After Giulio Bizzozero identified platelets at the end of the 19th century,1 many authors sought to define the normal concentration of these elements in human blood. However, methods to enumerate platelets remained inaccurate until the middle of the last century, and the proposed reference intervals for platelet count ranged from 130–350 to 500–900×109/L of whole blood.2
The development of the Coulter Principle in 19533 revolutionized blood counting and resulted in the development of the electronic instruments currently used in our laboratories. About thirty years ago, these instruments were used to study several thousands of blood samples of unselected donors thus defining the reference interval of platelet count as 150–450 or 150–400×109/L.4,5 These values are still used today in most Western countries, although in the meantime several studies have indicated that platelet count varies according to age, sex and ethnicity. It is, therefore, appropriate to discuss whether a single reference interval for all people is still valid or whether new normal ranges taking into account these variables have to be used in clinical practice.
Aging and platelet count
The matter of age-related changes in platelet count was first examined in 1977 by Stevens and Alexander, who measured platelet count in 868 blood donors aged between 18 and 65 years and did not find any age-related differences.6 In contrast, a progressive decline in platelet count with aging was shown a few years later in 477 ambulatory patients, with a difference of over 100×109/L between children aged 1–5 years old and seniors over the age of 71 years.7 A correlation between platelet count and age was also found by a larger study that evaluated 12,142 adult inhabitants of the United States and found statistically significant differences between young and old individuals.8 However, these differences were small: less than 30×109/L between people of 17–19 years and those over 70. Thus, until a few years ago, both the existence and the possible extent of age-related changes in platelet count were uncertain, but a series of cross-sectional studies performed recently in different Italian populations has definitively clarified this matter. Analysis of 12,517 inhabitants of Sardinian geographic isolates found that a 10-year increase in age corresponded to a 9×109/L decrease in platelet count.9 Very similar results were obtained in 7266 inhabitants of five additional geographic isolates located in different Italian areas10 and in the cohort of the Moli-Sani Project including 24,318 subjects from 30 Molise cities and villages.11 Finally, a recent study put together all data of subjects enrolled in the three population-based studies referenced above and concluded that age-related changes were actually very large: platelet count in old age was reduced by 35% in men and by 25% in women with respect to early infancy.12 As shown in Figure 1, most of this reduction occurred in childhood and in old age, with only minor changes in adulthood. Thus, there is no longer any doubt that age is a major determinant of platelet count in healthy people.
Figure 1.
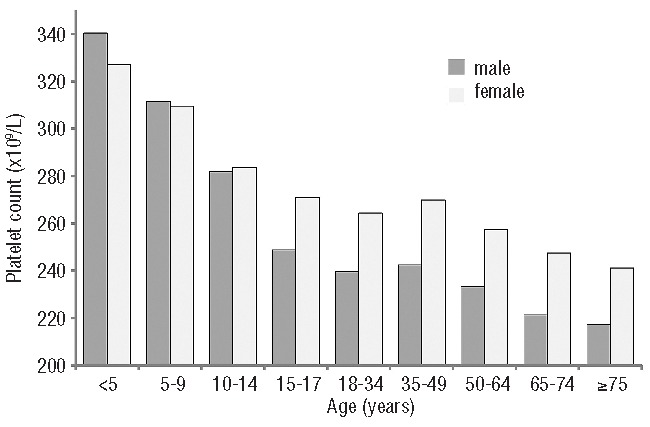
Platelet count by age and sex in 40,987 inhabitants of seven Italian areas. Platelet count decreases with age, and women have more platelets than man after puberty. Modified with permission (http://creativecommons.org/licenses/by/3.0/) from Büno et al.12
There is no proven explanation for these age-related changes, although it may be that the sharp decrease in platelet count during infancy reflects the decline of thrombopoietin levels occurring from birth to adulthood.13 Concerning the mechanism of platelet reduction in old age, it has been suggested that it derives from a survival advantage of subjects with lower platelet counts or a reduction in hematopoietic stem cell reserve during aging.12 However, both these explanations are purely hypothetical, and further investigation is required to clarify this matter.
Other physiological variables affecting platelet count
Gender
Sex-related differences in platelet count were described for the first time in 1977 in a study that analyzed 868 blood donors. The mean platelet count was higher in women than men in all age classes, although the differences were small (approx. 20–40×109/L) and tended to diminish after menopause. Subsequent studies confirmed that females have a slightly higher platelet count.7,8,14 The already mentioned studies of different Italian populations further supported this conclusion and precisely defined sex-related differences in relation to aging.9–12 In particular, no difference in the platelet count of men and women was found before the age of 15 years, whereas women had more platelets than men in the age range 15–64 years and over 64 years.12 In any case, sex-related differences in adults were only approximately 10% and much lower than those related to aging.
As for age-related variability, also the mechanisms of sex-related differences in platelet count are unknown. However, the finding that women have a higher platelet count than men only after the age of 14 years suggests that puberty makes the difference. We can speculate that the reduction in body iron in females, which occurs in menstruating women and persists in the elderly,15 stimulates platelet production.16,17 However, the hormonal differences between men and women after puberty could also play a role. In particular, the observation that estrogens favor platelet formation in mouse supports this hypothesis,18 although no data in humans are available.
