Abstract
Health-care-associated infections (HAIs) remain a major patient safety problem even as policy and programmatic efforts designed to reduce HAIs have increased. Although information on implementing effective infection control (IC) efforts has steadily grown, knowledge gaps remain regarding the organizational elements that improve bedside practice and accommodate variations in clinical care settings. We conducted in-depth, semistructured interviews in 11 hospitals across the United States with a range of hospital personnel involved in IC (n = 116). We examined the collective nature of IC and the organizational elements that can enable disparate groups to work together to prevent HAIs. Our content analysis of participants’ narratives yielded a rich description of the organizational process of implementing adherence to IC. Findings document the dynamic, fluid, interactional, and reactive nature of this process. Three themes emerged: implementing adherence efforts institution-wide, promoting an institutional culture to sustain adherence, and contending with opposition to the IC mandate.
Keywords: content analysis, health care, culture of, illness and disease, infectious, quality improvement, safety, patient
Health-care-associated infections (HAIs), acquired through receipt of medical or surgical treatment, are a major patient safety issue. The Centers for Disease Control and Prevention (CDC) estimates that 1 in 20 hospitalized patients will acquire an HAI (CDC, 2010); of these, a significant number will die. In 2002, approximately 1.7 million patients in hospitals in the United States acquired an HAI (Klevens et al., 2007). Nearly 1 million hospital deaths in the United States in 2002 were associated with an HAI (Klevens et al.). In the past 20 years, the overall incidence of HAIs has increased by 36% (Kohn, Corrigan, & Donaldson, 2000). This increase is partly because of the emergence of multidrug-resistant organisms (MDROs).
More than 70% of the bacteria that cause HAIs are resistant to at least one of the drugs most commonly used to treat them (Marschall, Agniel, Fraser, Doherty, & Warren, 2008; National Nosocomial Infections Surveillance System, 2004). Methicillin-resistant Staphylococcus aureus (MRSA) is an MDRO that has been at the center of attention. The number of MRSA infections in hospitals in the United States tripled between 2000 and 2005 (Elixhauser & Steiner, 2007). The significant public health burden represented by these rising infection rates has prompted the U.S. Department of Health and Human Services (HHS) to implement Roadmap to Elimination, their national action plan to prevent HAIs (HHS, 2009, 2012). A majority of states have enacted laws mandating that health care facilities collect and publicly report facility-specific HAI data (Reagan & Hacker, 2012).
Although policy and programmatic efforts designed to decrease preventable HAIs have increased, interest in how to implement effective infection control (IC) efforts has steadily grown (Uchida et al., 2011). A developing body of evidence supports the importance of organizational context and culture in the implementation of IC programs (Charles, McKee, & McCann, 2011; Scott, Mannion, Davies, & Marshall, 2003; Sinkowitz-Cochran et al., 2012; Welsh et al., 2012). Investigations have also been identifying common interpersonal practices in the health care setting that can facilitate or hinder the success of IC programs (Damschroder, Aron, et al., 2009; Sinkowitz-Cochran et al.). Building on the concept of the Institute for Healthcare Improvement’s evidence-based IC bundle (Resar, Griffin, Haraden, & Nolan, 2012), Welsh and colleagues (2012) have proposed a behavioral change bundle model of interrelated components that they have posited collectively addresses challenges and promotes success in HAI-reduction projects.
Although the evidence base on IC efforts is steadily increasing, gaps in knowledge remain. More information is needed about the organizational processes that will improve behavior at the bedside across variations in clinical care settings. One consequence of the paradigm shift in IC practices is that increasingly more processes are being initiated by the clinical unit, not the IC department. We conducted an investigation to advance understanding of how variations in the organization and structures of care relate to processes of infection prevention and control at the bedside. We drew a purposive sample of hospitals with known variation in both HAI rates and intensity of processes implemented. We conducted in-depth interviews at each site with a range of hospital personnel involved in infection prevention and control. In this article, we report on the collective nature of IC efforts and discuss the organizational elements that enable disparate groups to work together to implement compliance with IC guidelines.
Method
From October 2010 through February 2011, we conducted in-depth, semistructured interviews with hospital personnel at 11 nonspecialty, acute care hospitals across the nation as part of an ongoing mixed-methods investigation of HAIs. The hospitals in the sample were drawn from a sample of 250 hospitals in the National Healthcare Safety Network that participated in an earlier survey we had conducted on HAIs (Furuya et al., 2011; Pogorzelska et al., 2011; Stone et al., 2009). We purposively selected the hospitals for this qualitative study for maximum variation in size, geographic region, as well as HAI rates, and degree of implementation of HAI prevention strategies, based on the hospitals’ previous survey responses. At each participating hospital, we identified a site coordinator from the IC department who assisted with the identification and recruitment of personnel knowledgeable about IC in that setting.
To further our understanding of how variations in structures of care and responsibility related to the process of implementing infection prevention at the bedside, we purposively recruited employees with a range of areas of expertise and work experience. This recruitment strategy enabled us to obtain an array of perspectives and experiences regarding IC at that hospital site. We conducted, on average, 10 in-depth interviews at each hospital site. We provided each hospital with $1,000 in recognition of their participation. We stopped data collection when saturation was reached; we determined this had occurred when the round of interviews conducted at two hospital sites yielded only repetitive and confirmatory information.
