Abstract
Despite the benefits of regular physical activity among older adults, physical activity rates are low in this population. The Program for Active Aging and Community Engagement (PACE) is an ongoing randomized controlled trial designed to compare the effects of two interventions on physical activity at 12 months among older adults. A total of 300 men and women aged 55 years or older will be randomized into either a healthy aging (HA) control intervention (n = 150), which is largely based upon educational sessions, or a prosocial behavior physical activity (PBPA) intervention (n = 150), which incorporates structured physical activity sessions, cognitive-behavioral counseling, and opportunities to earn food for donation to a regional food bank based on weekly physical activity and volunteering. The PBPA intervention is delivered at a local YMCA, and a regional grocery store chain donates the food to the food bank. Data will be collected at baseline, 3, 6, and 12 months. The primary outcome is physical activity as assessed by the Community Healthy Activities Model Program for Seniors (CHAMPS) Questionnaire at 12 months. Secondary outcomes include physical function and health-related quality of life. If successful, the PACE study will demonstrate that prosocial behavior and volunteerism may be efficaciously incorporated into interventions and will provide evidence for a novel motivating factor for physical activity.
Keywords: Randomized controlled trial, Older adults, Physical activity, Prosocial behavior, Community partnership
1. Introduction/background
Despite overwhelming evidence of the benefits of regular physical activity upon health outcomes for older adults [1], it is a distressing fact that physical activity rates have remained quite low in this population. Indeed, it is estimated that among adults who begin an exercise program, approximately 50% will discontinue it within 6 months [2]. The urgency of this issue is compounded in light of estimates that the number of US adults aged 65 years or older will reach 70 million in 2030 [3]. Several studies [4,5] have demonstrated that traditional physical activity prescription can be coupled with cognitive-behavioral strategies grounded in Social Cognitive Theory [6] to facilitate long-term activity; however, developing novel, effective strategies to promote physical activity will continue to be of prime importance to maintain and improve health among older adults.
One novel strategy entails providing older adults with long-term opportunities to aid charitable causes through their own regular physical activity. For instance, many episodic “charity events” are purposely designed to combine physical activity with prosocial behavior, defined as “voluntary, intentional behavior that results in benefits for another” [7]. Usually, charity events draw participants from a large range of fitness, age, and socioeconomic categories, and generate considerable media interest. For example, the American Heart Association estimates that its Walk for Heart drew more than 1 million walkers in 2012 [8]. There is an abundance of other such events that are held yearly across the United States, such as the Arthritis Walk, the March of Dimes Walk for Babies, and numerous such events for cancer organizations. Also, many competitive races are often accompanied with non-competitive “fun walks” involving light- to moderate-intensity activity. Although the focus of these events is fundraising, it is intriguing that they inspire large numbers of possibly otherwise underactive individuals to participate in a single physical activity session. Thus, an interesting, yet largely unexplored research question concerns whether prosocial behavior may be successfully incorporated into programs to promote long-term physical activity.
Prosocial behavior, a long-standing and broad construct, garnered considerable research interest during the 1960's through the 1990's [9], with particular interest in factors that affect rendering aid in specific situations such as emergencies. More recently, prosocial behavior has been associated with positive outcomes in the problem solving and drug dependence literature, particularly among adolescents [10]. Volunteerism, a form of prosocial behavior, has also been associated with positive outcomes among older adults [11–15]. Of note, the Baltimore Experience Corps Program [16], which places predominately older African-American volunteers in public elementary schools [17], is designed to improve academic outcomes of children and physical activity, cognitive and social outcomes of volunteers [18]. However, there is little research on whether prosocial behavior can be used to produce favorable long-term health outcomes, and whether prosocial behavior and volunteerism may be employed within physical activity interventions.
In consideration of these issues, we designed a randomized trial to assess the effect of a theory-driven, cognitive-behavioral intervention that incorporates prosocial behavior and volunteerism into a physical activity intervention that is compared to a control group. Two particular strengths of the study are that it involves a partnership with three community-based organizations, and that the physical activity intervention is based largely upon the self-regulatory aspects of Social Cognitive Theory [6].
2. Study design/methods
2.1. Overview and design
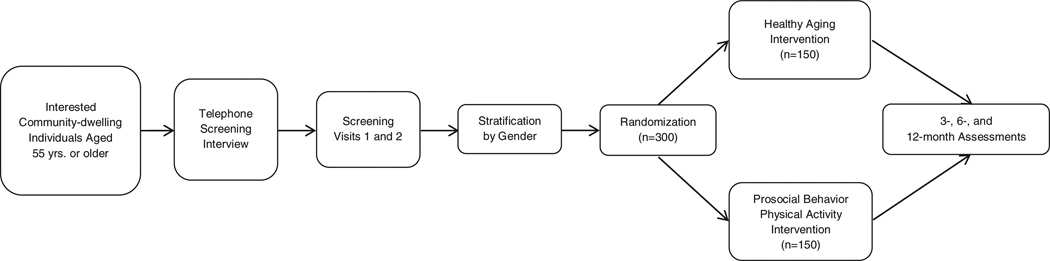
The Program for Active Aging and Community Engagement (PACE) is an ongoing two-arm, randomized controlled trial designed to investigate the relative effects of two interventions on physical activity (the primary outcome) at 12 months post-randomization in underactive adults aged 55 to 80 years. Secondary objectives include assessing the relative effect of the interventions on physical function and health-related quality of life. A total of 300 participants ultimately will be randomized into either a Prosocial Behavior Physical Activity (PBPA) intervention (n = 150) or a Healthy Aging (HA) control group (n = 150). Participants will be recruited in 14 groups, or “waves”,which each will consist of an average of approximately 22 participants. The primary and secondary outcomes are assessed using standardized protocols by trained personnel who are blinded to participants study arm assignment. Outcomes are assessed at baseline, 3, 6, and 12 months (Fig. 1, Table 1).
Fig. 1.
Overview of procedures.
Table 1.
PACE trial-wide measures by time point.
| Measure | Data collection time point |
||||
|---|---|---|---|---|---|
| Baseline | 1.5 monthsa | 3 months | 6 months | 12 months | |
| Patient rights and responsibilities | |||||
| Informed consent | X | ||||
| Emergency contact information | X | ||||
| Physician contact information | X | ||||
| Demographics and medical information | |||||
| Screening telephone interview | X | ||||
| Participant demographics | X | ||||
| Medications | X | X | X | X | |
| Tobacco and alcohol Use | X | X | |||
| Cognitive function | |||||
| Montreal Cognitive Assessment (MoCA) | X | X | |||
| Digit symbol substitution test | X | X | |||
| Health-related quality of life, perceived stress, and exercise-related affect | |||||
| VR-12 | X | X | X | X | |
| Centers for Epidemiological Studies — Depression Scale (CES-D) | X | X | X | X | |
| Exercise-induced feeling inventorya | X | X | X | X | |
| Perceived stress scale | X | X | X | X | |
| Self-efficacy/outcome expectations for physical activity | |||||
| Performance-based efficacya | X | X | X | X | |
| Barriers efficacya | X | X | X | X | |
| Outcome expectations for exercisea | X | X | X | X | |
| Prosocial behavior exercise surveya | X | X | X | X | |
| Exercise Motivations Inventory — 2a | X | X | X | X | |
| Performance testing/physical functions | |||||
| Pepper Assessment Tool for Disability (PAT-D) | X | X | X | X | |
| Short physical performance battery | X | X | X | X | |
| Handgrip strength test | X | X | X | X | |
| Anthropometric measures (height, weight, waist circumference) | X | X | X | X | |
| Physical activity | |||||
| CHAMPS physical activity questionnaire | X | X | X | X | |
| Accelerometry | X | X | X | X | |
| Volunteerism and social provisions | |||||
| Social capital survey questions on volunteerism and giving | X | X | X | X | |
| Social provisions | X | X | X | ||
PBPA participants only.
The following hypotheses were generated for the objectives;
Participants in the PBPA intervention will demonstrate greater levels of physical activity at 12 months compared to those in the HA intervention;
Participants in the PBPA intervention will demonstrate more favorable scores on physical performance tests at 12 months compared to the HA intervention; and
Participants in the PBPA intervention will demonstrate more favorable health-related quality of life (HRQL), perceived stress, and exercise-related affect compared to participants in the HA intervention.
2.2. Eligibility
The eligibility criteria were selected to ensure the enrollment of participants who are a representative sample of older, underactive community-dwelling adults who have no medical conditions that would contraindicate participation in unsupervised, independent physical activity. Furthermore, participants have to demonstrate a willingness to adhere to the programs by successfully completing a behavioral run-in.