Genetic background
Several studies showed that platelet count is highly heritable,14 and a few genetic factors responsible for platelet count variability in healthy individuals have been identified.19 The importance of genetic background in regulating the concentration of platelets is well illustrated by a recent study of five geographic isolates in Italy,10 where mean platelet count in healthy inhabitants of different areas ranged from 220 to 265×109/L. Similar ethnicity-related differences have been observed in the US population,8 and even more relevant differences have been described in different African countries.20
Should we up-date reference intervals for platelet counts?
A number of observations in different populations unequivocally demonstrated that age, sex and genetic background modulate platelet count in healthy people. The effect of aging is much bigger than those of sex and ethnicity, but also the latter variables may be clinically relevant when combined with age-related variation. This is well exemplified by Sardinian geographic isolates where different genetic backgrounds are responsible for large differences in mean platelet counts in different areas.9 The percentage of healthy people under the age of 18 years with platelet counts over 400×109/L was 11% in the isolates with higher mean platelet counts, while it was less than 4% in the isolates with lower mean platelet counts. Conversely, more than 10% of inhabitants older than 60 years had platelet counts of less than 150×109/L in isolates with lower mean platelet counts, while this proportion was reduced to 4.5% in isolates with higher mean platelet counts. Thus, using 150–400×109/L as the normal range for platelet count, a number of old people of some areas could be at risk of receiving a wrong diagnosis of thrombocytopenia, while young inhabitants of other areas could be at risk of an undue diagnosis of thrombocytosis.
The inappropriateness of the single limit of 150×109/L to define thrombocytopenia is also supported by the results of a study that monitored for five years 191 apparently healthy adults with incidentally discovered platelet counts between 100 and 150×109/L.21 In the vast majority of cases, the degree of thrombocytopenia remained stable without the appearance of any disease, and the authors concluded that the risk of developing severe thrombocytopenia in this category of patients was low. Based on the evidence discussed above, we hypothesize that these subjects (or a portion of them) were completely healthy and had platelet count lower than 150×109/L because of the combined action of sex, age and genetic background.
In conclusion, there is little doubt that a new reference range taking into account these variables would be desirable to identify more accurately subjects with platelet disorders. Indeed, such a tool has been recently developed for the Italian population.12 It indicates the normal ranges of platelet count for three age classes: under 15 years, between 15 and 64 years, and over 64 years. Moreover, because of the occurrence of sex-related differences after puberty, it indicates separate values for men and women in the last two age classes. Finally, it defines a sort of ‘extended reference interval’ whose upper and lower limits are those calculated in the Italian areas with the highest and the lowest mean platelet count, respectively. These reference intervals are shown in Figure 2.
Figure 2.
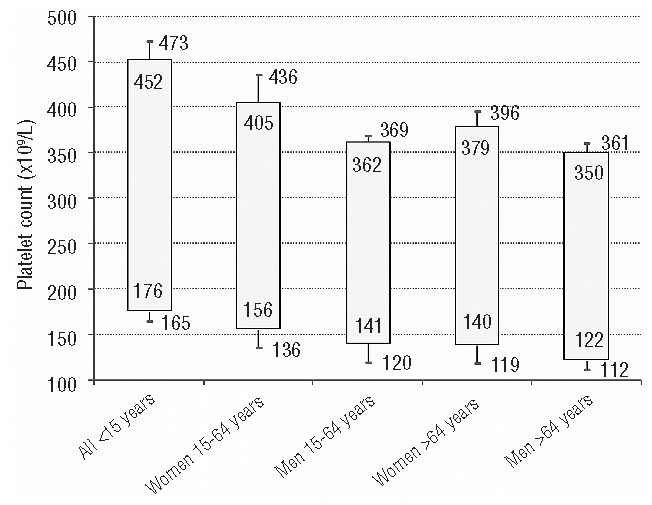
Age and sex-related variations in platelet count in 40,987 inhabitants of seven Italian areas. Numbers inside bars represent reference intervals (2.5th and 97.5th percentiles) estimated on the global population. Numbers outside bars define ‘extended reference intervals’ whose upper and lower limits are those defining the upper and the lower limits of normal ranges in the geographical areas with the highest and lowest mean platelet counts, respectively. Subjects with platelet counts within the reference intervals have to be considered normal, while those with platelet counts outside this range but within the extended one are in a ‘gray’ area that is still compatible with a normal phenotype, but also with mild forms of thrombocytosis or thrombocytopenia. Reproduced with permission (http://cre-ativecommons.org/licenses/by/3.0/) from Büno et al.12
Although the new reference intervals have not yet been used in clinical practice, they are expected to reduce the number of older subjects, especially men, who receive an undue diagnosis of mild thrombocytopenia, as well as the number of children with undue diagnosis of mild thrombocytosis. Conversely, the incidence of thrombocytopenia in children and that of thrombocytosis in adult males could increase. Further studies are required to confirm that these reference intervals better distinguish subjects with diseases affecting platelet count from healthy people. We do not know whether the new definition of normal platelet count in Italy could be generalized to other countries, but the observation that mean values of platelet count in Italy are similar to those observed in other Caucasian populations suggests that their use could be appropriate for other people with this ethnic origin.