The interviews were audiotaped and typically ranged from 30 to 60 minutes in length. We developed a semistructured interview guide tailored for each personnel type. The guide focused on (a) organization and structures of the IC program; (b) institutional IC priorities; (c) the participant’s role in IC; (d) processes/implementation of IC at the point of care (i.e., educational processes, implementing changes in policy, compliance, facilitators/barriers, challenges, and specific policies); and (e) specific scenarios where IC broke down. Both senior and junior investigators conducted the interviews. The senior investigators interviewed more senior informants, such as hospital administrators, and the junior investigators conducted interviews with more junior informants, such as staff nurses.
Prior to conducting the interviews, we trained all the interviewers as a group to facilitate a shared understanding of the nature and quality of the interview data sought and the techniques to be used to obtain them. To maintain rigor in data collection, we held debriefings with the entire study team after the round of interviews at each hospital was completed. We obtained approval for the study from the Institutional Review Boards of Columbia University Medical Center, New York University Medical Center, and the RAND Corporation.
Data Analysis
We transcribed the audiotaped interviews verbatim. We removed all personal identifiers from the transcripts and assigned each transcript a heading (personnel role title) and number (hospital code). We entered the transcripts into NVivo software (QSR International, 2010) to facilitate the content analysis. Three members of the research team coded the transcripts. Prior to beginning the actual coding process, the coders independently reviewed the transcripts to establish a general tone. They then compiled a comprehensive list of topics present in the transcripts to ensure the creation of an inclusive set of codes.
We began the coding analysis by identifying segments of text that related to a unique core code that represented a phenomenon of central interest. For each core code, we developed secondary codes that represented either more specific or restricted aspects of the phenomena. The list of codes was reviewed by all the investigators. In all, 9 core codes and 52 secondary codes were established. The coders collaboratively drafted definitions for each core and secondary code, and these definitions were then reviewed by all investigators. We also developed an audit trail. To maintain consistency throughout the coding process, we double-coded 11% of the transcripts and held weekly coding debriefing meetings. We resolved isolated coding discrepancies at these weekly meetings. The inter-rater agreement was excellent (exceeding 90%).
Results
We conducted in-depth, semistructured interviews with 116 hospital employees at 11 nonspecialty acute care hospitals across the nation. Three hospitals were located in the northeast, three in the south, three in the midwest, and two in the west. The number of hospital beds ranged from 160 to 1,300. A variety of personnel were interviewed at each hospital. The sample included 23 top administrators (i.e., chief executive officer, chief nursing officer), 7 hospital epidemiologists, 19 IC staff, 16 senior clinicians (i.e., intensivists, hospitalists, intensive care unit medical directors), 25 nurses, and 26 other personnel (i.e., 12 environmental services personnel, 9 respiratory therapists, 1 transport supervisor, 1 pharmacist, 2 nurse’s aides, and 1 physical therapist) identified by the hospital site coordinator as knowledgeable about the hospital’s IC policies and procedures (see Table 1 for a personnel breakdown by hospital). All participants spoke English and were employed at the hospital for at least 1 year prior to the interview.
Table 1.
Characteristics of Hospital Sites (n = 11) and Hospital Staff Participants (n = 116).
| Region | Northeast (n = 3) | South (n = 3) | Midwest (n = 3) | West (n = 2) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Beds (count rounded) | 1,300 | 860 | 430 | 470 | 420 | 350 | 510 | 250 | 160 | 510 | 410 |
| Staff participants | |||||||||||
| Administratora | 3 | 1 | 3 | 2 | 3 | 3 | 1 | 2 | 2 | 2 | 1 |
| Hospital epidemiologist | 1 | 1 | 1 | — | 1 | — | 1 | 1 | — | 1 | — |
| Infection control staff | 2 | 2 | 1 | 1 | 2 | 2 | 1 | 2 | 2 | 2 | 2 |
| Senior clinicianb | 2 | 1 | 3 | 2 | 1 | 2 | — | 1 | 1 | 1 | 2 |
| Staff nursec | — | 3 | 1 | 3 | 1 | 2 | 3 | 3 | 4 | 2 | 3 |
| Otherd | 2 | 3 | 1 | 2 | 3 | 2 | 4 | 2 | 2 | 3 | 2 |
| Total participants | 10 | 11 | 10 | 10 | 11 | 11 | 10 | 11 | 11 | 11 | 10 |
Chief nursing officers, directors, vice presidents
Medical doctors, intensive care unit directors, hospitalists
Nurse managers, nurse practitioners, patient care supervisors
Transport supervisors, pharmacists, nurse’s aides, physical therapists
Our content analysis of the participants’ narratives yielded a rich description of the organizational process of initiating compliance with IC. Three major themes emerged from this analysis: (a) implementing adherence efforts institution-wide, (b) promoting an institutional culture to sustain adherence, and (c) contending with opposition to the IC mandate. Each of these themes encompassed several subthemes (see Figure 1). They are discussed in greater detail below, with illustrative quotations drawn from the participants’ accounts.
