Abstract
Background
Sudden cardiac death (SCD) is a leading cause of death in the US, but the relative public health burden is unknown. We estimated the burden of premature death from SCD and compared it to other diseases.
Methods and Results
Analyses were based on the following data sources (using most recent sources that provided appropriately stratified data): 1) Leading causes of death among men and women from 2009 US death certificate reporting; 2) Individual cancer mortality rates from 2008 death certificate reporting from the CDC’s National Program of Cancer Registries; 3) County, state and national population data for 2009 from the US Census Bureau; 4) SCD rates from the Oregon Sudden Unexpected Death Study (SUDS) population-based surveillance study of SCD between 2002 and 2004. Cases were identified from multiple sources in a prospectively designed surveillance program. Incidence, counts and years of potential life lost (YPLL) for SCD and other major diseases were compared. The age-adjusted national incidence of SCD was 60 per 100,000 population (95% confidence interval = 54 – 66 per 100,000). The burden of premature death for men (2.04 million YPLL; 95% uncertainty interval 1.86 – 2.23 million) and women (1.29 million YPLL; 95% uncertainty interval 1.13 – 1.45 million) was greater for SCD than all individual cancers and most other leading causes of death.
Conclusions
The societal burden of SCD is high relative to other major causes of death. Improved epidemiologic surveillance of SCD and other forms of cardiovascular disease is necessary to evaluate and improve prevention and treatment.
Keywords: sudden cardiac death, epidemiology, population studies, public policy, causes of death
Introduction
Sudden cardiac death (SCD) is characterized by sudden circulatory collapse caused by a cardiac arrhythmia. A majority of cases occur in the setting of chronic or acute ischemic heart disease.1 There is very little information regarding the public health burden from SCD around the world and it was not reported as part of the Global Burden of Disease Study.2 Estimates of annual incidence of SCD in the US range between 180,000 and 450,000,3 corresponding to between 7% and 18% of all deaths in the US. The high degree of variability in these estimates is due to limitations in data regarding mode of cardiovascular death. Death certificate reporting provides annual national estimates for many diseases but has proven inaccurate for SCD.4–6 Cohort studies and randomized trials have produced important insights into heart disease. However, inferences regarding incidence and burden are limited because few studies are designed to prospectively identify SCD and it often takes many years to accrue sufficient numbers of cases for analysis. Detailed knowledge of SCD is critical for targeting SCD-specific prevention and treatment at the population level (designing and evaluating emergency medical response systems and automatic external defibrillator deployments) and patient level (better utilizing implantable cardioverter-defibrillators and developing new methods targeting arrhythmic death prevention).
We sought to provide estimates of national SCD incidence and burden of premature death based on data from the Oregon Sudden Unexpected Death Study (SUDS) in Portland, Oregon, and compare with other causes of death nationwide. Oregon SUDS is a multi-source, population-based study of SCD among all ages in a community of 680,000 people. We estimated the burden of premature death using a well-accepted metric, years of potential life lost (YPLL). YPLL measures the total lost years of life for all individuals with a disease compared to individuals who live to a normal life expectancy.
Methods
Data sources
Four primary data sources were used for this analysis and were selected from the most recent complete datasets available: 1) SCD rates from the Oregon SUDS population-based surveillance between 2002 and 2004. 2) Leading causes of death from 2009 death certificate reporting stratified by age group and gender, as reported by Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics National Vital Statistics System.7, 8 Data from 2009 were used because this was the most recent year in which both five-year age strata and information about causes of death in infants were available. 3) Individual (site-specific) cancer mortality rates from 2008 death certificate reporting stratified by age group and gender, as reported by the CDC’s National Program of Cancer Registries.9 Data from 2008 were used because this was the most recent year that reported 5-year age strata. 4) County, state and national population data for 2009, as reported by the US Census Bureau.10
Surveillance and adjudication of SCD
Annual cases of SCD were determined from three years of prospective, multiple-source surveillance in Multnomah County, Oregon. Cases were identified as previously described based on prospective surveillance methods using original information from the local emergency medical response system (EMS), medical examiner and all area hospitals.4, 11 Available records were gathered from clinics, hospitals, medical examiner reports and EMS reports. Three physicians reviewed all records in order to adjudicate cause and mode of death. A two-step approach is used for SCD adjudication. Based on arrest records that include circumstances, review of tracings captured by EMS and any known medical history, the patient is preliminarily categorized as SCD or non-SCD. After further record review including pre-arrest medical records, post-resuscitation medical records and autopsy when available, the SCD cases can be re-categorized as non-SCD if non-cardiac causes of arrest are identified. At either stage, the most definitive data are used to determine death in the case of any conflicting information (for example, an autopsy would supersede most information from post-arrest medical diagnostics and recordings of rhythm/vitals would supersede bystander observations of unresponsiveness).
