Abstract
Objective
This study documents the prevalence of HIV testing in a sample of college students and examines associated demographic and behavioral characteristics.
Participants
College students ages 18 or older were randomly selected to participate in a health behavior survey at a southeastern university in September 2011.
Methods
Only sexually active students were included (n = 905). Relationships between demographic and sexual behavior characteristics were explored using logistic regression and classification regression tree (p≤0.05).
Results
Only 36.2% reported having been tested for HIV. Age was the most significant factor associated with testing. Factors associated with those least likely to be tested were race and anal sexual activity. Unsafe sexual behaviors were also associated with lower rates of HIV testing.
Conclusions
Findings support the need for targeted HIV interventions on college campuses. Such interventions need to be tailored for at-risk students and take into consideration factors likely to contribute to HIV testing.
Keywords: college students, HIV, HIV testing, prevention, risky behavior
Human immunodeficiency virus (HIV) continues to be a major public health challenge. The Centers for Disease Control and Prevention (CDC) estimate 1.2 million adults and adolescents are living with HIV in the United States and approximately 50 thousand are newly infected each year.1 Public perception about the seriousness of the HIV epidemic has declined in recent years,2 yet HIV infection and acquired immune deficiency syndrome (AIDS) remain as a significant cause of death and illness in the United States.1 There is a necessity to further understand at-risk groups in order to implement targeted HIV prevention interventions.
Youth ages 13–24 account for about one-fourth (26%) of all new HIV infections each year3 yet research continues to demonstrate that a large portion of young people express little concern about becoming infected.4 The Health Belief Model provides an opportunity to understand an individual’s beliefs or perceptions of acquiring a disease such as HIV.5 Among college students, it is known that HIV is preventable; thereby decreased perceived susceptibility contributes to low levels of testing and late diagnosis. The CDC classifies a person to be at high risk of HIV infection if they (or a sexual partner) have had more than one sex partner since their most recent HIV test.6 HIV is not curable, yet the earlier the virus can be detected the increased likelihood it can be controlled at a level that helps the infected individual stay healthy and reduce their risk of transmitting HIV to sexual partners. Individuals under the age of 25 who are HIV-infected are significantly less likely than older adults to seek HIV care which is thought to be, in part, due to low levels of testing, knowledge of HIV status, and perception of risk.3
According to the spring 2012 American College Health Association National College Health Assessment (ACHA-NCHA), nearly 71% of students reported sexual activity within the last year, while only 27.1% reported ever being tested for HIV.7 College students whose behavior puts them at increased risk of HIV infection (i.e. participating in sexual activity without condoms, using condoms infrequently, having multiple sex partners, etc.) are ideally the persons who should be tested for HIV.8,9 As a population, college students continually practice behaviors that place them in the targeted high risk group, increasing their susceptibility to HIV. Among individuals who choose to be sexually active, consistent and correct condom use is the only reliable method of HIV prevention. Unfortunately rates of consistent condom use during all sexual acts among college students group continue to be low.9 Of the nearly 71% of college students who reported sexual activity within the last year, 45% reported one partner within the past 12 months, 10% two partners, and 16% three or more partners. The mean number of partners among students reporting at least one sexual partner within the last 12 months was 2.2 (SD=3.63), with males reporting more partners (M=2.7, SD=4.8) than females (M=1.9, SD=2.4).7 Among those students who were sexually active, 5.7% used a condom or other protective barrier within the last 30 days mostly or always during oral sex, 29.2% during anal sex, and 50.3% during vaginal sex.7 Clearly these students continue to put themselves at risk for increased susceptibility for HIV and other STIs considering their sexual health behaviors.
However, studies find that college students typically recognize high risk behavior of their peers, but their own perceived susceptibility of HIV infection remains low.9,10 Similarly, rates of HIV testing among persons most at risk of infection are generally low as well.11 Approximately 60% of HIV-infected youth ages 13–24 are unaware of their infection.3 Over 50% of new HIV infections (via sexual transmission) are reported by individuals who are HIV-infected but unaware of their status because they have not been tested for HIV,2 further reinforcing the lack of perceived susceptibility and perceived seriousness. Fortunately, HIV incidence rates have remained relatively stable in recent years and show evidence of decreasing in certain populations, but the least amount of progress has been in preventing sexual transmission of HIV, with youth ages 13–24 at greatest risk.6
Safer sexual health promotion interventions provide cues to action to influence an individual’s perception of risk and ultimately self-efficacy, one’s ability to take action.5 Unfortunately, these interventions have been found to have limited effectiveness in increasing college student’s perceived susceptibility or severity of HIV infection and associated behavior change to practice consistent, safe sexual behaviors.9 Public health experts agree that in addition to prevention measures, early detection of HIV has been successful in preventing future incidence.6 Within the college student population, high rates of sexual activity, low rates of consistent condom use, and low rates of HIV testing are consistent trends that continue to pose a threat to public health on college campuses and challenges to health practitioners.12 In 2006, the CDC released revisions to their recommendations for HIV testing to include universal opt-out testing for all adults in medical settings and a targeting of high-risk individuals to be tested annually.6 The CDC recommendations for HIV testing could greatly benefit college campuses considering the decreased perceived susceptibility and related lack of testing.