Figure 1.
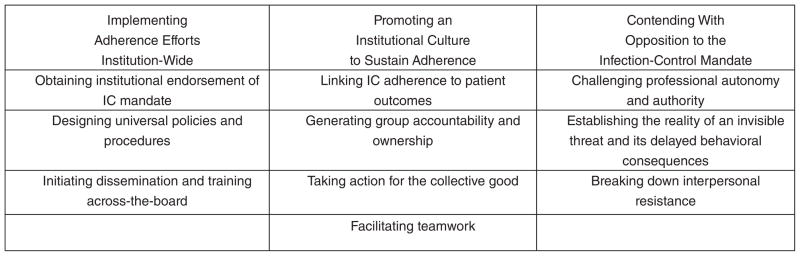
Emergent themes and subthemes describing the process of initiating adherence to infection control (IC).
Implementing Adherence Efforts Institution-Wide
Participants discussed the importance of implementing a system-wide effort involving the entire health care institution to foster compliance with IC policies and procedures. As summed up by one hospital administrator, “Infection control is not just one individual; it’s a hospital-wide initiative, a concern, whatever. And so I think everyone participates.” Numerous comments indicated that the process of implementing an institutional mandate on IC precipitates changes that ultimately affect the organizational environment. As one hospital epidemiologist succinctly stated, “To have success, you have to change the culture.” Participants’ observations identified several elements that could form the foundation to foster efforts that would facilitate compliance with IC: (a) obtaining institutional endorsement of the IC mandate, (b) designing appropriate policies and procedures, and (c) initiating dissemination and training across the board.
Obtaining institutional endorsement of the IC mandate
For a comprehensive policy on IC to be recognized as an institutional mandate, participants noted that the support and endorsement of hospital administration was required. As one hospital epidemiologist stated, what was needed was “buy-in from the senior management team and the Board.” It also needed to garner hospital-wide commitment, as elaborated by another hospital administrator: “It has to come from the top, and it has to be honored all the way to the bottom, and to the patients, and to the community. It’s a team effort.”
Participants’ observations indicated that for a comprehensive health initiative to be effective, policies and procedures should be implemented on a widespread basis and with consistency across the institution. The following description offered by a staff nurse encapsulates this type of approach: “They’re universal for our hospital. So just because you’re on one floor, you’re not going to follow different rules.” Similarly, a hospital administrator explained, “If we’re looking at one group of employees to be in compliance, then all groups of employees need to be in compliance … because it’s the best way for our community.” Indeed, it was commonly observed that universal compliance necessitated that no professional group would be exempt. Another hospital administrator noted, “We’re sharing this with doctors, too, saying, you know, when a nurse comes up to you and says, ‘Hey, Doc, I didn’t see you wash your hands,’ don’t run the mouth. Just go in there and wash your hands.”
Designing appropriate policies and procedures
The accounts also contained observations about the scope of effort involved in developing IC policies and procedures for universal implementation. Participants acknowledged the need to understand and accommodate the pertinent activities, facilities, and personnel issues and conditions that might vary across the institution. The following comments by an infection preventionist illustrate the type of activities required to ensure that service-relevant issues are taken into consideration: “If we don’t go to leadership meetings, we aren’t on patient care managers, we don’t go to supervision of care, how do we know what they need? We kind of live in our own little silo.”
A strong emphasis in the interviews was also placed on the value of outreach and engagement with different stakeholders’ groups in the organization to elicit their point of view during the planning and initial implementation periods. Participants’ comments indicated that such efforts were considered integral when designing IC protocols that would be effective and engender widespread compliance. One administrator explained:
It wouldn’t be beneficial for me to put something in place that really was not how it’s really practiced on the unit, per se. I would really definitely need their feedback to say, “This is what we have to accomplish. How can we do this?”
The necessity of applying a broad perspective when considering other factors that could impede widespread adherence to IC policy and protocols was also present in the narratives. For example, one physician pointed out that both practicality and relevance need to be considered when developing IC efforts:
This [IC] is a little slice of what all of our clinical people are doing. We have to make it a really important slice for them, but we have to make it easy for them to do the correct thing.
Initiating dissemination and training across the board
Launching widespread dissemination and training on the IC policies and procedures was another central implementation activity. Participants recounted that this was done to foster an environment that supports adherence to IC. One physician observed, “It’s an effective policy when everybody’s aware of it.” He noted further, “Collective effort means that: educating everybody.”
Ensuring that all personnel hospital-wide have a shared understanding and appreciation of institutional IC policies and procedures is a complex, multilayered task. The scope of such an effort is evident in a hospital administrator’s description of the planned IC education program:
Error-prevention techniques that we are going to be teaching … first to our Board, our physician leaders, our nurse leaders, and then we’re going out to clinical, nonclinical associates so that everybody understands that the goal is to try to provide safe care, prevent errors, prevent harm to patients, and that every single person that works in this organization has some little part in doing that.