Footnotes
Financial and other disclosures provided by the author using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are available with the full text of this paper at www.haematologica.org.
References
- 1.Bizzozero G. Su di un nuovo elemento morfologico del sangue dei mammiferi e della sua importanza nella trombosi e nella coagulazione. Osservatore Gazzetta Clin 1881;17:785–7 [Google Scholar]
- 2.Sloan AW. The normal platelet count in men. J Clin Path 1951;4(1):37–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coulter WH. (1953) Means for Counting Particles Suspended in a Fluid. US Patent 2656508
- 4.Giles C. The platelet count and mean platelet volume. Br J Haematol 1981;48(1):31–7 [DOI] [PubMed] [Google Scholar]
- 5.Dacie JV, Lewis SM. Practical Haematology, 7th ed London: Churchill Livingstone; 1991; p. 668 [Google Scholar]
- 6.Stevens RF, Alexander MK. A sex difference in the platelet count. Br J Haematol 1977;37(2):295–300 [DOI] [PubMed] [Google Scholar]
- 7.Graham SS, Traub B, Mink IB. Automated platelet-sizing parameters on a normal population. Am J Clin Pathol 1987;87(3):365–9 [DOI] [PubMed] [Google Scholar]
- 8.Segal JB, Moliterno AR. Platelet counts differ by sex, ethnicity, and age in the United States. Ann Epidemiol 2006;16(2):123–30 [DOI] [PubMed] [Google Scholar]
- 9.Biino G, Balduini CL, Casula L, Cavallo P, Vaccargiu S, Parracciani D, et al. Analysis of 12,517 inhabitants of a Sardinian geographic isolate reveals that predispositions to thrombocytopenia and thrombocytosis are inherited traits. Haematologica 2011;96(1):96–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Biino G, Gasparini P, D’Adamo P, Ciullo M, Nutile T, Toniolo D, et al. Influence of age, sex and ethnicity on platelet count in five Italian geographic isolates: mild thrombocytopenia may be physiological. Br J Haematol 2012;157(3):384–7 [DOI] [PubMed] [Google Scholar]
- 11.Santimone I, Di Castelnuovo A, De Curtis A, Spinelli M, Cugino D, Gianfagna F, et al. White blood cell count, sex and age are major determinants of heterogeneity of platelet indices in an adult general population: results from the MOLI-SANI project. Haematologica 2011;96(8):1180–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Biino G, Santimone I, Minelli C, Sorice R, Frongia B, Traglia M, et al. Age- and sex-related variations in platelet count in Italy: a proposal of reference ranges based on 40987 subjects’ data. PLoS One 2013;8(1):e54289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ishiguro A, Nakahata T, Matsubara K, Hayashi Y, Kato T, Suzuki Y, et al. Age-related changes in thrombopoietin in children: reference interval for serum thrombopoietin levels. Br J Haematol 1999;106(4):884–8 [DOI] [PubMed] [Google Scholar]
- 14.Buckley MF, James JW, Brown DE, Whyte GS, Dean MG, Chesterman CN, et al. A novel approach to the assessment of variations in the human platelet count. Thromb Haemost 2000;83(3):480–4 [PubMed] [Google Scholar]
- 15.Pirrie R. The influence of age upon serum iron in normal subjects. J Clin Pathol 1952;5(1):10–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beguin Y. Erythropoietin and platelet production. Haematologica 1999;84(6):541–7 [PubMed] [Google Scholar]
- 17.Kadikoylu G, Yavasoglu I, Bolaman Z, Senturk T. Platelet parameters in women with iron deficiency anemia. J Natl Med Assoc 2006;98(3): 398–402 [PMC free article] [PubMed] [Google Scholar]
- 18.Nagata Y, Yoshikawa J, Hashimoto A, Yamamoto M, Payne AH, Todokoro K. Proplatelet formation of megakaryocytes is triggered by autocrine-synthesized estradiol. Genes Dev 2003;17(23):2864–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shameer K, Denny JC, Ding K, Jouni H, Crosslin DR, de Andrade M, et al. A genome- and phenome-wide association study to identify genetic variants influencing platelet count and volume and their pleiotropic effects. Hum Genet. 2013. September 12 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kueviakoe IM, Segbena AY, Jouault H, Vovor A, Imbert M. Hematological reference values for healthy adults in togo. ISRN Hematol 2011;2011:736062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stasi R, Amadori S, Osborn J, Newland AC, Provan D. Long-term outcome of otherwise healthy individuals with incidentally discovered borderline thrombocytopenia. PLoS Med 2006;3(3):e24. [DOI] [PMC free article] [PubMed] [Google Scholar]