Various studies have examined college students’ awareness and knowledge of HIV and modes of basic transmission. General conclusions are consistent; as a group, college students are knowledgeable about how HIV is spread and how to prevent infection but continue to practice risky sexual behaviors that increase personal risk of HIV transmission.9 HIV related research examining the college student population in the United States is limited. While risk prevention efforts continue to be focused on historically affected groups, the college student population as a whole has traditionally been considered a group at low risk for HIV infection.9 Considering the broad reach of college campuses, further exploration of this diverse population is necessary to better understand possible profiles of college students most and least likely to seek HIV testing. 13 Results can be used to assist college health promotion professionals in the design and implementation of tailored inventions to evoke behavior change. Literature suggests that the framing of messages can impact efficacy. Providing personally relevant messages may deepen message processing and persuasion, leading to increased rates of compliance to recommendations for HIV testing among college students.14
Therefore, the purpose of this study was to summarize the prevalence of HIV testing in a sample of college students and further explore the associated demographic and behavioral characteristics of college students with low and high rates of HIV testing. Exploring such differences in HIV testing rates and associated risk factors will enlighten college health professionals as they develop future intervention strategies.
Methods
Participants
Study participants were sampled from a large Southeastern university. The university registrar provided a list of 7,183 randomly selected students age 18 or older from the total study population of approximately 28,000 students that were registered for the fall 2011 semester. A total of 1,103 students completed the general health behavior survey, yielding a response rate of 15.4%. Due to the deidentified nature of the data received from the registrar, it was not possible to determine the difference between non-responders and responders of the survey.
Procedures
The study was approved by the Institutional Review Board of the University. Potential participants were invited to participate in the study via cover letter sent to their official University email account explaining the purpose of the study, the importance of participating, and explanation that completion and submission of the online survey through the external link implied consent to participate. As an incentive to encourage participation, all respondents who completed the survey were prompted to a separate entry form link to enter into a drawing to win a commemorative basketball signed by the University’s head basketball coach.
The survey and entry form were administered through Qualtrics (Qualtrics Labs, Inc. Provo, UT), which assigned potential participants a code as an identifier to protect the confidentiality of participant responses. Returned surveys were identified by this code and reminder emails from survey codes not returned were sent a follow up email one week after the initial email outreach. After the second survey email reminder, another week was given to complete the survey. Surveys not returned after two weeks were considered non-responders and further follow-up was not made.
Measures
The instrument used in this study was an adaptation of previous surveys performed at the University which used the ACHA-NCHA as a framework for question development. The ACHA-NCHA was developed by an interdisciplinary team of college health professionals and is considered “both reliable and valid and of empirical value for representing the nation’s student.”15 University health professionals, including clinicians, student health service personnel, health promotion faculty members, and data analysis consultants provided input on items to include in the developed measure. The resulting survey included 46-items in an effort to examine student habits, behaviors, and perceptions on prevalent health topics to aid the development of prevention and health promotion programming efforts. The survey included questions related to sleep habits, eating and body image, gambling, stress, sexual health, along with demographic characteristics. For purposes of this study, researchers used a subset of survey items to explore the relationship between HIV testing and a number of demographic factors along with sexual behavior variables. Demographic measures included 9-items: gender, age, race/ethnicity, student status, student athlete, involvement in Greek organizations, living on/off campus, relationship status, and sexual orientation. Nine items assessed self-reported sexual health, including number of sexual partners within the last 12 months, sexual behavior within the past 30 days, history of HIV and STI testing, and contraception use. Three items assessed number of sexual partners in the last 12 months for anal, oral, and vaginal sex. Response options were collapsed into three categories: N/A, one, and two or more. Three items assessed participant condom use in the past 30 days for anal sex, oral sex, and vaginal sex. Response options were collapsed into three categories: N/A, no sexual activity in past 30 days; never, rarely, sometimes; most of the time, always. Two items assessed if participants had ever tested positive for a STI or HIV, with categorical response options of yes, no, not sure, N/A – have never been tested. Participants were also asked if they used birth control the last time they had vaginal sex, with a variety of options given. Responses were combined into four categories: condoms only (male condoms, female condoms), hormonal only (birth control pill, Depo-Provera, IUD, patch, vaginal ring), other/none (natural family planning, withdrawal, none, do not know what my partner used for birth control), condom and hormonal.