Definitions
The following definitions were used. “Sudden cardiac death” (SCD) referred to unexpected death without an obvious non-cardiac cause occurring within 1 hour of symptom onset (witnessed), or within 24 hours of last being observed in normal health (unwitnessed).12 Cases with likely non-cardiac causes of death were excluded (for instance diagnosed pulmonary embolism, known metastatic cancer or drug overdose). Deaths were verified by searching National Death Index records, published obituaries, and State of Oregon death certificates. “Sudden cardiac arrest” (SCA) included all cases of SCD as well as patients surviving to hospital discharge. “Burden of premature death” was used as a descriptor of magnitude of YPLL (see description below). “Overall cancer” referred to all forms of cancer, independent of site or histology. “Overall heart disease” referred to any form of heart disease, including SCD. “Leading causes of death” referred to those tracked and reported by the CDC’s National Center for Health Statistics National Vital Statistics System. “Individual cancer” was used to refer to a cancer originating from a specific anatomic site. Examples include breast cancer and prostate cancer. “Base case” estimates referred to national extrapolation of Multnomah County, Oregon rates of SCD and SCA using only age and gender adjustment.
Multnomah County SCD rates
Data from three years of active surveillance among residents of all ages in Multnomah County were used. Each adjudicated SCD case was assigned to a gender and age category. Eighteen age categories were used: 17 five-year categories (“0–5 years” to “80–85 years”) and 1 category of “≥85 years”. The total number of deaths over 3 years for each age-gender category was divided by 3, yielding numerators for each age-gender category. US Census Bureau data for the Multnomah County population at the middle time-point of the study period for each age-gender category constituted the denominators for the categories and allowed calculation of the population incidence of SCD for each age-gender category. These category incidences formed the basis for subsequent calculation of YPLL.
National SCD estimates
National incidences of SCD were estimated for women, men and overall using two methods. The first adjustment method extrapolated the gender- and age-stratified rates from Oregon SUDS to the nation overall, using conventional age standardization techniques with the 2009 US population as the reference. National counts of SCD were determined by multiplying the estimated incidences by the national population. Estimates of SCA (combination of SCD and non-lethal arrests meeting criteria above) were calculated in the same manner as SCD and reported in table 1 for comparison.
Table 1.
Comparison of national sudden death estimates using different definitions and analysis methods*
| Estimation method | Incidence in females |
Incidence in males |
Total incidence | Total events |
|---|---|---|---|---|
| Sudden cardiac death | ||||
| Base case | 45 (37–53) | 76 (66–87) | 60 (54–66) | 183,001 (164,218–203,205) |
| Cardiac-death-risk adjustment | 52 | 88 | 69 | 212,910 |
| Sudden cardiac arrest | ||||
| Base case | 49 (42–58) | 83 (73–95) | 66 (59–73) | 201,286 (181,417–222,594) |
| Cardiac-death-risk adjustment | 57 | 96 | 76 | 234,085 |
95% uncertainty intervals are shown in parentheses and were calculated using the gamma distribution method. Incidence rates are expressed per 100,000 national population and were extrapolated from Multnomah County data (with and without adjustment for state-specific differences in overall cardiac-death risk, as described in the methods section). Sudden cardiac death refers to patients who died within one hour of symptom onset if witnessed or within 24 hours of last being seen alive in normal state if unwitnessed. Sudden cardiac arrest refers to all patients with sudden cardiac death as well as those who survived until hospital discharge after resuscitation for a primary arrhythmia.