To be eligible for participation in the PACE study, interested individuals have to meet the following inclusion criteria: (a) age 55 years or older; (b) self-report of underactive physical activity, with less than 90 min of structured (i.e. purposeful) exercise participation per week during the past month; (c) no self-report of major psychological diagnoses (e.g. schizophrenia) for the preceding 3 years; (d) residence within 20 miles of the study site; (e) no time or work conflicts during times of the sessions; (f) plans to remain in the area for the duration of the study, and (g) successful completion of a behavioral run-in during screening.
Individuals are deemed ineligible if they meet any of the following exclusion criteria: (a) self-reported inability to walk for at least 10 min without having to stop due to pain; (b) self-report of falling within the past year; (c) self-report of cardiovascular disease; (d) self-report of diabetes; (e) self-report of liver disease; (f) self-report of renal disease; (k) directly-measured resting systolic blood pressure >160 mmHg, or diastolic blood pressure >100 mmHg; (l) Body Mass Index (BMI) >40 kg/m2; (m) self-report of psychiatric illness, such as treatment for major depression or schizophrenia within the past 3 years; (n) Center for Epidemiologic Studies — Depression (CES-D) score >22 (suggestive of major depression) during screening; (o) Montreal Cognitive Assessment (MoCA) score <26 during screening; (p) self-report of significant hearing or sight impairments; (q) self-report of alcohol consumption >14 drinks/week; (r) inability to read or speak English; (s) living in the same household as an already randomized participant; (u) current participation in any medical intervention study; and (v) judgment of investigators, based upon feedback from team members. However, it is important to note that potential participants with several highly prevalent conditions will be deemed eligible. For example, individuals with osteoarthritis will not be excluded from the study; nor will persons with controlled hypertension. Persons with Class I or Class II obesity will also be considered to be eligible for the study. Persons with rheumatoid arthritis, mild emphysema, bronchitis or thyroid issues will also be eligible, upon written physician approval. Eligibility is assessed using a combination of telephone screening and in-person visits to the assessment center.
2.3. Recruitment, screening and randomization
Recruitment of participants for PACE began in March 2012, and continues as of July 2013. Potential participants are identified through a variety of approaches, including the following: (a) direct referral to study staff from the Wake Forest Claude D. Pepper Older Adults Independence Center, (b) targeted mass mailings to specific zip codes in the Forsyth County, NC area; (c) placement of advertisements in local newspapers and websites; and (d) placement of informational brochures at physicians' offices within Wake Forest Baptist Health. Additional planned recruitment activities include: (e) in-person presentations at community-based organizations, including independent living centers, churches, and social organizations; and (f) use of social media, including placement of advertisements through email and the use of a study website geared toward participants.
Individuals who are interested in participating in the study contact the study staff (authors C.M-F., S.J.H., N.R., and D.B.), who administer a telephone screening interview to determine initial eligibility. If potential participants “pass” the telephone screening interview, they are invited to visit the assessment center for two screening visits (SV1 and SV2) which are held one week apart. If feasible, before SV1, potential participants are mailed a copy of the informed consent. At the beginning of SV1, study staff review the informed consent form with the potential participant, who signs the informed consent before any assessments begin. Also, because PBPA participants are asked to self-monitor physical activity for 9 months, all potential participants are asked to complete a one-week behavioral run-in between SV1 and SV2. During this period, volunteers are asked to record their physical activity onto a paper log. At SV2, this log is reviewed for completeness by the study staff. Individuals who are unwilling or unable to return a satisfactorily completed log may have difficulty with the self-monitoring that is a central component of the PBPA intervention, and thus are deemed to be ineligible. Participants who “pass” the screening visits are deemed eligible for randomization. Eligible and interested participants are randomly assigned with equal probability to one of the two intervention arms (PBPA or HA), using a variably sized random block allocation. The randomized assignments are accessed through the study website and are concealed from the study staff. We anticipate accruing 25% male and 20% African-American participants.
2.4. Informed consent
The study protocol and informed consent documents have been approved prior to the initiation of recruitment procedures by the Wake Forest School of Medicine Institutional Review Board. As noted earlier, all participants complete an informed consent prior to screening assessments. In addition, participants are asked to provide consent to use their photographs for research purposes and to permit contact for invitation to future studies. However, volunteers can refuse permission for photographs and future contact without impacting their eligibility for this study.
2.5. Measures
Assessments of study measures are obtained at baseline, 1.5 months (PBPA only), 3 months, 6 months, and 12 months post-randomization (Table 2). Most of the measures have established validity and reliability which have been demonstrated in prior studies of physical activity interventions among older adults. In addition, assessments are administered by trained personnel using standardized procedures as outlined in a Manual of Procedures. Below, the measures are described in further detail.
Table 2.
List of healthy aging intervention topics.
| Topic |
|---|
| Welcome to the PACE Study — part 1: general procedures |
| Getting started: what is healthy aging? |
| Become more active |
| Falls and fractures |
| Lower your systolic blood pressure |
| Stop smoking |
| Participate in cancer screenings |
| Regulate your blood glucose |
| Lower your LDL cholesterol |
| Maintain healthy bones, joints and muscles |
| Maintain social contact |
| Combat depression |
| Get adequate sleep |
| Urinary incontinence |
| Dietary supplements |
| Proper foot care |
| Forgetfulness: knowing when to ask for help |
| Preventing and treating hearing loss |
| Managing your finances and avoiding scams |
| Are you part of the sandwich generation? |
| Proper dental care |
| Preventing and managing gout |
| Shingles |
| Holistic approaches to medicine |
| Gearing up for the holidays |
| Healing touch |
| Pursue your passion |
| Congratulations on completing the healthy aging program! |
| Field trip: healthy food choices tour of Lowe's foods |
| Field trip: tour of second harvest food bank |
2.5.1. Primary outcome: Physical activity
Physical activity is assessed using both self-report and objective measures. The Community Healthy Activities Model Program for Seniors (CHAMPS) Questionnaire [5] is used to measure self-reported physical activity. The CHAMPS is a validated, 41-itemmeasure designed to assess physical activity among adults aged 50 years or older. Of the 41 items, 27 items are scored to yield estimates of weekly kilocalories expended in moderate- or vigorous-intensity physical activity. In addition, the CHAMPS can provide estimates of duration and frequency of moderate- or vigorous-intensity physical activity. The CHAMPS is administered via interview with PACE staff to reduce the likelihood of over-reporting of physical activity.
Two of the three reviewers of the original NIH proposal recommended that accelerometry be assessed along with self-reported physical activity. Thus, starting with the fourth group of participants (“Wave” 4), objectively assessed physical activity will be obtained on approximately 220 participants using the LIFECORDER EX-Plus accelerometer (Suzuken Kenz Inc. Limited, Japan), which has been validated for physical activity among older adults [19]. Participants will wear the LIFECORDER EX-Plus on their right hip attached to a waistband or belt during all waking hours, except when showering, bathing or swimming, for 7 consecutive days between SV1 and SV2, and during the 3-month, 6-month and 12-month assessments. In this study, moderate-intensity activity will be defined as intensity levels of 3 to 6 metabolic equivalents (METS), and vigorous-intensity physical activity will be defined as >6 METS. Participants will record the times they put on and take off the accelerometer on a self-monitoring log for one week after the 3-month, 6-month, and 12-month assessment appointments. After the participants return the accelerometer, data will be downloaded to a computer using proprietary software. The LIFECORDER EX provides estimates of total daily steps and daily minutes of light-, moderate-, and vigorous-intensity of physical activity in as little as 4-sec epochs. The display of the accelerometer will be locked so that participants will not able to view these estimates.
2.5.2. Secondary outcomes
2.5.2.1. Volunteerism and prosocial behavior
Volunteerism and giving contributions over the past month is assessed using 11 ‘yes/no’ items from the Social Capital Benchmark Community Survey [20]. The items assessed include volunteering at cultural or arts organizations, places of worship, healthcare organizations, schools or youth groups, volunteering to help the poor and needy, and working on community projects. Giving contributions to religious and non-religious charities and organization is also queried, as is working on community projects. In addition, an item queries donations of blood, platelets, plasma, bone marrow or other body parts. An added item queries participants regarding participating in “charity walks” or other charity events that involved exercise or physical activity. The frequency of “yes” responses is summed to calculate the score.