The survey was pilot tested with a group of ten college students to determine readability, content validity, length of completion, and formatting issues. Students in a health promotion class were given the Qualtrics survey link and asked to review, considering both content and format. Feedback was incorporated into the final, IRB-approved instrument utilized in this study. On average, students took 15–20 minutes to complete the entire online survey.
Data Analysis
Students were identified as being sexually active if they indicated sexual activity (oral, anal, or vaginal) in the last 12 months. Those who were not sexually active and those whose data were missing regarding HIV testing were removed from the analysis, resulting in a sample size of 905. All categorical variables were described with counts and percentages. The continuous variables were summarized with means and standard deviation. The binary measure remained constant (ever having an HIV test) and comparisons of categorical variables were analyzed by chi-square tests of independence while continuous variables were analyzed for significance through a two-sample t-test. To measure the prevalence ratio in cross-sectional studies with binary outcomes, multiple logistic regression is a common tool to use in the epidemiological literature. Therefore, multiple logistic regression was used to investigate demographic characteristics associated with the binary variable HIV testing (yes/no). Crude and adjusted odds ratios are presented with 95% confidence intervals (Table 2).
Table 2.
Crude and Adjusted Odds Ratios for Demographic Variables
| Odds Ratios (95% Confidence Interval) | |||
|---|---|---|---|
| Factors | Categories | Unadjusted | Adjusted |
| Age | 0.91 (0.89, 0.93) | 1.1(1.07, 1.12) | |
| Sexual orientation | Bisexual/gay/lesbian | reference | reference |
| Heterosexual | 0.30 (0.19, 0.47) | 0.32(0.19, 0.51) | |
| Gender | Male | reference | reference |
| Female | 1.35 (1.04, 1.76) | 1.35(1.01, 1.79) | |
| Race | White | reference | reference |
| Non-white | 1.62 (1.13, 2.32) | 1.55(1.05, 2.28) | |
Classification regression tree (CART), a form of binary recursive partitioning, is a statistical tool widely used to identify high-risk groups by classifying observations into partitions with and without the target outcome based on a series of select independent variables.16 In choosing the best variable to split, the method seeks the variable with the best splitting value among all possible values to maximize the “impurity” of the divided sample. The most common splitting criterion is the “Gini” index. Once the variable and the splitting value are chosen, the entire sample is divided (into nodes). This process continues and branches out for each subsample until the stopping rule is applied. Given the hierarchical nature of the model, combinations of factors can be easily discerned using a tree-like plot. It can efficiently identify interactions among explanatory variables.17 To better understand factors that were related with rates of HIV testing, CART analysis was utilized to divide the sample into groups based on common characteristics likely to influence HIV testing. Comparisons were then made between the group with the lowest rates of HIV testing and the remaining sexually active students. P-values less than or equal to 0.05 were considered statistically significant for all statistical tests. CART analysis was performed using RStudio and all other analyses were performed using SAS v9.3.
Results
Characteristics of the Sample
Table 1 provides the overall demographic information for the sample. The mean age of participants was 26.4 (SD = 6.4), 61.3% (n = 554) were female and over half (n = 537, 59.5%) were graduate/professional students. Nearly half (n = 373, 41.3%) reported relationship status as being in a committed relationship and living with a partner or married. A majority of the sample reported ethnic affiliation as White (n = 790, 87.4%) and heterosexual sexual orientation (n = 827, 92.2%).
Table 1.
