Abstract
Objectives
Recent evidence suggests that children are increasingly diagnosed with bipolar disorder, yet no studies have quantified treatment costs for pediatric patients. The objectives are to identify one-year health services utilization and treatment costs among youth with new bipolar diagnoses.
Methods
MarketScan administrative claims from 2005–2007 were used to construct a retrospective person-level cohort of children ages 0–17 to identify one-year health services utilization and costs among privately insured youth with bipolar diagnoses. Inpatient and outpatient services were categorized as mental health related and non-mental health related. Pharmacy costs were classified as psychotropic or non-psychotropic.
Results
In the sample (N=4,973), one-year mean reimbursements for health services were $10,372, and patient out-of-pocket spending $1,429 per child. Mental health services comprised 71% of all health care spending, with psychotropic medications and inpatient care contributing the largest proportions of total spending (24% and 27%, respectively).
Conclusions
The costs of care among privately insured children with bipolar disorder are similar to that of adults. However, spending on children is concentrated on mental health related services. Because private insurance plans have historically limited mental health service benefits, the concentration of spending on mental health services may place a greater burden on families for out of pocket payments. As mental health parity is adopted by private insurers it will be important to monitor the impact on patient utilization and costs of health services, particularly for children with severe mental illness.
Keywords: Bipolar Disorder, Utilization, Expenditures, Children, Pharmacotherapy, Epidemiology
INTRODUCTION
Bipolar disorder is a chronic affective disorder that results in substantial impairments. According to the World Health Organization, bipolar disorder is ranked sixth among all medical disorders in years of lost life due to death or disability,(1) and it has been consistently rated among the top causes of disability adjusted life years for 15–44 year olds in developed countries.(2) Individuals with bipolar disorder generally experience a chronic, recurrent course of illness that increases their risk of lifelong disability and greatly impacts their lives and the lives of their families.(3)
Once considered rare in children, recent studies have indicated a sharp increase in the number of children diagnosed with bipolar disorder in both inpatient and outpatient settings.(4–8) Children with bipolar disorder have significantly higher rates of morbidity and mortality than children without the disorder,(9) including psychosocial morbidity, impaired academic performance, impaired social and familial support, increased levels of substance abuse, weight problems, legal difficulties, and hospitalizations.(10–14) Although the criteria for diagnosing and the use of the bipolar diagnostic label among children with non-classical symptom presentations is a matter of clinical debate, (14, 15) a growing number of children over recent years have received these diagnoses and related treatment.
In addition to the enormous personal and familial burden, the economic impact of bipolar disorder is extremely high, particularly when accounting for the opportunity costs of living with a mental illness.(16) In fact, a 2003 study found that bipolar disorder was the most expensive behavioral health care diagnosis for both patients and their insurance plans.(17) Since over 90% of patients with bipolar disorder suffer recurrences and many experience progressive deterioration in functioning,(18) it is important to consider the financial impact of this disease from both the family and the health plan’s perspective.
The costs related to treating children with bipolar spectrum disorders are likely to differ from adults. No cost-related study in bipolar disorder (19–25) has focused on children. Additionally, only two studies used data from 2003 or later.(19, 25) This is a critical limitation for several reasons. First, during the past decade, there has been a dramatic increase in the diagnostic prevalence among children. Second, there has been a growth in psychotherapeutic options for treatment (e.g., second-generation antipsychotics, anticonvulsants). Finally, inpatient lengths of stay among patients with mental illness, including children, has also decreased, (7) suggesting that costs for bipolar treatment may have shifted from inpatient to outpatient care.
Research has also found that families with private health insurance are more likely to be underinsured and report inadequate coverage of needed services, especially families of children with special health care needs.(26) Given that private health insurance remains the dominant payer for childrens’ mental health and hospital services,(27) estimating service use and costs of treatment for privately insured youth with bipolar disorder will help to quantify the impact of this disorder on children, their families, and the health care system. The objectives are to identify utilization patterns and estimate health plan payments for inpatient, outpatient and pharmacy services among privately insured children with bipolar disorder diagnoses.
METHODS
Data Source
A longitudinal retrospective person-level cohort study was conducted using data from the Thomson Reuters MarketScan database (Copyright © 2009 Thomson Healthcare Inc. All Rights Reserved). These data include de-identified clinical utilization and expenditures information for inpatient, outpatient and pharmacy services for approximately 35 million Americans insured by some 100 payers.