A 7-item, internally-developed instrument (the Prosocial Behavior and Exercise Survey) queries PBPA participants regarding their perceptions of how the ability to earn cans or boxes of food for donation influences physical activity and Social Cognitive Theory cognitive processes. Each item uses a 5-item scale ranging from 0 (does not help at all) to 4 (helps a great deal). Scores on this instrument range from 0 to 28, with higher scores indicating more favorable perceptions regarding the ability to earn cans for food for donation. Examples of items on the Prosocial Behavior and Exercise Survey are included in Table 3.
Table 3.
Sample items from the Prosocial Behavior and Exercise Survey.
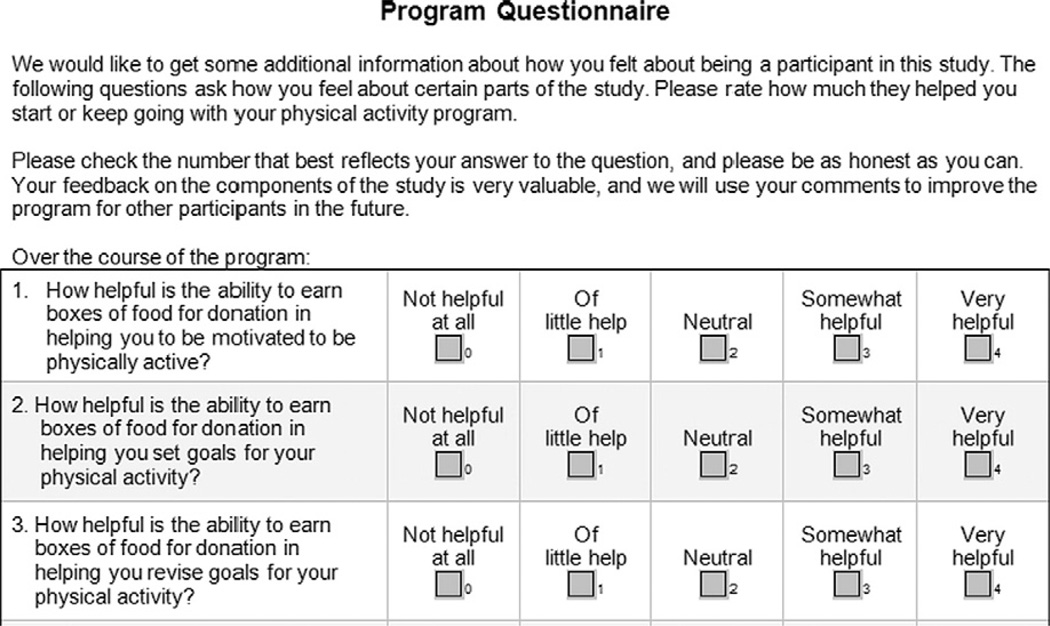 |
2.5.2.2. Cognitive function
Cognitive function is assessed at baseline and at 12 months using two measures. The Montreal Cognitive Assessment (MoCA) [21], which is administered via interview, is designed as a brief screening tool for cognitive dysfunction. It assesses several cognitive domains, including attention and concentration, executive functions, memory, language, visuoconstructional skills, conceptual thinking, calculations and orientation. Scores on the MoCA range from 0 to 30 with higher scores indicating less cognitive dysfunction. During the baseline assessment, individuals with a MoCA score <26 are deemed ineligible.
The Digit Symbol Substitution Test assesses attention, concentration, persistence, vasomotor coordination, and perceptual speed [22]. Participants are given a series of numbered symbols, and then are asked to draw the appropriate symbols in boxes below a list of 140 random numbers, arranged in 7 rows as quickly as possible for 2 min. The first row serves as a “practice” row, and is not scored. The total score is the number of boxes completed correctly. Scores on the DSST range from 0 to 133, with higher scores indicating better function.
2.5.2.3. Physical performance
The Short Physical Performance Battery (SPPB) is used to objectively assess physical performance in PACE. The SPPB [23] is a validated battery of 3 tests (3 hierarchical balance tests, 4-meter walk and repeated chair stands) of physical function. Each of the three tests is scored from 0 to 4, in which 0 represents an inability to complete the test, and 4 represents the highest level of performance. Study staff follow a script as described by Guralnik et al. to administer the tests.
The Pepper Assessment Tool of Disability (PAT-D) [24] is used to assess self-reported physical function. The PAT-D is a 19-item questionnaire that includes 3 domains, including (a) basic activities of daily living (e.g., moving in and out of a chair, moving in and out of bed, using the toilet, getting in and out of a car, walking across a small room); (b) mobility (e.g., including walking several blocks, lifting heavy objects, walking one block, lifting or carrying 10 lbs; and (c) instrumental activities of daily living (e.g., participating in community activities, visiting with relatives or friends, using the telephone, taking care of a family member). Higher scores on each of the three domains, as well as the summary score (calculated as the mean of the three domains) indicate higher perceived disability.
2.5.2.4. Health-related quality of life (HRQL), perceived stress, and exercise-related affect
Self-reported generic health status is assessed using the Veterans Rand Short-Form 12 (VR-12) [25,26]. The VR-12 is a 12-item questionnaire that is derived from the SF-36 [27], and consists of 8 scales (general health perceptions; physical functioning; role limitations due to physical and emotional problems; bodily pain; energy–fatigue; social functioning and mental health), from which 2 composite scales (Mental Health and Physical Health Summary Scores) can be calculated. Higher scores indicate more favorable health status.
Perceived stress is assessed using the 10-itemversion of the Perceived Stress Scale (PSS) [28]. The PSS queries participants about the degree to which they feel life has been stressful, unpredictable or uncontrollable over the past month. Scores range from 0 to 40,with higher scores indicating greater stress.
Exercise-related affect is assessed using the Exercise Feeling Inventory — Chronic version (EFI-C) [29]. The EFI-C consists of 12 items in which participants are asked how often they have experienced various moods or feelings over the past month. Responses are scored using a 6-point scale ranging from “all of the time” to “none of the time”. The EFI-C has two subscales, including pleasant feeling states (range of 0 to 45) and physical exhaustion (range 0 to 15). Higher scores indicate increased perception of each factor.
2.5.2.5. Social cognitive process measures
The following measures based upon Social Cognitive Theory [6] cognitive processes are assessed in the PBPA intervention. These measures are not assessed in the HA intervention, with the assumption that the majority of participants would prefer to be randomized into the physical activity intervention. Thus, assessing multiple measures of perceptions of physical activity among the HA participants may result in increased resentful demoralization, and thus potentially negatively impact adherence and retention of HA participants. A 14-item barrier self-efficacy measure [30] assesses perceived ability to be physically active when confronted with several barriers, ranging from poor weather to lack of support from family and friends. Scores are calculated by summing the 14 items and transforming them so that values range from 0 to 100.
The 13-item Outcome Expectancies for Exercise scale (OEE-2) [31] was developed to assess positive and negative expectations that older adults associate with exercise. For each item, scores range from 1 (“Strongly Disagree”) to 5 (“Strongly Agree”). Two scores may be computed from the OEE-2, which comprise of positive expectations (9 items), and the 3 items which assess negative expectations, with higher scores indicating increased positive or negative expectations.
An internally-developed 12-item form has been developed to assess performance efficacy for walking (6 items) and using cardiovascular equipment (6-item). For each item, scores range from 0 (“Not at all Confident”) to 10 (“Completely confident”). Scores for walking efficacy and performance efficacy range from 0 to 60, with higher scores indicating increased efficacy.
2.5.2.6. Social Provisions Scale
The Social Provisions Scale [32] is used to assess perceived social support in generalized settings. This scale consists of 24 items, with 6 subscales, each of which consists of 4 items. The subscales include attachment, social integration, reassurance of worth, reliable alliance, guidance, and opportunity for nurturance. In addition, an overall score may be calculated from summing all of the items. Each item is scored on a 4-point Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree). Negatively worded items are reverse scored. For the overall score, scores range from 24 to 96, with higher scores representing increased perception of social support.
2.5.2.7. Exercise Motivation Inventory — 2
The Exercise Motivation Inventory — 2 (EMI-2) [33] is used to assess motivations for exercise among regular exercisers and non-exercisers. This 51-item instrument queries individuals regarding the degree to which they feel that each statement is, or would be true. Each statement is scored using a 6-point Likert scale ranging from 0 (not at all true for me) to 5 (very true for me). The EMI-2 has 14 scales, including appearance, nimbleness, strength and endurance, health pressures, ill-health avoidance, positive health, weight management, competition, affiliation, social recognition, challenge, enjoyment, revitalization, and stress management. Scales are scored by using the mean score of the items for each scale.