Relationship Between HIV Testing and Demographic Characteristics
| Total (N=905) | HIV testing (N=328) | No (N=577) | p-value | |
|---|---|---|---|---|
| Mean Age (SD) | 26.35 (6.41) | 28.76 (7.03) | 25.00 (5.60) | <.0001 |
| Gender | 0.1723 | |||
| Male | 350 (38.7%) | 117 (35.8%) | 233 (40.4%) | |
| Female | 554 (61.3%) | 210 (64.2%) | 344 (59.6%) | |
| Ethnic Background | 0.0045 | |||
| White | 790 (87.4%) | 273 (83.2%) | 517 (89.8%) | |
| Non-white | 114 (12.6%) | 55 (16.8%) | 59 (10.2%) | |
| Sexual Orientation | <.0001 | |||
| Bisexual/Homosexual | 70 (7.8%) | 42 (12.9%) | 28 (4.9%) | |
| Heterosexual | 827 (92.2%) | 283 (87.1%) | 544 (95.1%) | |
| Relationship Status | <.0001 | |||
| Single (never married) | 237 (26.2%) | 80 (24.4%) | 157 (27.3%) | |
| In a relationship but not living together | 267 (29.5%) | 81 (24.7%) | 186 (32.3%) | |
| In a relationship and living together/Married | 373 (41.3%) | 147 (44.8%) | 226 (39.2%) | |
| Separated/Divorced/Widowed | 27 (3.0%) | 20 (6.1%) | 7 (1.2%) | |
| Academic status | 0.2402 | |||
| Undergraduate Student | 365 (40.5%) | 124 (37.9%) | 241 (41.9%) | |
| Graduate/Professional Student | 537 (59.5%) | 203 (62.1%) | 334 (58.1%) | |
| Fraternity/Sorority | 0.0046 | |||
| Yes | 159 (17.6%) | 42 (12.8%) | 117 (20.3%) | |
| No | 744 (82.4%) | 285 (87.2%) | 459 (79.7%) | |
| Living | 0.5607 | |||
| On campus | 32 (3.5%) | 10 (3.1%) | 22 (3.8%) | |
| Off campus | 871 (96.5%) | 316 (96.9%) | 555 (96.2%) |
Relationship Between HIV Testing and Demographic Characteristics
More than one-third of the college students (n = 328, 36.2%) reported ever having been tested for HIV. Table 1 summarizes HIV testing status in relation to demographic variables. Multiple logistic regression was employed to further analyze demographic variables while controlling for the effect of all demographic variables. Crude and adjusted odds ratios are presented with 95% confidence intervals (Table 2). Although gender was not significant at the selected alpha of 0.05, females were 1.4 times more likely than males (aOR=1.35, 95% CI 1.01 to 1.79) to have been tested for HIV. Age was significantly associated with HIV testing status (p <0.0001). The mean age of students who had been tested indicated that a higher proportion of older students (M = 28.76, SD = 7.03) sought testing while a higher proportion of younger students (M = 25.00, SD = 5.60) had not been tested (aOR=1.07, 95% CI 1.07 to 1.12). Also significantly associated with HIV testing was relationship status (p <0.0001); this was divided into four categorical response options based on level of commitment (as displayed in Table 1). Students in a more committed relationship currently or who had been married previously (in a relationship and living together/married or separated/divorced/widowed) reported higher testing rates (n = 167, 42%) than students who had never been married and were less committed (single or in a relationship but not living together) (n = 161, 32%). Additionally, sexual orientation was significantly associated with HIV testing, (p < 0.001), finding that heterosexuals were 32% more likely to have been tested than homosexuals/bisexuals (aOR=.32, 95% CI .19 to .51). Respondents who declared ethnic affiliation as non-white were 1.6 times more likely to be tested than white respondents (aOR=1.55, 95% CI 1.05 to 2.28).
Relationship Between HIV Testing and Sexual Behaviors
Table 3 describes the relationship between HIV testing status and sexual activity, number of sexual partners, and condom use while engaged in oral, anal, and vaginal sexual activity. Students who reported ever having been tested for HIV were compared to students who had not been tested to determine if there were differences regarding sexual behaviors and testing status.
Table 3.
Relationship Between HIV Testing and Sexual Behaviors
| Total (N=905) | HIV testing (N=328) | No (N=577) | p-value | |
|---|---|---|---|---|
| STI testing positive: | <.0001 | |||
| N/A; have never been tested | 97 (10.7%) | 2 (0.6%) | 95 (16.5%) | |
| Yes | 118 (13.1%) | 73 (22.4%) | 45 (7.8%) | |
| No | 681 (75.4%) | 249 (76.4%) | 432 (74.9%) | |
| Not sure | 7 (0.8%) | 2 (0.6%) | 5 (0.9%) | |
| In past 30 days used condom or dental dam during anal sex: | 0.0037 | |||