Promoting an Institutional Culture to Sustain Adherence
In the patient safety literature, the notion of organizational or institutional culture has been defined as the accumulation of invisible, often unspoken ideas, values, and approaches that permeate organizational life. Culture is typically discussed in terms of a deeply ingrained set of ideas and experiences that serve as a frame for actions and experiences in workplaces. It is possible to view culture as at least partially reflecting leadership decisions in organizations that over time result in the norms of the setting (Clarke, 2006). This notion of culture was another major theme in the participants’ accounts. It reflected their awareness that promoting adherence to IC policies and practices necessitates an institutional culture in which IC is viewed as central to outcomes that are viewed as meaningful by all personnel groups. Their accounts revealed that establishing this type of institutional culture can involve (a) linking IC adherence to patient outcomes, (b) generating group accountability and ownership, (c) taking action for the collective good, and (d) facilitating teamwork.
Linking IC adherence to patient outcomes
The participants’ statements emphasized that explicitly linking IC compliance to patient outcomes featured prominently in efforts promoting adherence to IC. They recounted that this connection was pointed out when IC was discussed at employee training sessions, inservice conferences, and employee orientation. One hospital epidemiologist related how she routinely told hospital staff, “If you don’t wash your hands, your patient is going to get sick. If you don’t do these things in this bundle, that patient is going to get sick. And it is your responsibility for this.” Another hospital epidemiologist reported delivering the same message content embedded in the context of other patient safety behaviors:
[You] wouldn’t willingly give the patient the wrong medication. You wouldn’t willingly leave the bedrail down with somebody who could fall out of bed. But you willingly do not wash your hands or wear personal protective equipment, and you can transmit disease to another patient.
Although the narratives indicated that this type of communication was tailored to be relevant to the audience and appropriate for the venue, the IC message conveyed to all employee groups was consistent: “You are doing harm to your patient by not complying.”
Generating group accountability and ownership
The participants commented that cultivating a sense of ownership and pride in ensuring patient safety through their personal actions will engender compliance with IC policies. As one hospital epidemiologist explained,
What I want to convey, “Not on my watch—when I come into work in the morning, when I leave at night, no one will have gotten an infection on my watch.” And when people buy into that and believe it, it will work.
An administrator expressed a similar belief in the value of instilling responsibility and ownership:
As we teach everybody and empower everybody to do these error prevention things, [we expect] that the culture will shift so that everybody is feeling like, “I have this sense of pride that I am doing everything that I can do today to try to prevent my patients from being harmed in this organization.”
Consistent with a system-wide mandate of compliance with IC, the narratives also contained examples of message content framed to motivate IC compliance in different groups of employees. The following statement by a director of environmental services provides an example of how this message of group accountability and ownership was communicated to the housekeeping staff:
I’ve tried in our monthly meetings with our employees [to] give them pride in their work…. I say our job is just as important as the doctors or nurses. People’s lives do depend on how well we clean these rooms … so when they go in there they feel they’ve got an important job here at the hospital, so that they take that extra effort.
It was also evident throughout the accounts that similar efforts were being made to instill a sense of personal accountability and ownership on a unit or service level. As one hospital epidemiologist explained,
Every department needs to be part of infection control and own it. Own their piece. It’s not infection control putting something on somebody else…. Each department needs to realize that infection control is their job, their job, and they need to come up with ways in their department … what could be done better.
Taking action for the collective good
Although an emphasis on personal accountability was evident in the narratives, participants’ accounts also documented that collective responsibility was perceived as an integral component of the institutional culture that supported adherence to IC. Specifically, the participants’ statements delineated how acting on the broad mandate of collective responsibility for IC compliance goes beyond personal adherence to IC protocols. One physician concisely stated this behavioral precept as, “You’re the patient’s advocate when you see something not being done right.” IC adherence confers responsibility on every hospital employee to intervene and stop an activity when noncompliance is observed, as comments of one hospital administrator illustrated: “It’s everyone’s job to stop the line [central venous catheter insertion] if something’s not occurring that should be occurring.” Participants also conveyed that inaction is not acceptable. As another physician explained, “If you don’t say something to someone who has not washed their hands, then you haven’t washed your hands. It’s just as good. You haven’t done it, but now you’re responsible because you’re seeing that happening.”
The narratives indicated that although there is a behavioral expectation to take action, it presents a difficult challenge. They indicated that hospital culture would need to change for this to be broadly acted on. This awareness is reflected in the following comment offered by an administrator:
We don’t have a culture here where people always are willing to say, “Oh, by the way, would you mind dressing appropriately before entering that room?” That’s not our culture. It needs to become our culture…. There’s still a hesitation or fear for people sometimes to say the right thing.
Similarly, a respiratory therapist’s words reinforce the difficulty of engendering this type of behavior in health care workers: “The inability to speak up, tell people; you know, enforce the rules. A lot of people just see it and say, ‘Okay, next time I’ll say something.’” Power differentials can also impede staff taking action to ensure that others follow appropriate IC behavior. As one nurse acknowledged, “Part of it is probably still some intimidation, because it’s like, ‘I’m not going to tell Dr. A to wash his hands or to put on gloves.’”