2.5.3. Web-based data entry system
Data from the assessments are entered from the physical forms into a web-based data entry system (developed by author R.J.H.) built using Microsoft Notepad, Microsoft Access, the javascript scripting language and Cascading Style Sheets to develop Active Server Pages (.asp and .aspx) web forms. These forms include logical and range checks to ensure that only specific values can be entered into the “backend” Microsoft Access database that resides on a secure server. These tables are joined together in SAS to generate analysis files, and additional edit checks and reports are generated at that stage.
To ensure data quality, data are “double-entered” on a periodic basis onto a duplicate web-based data entry system, and variables are compared using the SAS PROC COMPARE procedure. Discrepancies between the two databases are resolved by reviewing the original physical forms, and if necessary, correcting them in the original database.
2.6. Interventions
2.6.1. Healthy Aging (HA) Intervention
The HA Intervention is designed to represent an active control condition that is not expected to impact physical activity or physical function. However, as noted by Wesche-Thobaben [34], retention of the control group is essential to the success of a trial. Thus, considerable attention is given to make the HA intervention interesting and enjoyable for participants. In this intervention, participants meet weekly with the PACE interventionists (authors L.G., B.S., J.G. and K.Y.) for approximately 1 h during the first 3 months (Phase I), biweekly during months 4 to 6 and monthly during months 7 to 9 (Phase 2), for a total of 21 sessions. During months 10 to 12 (Phase 3), no sessions are offered. Also, at the beginning of each session, a small raffle is held, and the “winner” receives an inexpensive (≤$10) gift (e.g. USB flash drive) or gift card. Afterwards, participants engage in a short, 10-min session of light-intensity chair exercise and stretching, followed by a 45-min educational lecture and group discussion on topics relevant to healthy aging (e.g. sessions on healthy nutrition, awareness of financial “scams” targeted toward older adults, forgetfulness, and falls and fractures). The educational content is largely based on the University of Pittsburgh 10 Keys to Healthy Aging and the National Institute on Aging's Age Pages, and is delivered via a combination of PowerPoint presentations and group discussions. Participants in the HA intervention receive a participant manual, and handouts of each session. Participants may also accrue “PACE points” based on attendance to sessions, which they can redeem for small items (e.g. coffee mugs). The current list of all session topics offered is described in Table 2.
Due to the wide age range of participants, additional sessions have been developed to focus on issues such as the “sandwich generation”, financial literacy, navigation of the Wake Forest Baptist Health healthcare system, proper dental and oral care, urinary incontinence, gout and shingles. In addition, the sessions offered are tailored to the characteristics of each wave. For example, if there are no current smokers in a wave, the smoking cessation session is substituted with another session. Along with the raffles, HA participants receive t-shirts, tote bags, and small gifts in order to enhance adherence and retention. HA participants also engage in “field trips” and other group activities, including a “healthy nutrition” tour at Lowes Foods®, a regional grocery chain, and a tour of Second Harvest Food Bank of Northwest North Carolina. Upon completion of the 12-month assessment, participants in the Healthy Aging condition receive a 1-yearmembership to the William G. White, Jr. YMCA, as well as an Omron HJ-112® pedometer, and are referred to the Active Older Adults coordinator at the “Y” for an initial visit.
2.6.2. Prosocial Behavior Physical Activity (PBPA) Intervention
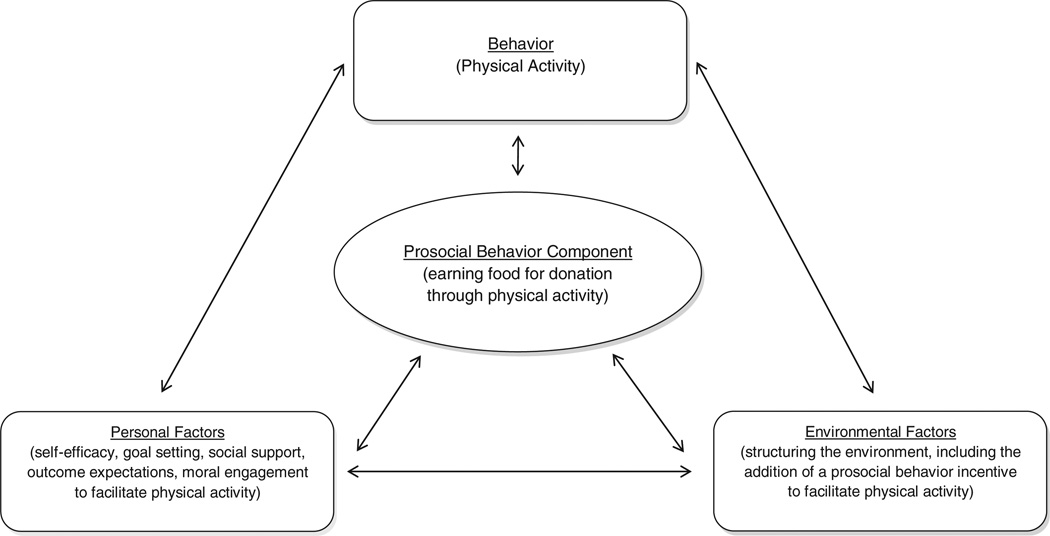
The primary goal of the PBPA intervention is to promote independent physical activity by embedding incentives for prosocial behavior and volunteerism within a physical activity program that is based upon Social Cognitive Theory [6]. Social Cognitive Theory, an established theory of behavioral change developed by Albert Bandura, posits a dynamic and reciprocal determinism between environmental factors, personal factors, and behavior (Fig. 2). Social Cognitive Theory assumes that humans have several capabilities, including symbolizing and forethought capability; vicarious ability (or modeling), self-regulatory capacity, and self-reflective capacity. The PBPA intervention addresses each of these aspects, by incorporating the prosocial behavior component along with behavioral strategies to teach participants how to self-regulate physical activity and use each other's experiences to aid in setting, achieving, and maintaining goals.
Fig. 2.
Reciprocal determinism in social cognitive theory and prosocial behavior.
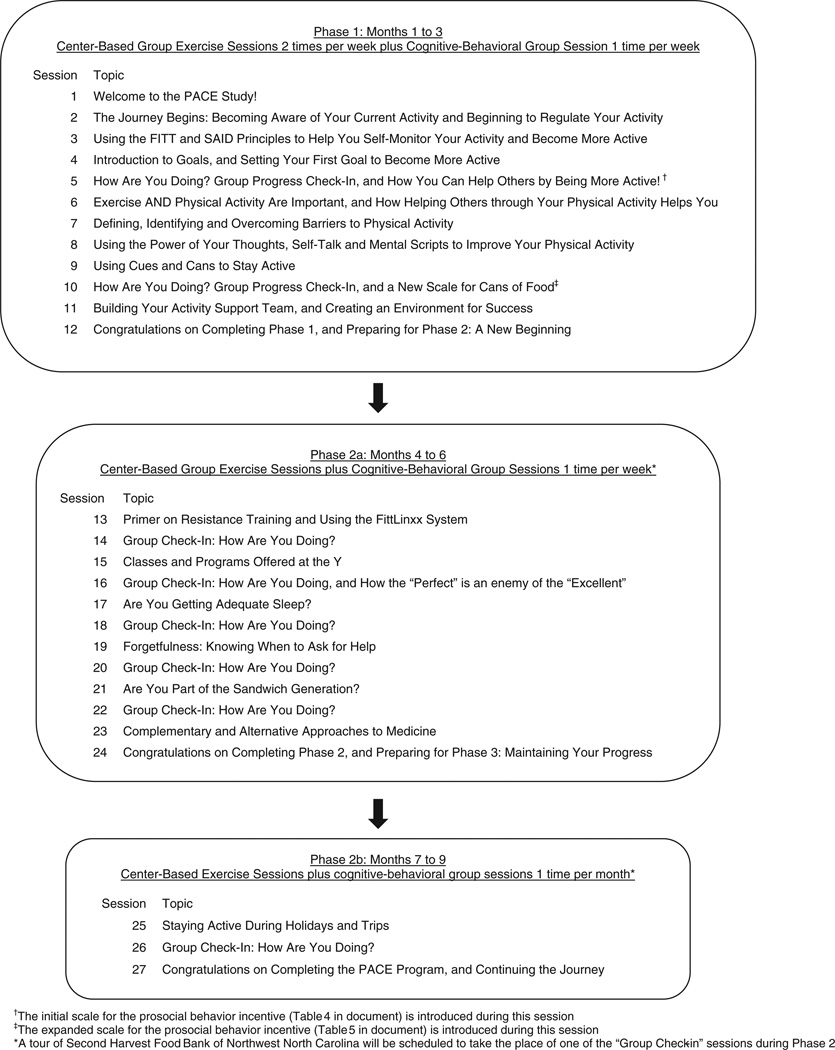
Participants receive a total of 39 center-based sessions at the William G. White, Jr. Family YMCA over a period of 9 months, divided into three phases, which involve a process of phased decrease in staff and group dependency (Fig. 3). In addition, the PBPA intervention is designed to allow participants to avail themselves of the multiple opportunities for physical activity that exist at the “Y”. In Phase 1 (months 1 to 3), participants meet for structured exercise sessions 2 times per week. During Phase 2 (months 4 to 9), participants meet 1 time per week during months 4 to 6 and once per month during months 7 to 9. During Phase 3 (months 10 to 12), no staff-initiated contact is provided.