| N/A, No activity in past 30 days | 787 (88.4%) | 278 (85.5%) | 509 (90.1%) | |
| Never/Rarely/Sometimes | 87 (9.8%) | 35 (10.8%) | 52 (9.2%) | |
| Most of the time/Always | 16 (1.8%) | 12 (3.7%) | 4 (0.7%) | |
| In past 30 days used condom or dental dam during oral sex: | 0.1730 | |||
| N/A, No activity in past 30 days | 406 (45.6%) | 136 (42.1%) | 270 (47.5%) | |
| Never/Rarely/Sometimes | 478 (53.6%) | 183 (56.7%) | 295 (51.9%) | |
| Most of the time/Always | 7 (0.8%) | 4 (1.2%) | 3 (0.5%) | |
| In past 30 days used condom or dental dam during vaginal sex: | 0.0744 | |||
| N/A, No activity in past 30 days | 283 (31.6%) | 111 (34.3%) | 172 (30.1%) | |
| Never/Rarely/Sometimes | 351 (39.2%) | 133 (41.0%) | 218 (38.1%) | |
| Most of the time/Always | 262 (29.2%) | 80 (24.7%) | 182 (31.8%) | |
| Partners you had anal sex with in last 12 months: | 0.0006 | |||
| N/A | 724 (82.7%) | 247 (77.7%) | 477 (85.6%) | |
| 1 | 126 (14.4%) | 54 (17.0%) | 72 (12.9%) | |
| 2 or more | 25 (2.9%) | 17 (5.3%) | 8 (1.4%) | |
| Partners you had oral sex with in last 12 months: | 0.0947 | |||
| N/A | 108 (12.2%) | 34 (10.7%) | 74 (13.1%) | |
| 1 | 586 (66.4%) | 203 (64.0%) | 383 (67.7%) | |
| 2 or more | 189 (21.4%) | 80 (25.2%) | 109 (19.3%) | |
| Partners you had vaginal sex with in last 12 months: | 0.0391 | |||
| N/A | 51 (5.7%) | 24 (7.5%) | 27 (4.7%) | |
| 1 | 638 (71.5%) | 214 (66.7%) | 424 (74.3%) | |
| 2 or more | 203 (22.8%) | 83 (25.9%) | 120 (21.0%) | |
| Birth control last time you had vaginal sex: | 0.0158 | |||
| Condoms only (Female condoms, male condoms) | 141 (15.6%) | 49 (14.9%) | 92 (15.9%) | |
| Hormonal Only (Birth control pill, Depro-Provera, IUD, Patch, vaginal ring, spermicide | 231 (25.5%) | 84 (25.6%) | 147 (25.5%) | |
| Others/None only (Natural family planning, withdrawal, none, do not know what my partner used for birth control) | 153 (16.9%) | 72 (22.0%) | 81 (14.0%) | |
| Condom and hormonal | 380 (42.0%) | 123 (37.5%) | 257 (44.5%) |
Sexual behavior questions were reported by type of sexual activity. Although many of the students were not participating in anal sex (n = 724, 83%), participation in the past 12 months (p = 0.006) and condom use while engaging in anal sex activity in the past 30 days (p = 0.0037) were found to be significantly associated with HIV testing. Among the students who did report anal sex activity within the last 30 days (n =103), only 15.5% (n = 16) reported using a condom most of the time/always. Safer sex behaviors while engaged in anal sexual activity did lead to increased rates of testing. While 40% (n = 35) of students who reported inconsistent condom use had been tested, 75% (n = 12) who used a condom consistently reported having been tested. Also, as number of anal sex partners in the last 12 months increased from one partner (n = 126), to two or more (n = 25), so did rates of HIV testing (43% and 68% respectively).
Vaginal sexual activity in the past 12 months (p =0.039) and birth control method the last time engaging in vaginal sexual activity (p =0.016) were additional sexual behavior characteristics found to be significantly associated with having been tested for HIV. Most students reported one vaginal sex partner within the last 12 months (n = 638, 71.5%) and 22.8% (n = 203) reported having more than one. Associated HIV testing rates also increased as number of partners within the last 12 months increased from one (n = 214, 34%) to two or more (n = 83, 41%,). Although not significant at alpha of 0.05, consistent condom use rate was higher for vaginal sex than in anal or oral sexual activities. Two-thirds of the college students (n = 613, 68.4%) reported vaginal sexual activity within the past 30 days, and nearly half (n = 262, 42.7%) reported using a condom most of the time/always, while over half (n = 521, 57.7%) reported condom use the last time they engaged in vaginal sexual activity. Consistent condom use while engaging in vaginal sex activity was not, however, associated with increased rates of HIV testing. Rates of HIV testing among students who reported consistent condom use during vaginal sex activities were 31% (n = 80) while testing rates for those who reported inconsistent condom use were 38% (n = 133).