Recognition that this situation would need to be addressed was reflected in a statement made by a hospital administrator: “We have to empower the clerk to say to the doctor: ‘Doc, you just left that room and didn’t use the hand gel.’” Empowerment was often mentioned in the accounts as a strategy that was being used to enable personnel to act for the collective good in situations where power differentials might hamper their behavior. A hospital administrator explained,
We have the nurse in the units know that the doctors have been told. We’ve told them through letters, we’ve told them through Dr. X, we’ve told them through different committees where we present data. And then we have to say, “Okay, nurses, you are empowered one on one. If your doctor comes in there and you’re going to have to put in a central line, you are empowered to stop him when he is doing something that is incorrect. Point it out to him.”
Facilitating teamwork
The collective nature of health care extends to efforts to promote adherence to IC. The importance of addressing compliance with IC from a team perspective was noted throughout the narratives. It was explicitly acknowledged that adherence requires more than just attending to the individual level. As one nurse stated, “I’m doing a good job, but just one person doing a good job for a patient does not prevent anything. It is teamwork. It needs to be twenty-four/seven. Those central lines need to be protected twenty-four/seven.”
Indeed, implementing compliance with IC involves, as one hospital epidemiologist commented, “Making everybody aware that it’s a team effort. It’s not a one-person show.” Similar sentiments were expressed by a physician:
They’ve got to buy into the system, to understand and buy in…. It’s part of believing and understanding the process: “Okay, so I didn’t scrub so hard on this wall. Big deal.” What’s the big deal? … This is an area that requires multiple pieces from a lot of people. And if one of the pieces breaks down, then the whole system breaks down.
Recognition that this was an important objective to reach in moving toward a culture that supports IC compliance was evident throughout the interview accounts. As a director of environmental services explained, “If everybody would see that we’re all here for one common goal, one common purpose—the patient, you know—that would be great. Not everybody does, but, you know, it helps when we do have that understanding among everyone.”
Facilitating adherence to IC on a collective level can often involve crossing disciplinary lines, job titles, and services. Silos are broken down as individuals work together in unison to achieve the shared goal of “do no harm.” A physician described this aspect of teamwork:
The disease process doesn’t obey barriers. It’s everywhere. So if you don’t attack it with a team approach, multidisciplinary approach, you’re not going to be able to attack it. So you need to have less about my territory and your territory, and more about, “All right, let’s just get down to the nuts and bolts.”
Contending With Opposition to the Infection Control Mandate
Contained in the participants’ narratives were descriptions of the opposition that was encountered when efforts were implemented to move toward universal compliance of the IC protocols. This final theme reflected the following accounts: (a) challenging professional autonomy and authority, (b) establishing the reality of an invisible threat and its delayed behavioral consequences, and (c) breaking down interpersonal resistance.
Challenging professional autonomy and authority
Resistance to an institution’s IC mandate was reported for groups of professionals trained to act autonomously. As one hospital epidemiologist noted, “The private physician, I think, is the hardest nut to crack, because they’re their own boss.” Professional expertise confers autonomy in behavior (i.e., professional privilege) that can impede compliance with institutional mandates.
Consequently, mandated practice change, even when necessitated by new evidence, can be perceived as a threat to professional identity, negating prior training and expertise and generating a loss of professional authority. As one administrator explained, “There is a fear that you’re starting to take away some of the autonomy of physicians and nurses. You’re almost negating their training by telling them this, being so prescriptive.” This situation is compounded when someone has been practicing in the field for a lengthy period of time, as illustrated by a comment from a hospital epidemiologist, recalling presenting the changes in IC protocols to the hospital staff: “We have some older physicians, particularly surgeons, who are like, ‘I’ve been doing it this way for thirty years. No one is going to tell me that I’m going to change now.’”
Establishing the reality of an invisible threat and its delayed behavioral consequences
IC is addressing an invisible danger. The accounts document that this lack of a visual indication of a threat presents a difficult challenge in conveying that, even when there are no recognizable signs that a safety issue exists, compliance with IC needs to be maintained. As one infection preventionist explained, “You know, the concept of infection prevention, it’s that you can’t see it. And so you really have to build faith in people that what you do, what you can’t see really can cause a serious outcome.” Similarly, a hospital epidemiologist commented,
You’re dealing with something you can’t see. People go in there and say, “I don’t see the MRSA. I don’t see the C. diff [Clostridium difficile]. I don’t see the gram negatives. So what’s the big deal?” And that’s the issue. It’s not like it is some big obvious black plague that you’re seeing. It’s often not so obvious.
Indeed, it can be valuable to see a visual reminder of the potential harm that failing to instill adherence to safety precautions can engender. This is vividly apparent in the following description, offered by a nurse speaking about when staff members were confronted with a lice and scabies outbreak:
Both [patients] had lice and scabies, and so it was very interesting the amount of panic in the unit. Any time somebody had to go into the room, I mean the booties were on. They were calling the OR [operating room]. They wanted bonnets. If they had to transport the patient, the transporters were freaked out…. It’s something about the bug you can see versus the bug you can’t.
Compounding the difficulty in instilling behavior to deal with a threat that one cannot see is having to establish a link between specific behavior, however minor, and a delayed outcome, sometimes days past the event. This challenge to promoting compliance was succinctly described by an infection preventionist:
Difficult to tie the outcome to specific actions or lack of actions…. If you don’t wash your hands, or handle the line poorly, and three days or later that person has a bloodstream infection, they don’t make the connection between what they did and that patient’s outcome.