Fig. 3.
Timeline of sessions in the PBPA intervention.
At the beginning of the intervention, participants are informed that their first month of sessions at the “Y” will focus on learning on how to engage in physical activity safely and effectively using the Frequency, Intensity, Time and Type (FITT), and the Specific Adaptations to Imposed Demands (SAID) Principles. Each exercise session consists of 4 phases: measurement of pre-exercise blood pressure and weight (5 min); a warm-up (5 to 10 min); an aerobic stimulus phase (30 to 40 min), and a cool-down phase that includes stretching exercises (5 to 10 min). Participants are encouraged to exercise at a training heart rate range of 50% to 85% using the Karvonen formula, and a rating of perceived exertion (RPE) between 11 and 15. Participants are instructed to monitor and record their heart rate and RPE after 20 min of exercise, and after the cool-down. Along with the PACE interventionists (authors L.G., B.S., J.G. and K.Y.), the coordinator of the Active Older Adults Program at the William G. White, Jr. YMCA assists in delivering the exercise sessions. The interventionists record the attendance at each session and enter the values into the web-based data entry system. Also, starting at the end of month 2, participants are provided with a monthly report of their attendance to the center-based sessions and amount of home-based exercise.
In addition, during months 1 through 3, participants engage in a weekly, 45-minute session of group-based, cognitive-behavioral counseling based on Social Cognitive Theory, in which participants learn behavioral skills and self-regulatory process (e.g. self-monitoring to promote self-awareness, goal setting, social support, use of technical feedback, self-instruction and self-talk and interpreting physiological feedback) to promote physical activity. Participants are also encouraged to identify barriers to physical activity and are taught how to problem-solve to prevent or circumvent them. In addition, participants set goals for each week using the FITT Principle. The session topics and timelines are provided in Fig. 3.
During the second week of sessions, participants are provided with the first two tangible tools they will use to monitor physical activity. The Omron HJ-112® pedometer is provided to participants, along with a calendar for weeks 2, 3 and 4. Participants are taught how to use the pedometer, and their stride lengths are set. Participants are also shown how to track their daily minutes of activity and pedometer steps using the calendar.
In addition, at the beginning of month 2 (Session 5: How Are You Doing?…), participants are informed that based upon their weekly physical activity or volunteer minutes through month 9 that Lowes Foods®, a grocery store chain that operates in North Carolina, South Carolina and Virginia, will donate packaged food (i.e. cans, boxes or bags of food) to the Second Harvest Food Bank on their behalf.
The introductory session for the prosocial behavior component starts as a review session of the participants' progress to date. Participants are asked to reflect upon their first month of regular physical activity and share accomplishments they have made. Afterwards, the prosocial component is introduced as a newly-developed tool that is designed to help participants remain active. The popularity of “charity” walk and run events are discussed, with several examples of national and local events. Participants share if they have ever participated in a walk or run, what the experience was like, and why they participated. It is also discussed that while these walk/runs are popular, they are often single events, and don't provide long-term opportunities for donations through physical activity. Also, the fact that often a fee is required to participate in these events is discussed. Thus, in response to these limitations, participants are informed that a new system has been developed with the intention of allowing persons to engage in long-term physical activity that can provide benefits to themselves and to others.
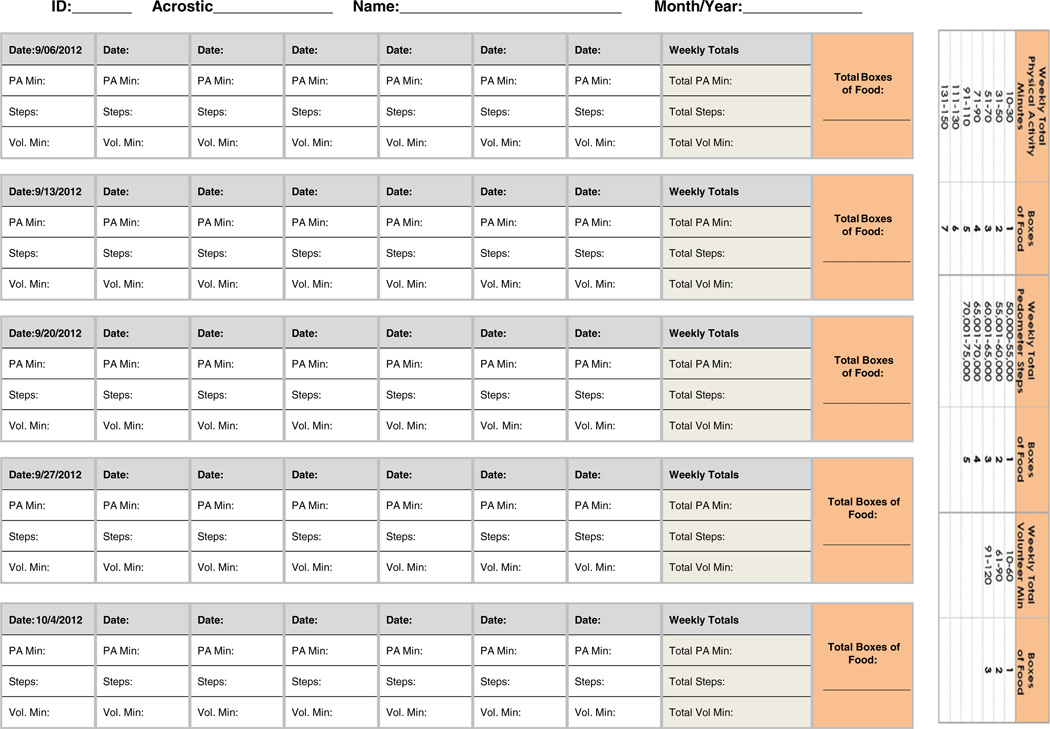
Participants are provided with new calendar, which includes a scale for cans of food that will be used for the next 4 weeks that will allow participants to earn cans or boxes of food based on their weekly minutes of physical activity, pedometer steps, and volunteer minutes. The donation scale is shown in Table 4, with its accompanying calendar shown in Fig. 4. The purpose of the scale is to incorporate prosocial behavior to encourage participants to attain 150 min of weekly physical activity by the end of Phase 1. This initial scale is based on the joint recommendation from American College of Sports Medicine and American Heart Association for older adults [35], which recommends at least 150 min of moderate-intensity physical activity per week. Indeed, this scale is structured to facilitate mastery experiences during the initial phase of a physical activity program, so that attaining at least 130 min of moderate-intensity physical activity per week (approximately 85% of the ACSM recommendation) will result in earning the maximum number of cans or boxes. Participants are also provided with information from the Second Harvest Food Bank of Northwest North Carolina regarding the issue of hunger in the region, and the positive impact of donating food on families in the region.
Table 4.
Scale for cans of food based on weekly physical activity and volunteer minutes for weeks 5 to 9 of the PBPA intervention.
| Weekly total physical activity minutes | Boxes of food | Weekly total pedometer steps | Boxes of food | Weekly total volunteer minutes | Boxes of food |
|---|---|---|---|---|---|
| <10 | 0 | <50,000 | 0 | <10 | 0 |
| 10–30 | 1 | 50,000–55,000 | 1 | 10–60 | 1 |
| 31–50 | 2 | 55,001–60,000 | 2 | 61–90 | 2 |
| 51–70 | 3 | 60,001–65,000 | 3 | >90 | 3 |
| 71–90 | 4 | 65,001–70,000 | 4 | ||
| 91–110 | 5 | >70,000 | 5 | ||
| 111–130 | 6 | ||||
| >130 | 7 |
Fig. 4.