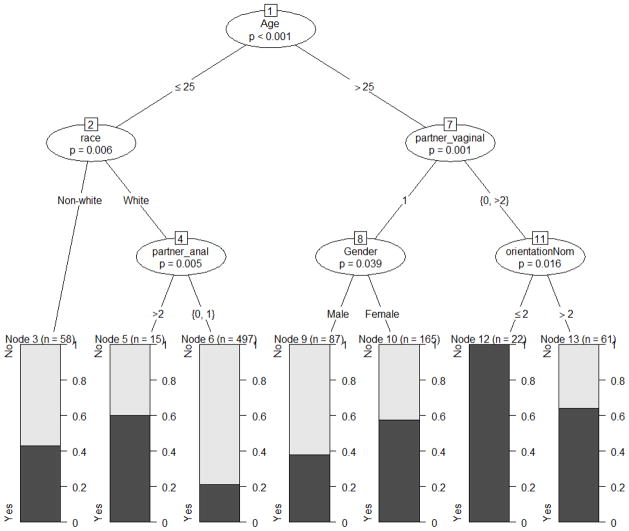
CART analysis, displayed in Figure 1, found that age had the greatest impact on probability of HIV testing. Factors related to HIV testing among respondents 18–25 years of age were race and anal sex activity. Factors related to HIV testing among respondents older than 25 years of age were vaginal sex activity, female gender, and heterosexual orientation. Node 6 displays the group having the lowest rates of HIV testing; characteristics included respondents who were 25 years of age or younger, declared ethnic affiliation as White, and had zero to one anal sex partners in the past 12 months. Node 12 displays the group having the highest rates of HIV testing; characteristics included respondents over the age of 25, those with zero or at least two vaginal sex partners within the last 12 months, and homosexual/bisexual sexual orientation.
Figure 1.
Group Profiles in Relation to HIV Testing Rates
Comment
This study explored differences in risk factors among the college student population at a large Southeastern university and examined characteristics associated with low rates of HIV testing. Measuring the prevalence ratio of HIV testing among college students, the group with the lowest levels of testing were younger students, indicating a need for HIV testing interventions. Latest reports from the CDC confirm that adolescents and young adults are becoming infected with HIV at the highest rates3 and although prevention of infection is the ultimate goal, the reality is that intervention by way of education to increase HIV knowledge and safer sex practices may be coming too late for college students. As a population, college students are likely to be sexually active and at a developmental stage where they see themselves as invincible, rendering them blind to any negative consequences of their behaviors.9 This might hold particularly true in the case of HIV infection that might not manifest for many years after exposure.
The observed prevalence of ever having an HIV test among this sample was 36.2% which was somewhat higher than the 27% reported in the most recent results of the NCHA assessment.7 However, within this study, among the group with the lowest rates of HIV testing (Figure 1, Node 6), only 21% had ever been tested. These overall campus rates are low considering the CDC’s recommendations for HIV testing.6 Demographic characteristics found to be associated with lower levels of HIV testing and thereby increased risk of HIV infection were students who reported gender as male, sexual orientation as homosexual/bisexual, and students in a less committed relationship. Consistent with previous research, similar gender differences in HIV testing have been found,4,8,11,12 implicating an increase in risk for HIV considering that men account for 73% of all new HIV infections in the United States annually.8 It is not clear from this study why males were less likely to get tested, however, future HIV awareness efforts may benefit targeting college males. In the general population, men who have sex with men (MSM) accounted for 78% of all new HIV infections among males and 63% of all new infections in 2010,1 rendering male homosexual/bisexual students at higher risk of HIV infection. This reinforces the need for continued outreach to increase HIV testing in male and homosexual/bisexual college student subpopulations. Future research should investigate the perceptions of HIV testing among both heterosexual and homosexual/bisexual students on college campuses.
Although women reported higher rates of HIV testing, only 64% of the sexually active college women in this study reported being tested. This underscores the fact that 1/3 of these sexually active women were not being tested. Typically, women may be more likely to get tested for HIV because they associate it with medical practices, such as pelvic exams, pregnancy-related issues, and STIs.18 Future research is warranted to determine rationale for college women to seek out HIV testing. Is it because it is already included in women’s yearly exams or are college women who are at risk due to their sexual behaviors being tested for HIV as a means of protection? Studies have found that although college students consider HIV testing as a means to protect against HIV, many are concerned that discussing HIV or HIV testing would be seen as accusing their partner of cheating or being promiscuous.19 Few studies have addressed barriers reported by college students related to HIV testing. Barriers tend to include fears about privacy protection, the stress of waiting for the test result, and fear of a positive test result and what that would potentially mean for a current relationship.19 Female college students may have increased propensity for such barriers, which may translate to an understanding of why 1/3 of college females are not being tested for HIV. Clearly it is important to target both males and females on college campuses, but it is necessary to understand what factors influence the decision to be tested for HIV among both groups.