A second national extrapolation technique, cardiac-death-risk adjustment, was used to adjust for potential regional differences in SCD rates beyond that explained by differences in population age and gender characteristics. For this extrapolation technique, we assumed that the ratio of SCD rates between each state and Multnomah County varied to the same degree as the ratio of overall heart disease mortality between each state and Multnomah County. The Multnomah County population-based SCD rate for each age-gender category was multiplied by the population of the corresponding age-gender category in each of the 50 states plus District of Columbia to yield an estimated state SCD event count. Each state count (stratified by gender) was multiplied by the ratio of overall heart disease mortality between that state and Multnomah County,8, 13 resulting in an adjusted SCD count. The sum of the adjusted counts yielded the adjusted national totals for SCD. The totals were divided by the national population to create an estimate of national SCD rates adjusted for differences by age, gender and state. Implicit to this technique were two assumptions: 1) regional differences in SCD rates mirror the differences in overall cardiac death risk, and 2) differences in cardiac death risk between regions are constant across gender and age categories.
National rates of death from non-SCD causes
Deaths counts from common diseases were identified from national death certificate summary reports that were stratified by the same age-gender categories as the Multnomah County data. Total counts for each gender were divided by the national population of that gender during the year of measurement (2008 for cancers and 2009 for all other causes of death) and multiplied by 100,000 to yield a national population-based rate. Counts within each age-gender category were used for the YPLL comparisons.
Years of potential life lost
YPLL were calculated for SCD and other causes of death by multiplying the estimated number of nationwide deaths in each age-gender category by the 2009 US population life expectancy at the mid-point of that age category. For each cause of death, YPLL were totaled for all age categories. An additional analysis for YPLL from SCD was performed using the cardiac-death-risk adjustment described above.
Statistical analysis
Calculations were performed using Microsoft Excel version 14.0 and SAS version 9.4. The statistical level of uncertainty surrounding national SCD incidence rates was calculated using 95% confidence intervals (CI) according to the gamma distribution method14 as suggested for age-adjusted rates15 as follows: , where is R age adjusted rates, m is the number of age groups, di is number of deaths in age group i, Pi is the population in age group i, and si is the proportion of the standard population in age group i. Variance is given by . Confidence intervals are: and , where ν is the variance, wM is the maximum likelihood of the weights si/Pi, 1−∝ is the confidence interval desired and is the inverse of the X2 distribution with x degrees of freedom. 95% uncertainty intervals for YPLL from SCD were calculated based on the 2.5th and 97.5th percentile distributions from Monte Carlo simulations using 10,000-sample draws with binomial distributions of the Multnomah County SCD rates.
According to convention for national demography reporting (as employed by the US Centers for Disease Control and Prevention and others), counts, rates and YPLL for nationally measured diseases were reported and compared without use of inferential statistical testing because they represent directly measured national data rather than samples of a population.
Informed consent
This study was approved by the institutional review boards of all area hospitals. All living patients gave informed consent for participation.
Results
Population characteristics
The population of Multnomah County Oregon in 2003 was 679,348 and grew to 727,721 by 2009. County residents were 83% white and 6% African American, with 17% of all races reporting Hispanic ethnicity. The population of the United States in 2003 was 290,107,933 and grew to 306,771,529 by 2009. US residents were 80% white and 13% African American, with 14% reporting Hispanic ethnicity.
National SCD estimates (Table 1)
The national age- and gender-adjusted rate for SCD in the base case analysis was 60 per 100,000 population (95% CI = 54 to 66 per 100,000). Rates among women were 45 per 100,000 (95% CI = 37 to 53 per 100,000) and among men were 76 per 100,000 (95% CI = 66 to 87 per 100,000). There were an estimated 183,001 SCD cases annually (95% uncertainty interval = 164,218 to 203,205) for both genders. Adding cardiac-death-risk adjustment (adjusting for age, gender and state variability in heart disease mortality) resulted in an estimated national SCD rate point estimate of 69 per 100,000 and a national total of 212,910 cases.