Breaking down interpersonal resistance
The accounts also contained discussion of interpersonal strategies that were evoked to resolve opposition to IC compliance. One approach involves evoking the assistance or buy-in of a respected or experienced health professional who can function as an advocate or champion, helping promote widespread adoption and acceptance of new practices and policies. As one administrator commented,
I think it’s if the boss, or the chiefs, or the attending physicians are into it…. It’s like a role model. If your boss is not into it, then, “I will not be either.” So I think good role models, a good buy-in from the hospital administrators, directors, people you look up to, or people who are supposed to be good role models, set an example.
Peers are also a powerful influence. The accounts contain reports of the value of peers in reinforcing and sustaining behavior. One nurse explained, “You can learn something in class, but if your coworkers and role models around you aren’t practicing it, you pick up their bad habits also.”
In instances when opposition is strong, adherence might be accomplished only by direct intervention of someone in authority. As one infection preventionist explained,
Our medical executive, Dr. Z, will address that with the physicians. That’s his job, takes us out of the bad guy…. They don’t always like it, but they have changed behavior…. So I think that that feedback and having a mechanism where someone that can talk to the physician can talk to them, that works.
Discussion
Using a qualitative approach that elicited the perspectives of multiple types of personnel involved in health care, we obtained a comprehensive and broad understanding of the complex, multifactorial, and interdisciplinary issues involved in implementing a change in IC policies and procedures. The participants’ narratives offered a rich description of the elements of this process, underscoring that engendering compliance is dynamic, fluid, interactive, and reactive.
As Weiner, Belden, Bergmire, and Johnston (2011) observed, research in implementation science has made evident that there are often multiple ways to achieve the same outcomes. The accounts offered by participants revealed that a range of strategies and organizational components were being drawn on to enable disparate groups of individuals to achieve the common goal of reducing HAIs. Participants’ statements elucidated the strategic application of business and marketing concepts, as well as the employment of behavioral science principles, to promote individual- and system-level change. Such techniques are consistent with the IC behavioral change bundle model that Welsh and colleagues (2012) proposed.
Incidents participants disclosed made clear that when evidence-based changes in IC policies and procedures were implemented that conflicted with the health care providers’ widely held beliefs and practices, prior training, or practice expertise, the providers’ professional autonomy and authority were threatened. The participants’ reports substantiated that supportive leadership and the pivotal contribution of a trusted champion were strategies used to foster engagement, break down disciplinary silos, and promote adherence to IC practices. Indeed, Damschroder, Banaszak-Holl, and colleagues (2009) noted that coalitions of champions are required when infection prevention crosses professional and organizational boundaries.
The narrative reports detailed the initiation of various efforts to expand responsibility for infection prevention and control in health care settings. There is a large and long history of overall low compliance with hand hygiene, and physicians are consistently rated the worst in performing hand hygiene appropriately (Garcia-Williams, Brinsley-Rainisch, Schillie, & Sinkowitz-Cochran, 2010; Lipsett & Swoboda, 2001). Consequently, many initiatives in hospitals have been implemented to break this cycle. The participants’ reports of these efforts provided multiple stakeholder insights into the challenges and changes necessary for positive outcomes.
The realization that shared ownership of this responsibility by all levels of health care personnel would require broad, systemic changes was evident in the participants’ statements. Although there was acknowledgment that IC personnel would continue to remain central, participants perceived that enabling staff to intervene to ensure adherence to IC guidelines would require an organizational culture change. Hawe, Shiell, and Riley (2009) posited that interventions impact person–time–place interactions and are best viewed as system-level events that change the future trajectory of the system dynamics.
Indeed, consistent with Scott and colleagues’ (2003) report on implementing culture change within the United Kingdom National Health Service, our examination of the participants’ accounts substantiated that this type of change does not occur spontaneously or rapidly. As detailed in their narratives, a conscious effort toward organizational, multilevel strategic planning and supportive tactics were required to support the authority of any health care worker to act when IC guidance was not being followed and to address the interactional impediments that arose.
The emergent themes and subthemes describing the process of initiating adherence to IC inform a number of domains that Damschroder, Aron, and colleagues (2009) proposed in their consolidated framework for implementation research (CFIR). CFIR is an overarching typology developed to foster theory development and implementation of health services findings into practice. The participants’ narratives provide relevant insights on a number of CFIR domains. Specifically, our findings provide insights relevant to the following constructs in the “intervention characteristics” domain: intervention sources, evidence strength and quality, adaptability, and complexity. In the “inner setting” domain, the participants’ accounts address the constructs of networks and communications, culture, and implementation climate. For the “characteristics of individuals” domain, participants’ narratives inform the construct’s knowledge and beliefs about the intervention and self-efficacy. The participants’ reports also provide information for the following constructs in the “process” domain: planning and engaging.
