–23. doi: 10.1016/0735-1097(94)00371-v. [DOI] [PubMed] [Google Scholar]
- 13.Gubner RS, Ungerlieder HE. Electrocardiographic criteria of left ventricular hypertrophy: factors determining the evolution of the electrocardiographic patterns in hypertrophy and bundle branch block. Arch Intern Med. 1943;72:196–209. [Google Scholar]
- 14.Kannel WB, Gordon T, Castelli WP, Margolis JR. Electrocardiographic left ventricular hypertrophy and risk of coronary heart disease: the Framingham Study. Ann Intern Med. 1970;72:813. doi: 10.7326/0003-4819-72-6-813. [DOI] [PubMed] [Google Scholar]
- 15.Kannel WB. Framingham Risk stratification in hypertension: new insights from the Framingham study. Am J Hypertension. 2000;13(1):S3–S10. doi: 10.1016/s0895-7061(99)00252-6. [DOI] [PubMed] [Google Scholar]
- 16.Sundström J, Lind L, Arnlöv J, Zethelius B, Andrén B, Lithell HO. Echocardiographic and electrocardiographic diagnoses of left ventricular hypertrophy predict mortality independently of each other in a population of elderly men. Circulation. 2001;103:2346– 51. doi: 10.1161/01.cir.103.19.2346. [DOI] [PubMed] [Google Scholar]
- 17.Verdecchia P, Porcellati C, Reboldi G , et al. Left ventricu-lar hypertrophy as an independent predictor of acute cerebrovascular events in essential hypertension. Circulation. 2001;4:2039. doi: 10.1161/hc4201.097944. [DOI] [PubMed] [Google Scholar]
- 18.Correa R, Prini PD , Valentinuzzi ME, Lacien E. Novel set of vectorcardiographic parameters for the identification of ischemic patients. Med Engin Phs. 2013;35:16–22. doi: 10.1016/j.medengphy.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 19.Bacharova L, Estes EH, Bang L, Rowlandson I, Schillaci G, Verdecchia P, Macfarlane P. The first statement of the Working Group on ECG Diagnosis of Left Ventricular Hy-pertrophy. J Electrocardiol. 2010;43:197–9. doi: 10.1016/j.jelectrocard.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 20.Bacharova L, Estes EH, Bang LE, Hill JA, Macfarlane PW, Rowlandson I, Schillaci G. Second statement of the Working Group on Electrocardiographic Diagnosis of Left Ventricular Hypertrophy. J Electrocardiol. 2011;44:568–70. doi: 10.1016/j.jelectrocard.2011.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]