Sample Selection
Children (ages 0–17 years) were included if they had 1 inpatient or at least 2 outpatient insurance claims for a bipolar spectrum disorder (on separate service dates) from January 1, 2005 through December 31, 2007. Diagnostic and Statistics Manual for Mental Illness, Fourth Edition codes were mapped to the respective International Classification of Diseases, Ninth Edition (ICD-9) codes to identify claims for a bipolar spectrum disorder (ICD-9-CM: 296.0, 296.1, 296.4–296.8, or 301.13).(28–30)
To assess prior diagnoses and to allow for continuous follow-up, children were required to have at least one of their bipolar diagnoses between July 1, 2005 and December 31, 2006 (hereafter called the index diagnosis date). Children with incident and prevalent diagnoses who were continuously enrolled for 180 days prior to and 365 days following their index diagnosis date were included (N = 7,119). From this sample, children with conditions that mimic symptoms of mania, (multiple sclerosis, hyperthyroidism, closed or open head injury, lupus), require a bipolar-related treatment (epilepsy), or complicate bipolar disorder treatment (pregnancy) (11, 31) were excluded, as were children with schizophrenia, pervasive developmental disorders, mental retardation, or substance abuse disorders in the 180 days prior to their first bipolar diagnosis (n = 1,011).(32) Finally, children whose insurance plans did not provide information on medication use were excluded to differentiate between non-use and non-reporting of medications (n = 1,135).
Study Variables
Inpatient and Outpatient Service Utilization and Cost Classification
Using inpatient and outpatient service claims associated with the primary ICD-9 code, each claim was classified as being related to mental health conditions, including bipolar disorder (ICD-9 codes 290.00–319.99); or non-mental health conditions (all other ICD-9 codes). To avoid overestimating the number of visits received by children in the cohort we excluded duplicate claims on the same service date and outpatient visits during which only laboratory services were provided (CPT codes 80048 through 89356). However, charges for all services received, including laboratory claims, were included in cost estimates. Mean patient out-of-pocket costs and mean total health costs were estimated among children in the sample. Patient out-of-pocket costs were calculated as the sum of copayments, coinsurance, and deductible payments. Total health costs included both patient out-of-pocket costs and health plan costs (negotiated fees paid to providers for services).
Prescription Drug Utilization and Cost Classification
Prescription drug use was classified as psychotropic or non-psychotropic medication use. Psychotropic medications, identified using the American Hospital Formulary Service Classifications, included lithium, anticonvulsants, antipsychotics, antidepressants, stimulants, anxiolytics/sedatives/hypnotics, and other psychotropic agents (including anti-parkinsonian agents, and two alpha-agonists prescribed for attention deficit hyperactivity disorder - clonidine and guanfacine). All other drugs were categorized as non-psychotropic medications.
Statistical Analysis
The number and proportion of patients who utilized services is presented, both overall and by the type of services used (inpatient, outpatient, pharmacy; for mental health and non-mental health). Mean costs of health services among all children in the cohort (users and non-users) are presented separately by type of service. All costs were inflation adjusted to 2007 dollars using the medical component of the consumer price index.
RESULTS
Sample Characteristics
Characteristics of children included in the sample are provided in Table 1. Among the 4,973 children who met eligibility criteria, approximately 29% were under 13 years of age at their index diagnosis date, and just under half were female. Approximately 34% of patients experienced inpatient mental health visits over the study period. Attention deficit hyperactivity disorder was the most commonly diagnosed condition in the 180 days prior to the patients’ index bipolar diagnosis, occurring in 25% of the children in the sample.
Table 1.