While relationship status alone does not pose an increased risk of HIV infection and one cannot presume that students in a more committed relationship are mutually monogamous, multiple lifetime sex partners and inconsistent condom use do increase HIV risk.6 The CDC recommends repeat HIV testing for individuals who themselves or whose sex partners have had more than one sex partner since their most recent HIV test.6 Sexual risk behaviors among college students in this study were also consistent with previous research, indicating that students use condoms roughly half of the time during vaginal sex and report much lower consistency rates while engaging in oral and anal sex.9 Findings in this study show that students who have inconsistent condom use practices generally reported lower rates of HIV testing than students who used condoms consistently, indicating that students at higher risk are less likely to report HIV testing. This is in contrast to previous reports that individuals engaging in high-risk sexual behaviors such as having sex without condoms or using condoms infrequently are more likely to get tested for HIV.12, 20
A positive association between increased number of sex partners (two or more) and increased rates of HIV testing was found, indicating that those at highest risk based on number of sex partners within the last 12 months are more likely to report being tested but those who are sexually active and had one sex partner in the past 12 months continue to report lower rates of testing. These findings were consistent with previous research indicating having a greater number of sexual partners increased the likelihood for college students to get tested for HIV.11, 21 Although repeat HIV testing information was not gathered in this study (i.e. HIV testing before entering a relationship, HIV testing since last sex partner), gathering such information will provide researchers further insight into common characteristics and risk factors associated with sexual behaviors related to HIV testing within the college student population.6
Results of this study demonstrate diversity that exists within the larger college student population and differences among subpopulations do influence HIV risk factors compliance with HIV testing. Findings from this study show that students continue to practice high-risk sexual behavior at high rates and students at moderate or high risk maintain lower rates of HIV testing. Younger students in particular are at increased risk due to lower rates of HIV testing and should be classified as a risk group in need of targeted HIV testing outreach. However, Mattson and colleagues20 found that both those students who sought HIV testing and those who did not seek testing were at risk for HIV due to their mistaken perception of decreased susceptibility and severity and their related risky sexual behaviors.
Future research is warranted to understand the settings in which college students are likely to seek HIV testing.22 Anastasi and colleagues reinforced the importance of HIV testing on college campuses, with 73% of the individuals seeking voluntary testing stating they would not have sought an HIV test had it not been offered through the college health center. These findings have been found previously in a sample of college students, with students indicating they would be more likely to seek testing if available on campus.23 Partnerships between on-campus health clinics and college health promotion professionals need to be established to address barriers to HIV testing among at risk college students. HIV testing can be used as a prevention tool, an opportunity for education and discussion on risky sexual behaviors on the college campus.20 By emphasizing and personalizing the risk of HIV infection, campus health professionals can encourage positive sexual health behavior choices and empower students to take responsibility for their own protective behaviors.22
Limitations
This study is not without limitations. Results are limited by the validity of the self-reported measures. Previous research indicates sexual history is subject to social desirability bias and memory.11 However, individuals were invited to participate via an online survey, potentially decreasing the need to respond in a socially desirable way on information that could be deemed confidential and private. Participants were also recruited from one university, and although the overall sample size was large, the response rate was only 15%. This is typical of online surveys without large incentive pools. A majority of the sample was White and heterosexual, however, this is in line with the demographic characteristics of the university. A high percentage of the sample were also graduate students and older than in other studies of college students. This makes it difficult to generalize to the larger ‘college population’ and limits the external validity of the study. Future research should be conducted on demographically-diverse college campuses to investigate the number of students being tested for HIV and the associated individual, social, and environmental factors influencing this decision.
Conclusions
This study provides further evidence that future interventions among college students should include HIV testing as a method to improve early detection rates. In addition, this HIV testing time should capitalize on the opportunity to also educate college students on overall sexual health promotion. Research has shown that being tested for HIV can act as a cue to action as students are more likely to reevaluate their health beliefs and improve their risky sex behaviors.9 Targeted interventions and awareness campaigns may be an effective strategy to emphasize HIV testing services and increase testing compliance as recommended by the CDC.6 Future research is necessary to evaluate barriers and benefits to HIV testing from the perspective of college students. Without such research, the prevalence of HIV and related risky sexual behaviors will continue to rise.
Acknowledgments
Funding
This study was supported by the Applied Statistics Lab and the Center for Clinical and Translational Science (CCTS) at the University of Kentucky. The CCTS is supported by grant number UL1RR033173 from the National Center for Research Resources (NCRR), funded by the Office of the Director, National Institutes of Health (NIH) and supported by the NIH Roadmap for Medical Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of NCRR and NIH.
References
- 1.Centers for Disease Control and Prevention. [Accessed March 2012.];HIV in the United States: At a glance. http://www.cdc.gov/hiv/pdf/statistics_basics_factsheet.pdf. Published February 2013.
- 2.U.S Department of Health and Human Services. HIV. Healthy People 2020. 2012 http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=22.
- 3.Centers for Disease Control and Prevention. [Accessed November 2012.];More than half of young HIV-Infected Americans are not aware of their status. http://www.cdc.gov/nchhstp/newsroom/2012/Vital-Signs-PressRelease.htmlPublished November 27, 2012.