Home-based PACE physical activity log for PBPA participants, weeks 5 to 9.
In addition, during the goal setting portion of each session, it is recommended that by the end of week 9 in the program, participants are attaining at least 150 min of physical activity per week. The scale for pedometer steps is based upon literature that suggests that adults who take between 7500 and 10,000 steps per day (or 52,000 to 70,000 steps per week) are considered to be active [36,37]. The scale is cumulative, so that the combination of physical activity minutes, steps, and volunteer minutes determine the number of cans or boxes a participant earns each week. For example, if for a given week, “Participant A” has a total of 150 min of physical activity (7 boxes), 56,000 pedometer steps (2 boxes), and 30 min of volunteer time (1 box), he or she will earn 10 cans or boxes of food for donation to Second Harvest Food Bank for that week.
The initial scale is included in a new calendar that participants use for the next 4 weeks, and is used in the weekly goals that participants set each week. In month 3 (Session 10), a new scale (Table 5), with a new calendar is introduced, which contains the categories of the initial scale plus additional categories of physical activity minutes and volunteer minutes. The purpose of the expanded scale is to provide participants who are attaining the highest levels of the initial scale with additional motivation and positive challenge. In addition, participants are provided with a list of charity walk-runs for the next 6 months within a 50-mile radius of zip code 27101 (the zip code of the William G. White, Jr. Family YMCA) based upon the www.active.com website. As stated earlier, during Phase 2 (months 4 to 9), there is a phased decrease in staff-initiated contact. However, participants are able to continue to earn boxes of food for donation through month 9. In addition, during Phase 2, PBPA participants receive a tour of the Second Harvest Food Bank of Northwest North Carolina. During months 2 through 9, participants will receive a monthly report that summarizes their center-based and total physical activity. At the end of months 2 through 9, the study staff will generate a report of the number of boxes earned for that month to personnel at Lowes Foods®, who in turn will prepare the food for delivery to Second Harvest Food Bank on behalf of the study. The food to be delivered is selected by the community nutritionist for Lowes Foods® to ensure a high nutritional value.
Table 5.
Scale for cans of food based on weekly physical activity and volunteer minutes for weeks 10 to 36 of the PBPA intervention.
| Weekly total physical activity minutes | Boxes of food | Weekly total pedometer steps | Boxes of food | Weekly total volunteer minutes | Boxes of food |
|---|---|---|---|---|---|
| <10 | 0 | <50,000 | 0 | <10 | 0 |
| 10–30 | 1 | 50,000–55,000 | 1 | 10–60 | 1 |
| 31–50 | 2 | 55,001–60,000 | 2 | 61–90 | 2 |
| 51–70 | 3 | 60,001–65,000 | 3 | 91–120 | 3 |
| 71–90 | 4 | 65,001–70,000 | 4 | 121–150 | 4 |
| 91–110 | 5 | >70,000 | 5 | >150 | 5 |
| 111–130 | 6 | ||||
| 131–150 | 7 | ||||
| 151–160 | 8 | ||||
| 161–170 | 9 | ||||
| 171–180 | 10 | ||||
| 181–190 | 11 | ||||
| 191–195 | 12 | ||||
| 196–200 | 13 | ||||
| 201–205 | 14 | ||||
| >205 | 15 |
In the context of Social Cognitive Theory (Fig. 2), the development of the prosocial behavior physical activity intervention represents an attempt to provide a sustainable, constructed organizational environment that may facilitate physical activity [38]. In addition, the feedback regarding the food earned may be used to provide participants with proximal, and hopefully salient feedback regarding their physical activity, which also may be a useful means of improving self-efficacy through mastery experiences. Also, self-efficacy may be enhanced by verbal persuasion during the session by the interventionists and other participants, and by written persuasion through the monthly reports, which will include performance-based feedback on how many cans or boxes have been earned for the month. In addition, if participants witness each other improving in the amount of food earned, this may be beneficial in providing modeling and positive vicarious experiences, which may enhance self-efficacy. Also, the feedback regarding the amount of food earned may be shared among participants to foster social support, and perhaps collaboration regarding physical activity and earning cans. In addition, the feedback regarding food earned may be used by participants to help set realistic goals, and evaluate and revise goals that are either too challenging or not sufficiently challenging.
The prosocial behavior component may also involve less-studied concepts within Social Cognitive Theory, including outcome expectations and outcome expectancies, or beliefs (expectations), and values (expectancies) used in evaluation of a given outcome [39,40]. Outcome expectations and expectancies are in large part a function of the capacity for symbolization and foresight. Thus, providing information which individuals may use to form additional expectations and expectancies for physical activity, (such as knowing that physical activity will result in earning food for individuals in need), or to revise existing expectations may influence physical activity by allowing participants to symbolize physical activity in a manner that may be consistent with other valued outcomes (such as aiding others). Another less-studied concept within Social Cognitive Theory that may be relevant to the PBPA intervention is moral dis (engagement) [41], or moral justification for a given behavior. It may be plausible that providing individuals with the opportunity to engage in behaviors that are in accord with their personal beliefs and in concert with physical activity may have a beneficial effect upon physical activity. Thus, pairing physical activity with a moral value, such as helping to feed families in need, may help motivate a person to engage in physical activity. In essence, the PBPA intervention is designed to implement several evidence-based strategies, while incorporating novel concepts and strategies to deliver physical activity programming.
2.7. Statistical considerations
2.7.1. Analysis plan
The primary objective of PACE is to assess the relative effect of the PBPA and HA interventions on energy expenditure (kcal/week) from ≥moderate-intensity physical activity as measured by the CHAMPS questionnaire. We hypothesize that the PBPA intervention will result in greater energy expenditure compared to the HA intervention. Analyses will be performed using the intention-to-treat principle. The primary outcome will be analyzed using repeated measures analysis of covariance (ANCOVA). The model testing this hypothesis will adjust for the stratification factor gender and the baseline CHAMPS score. Time (3 months, 6-months, and 12-months) will be included as a classification factor and a time by treatment interaction will be included in the model. An unstructured covariance matrix will be used to account for correlation between repeated measures; estimation will be performed using maximum likelihood. The primary hypothesis will be tested as a contrast representing the difference between interventions at 12 months using a two-sided 0.05 level of significance. Analyses of secondary outcomes will be analyzed similarly. Exploratory analyses will also be done in which age, race/ethnicity, and other covariates are included, along with their interactions with intervention.
Although we will attempt to minimize attrition, we expect that there will be missing measurements at the 12-month assessments due to missed visits or study dropout. The analytic method described above assumes the data will be missing at random. We will also employ several methods of imputation and assess the effects of our assumptions on the results.
2.7.2. Power/sample size
Our sample size of 150 participants per group was selected to provide adequate power for detecting a group difference in physical activity as quantified by the CHAMPS questionnaire. Stewart et al. [5], who assessed the effect of a cognitive-behavioral intervention on physical activity at 6 months in older adults, found that the standard deviation for the CHAMPS score was approximately 1500. Further, they found that the correlation between the baseline and 6-month scores was around 0.65. Our primary comparison of interest will occur at one year, so we conservatively anticipate a smaller correlation of 0.36, so the adjusted (for baseline CHAMPS) standard deviation of the CHAMPS score at one year will be approximately . Ignoring the extra information provided by the earlier repeated measures and assuming a 10% drop-out over one year, a sample size of 150 participants provides 80% power for detecting a 480 cal * wk−1 difference between groups with 80% power at the 5% two-sided level of significance. This is close to the difference reported by Stewart et al. [5]. If the baseline/one year correlation is 0.6, then we would be able to detect a difference of 411 cal * wk−1 with 80% power. We will also assess the effect of the intervention on post-randomization physical activity averaged over the 3-, 6-, and 12-month times. Assuming a correlation of 0.4 between all measurements (i.e., compound symmetry assumption) then we would be able to detect a difference of 321 cal * wk−1 between the two groups with 80% power in the average post-randomization CHAMPS.
3. Discussion
The PACE study is a two-arm randomized controlled trial that is designed to compare the efficacy of a “healthy aging” control condition with that of a theory-based physical activity intervention that incorporates prosocial behavior upon the primary outcome of physical activity at 12 months postrandomization. Long-term physical activity incorporating FITT and SAID Principle concepts is beneficial for older adults, and cognitive-behavioral interventions based upon Social Cognitive Theory can enhance independent physical activity among older adults [42]. However, there yet may be additional, unexplored motivating factors that can facilitate physical activity. To our knowledge, the PACE study represents the first attempt to test the efficacy of an innovative, cognitive-behavioral intervention that incorporates prosocial behavior as a motivational factor to enhance long-term, independent physical activity among older adults.