Sample Characteristics (N = 4,973)
| Patient Characteristics a | N | % |
|---|---|---|
| Age – Mean, SD | 13.5 | 3.1 |
| 0 – 6 Years | 193 | 3.9 |
| 7 – 12 Years | 1,248 | 25.1 |
| 13 – 17 Years | 3,532 | 71.0 |
| Sex - Female | 2,393 | 48.1 |
|
| ||
| Bipolar Subtype | N | % |
|
| ||
| Bipolar I | 1,743 | 35.0 |
| Bipolar II | 632 | 12.7 |
| Bipolar NOS | 2,466 | 49.6 |
| Cyclothymia | 132 | 2.6 |
|
| ||
| Disease Severity | N | % |
|
| ||
| Co-morbid Mental Health Conditions – Mean, SD | 1.5 | 1.3 |
| Any Inpatient Mental Health Visits | 1,705 | 34.3 |
|
| ||
| Prior Mental Health Diagnoses | N | % |
|
| ||
| Attention Deficit Hyperactivity Disorder | 1,249 | 25.1 |
| Oppositional Defiant Disorder | 313 | 6.3 |
| Conduct Disorder | 299 | 6.0 |
| Dysthymic Disorder | 248 | 5.0 |
| Anxiety Disorder | 222 | 4.5 |
| Other Mood Disorder | 548 | 11.0 |
| Substance Use (Drug or Alcohol Use) | 113 | 2.3 |
|
| ||
| Received Care from a Psychiatrist | N | % |
|
| ||
| Yes | 2,799 | 56.3 |
| No | 2,174 | 43.7 |
N(%) unless otherwise noted.
Co-morbid mental health conditions, prior mental health diagnoses, and receipt of care for bipolar disorder from a psychiatrist were identified from paid inpatient or outpatient claims from the 6-month pre-index diagnosis period. The occurrence of inpatient mental health visits were measured during the 18 month study period.
Utilization of Health Care
Annual utilization of inpatient, outpatient, emergency and pharmacy services is summarized in Table 2. Overall, 31% of children received inpatient services in the year following their index bipolar diagnosis. Of those receiving inpatient services, 93% (1,455 of 1,564) received services for a mental health related condition, and approximately 11% (174 of 1,564) for non-mental health services.
Table 2.
Inpatient, Outpatient, Emergency and Pharmacy Service Utilization, Overall and by Primary Diagnosis
| Any Visits | Mental Health | Non-Mental Health | ||||
|---|---|---|---|---|---|---|
| Inpatient Services | N | % | N | % | N | % |
|
| ||||||
| Children Receiving Inpatient Services - N (%) | 1,564 | 31.4 | 1,455 | 29.3 | 174 | 3.5 |
| Outpatient Services | N | % | N | % | N | % |
|
| ||||||
| Children Receiving Outpatient Services, N (%) | 4,963 | 99.8 | 4,963 | 100.0 | 4,581 | 92.3 |
| Outpatient Visits per Patient and Type of Service | ||||||
| Mean (SD) | 19.6 | 16.3 | 14.1 | 13.9 | 5.4 | 7.3 |
| Median (IQR) | 15.0 | 18.0 | 10.0 | 16.0 | 3.0 | 6.0 |
|
| ||||||
| Emergency Services | N | % | N | % | N | % |
|
| ||||||
| Children Receiving Emergency Room Services, N (%) | 302 | 6.0 | 283 | 5.7 | 266 | 5.3 |
|
| ||||||
| Pharmacy Services a | N | % | N | % | N | % |
|
| ||||||
| Children Receiving Pharmacy Services, N (%) | 4,631 | 93.1 | 4,342 | 87.3 | 3,690 | 74.2 |
Pharmacy services for mental health include the following psychotropic medications: lithium, anticonvulsants, antipsychotics, antidepressants, stimulants, anxiolytics/sedatives/hypnotics, and other psychotropic agents (including anti-parkinsonian agents, and two alpha-agonists prescribed for attention deficit hyperactivity disorder - clonidine and guanfacine).
Children in the sample averaged 19.6 outpatient visits over the course of one year, with 14.1 mental health-related visits per patient. Approximately 6% of the children in our sample had emergency room visits. The most common reasons for emergency visits were for mental health-related conditions (e.g., depressive psychosis, attention deficit hyperactivity disorder, and other mood disturbances).
Finally, 93% of children received medications, with 87% receiving psychotropic and 74% receiving non-psychotropic medications.