In this study, we focused on those who were knowledgeable about IC in the setting in which they worked. These included individuals in leadership positions, such as hospital administrators and senior clinicians, as well as those responsible for maintaining IC protocols at the bedside, such as staff nurses, nurse’s aides, and housekeeping personnel. Although the participants reflected a range of areas of expertise and work experience, we did not interview new hires or residents, which might be a limitation. These types of people might have brought different perceptions about how they learn about IC policies. Future researchers might want to address this gap.
We purposively selected hospital sites so that variation in size, geographic locale, HAI rates, and degrees of implementation of IC were represented. The narrative accounts of the varied personnel interviewed at these hospitals necessarily reflected experiences in the context of their hospital environment; however, the findings do not specifically address the contextual characteristics of the different kinds of hospitals.
Participants’ descriptions of events reflected their perceptions and assessment of circumstances. By including multiple perspectives from diverse hospital personnel with different areas of expertise and work experience, we obtained a deeper understanding of the process. However, the data obtained are not sufficient to determine the extent to which strategies were effective and what components facilitated or impeded achieving the desired change. To that end, longitudinal data would be needed.
Conclusions
As Sandelowski and Leeman (2012) noted, hospitals are complex, multilayered social systems. The growing evidence-based practice advances in implementation science (Damschroder, Aron, et al., 2009) support an implementation process that incorporates attention to the values, practices, and interpersonal networks of health care personnel, as well as other situational factors present in these settings to promote adherence to IC policies (Sandelowski & Leeman). Indeed, the participants’ narratives underscored the utility of a systems approach framework when implementing a hospital-wide change in practice.
Given their accounts of the interpersonal dynamics in operation in the work environment, IC efforts would also benefit from further research on social engagement, building collaborations, and fostering collective action as a means of impacting HAI outcomes. Sophisticated, evidence-based social and behavioral approaches that promote the performance of new routines and the relinquishment of established behaviors might be useful resources for infection preventionists and epidemiologists to draw on when implementing adherence to changes in IC practice.
Acknowledgments
We thank the participating hospitals and their employees for their contributions to this study. We acknowledge the contribution of Shanelle Nelson to the coding of the qualitative transcripts, and thank Monique Carrero for her work on the preparation of the article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors received a grant from the National Institute of Nursing Research (R01-NR010107, P. Stone principal investigator).
Biographies
Victoria H. Raveis, PhD, is a research professor and director of the Psychosocial Research Unit on Health, Aging and the Community at New York University’s Colleges of Dentistry and Nursing, and a research professor at the NYU Global Institute of Public Health in New York, New York, USA.
Laurie J. Conway, RN, MSN, CIC, is an infection preventionist and PhD student at the Columbia University School of Nursing in New York, New York, USA.
Mayuko Uchida, MSN, GNP-BC, is a PhD student at Columbia University School of Nursing in New York, New York, USA.
Monika Pogorzelska-Maziarz, PhD, is a research associate at the Center for Health Policy, Columbia University School of Nursing, in New York, New York, USA.
Elaine L. Larson, PhD, FAAN, CIC, is associate dean for research and Anna C. Maxwell Professor of Nursing Research, Columbia University School of Nursing, and professor of epidemiology, Columbia University Mailman School of Public Health, in New York, New York, USA.
Patricia W. Stone, PhD, FAAN, is centennial professor in health policy and director of the Center for Health Policy at the Columbia University School of Nursing in New York, New York, USA.
Footnotes
Reprints and permissions: sagepub.com/journalsPermissions.nav
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Centers for Disease Control and Prevention. Health care-associated infections (HAIs): The burden. 2010 Retrieved from www.cdc.gov/hai/burden.html.
- Charles K, McKee L, McCann S. A quest for patient-safe culture: Contextual influences on patient safety performance. Journal of Health Services Research & Policy. 2011;16(Suppl 1):57–64. doi: 10.1258/jhsrp.2011.010093. [DOI] [PubMed] [Google Scholar]
- Clarke SP. Organizational climate and culture factors. Annual Review of Nursing Research. 2006;24(1):255–272. [PubMed] [Google Scholar]
- Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damschroder LJ, Banaszak-Holl J, Kowalski CP, Forman J, Saint S, Krein SL. The role of the champion in infection prevention: Results from a multisite qualitative study. Quality & Safety in Health Care. 2009;18(6):434–440. doi: 10.1136/qshc.2009.034199. [DOI] [PubMed] [Google Scholar]