As noted earlier, volunteerism has been associated with positive health outcomes. Harris and Thoresen [11], studying 7527 older adults in the Longitudinal Study of Aging, found that in adjusted Cox proportional hazards models, frequent volunteers demonstrated significantly lower mortality compared to non-volunteers. Morrow-Howell et al. [12], studying three “waves” of participants in the Americans' Changing Lives Study aged 60 years or older, found that increases in hours of volunteering were associated with higher levels of well-being, independent of race or gender. Similarly, Musick and Wilson [13], analyzing data from the Americans' Changing Lives Study, found that volunteering was associated with lower (i.e. more favorable) scores on the 11-item version of the Center for Epidemiologic Studies Depression (CES-D) scale. Other researchers have found that volunteering is associated with increased life satisfaction [14] and quality of life [15]. Tan et al. [18], in adjusted analyses of 113 volunteers who were randomized into either the Baltimore Experience Corps condition or a waiting list control condition, found that although Experience Corps volunteers reported increased physical activity at 8 months post-randomization compared to those in the control group, the difference was not significant (p = 0.49). However, in subgroup analyses of participants not meeting Healthy People 2010 goals for physical activity, Experience Corps participants reported significantly higher physical activity at 8 months compared to control participants (p = 0.03). The authors stated that “These results provide additional evidence that a health promotion intervention that is embedded in an intergenerational volunteer program has the potential to increase physical activity”.
In the PACE study, the PBPA intervention incorporates prosocial behavior and volunteerism into several of the self-regulatory concepts within Social Cognitive Theory, including self-monitoring to enhance self-awareness, goal setting, and self-efficacy. In addition, participants engage in collaborative problem-solving with each other and the interventionists to prevent or address barriers to physical activity. The resources of the William G. White, Jr. Family YMCA are also available to PBPA participants. Also, although HA participants do not receive extensive physical activity instruction during the study, all HA participants will receive a 12-month membership to the “Y” and an Omron HJ-112 pedometer upon completion of the study. In addition, HA participants are referred to the Older Adults program at the YMCA after completion of the study.
The “currency” of prosocial behavior in this study is packaged food, which was selected because it may address an issue that may have widespread notoriety and appeal (e.g. combating hunger). Through examining associations and partnerships to combat hunger, the Principal Investigator (author C.G.F.) learned of an existing relationship between Lowes Foods® and the Second Harvest Food Bank through the “Friends Feeding Friends” campaign, and found that Lowes Foods® is a subsidiary of a food distributorship company. Also, it was discovered that several executives of Lowes Foods® were members of boards at Second Harvest Food Bank. Thus, it was deemed that Lowes Foods had the resources to provide the currency for the intervention. The Community Nutritionist of Lowes Foods® was approached initially with the study idea to gauge the interest of Lowes Foods®. The Nutritionist felt that this project fits well with the mission of Lowes Foods, and signed a letter of support which was included in the grant proposal. After the grant was funded, a meeting was held with the study team, the Community Nutritionist, and the Executive Assistant to the President, during which the study team was informed that it could develop the intervention as desired, without limits placed on the amount of food that would donated.
Although the current study focuses on food as the currency for prosocial behavior, other interventions involving prosocial behavior may be developed to meet the goals and resources of specific communities. For example, in other communities and settings, other currencies may be more salient. Among clinical populations, such as colorectal cancer survivors, developing a currency that may benefit colorectal cancer research or resources may be more resonant with participants. Also, partnerships may be made with different organizations which may have other existing currencies. For instance, the Striiv® (sic) company has recently developed the “smart” pedometer, which has a “walkathon” feature, in which the company and other partners such as the GlobalGiving Foundation donate water, vaccinations, and rainforest conservation in developing countries based upon pedometer steps after upload of data through a personal computer.
However, there are potential limitations to the PACE study which relate primarily to the generalizability of the study. The results of this study are not generalizable to the entire US population, but are limited to sedentary or underactive older adults who live in or near an urban area in the Southeastern United States. The results may be less generalizable to persons who live in rural areas that may not have YMCAs or fitness centers, or infrastructure such as sidewalks to facilitate physical activity. Also, we anticipate a sample which is primarily composed of women, which will limit generalizability to men. It should be noted that financial issues associated with “Y” membership is not a limitation, as many YMCAs offer partial or full scholarships to cover the cost of membership based on a member's household income. Our participant manuals are developed for an audience with a 7th grade reading level of higher; thus these interventions will not be generalizable for adults with very low literacy.
Furthermore, there are limitations associated with the prosocial behavior and volunteerism component of this study. The prosocial component relies heavily on a partnership with Lowes Foods®, a long-standing grocery chain of more than 100 stores in three states. However, this component may be less generalizable in geographic areas where there is limited opportunity or interest among potential partners to provide the “currency” for a prosocial intervention. This intervention may not appeal to individuals who are not motivated by prosocial behavior to engage in physical activity. Indeed, it will be informative to determine whether there is a positive association between scores on the internally-developed Prosocial Behavior and Exercise Survey and physical activity among PBPA participants. If physical activity levels are inversely associated with scores on the Prosocial Behavior and Exercise Survey, it would suggest that the form of prosocial behavior offered is not favorably associated with physical activity. However, increases in physical activity levels and Prosocial Behavior and Exercise Survey scores after the introduction of the enhanced scale in Session 10 would support the plausibility of prosocial behavior as a motivating factor.
Even if prosocial behavior may be a motivating factor for physical activity, the “currency” we are using for prosocial behavior (e.g. earning cans of food for donation) may not be as salient to participants as other forms of currency, such as earning monetary funds to donate to the charity of one's choice, or earning funds to donate toward curing or treating specific conditions such as heart disease or cancer. Additionally, even if prosocial behavior is a motivating factor, and the currency is salient, the scale may not be sufficiently challenging for participants who will accrue >205 minutes of weekly physical activity, or >70,000 weekly steps. Finally, it is unknown whether the influence of the prosocial behavior incentive may fluctuate over time, as participants continue physical activity. Some participants may continue to perceive it as a stable motivating factor, while for others, it may be viewed as a temporary “novelty” that loses its appeal over time. For others, it may be an incentive that periodically will be salient, while during other periods, other motivating factors may become more prominent. Some participants may prefer to first focus on becoming competent in engaging in physical activity safely before turning to prosocial behavior as a motivating factor. Also, the prosocial intervention may be positively influenced by history threats, e.g. public awareness campaigns regarding childhood hunger.
In summary, the PACE study addresses a significant issue, which is physical inactivity and underactivity among older adults, by testing an innovative strategy to promote physical activity in this population. If the PBPA intervention is shown to be more efficacious in promoting physical activity compared to a healthy aging control, it will add to the body of knowledge by suggesting that prosocial behavior may be successfully implemented within a cognitive-behavioral intervention to facilitate physical activity. An informative next step would be to test the PBPA intervention compared to a standard, structured physical activity intervention.
Acknowledgments
The authors would like to acknowledge the support of several individuals for their support during the development and implementation of the PACE study. First, the authors thank Drs. Sally Shumaker, Lynne Wagenknecht, Doug Easterling and Stephen Kritchevsky for their ongoing encouragement to develop the prosocial behavior intervention. Also, the authors thank the following individuals of the William G. White, Jr, Family YMCA for their collaboration as partners: Mr. Darryl Head, Executive Director; Ms. Erin Kennedy, Senior Program Director of Membership; Mr. Luke Harris, Wellness Director; and Ms. Melissa Warren, Active Older Adults Coordinator. We also thank Lowes Foods® and Ms. Debbie Williams, Executive Assistant to the President, and Ms. Cindy Silver, the community nutritionist at Lowes Foods®, for their collaboration as community partners. We also thank Ms. Debbie Clark, Volunteer and Coordinator for the Second Harvest Food Bank of Northwest North Carolina. We also thank Drs. Josephine Boyington and Bill Riley, and Ms. Tawana McKeither of the National Institutes of Health.
Funding
This study is funded through the National Heart, Lung and Blood Institute (1R01HL109429-01, 5R01HL109429-02). This work also is partially supported by the Wake Forest University Claude D. Pepper Older Adults Independence Center (P30-AG21332).