Cost of Health Care
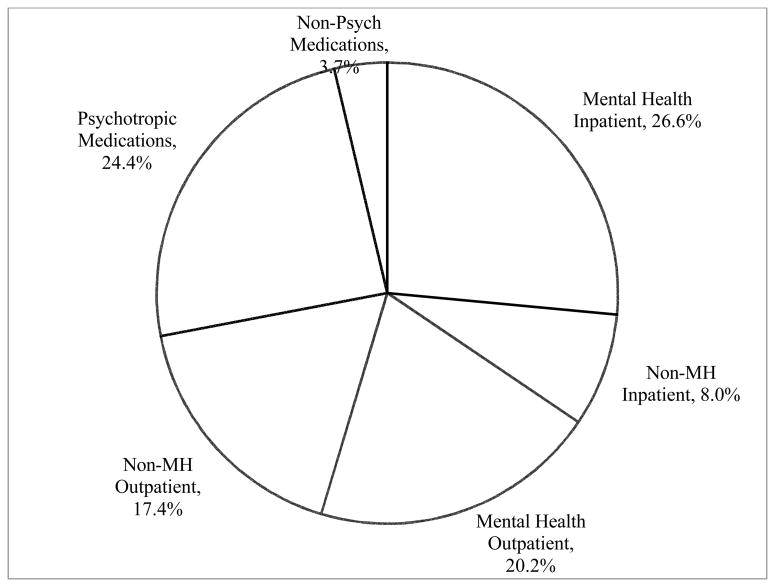
Average annual cost of inpatient, outpatient and pharmacy services is summarized in Table 3. Over the course of one year total health care costs averaged $10,372 and family out-of-pocket costs for all services averaged $1,429. Total costs for all mental health services were $7,356, making up over 71% of all health care spending. The largest portion of health care expenditures were made for inpatient mental health visits (26.6%), outpatient mental health visits (20.2%) and psychotropic medications (24.4%) (Figure 1).
Table 3.
Inpatient and Outpatient Pharmacy Service Cost,a Overall and by Primary Diagnosis
| All Services | Mental Health | Non-Mental Health | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mean | SD | Mean | SD | Mean | SD | |
| Patient Health Costsb | ||||||
| Inpatient Services | $307 | $1,504 | $282 | $1,453 | $25 | $245 |
| Outpatient Services | $664 | $906 | $401 | $697 | $263 | $519 |
| Pharmacy Services | $458 | $504 | $373 | $450 | $85 | $161 |
| Total Health Costsc | ||||||
| Inpatient Services | $3,574 | $16,888 | $2,746 | $8,137 | $828 | $14,548 |
| Outpatient Services | $3,895 | $6,442 | $2,092 | $4,482 | $1,803 | $4,077 |
| Pharmacy Services d | $2,903 | $3,426 | $2,518 | $2,836 | $385 | $1,676 |
All dollars are inflation adjusted to 2007 dollars using the Medical Consumer Price Index.
Patient costs represent the total that the patient paid in copayments, coinsurance, and deductible payments. Patient costs do not include premiums paid for insurance benefits.
Total health costs represent payments made for services after applying pricing guidelines (fee schedules and discounts) but before applying deductibles, copayments, and coinsurance.
Pharmacy services for mental health include the following psychotropic medications: lithium, anticonvulsants, antipsychotics, antidepressants, stimulants, anxiolytics/sedatives/hypnotics, and other psychotropic agents (including anti-parkinsonian agents, and two alpha-agonists prescribed for attention deficit hyperactivity disorder - clonidine and guanfacine).
Figure 1.
Proportion of One Year Total Health Care Costs by Source of Expenditure
The mean total cost for pharmacy services for both psychotropic and non-psychotropic medications was $2,903 per patient, with psychotropic medications accounting for 87% of total prescription drug spending.
DISCUSSION
Although there has been increasing attention paid to pediatric bipolar disorder over the past decade, little is known about treatment utilization patterns and costs in this growing population. In this sample the mean one-year total health costs among children were found to be remarkably similar to published cost estimates for adults with bipolar disorder.(19–25, 33) Outpatient costs made up 38% of total costs, inpatient costs 35%, and medication costs 28%, which are similar to estimates in adults.(20) However, mental health related spending represented 71% of total spending in this sample. This is in contrast to estimates in adult samples (21) that have found spending on mental health to represent only 22% of health care spending.
When considering the differences between adults and children in the proportion spent on mental health care as compared with that spent on total health care, it is important to note that cost estimates also include care for chronic medical conditions, which are more prevalent in adults than in children. As such, a higher concentration of spending on mental health services was anticipated for children as compared with adults. However, lower total costs of care (mental health and non-mental health combined) were also anticipated for children, given the expectation of higher non-mental health spending among adults. Instead, total costs were similar when comparing adult and child estimates because of higher spending on mental health treatment among children. This may be due to difficulties in accurately diagnosing bipolar disorder in children (i.e., diagnostic uncertainty) and the high rates of co-morbid mental health conditions that accompany pediatric bipolar disorder.