- Elixhauser A, Steiner C. Infections with methicillin-resistant Staphylococus aureus (MRSA) in U.S. hospitals, 1993–2005. Rockville, MD: Agency for Healthcare Research and Quality; 2007. (Healthcare Cost and Utilization Project Statistical Brief No. 35) Retrieved from www.hcup-us.ahrq.gov/reports/statbriefs/sb35.pdf. [PubMed] [Google Scholar]
- Furuya EY, Dick A, Perencevich EN, Pogorzelska M, Goldmann D, Stone PW. Central line bundle implementation in US intensive care units and impact on bloodstream infections. PLOS ONE. 2011;6(1):e15452. doi: 10.1371/journal.pone.0015452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Williams A, Brinsley-Rainisch K, Schillie S, Sinkowitz-Cochran R. To ask or not to ask? The results of a formative assessment of a video empowering patients to ask their health care providers to perform hand hygiene. Journal of Patient Safety. 2010;79:71–80. doi: 10.1097/PTS.0b013e3181cb43c9. [DOI] [PubMed] [Google Scholar]
- Hawe P, Shiell A, Riley T. Theorising interventions as events in systems. American Journal of Community Psychology. 2009;43:267–276. doi: 10.1007/s10464-009-9229-9. [DOI] [PubMed] [Google Scholar]
- Klevens RM, Edwards JR, Richards CL, Jr, Horan TC, Gaynes RP, Pollock DA, Cardo DM. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Reports. 2007;122(2):160–166. doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohn LT, Corrigan J, Donaldson MS. To err is human: Building a safer health system. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- Lipsett PA, Swoboda SM. Handwashing compliance depends on professional status. Surgical Infections. 2001;2(3):241–245. doi: 10.1089/109629601317202722. [DOI] [PubMed] [Google Scholar]
- Marschall J, Agniel D, Fraser VJ, Doherty J, Warren DK. Gram-negative bacteraemia in non-ICU patients: Factors associated with inadequate antibiotic therapy and impact on outcomes. Journal of Antimicrobial Chemotherapy. 2008;61(6):1376–1383. doi: 10.1093/jac/dkn104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) System report, data summary from January 1992 through June 2004, issued October 2004. American Journal of Infection Control. 2004;32(8):470–485. doi: 10.1016/S0196655304005425. [DOI] [PubMed] [Google Scholar]
- Pogorzelska M, Stone PW, Furuya EY, Perencevich EN, Larson EL, Goldmann D, Dick A. Impact of the ventilator bundle on ventilator-associated pneumonia in intensive care unit. International Journal for Quality in Health Care. 2011;23(5):538–544. doi: 10.1093/intqhc/mzr049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- QSR International. NVivo (Version 9) 2010 [Computer software]Retrieved from www.qsrinternational.com.
- Reagan J, Hacker C. Laws pertaining to health care-associated infections: A review of 3 legal requirements. Infection Control and Hospital Epidemiology. 2012;33(1):75–80. doi: 10.1086/663204. [DOI] [PubMed] [Google Scholar]
- Resar R, Griffin FA, Haraden C, Nolan TW. Using care bundles to improve health care quality. Cambridge, MA: Institute for Healthcare Improvement; 2012. (IHI Innovation Series white paper) Retrieved from www.ihi.org/knowledge/Pages/IHIWhitePapers/UsingCareBundles.aspx. [Google Scholar]
- Sandelowski M, Leeman J. Writing usable qualitative health research findings. Qualitative Health Research. 2012;22:1404–1413. doi: 10.1177/1049732312450368. [DOI] [PubMed] [Google Scholar]
- Scott T, Mannion R, Davies HTO, Marshall MN. Implementing culture change in health care: Theory and practice. International Journal for Quality in Health Care. 2003;15(2):111–118. doi: 10.1093/intqhc/mzg021. [DOI] [PubMed] [Google Scholar]
- Sinkowitz-Cochran RL, Burkitt KH, Cuerdon T, Harrison C, Gao S, Obrosky DS, Jernigan JA. The associations between organizational culture and knowledge, attitudes, and practices in a multicenter Veteran Affairs quality improvement initiative to prevent methicillin-resistant Staphylococcus aureus. American Journal of Infection Control. 2012;40(2):138–143. doi: 10.1016/j.ajic.2011.04.332. [DOI] [PubMed] [Google Scholar]
- Stone PW, Dick A, Pogorzelska M, Horan TC, Furuya EY, Larson E. Staffing and structure of infection prevention and control programs. American Journal of Infection Control. 2009;37(5):351–357. doi: 10.1016/j.ajic.2008.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchida M, Stone PW, Conway L, Pogorzelska M, Larson EL, Raveis VH. Exploring infection prevention: Policy implications from a qualitative study. Policy, Politics and Nursing Practice. 2011;12(2):82–89. doi: 10.1177/1527154411417721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. HHS action plan to prevent healthcare-associated infections. 2009 Retrieved from www.hhs.gov/ash/initiatives/hai/action-plan/hhs_hai_action_plan_final_06222009.pdf.
- U.S. Department of Health and Human Services. National action plan to prevent healthcare-associated infections: Roadmap to elimination. 2012 doi: 10.1097/MLR.0000000000000030. Retrieved from www.hhs.gov/ash/initiatives/hai/infection.html. [DOI] [PubMed]
- Weiner BJ, Belden CM, Bergmire DM, Johnston M. The meaning and measurement of implementation climate. Implementation Science. 2011;6:78. doi: 10.1186/1748-5908-6-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welsh CA, Flanagan ME, Hoke SC, Doebbeling BN, Herwaldt L Agency for Healthcare Research Quality Hospital-Acquired Infections Collaborative. Reducing health care-associated infections (HAIs): Lessons learned from a national collaborative of regional HAI programs. American Journal of Infection Control. 2012;40(1):29–34. doi: 10.1016/j.ajic.2011.02.017. [DOI] [PubMed] [Google Scholar]