- 4.Centers for Disease Control and Prevention. Vital signs: HIV infection, testing, and risk behaviors among youths – United States. MMWR Morb Mort Wkly Rep. 2012;61(RR-47):971–976. [PubMed] [Google Scholar]
- 5.Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education. 3. San Francisco: Jossey-Bass; 2002. [Google Scholar]
- 6.Centers for Disease Control and Prevention. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Morb Mort Wkly Rep. 2006;55(RR-14):1–17. [PubMed] [Google Scholar]
- 7.American College Health Association. American College Health Association-National College Health Assessment II: Reference Group Executive Summary. Hanover, MD: American College Health Association; Spring. 2012. [Google Scholar]
- 8.Calderia KM, Singer BJ, O’Grady KE, Vincent KB, Arria AM. HIV testing in recent college students: Prevalence and correlates. AIDS Edu Prev. 2012;22(4):363–376. doi: 10.1521/aeap.2012.24.4.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewis JM. HIV risk behavior among college students in the United States. Coll Stud J 2009. 2009;43(2):475–491. [Google Scholar]
- 10.Buhi ER, Marhefka S, Hoban MT. The state of the union: Sexual health disparities in a national sample of US college students. J Am Coll Health. 2010;58(4):337–346. doi: 10.1080/07448480903501780. [DOI] [PubMed] [Google Scholar]
- 11.Crosby RA, Miller KH, Staten RR, Noland M. Prevalence and correlates of HIV testing among college students: An exploratory study. Sex Health. 2005;2:19–22. doi: 10.1071/sh04047. 2005. [DOI] [PubMed] [Google Scholar]
- 12.Bontempi J, Mugno R, Bulmer SM, Danvers K, Vancour ML. Exploring gender differences in the relationship between HIV/STD testing and condom use among undergraduate college students. Am J Health Educ. 2009;40(2):97–105. doi: 10.1080/19325037.2009.10599084. [DOI] [Google Scholar]
- 13.Erin W, Moore MA. Human immunodeficiency virus and chlamydia/gonorrhea testing among heterosexual college students: Who is getting tested and why do some not? J AM Coll Health. 2013;61(4):196–202. doi: 10.1080/07448481.2013.789880. [DOI] [PubMed] [Google Scholar]
- 14.Norton WE, Fisher JD, Amico R, Dovidlo D, Johnson B. Relative efficacy of a pregnancy, sexually transmitted infection, or human immunodeficiency virus prevention-focused intervention on changing sexual risk behavior among young adults. J AM Coll Health. 2012;60(8):574–582. doi: 10.1080/07448481.2012.721428. [DOI] [PubMed] [Google Scholar]
- 15.American College Health Association National College Health Assessment. [Accessed November 2013.];Generalizability, reliability, and validity analysis. http://www.acha-ncha.org/grvanalysis.html. Published 2013.
- 16.Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and Regression Trees. Chapman & Hall (Wadsworth, Inc.); New York: 1984. [Google Scholar]
- 17.De’ath, Glenn, Fabricius KE. Classification and regression trees: A powerful yet simple technique for ecological data analysis. Ecology 2000. 2000;81(11):3178–3192. [Google Scholar]
- 18.Lear D. Sexual communication in the age of AIDS: The construction of risk and trust among young adults. Soc Sci Med. 1995;41(9):1311–1323. doi: 10.1016/0277-9536(95)00010-5. [DOI] [PubMed] [Google Scholar]
- 19.Hammer JC, Fisher JD, Fitzgerald P. When two heads aren’t better than one: AIDS risk behavior in college-age couples. J Applied Social Psychol. 1996;26(5):375–397. [Google Scholar]
- 20.Mattson M. Impact of HIV tests counseling on college students’ sexual beliefs and behaviors. Am J Health Behav. 2002;26(2):121–136. doi: 10.5993/ajhb.26.2.5. [DOI] [PubMed] [Google Scholar]
- 21.Thomas PE, Voetsch AC, Song B, Calloway D, Goode C, Mundey L, Nobles J, Heffelfinger JD. HIV risk behaviors and testing history in historically black college and university settings. Public Health Reports. 2008;123(S3):115–125. doi: 10.1177/00333549081230S314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anastasia MC, Sawyer RG. A Descriptive Analysis of Students Seeking HIV Antibody Testing at a University Health Service. J Am Coll Health. 1999 Jul;48(Issue 1):p137p. doi: 10.1080/07448489909595667. [DOI] [PubMed] [Google Scholar]
- 23.Hayden J. HIV testing on campus. J Coll Stud Dev. 1994;35:208–211. [Google Scholar]