Non-mental health outpatient care was among the highest cost categories in the study sample. This was due primarily to high levels of utilization of services, rather than high costs of services in this category. Closer evaluation of the study sample showed that nearly 56% of non-mental health outpatient visits had total costs of less than $100 and nearly 91% had total costs of less than $500. The most common diagnosis coded for non-mental health visits was for routine infant or child health checks. Other common reasons for visits were acute sinusitis, acute pharyngitis, respiratory infections, allergies, asthma, abdominal pain, and fatigue/malaise.
Understanding the financial burden for pediatric bipolar disorder treatment is important as previous studies found that, even among families with private insurance coverage, those with special health care needs (including mental health) have significantly greater financial barriers than families of children without these conditions.(34, 35) Research suggests that as many as 25% of continuously insured families with private health insurance, are underinsured, as defined by the family’s perspective on the reasonableness of out-of-pocket expenses.(26) In the study sample, families paid $1,429 out of pocket per child on average during one year with bipolar disorder. These payments represent the reported patient out-of-pocket expenses (copayments, co-insurance, and deductibles) but do not include information on premiums paid by the patient. Additionally, these estimates do not consider indirect costs, such as lost productivity/absenteeism at work or school, (for family members or the patient), childcare, or other time and services for managing the child’s bipolar disorder. Given the chronic, recurrent nature of bipolar disorder, these costs may be substantial.
Private insurance plans have historically limited mental health service benefits more aggressively than physical health benefits. In this sample there is some evidence of higher patient cost sharing for mental health care than for physical health care. For example, when looking at the total costs of outpatient mental health services, 54% of total costs for outpatient services were mental health related, yet these visits accounted for 60% of patient out-of-pocket costs. Similarly, 77% of inpatient costs were mental health related, but these accounted for 92% of patient out-of-pocket inpatient costs. Not surprisingly, this relationship was not found with psychotropic medication cost sharing as medications are generally managed separately from mental health benefits.
Recently there have been important changes in the legislation surrounding mental health benefits. With the signing of the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity (MHPAE) Act in October of 2008 (P.L. 110–343), and more recently the Patient Protection and Affordable Care Act, employer-sponsored health plans are now required to cover mental health/substance abuse services at the same level as medical/surgical benefits. These policy changes may help to reduce the discrepancies between the mental health and non-mental health cost sharing burden as described above. However, insurers are able to opt-out of offering mental health/substance abuse services, or they may elect to cover only specific disorders.(36) Given the high proportion of spending on mental health services among privately insured children with bipolar disorders, it will be important to monitor health plan coverage for bipolar disorder and the impact of benefit changes on children’s health services utilization.
While no previous studies have estimated total costs of treating bipolar disorder, our inpatient cost and utilization estimates are consistent with a recent study focused on estimating the inpatient burden of pediatric bipolar disorder. In that study, average costs of inpatient treatment were slightly higher but similar to our results, and differences between estimates were likely due to higher costs and longer inpatient stays among youth on Medicaid in the former study.(37)
Data directly comparing healthcare costs for our bipolar sample and similarly aged children, or even subgroups of patients with other chronic conditions, is not readily available. One example of comparison data for a similar population comes from a study of children with diabetes. This study assessed the total average annual costs of diabetes treatment in 2007 using the MarketScan insurance claims data and found that youth with diabetes had $9,061 average annual total expenditures, while youth without diabetes had expenditures of only $1,468.(38) In contrast to these estimates, average annual total costs for youth with bipolar disorder in the present study were $10,372 (in 2007 dollars), with much of this cost attributed to mental health related spending. Costs for non-mental health treatments among children with bipolar disorder in our sample were also higher than costs estimated for children without diabetes. Reasons for this may include more frequent health care utilization or possibly increased physical comorbidities associated with treating bipolar disorders (e.g., metabolic conditions developing subsequent to second-generation antipsychotic use).