Footnotes
Support for the present study is provided by NIH/NHLBI grant #R01HL109429.
The ClinicalTrials.gov identifier for this study is NCT01528761.
References
- 1.Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ, et al. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41:1510–1530. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- 2.Dishman RK. Overview. In: Dishman RK, editor. Exercise adherence: its impact on public health. Champaign, IL: Human Kinetics Press; 1998. [Google Scholar]
- 3.Census Bureau Population Division. Propulation Projections Branch. U.S. Interim Projections by Age, Sex, Race, and Hispanic Origin - Table 2. 2004 [Google Scholar]
- 4.Rejeski WJ, Foy CG, Brawley LR, Brubaker PH, Focht BC, Norris JL, et al. Older adults in cardiac rehabilitation: a new strategy for enhancing physical function. Med Sci Sports Exerc. 2002;34:1705–1713. doi: 10.1097/00005768-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33:1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Bandura A. Social foundations of thought and action: a social cognitive theory. 1986 [Google Scholar]
- 7.Eisenberg N, Miller PA. The relation of empathy to prosocial and related behaviors. Psychol Bull. 1987;101:91–119. [PubMed] [Google Scholar]
- 8.American Heart Association. American Heart Association Heart Walk. 2012 [Google Scholar]
- 9.Penner LA, Dovidio JF, Piliavin JA. Prosocial behavior: multilevel perspectives. Annu Rev Psychol. 2005;56:365–392. doi: 10.1146/annurev.psych.56.091103.070141. [DOI] [PubMed] [Google Scholar]
- 10.Duncan SC, Duncan TE, Strycker LA, Chaumeton NR. Relations between youth antisocial and prosocial activities. J Behav Med. 2002;25:425–428. doi: 10.1023/a:1020466906928. [DOI] [PubMed] [Google Scholar]
- 11.Harris AH, Thoresen CE. Volunteering is associated with delayedmortality in older people: analysis of the longitudinal study of aging. J Health Psychol. 2005;10:739–752. doi: 10.1177/1359105305057310. [DOI] [PubMed] [Google Scholar]
- 12.Morrow-Howell N, Hinterlong J, Rozario PA, Tang F. Effects of volunteering on the well-being of older adults. J Gerontol B Psychol Sci Soc Sci. 2003;58:S137–S145. doi: 10.1093/geronb/58.3.s137. [DOI] [PubMed] [Google Scholar]
- 13.Musick MA, Wilson J. Volunteering and depression: the role of psychological and social resources in different age groups. Soc Sci Med. 2003;56:259–269. doi: 10.1016/s0277-9536(02)00025-4. [DOI] [PubMed] [Google Scholar]
- 14.Van Willigen M. Differential benefits of volunteering across the life course. J Gerontol Soc Sci. 2000;55B:S308–S318. doi: 10.1093/geronb/55.5.s308. [DOI] [PubMed] [Google Scholar]
- 15.Cattan M, Hogg E, Hardill I. Improving quality of life in ageing populations: what can volunteering do? Maturitas. 2011;70:328–332. doi: 10.1016/j.maturitas.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 16.Glass TA, Freedman M, Carlson M, Hill J, Frick KD, Ialongo N, et al. Experience Corps: design of an intergenerational program to boost social capital and promote the health of an aging society. J Urban Health. V81:94–105. doi: 10.1093/jurban/jth096. 3-13-2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martinez IL, Frick K, Glass TA, Carlson M, Tanner E, Ricks M, et al. Engaging older adults in high impact volunteering that enhances health: recruitment and retention in the Experience Corps. J Urban Health. 2006;V83:941–953. doi: 10.1007/s11524-006-9058-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan EJ, Xue QL, Li T, Carlson MC, Fried LP. Volunteering: a physical activity intervention for older adults. J Urban Health. 2006;V83:954–969. doi: 10.1007/s11524-006-9060-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marsh AP, Vance RM, Frederick TL, Hesselmann SA, Rejeski WJ. Objective assessment of activity in older adults at risk formobility disability. Med Sci Sports Exerc. 2007;39:1020–1026. doi: 10.1249/mss.0b013e3180423ac3. [DOI] [PubMed] [Google Scholar]
- 20.Research TRCfPO. The Social Capital Benchmark Survey (Data Codebook) 2002 [Google Scholar]
- 21.Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 22.Wechsler H. Manual for the Wechsler Adult Intelligence Scale Revised. 1981 [Google Scholar]
- 23.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 24.Rejeski WJ, Ip EH, Marsh AP, Miller ME, Farmer DF. Measuring disability in older adults: the International Classification System of Functioning, Disability and Health (ICF) framework. Geriatr Gerontol Int. 2008;8:48–54. doi: 10.1111/j.1447-0594.2008.00446.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The veterans RAND 12 item health survey: what it is and how it is used. 2012 [Google Scholar]
- 26.Selim AJ, Rogers W, Fleishman JA, Qian SX, Fincke BG, Rothendler JA, et al. Updated U.S. population standard for the Veterans RAND 12-item Health Survey (VR-12) Qual Life Res. 2009;18:43–52. doi: 10.1007/s11136-008-9418-2. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE, Kosinski M, Keller SK. SF-36 Physical and mental health summary scales: a user's manual. Boston: The Health Institute, New England Medical Center; 1994. [Google Scholar]
- 28.Cohen S, Karmack T, Mermelstein R. A global measure of perceived stress. J Heatlh Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 29.Rejeski WJ, Reboussin BA, Dunn AL, King AC, Sallis JF. A modified exercise-induced feeling inventory for chronic training and baseline profiles of participants in the Activity Counseling Trial. J Health Psychol. 1999;4:97–108. doi: 10.1177/135910539900400107. [DOI] [PubMed] [Google Scholar]
- 30.Garcia AW, King AC. Predicting long-termadherence to aerobic exercise: a comparison of two models. J Sport Exerc Psychol. 1991;13:394–410. [Google Scholar]
- 31.Resnick B, Luisi D, Vogel A, Junaleepa P. Reliability and validity of the self-efficacy for exercise and outcome expectations for exercise scales with minority older adults. J Nurs Manag. 2004;12:235–247. doi: 10.1891/jnum.12.3.235. [DOI] [PubMed] [Google Scholar]
- 32.Cutrona CE, Russell D. The provisions of social relationships and adaptation to stress. In: Jones WH, Perlman D, editors. Advances in personal relationships. Vol. 1. Greenwich, CT: JAI Press; 1987. pp. 37–67. [Google Scholar]
- 33.Markland D, Hardy L. The exercise motivations inventory: preliminary development and validity of a measure of individuals' reasons for participation in regular physical exercise. Pers Individ Differ. 1993;15:289–296. [Google Scholar]
- 34.The Look AHEAD Research Group. The development and description of the comparison group in the Look AHEAD trial. Clinical Trials. 8:320–329. doi: 10.1177/1740774511405858. 6-1-2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1435–1445. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 36.Tudor-Locke C, Craig C, Aoyagi Y, Bell R, Croteau K, De Bourdeaudhuij I, et al. How many steps/day are enough? For older adults and special populations. I. J Behav Nutr Phys Act. 2011;8:80–98. doi: 10.1186/1479-5868-8-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tudor-Locke CE, Myers AM. Methodological considerations for researchers and practitioners using pedometers to measure physical (ambulatory) activity. Res Q Exerc Sport. 2001;72:1–12. doi: 10.1080/02701367.2001.10608926. [DOI] [PubMed] [Google Scholar]
- 38.Bandura A. Social cognitive theory: an agentic perspective. Asian J Soc Psychol. 1999;2:21–41. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 39.Wilcox S, Castro CM, King AC. Outcome expectations and physical activity participation in two samples of older women. J Health Psychol. 11:65–77. doi: 10.1177/1359105306058850. 1-1-2006. [DOI] [PubMed] [Google Scholar]
- 40.Williams DM, Anderson ES, Winett RA. A review of the outcome expectancy construct in physical activity research. Ann Behav Med. 2005;29:70–79. doi: 10.1207/s15324796abm2901_10. [DOI] [PubMed] [Google Scholar]
- 41.Bandura A, Barbaranelli C, Caprara GV, Pastorelli C. Mechanisms of moral disengagement in the exercise of moral agency. J Pers Soc Psychol. 1996;71:364–374. [Google Scholar]
- 42.Brawley LR, Rejeski WJ, Lutes L. A group-mediated cognitive-behavioral intervention for increasing adherence to physical activity in older adults. J Appl Behav Res. 2000;5:47–55. [Google Scholar]