There are several important limitations that should be mentioned. First, administrative claims rely on diagnosis codes, rather than structured evaluations, to identify patients with bipolar disorder, which may result in disease misclassification. In an attempt to minimize bias from misclassification, the sample was restricted by including only children with more than one bipolar diagnosis and/or an inpatient stay, which has been shown to increase the specificity of the diagnosis.(39) Related to this, a large proportion of our sample received bipolar disorder not otherwise specified diagnoses (bipolar NOS). This diagnosis may represent diagnostic uncertainty on the part of the clinician. It is unclear whether children with these diagnoses would convert to a bipolar-I or bipolar-II diagnosis, but evidence suggest that conversion from bipolar NOS to a more specific diagnosis occurs frequently among youth.(40) Importantly, inclusion of children with less severe behavioral diagnoses would likely result in conservative estimates of treatment costs and utilization for the sample. Second, it is unclear whether diagnoses made in childhood would persist as the child ages into adulthood, although some suggest that bipolar I and bipolar II may be continuous from childhood to adulthood.(41) These factors may impact the long term costs of treatment, but would not impact the short-term estimates provided in this study. Third, total costs are based on actual payments received by physicians from both the health plan and the patient. These costs are based on negotiated prices between the health plan and the provider and may not be generalizable to publicly insured or to uninsured populations. Finally, cost estimates generated for patient out-of-pocket payments must be interpreted with caution as details on the cost-sharing arrangements between health plans and patients (such as the plan premium) were not available for this analysis.
CONCLUSIONS
The costs of care among privately insured children with bipolar disorder are similar to that of adults. However, spending on children is concentrated on mental health related services. This is important as private insurance plans have historically limited mental health service benefits, which may place a greater burden on families for out of pocket payments. As mental health parity is adopted by private insurers it will be important to monitor the impact on patient utilization and costs of health services, particularly for children with severe mental illness.
Acknowledgments
Funding
Funding for this project was provided by a National Research Service Award grant 5-T-32 HS000032-20 from the Agency for Healthcare Research and Quality (AHRQ). AHRQ played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Dr. Dusetzina is funded by a Ruth L. Kirschstein-National Service Research Award T32MH019733-17 sponsored by the National Institute of Mental Health (NIMH) and Harvard Medical School, Department of Health Care Policy. Dr. Weinberger receives support from a Department of Veterans Affairs Health Services Research and Development Career Scientist Award (RCS91-408). Dr. Gaynes has received support from a grant from the NIMH and AHRQ.
Dr. Farley has received consulting support from Novartis Pharmaceuticals Corp. and Takeda Pharmaceuticals. Dr. Gaynes has received grants and research support from Ovation Pharmaceuticals, Pfizer, Bristol-Myers Squibb, Novartis, and M-3 Corporation and has been on advisory boards of Pfizer, Bristol-Myers Squibb, and Shire Pharmaceuticals. Dr. Sleath is a consultant for Abbott Laboratories on risk communication and a consultant for Alcon Research Ltd. on glaucoma research. Dr. Hansen has received research and consulting support from Takeda, Glaxo-Smith-Kline, and Novartis.
Footnotes
Potential Conflicts of Interest:
Drs. Dusetzina and Weinberger have no competing interests.
References
- 1.WHO. The global burden of disease: 2004 update, Part 3: Disease incidence, prevalence and disability. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 2.WHO. The global burden of disease: 2004 update, Part 4: Burden of disease: DALYs. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 3.Costello EJ, Pine DS, Hammen C, et al. Development and natural history of mood disorders. Biological Psychiatry. 2002;52:529–542. doi: 10.1016/s0006-3223(02)01372-0. [DOI] [PubMed] [Google Scholar]
- 4.Blader JC, Carlson GA. Increased rates of bipolar disorder diagnoses among U.S. child, adolescent, and adult inpatients, 1996–2004. Biological Psychiatry. 2007;62:107–114. doi: 10.1016/j.biopsych.2006.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Archives of General Psychiatry. 2007;64:1032–1039. doi: 10.1001/archpsyc.64.9.1032. [DOI] [PubMed] [Google Scholar]
- 6.Youngstrom E, Youngstrom JK, Starr M. Bipolar diagnoses in community mental health: Achenbach Child Behavior Checklist profiles and patterns of comorbidity. Biological Psychiatry. 2005;58:569–575. doi: 10.1016/j.biopsych.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Case BG, Olfson M, Marcus SC, et al. Trends in the inpatient mental health treatment of children and adolescents in US community hospitals between 1990 and 2000. Archives of General Psychiatry. 2007;64:89–96. doi: 10.1001/archpsyc.64.1.89. [DOI] [PubMed] [Google Scholar]
- 8.Martin A, Leslie D. Psychiatric inpatient, outpatient, and medication utilization and costs among privately insured youths, 1997–2000. American Journal of Psychiatry. 2003;160:757–64. doi: 10.1176/appi.ajp.160.4.757. [DOI] [PubMed] [Google Scholar]
- 9.Geller B, Bolhofner K, Craney JL, et al. Psychosocial functioning in a prepubertal and early adolescent bipolar disorder phenotype. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:1543–1548. doi: 10.1097/00004583-200012000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Goldstein TR, Birmaher B, Axelson D, et al. Psychosocial functioning among bipolar youth. Journal of Affective Disorders. 2009;114:174–183. doi: 10.1016/j.jad.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dickstein DP, Rich BA, Binstock AB, et al. Comorbid anxiety in phenotypes of pediatric bipolar disorder. Journal of Child and Adolescent Psychopharmacology. 2005;15:534–548. doi: 10.1089/cap.2005.15.534. [DOI] [PubMed] [Google Scholar]
- 12.Wilens TE, Biederman J, Forkner P, et al. Patterns of comorbidity and dysfunction in clinically referred preschool and school-age children with bipolar disorder. Journal of Child and Adolescent Psychopharmacology. 2003;13:495–505. doi: 10.1089/104454603322724887. [DOI] [PubMed] [Google Scholar]
- 13.Jolin EM, Weller EB, Weller RA. The public health aspects of bipolar disorder in children and adolescents. Current Psychiatry Reports. 2007;9:106–113. doi: 10.1007/s11920-007-0079-6. [DOI] [PubMed] [Google Scholar]
- 14.Pavuluri MN, Birmaher B, Naylor MW. Pediatric bipolar disorder: a review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:846–871. doi: 10.1097/01.chi.0000170554.23422.c1. [DOI] [PubMed] [Google Scholar]
- 15.McClellan J, Kowatch R, Findling RL. Practice parameter for the assessment and treatment of children and adolescents with bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:107–125. doi: 10.1097/01.chi.0000242240.69678.c4. [DOI] [PubMed] [Google Scholar]
- 16.Feinberg DT. The real cost of pediatric bipolar disorder. Journal of Child and Adolescent Psychopharmacology. 2003;13:431–433. doi: 10.1089/104454603322724797. [DOI] [PubMed] [Google Scholar]
- 17.Peele PB, Xu Y, Kupfer DJ. Insurance expenditures on bipolar disorder: clinical and parity implications. American Journal of Psychiatry. 2003;160:1286–1290. doi: 10.1176/appi.ajp.160.7.1286. [DOI] [PubMed] [Google Scholar]
- 18.Perlis RH, Ostacher MJ, Patel JK, et al. Predictors of recurrence in bipolar disorder: primary outcomes from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD) American Journal of Psychiatry. 2006;163:217–224. doi: 10.1176/appi.ajp.163.2.217. [DOI] [PubMed] [Google Scholar]
- 19.Stensland MD, Jacobson JG, Nyhuis A. Service utilization and associated direct costs for bipolar disorder in 2004: an analysis in managed care. Journal of Affective Disorders. 2007;101:187–193. doi: 10.1016/j.jad.2006.11.019. [DOI] [PubMed] [Google Scholar]
- 20.Guo JJ, Keck PE, Jr, Li H, et al. Treatment costs and health care utilization for patients with bipolar disorder in a large managed care population. Value in Health. 2008;11:416–423. doi: 10.1111/j.1524-4733.2007.00287.x. [DOI] [PubMed] [Google Scholar]
- 21.Bryant-Comstock L, Stender M, Devercelli G. Health care utilization and costs among privately insured patients with bipolar I disorder. Bipolar Disorders. 2002;4:398–405. doi: 10.1034/j.1399-5618.2002.01148.x. [DOI] [PubMed] [Google Scholar]
- 22.Simon GE, Unutzer J. Health care utilization and costs among patients treated for bipolar disorder in an insured population. Psychiatric Services. 1999;50:1303–1308. doi: 10.1176/ps.50.10.1303. [DOI] [PubMed] [Google Scholar]
- 23.Begley CE, Annegers JF, Swann AC, et al. The lifetime cost of bipolar disorder in the US: an estimate for new cases in 1998. Pharmacoeconomics. 2001;19:483–495. doi: 10.2165/00019053-200119050-00004. [DOI] [PubMed] [Google Scholar]
- 24.Wyatt RJ, Henter I. An economic evaluation of manic-depressive illness--1991. Social Psychiatry and Psychiatric Epidemiology. 1995;30:213–219. doi: 10.1007/BF00789056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centorrino F, Mark TL, Talamo A, et al. Health and economic burden of metabolic comorbidity among individuals with bipolar disorder. Journal of Clinical Psychopharmacology. 2009;29:595–600. doi: 10.1097/JCP.0b013e3181bef8a6. [DOI] [PubMed] [Google Scholar]
- 26.Kogan MD, Newacheck PW, Blumberg SJ, et al. Underinsurance among children in the United States. New England Journal of Medicine. 2010;363:841–851. doi: 10.1056/NEJMsa0909994. [DOI] [PubMed] [Google Scholar]
- 27.Glied SA, Frank RG. Better but not best: recent trends in the well-being of the mentally ill. Health Affairs. 2009;28:637–648. doi: 10.1377/hlthaff.28.3.637. [DOI] [PubMed] [Google Scholar]
- 28.Busch AB, Huskamp HA, Landrum MB. Quality of care in a Medicaid population with bipolar I disorder. Psychiatric Services. 2007;58:848–854. doi: 10.1176/ps.2007.58.6.848. [DOI] [PubMed] [Google Scholar]
- 29.Baldessarini RJ, Leahy L, Arcona S, et al. Patterns of psychotropic drug prescription for U.S. patients with diagnoses of bipolar disorders. Psychiatric Services. 2007;58:85–91. doi: 10.1176/ps.2007.58.1.85. [DOI] [PubMed] [Google Scholar]
- 30.Baldessarini R, Henk H, Sklar A, et al. Psychotropic medications for patients with bipolar disorder in the United States: polytherapy and adherence. Psychiatric Services. 2008;59:1175–1183. doi: 10.1176/ps.2008.59.10.1175. [DOI] [PubMed] [Google Scholar]
- 31.Maniscalco ER, Hamrin V. Assessment and diagnostic issues in pediatric bipolar disorder. Archives of Psychiatric Nursing. 2008;22:344–355. doi: 10.1016/j.apnu.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 32.Carlson GA, Jensen PS, Findling RL, et al. Methodological issues and controversies in clinical trials with child and adolescent patients with bipolar disorder: report of a consensus conference. Journal of Child and Adolescent Psychopharmacology. 2003;13:13–27. doi: 10.1089/104454603321666162. [DOI] [PubMed] [Google Scholar]
- 33.Harley C, Li H, Corey-Lisle P, et al. Influence of medication choice and comorbid diabetes: the cost of bipolar disorder in a privately insured US population. Social Psychiatry and Psychiatric Epidemiology. 2007;42:690–697. doi: 10.1007/s00127-007-0222-z. [DOI] [PubMed] [Google Scholar]
- 34.Busch SH, Barry CL. Mental health disorders in childhood: assessing the burden on families. Health Affairs. 2007;26:1088–1095. doi: 10.1377/hlthaff.26.4.1088. [DOI] [PubMed] [Google Scholar]
- 35.Busch SH, Barry CL. Does private insurance adequately protect families of children with mental health disorders? Pediatrics. 2009;124:S399–S406. doi: 10.1542/peds.2009-1255K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barry CL, Huskamp HA, Goldman HH. A political history of federal mental health and addiction insurance parity. Milbank Quarterly. 2010;88:404–433. doi: 10.1111/j.1468-0009.2010.00605.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berry EA, Heaton PT, et al. National estimates of the inpatient burden of pediatric bipolar disorder in the United States. The Journal of Mental Health Policy and Economics. 2011;14:115–123. [PubMed] [Google Scholar]
- 38.Shrestha SS, Zhang P, Albright A, et al. Medical expenditures associated with diabetes among privately insured U.S. youth in 2007. Diabetes Care. 2007;34:1097–1101. doi: 10.2337/dc10-2177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schneeweiss S, Avorn J. A review of uses of health care utilization databases for epidemiologic research on therapeutics. Journal of Clinical Epidemiology. 2005;58:323–337. doi: 10.1016/j.jclinepi.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 40.Birmaher B, Axelson D, Goldstein B, et al. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: the Course and Outcome of Bipolar Youth (COBY) study. American Journal of Psychiatry. 2009;166:795–804. doi: 10.1176/appi.ajp.2009.08101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chang K. Adult bipolar disorder is continuous with pediatric bipolar disorder. Canadian Journal of Psychiatry. 2007;52:418–425. doi: 10.1177/070674370705200703. [DOI] [PubMed] [Google Scholar]