Comparisons of national rates of SCD to other leading causes of death
Among women, overall heart disease and cancer were the leading causes of death with rates of 188 per 100,000 and 174 per 100,000 respectively (Table 2). Rates of cerebrovascular disease (49 per 100,000), chronic lower respiratory disease (46 per 100,000), lung cancer (45 per 100,000) and SCD (45 per 100,000; 95% CI 37 to 53 per 100,000) were all in a similar range. Among men, heart disease and cancer death rates were 205 per 100,000 and 197 per 100,000 respectively (Table 3). Deaths from SCD (76 per 100,000; 95% CI 66 to 87 per 100,000) exceeded all other individual causes of death including lung cancer, accident, chronic lower respiratory disease, cerebrovascular disease, diabetes mellitus, prostate cancer and colorectal cancer.
Table 2.
Female mortality for sudden cardiac death, common diseases and individual cancers*
| Disease | Number of deaths | Death rate |
|---|---|---|
| Overall heart disease | 293,187 | 188 |
| Sudden cardiac death | 69,524 (58,152 – 82,294) | 45 (37 – 53) |
| Overall cancer | 270,865 | 174 |
| Lung cancer | 70,040 | 45 |
| Breast cancer | 40,576 | 26 |
| Colorectal cancer | 25,918 | 17 |
| Cerebrovascular disease | 76,769 | 49 |
| Chronic lower respiratory disease | 72,234 | 46 |
| Alzheimer’s disease | 54,916 | 35 |
| Accidents | 42,999 | 28 |
Sudden cardiac death was estimated using base case rates from the Oregon Sudden Unexpected Death Study. All other estimates were measured by death certificate based data from US Centers for Disease Control and Prevention. (Counts may vary from CDC totals by < 0.5% due to differences in cause of death categorization in infants and suppression of cell counts < 16.) Death rates are expressed per 100,000 national female population. 95% uncertainty intervals are listed in parentheses.
Table 3.
Male mortality for sudden cardiac death, common diseases and individual cancers*
| Disease | Number of deaths | Death rate |
|---|---|---|
| Overall heart disease | 308,619 | 205 |
| Sudden cardiac death | 114,948 (99,722 – 131,505) | 76 (66 – 87) |
| Overall cancer | 296,763 | 197 |
| Lung cancer | 88,527 | 59 |
| Prostate cancer | 28,464 | 19 |
| Colorectal cancer | 26,923 | 18 |
| Accidents | 75,022 | 50 |
| Chronic lower respiratory disease | 65,119 | 43 |
| Cerebrovascular disease | 52,073 | 35 |
| Diabetes mellitus | 35,054 | 23 |
Sudden cardiac death was estimated using base case rates from the Oregon Sudden Unexpected Death Study. All other estimates were measured by death certificate based data from US Centers for Disease Control and Prevention. (Counts may vary from CDC totals by < 0.5% due to differences in cause of death categorization in infants and suppression of cell counts < 16.) Death rates are expressed per 100,000 national male population. 95% uncertainty intervals are listed in parentheses.
Comparisons of burden of premature death from SCD to other leading causes of death
Total YPLL from SCD for men (2.04 million; 95% uncertainty interval 1.86 – 2.23 million) was greater than chronic lower respiratory disease (0.72 million), cerebrovascular disease (0.62 million) and diabetes mellitus (0.53 million). SCD accounted for 50% of all YPLL due to overall heart disease (4.11 million) and trailed only overall cancer (4.32 million) and accidental death (2.38 million) among non-cardiovascular causes of death. Use of the cardiac-death-risk adjustment method increased the YPLL from SCD to 2.36 million.
Among women, total YPLL for SCD (1.29 million; 95% uncertainty interval 1.13 – 1.45 million) was greater chronic lower respiratory disease (0.87 million), cerebrovascular disease (0.78 million) and Alzheimer’s disease (0.35 million). It was of borderline greater magnitude than accidental death (1.17 million). SCD accounted for 41% of YPLL due to overall heart disease (3.11 million) and was exceeded in magnitude only by overall cancer (4.47 million) among non-cardiovascular causes of death. Use of the cardiac-death-risk adjustment method increased the estimated YPLL from SCD to 1.49 million.
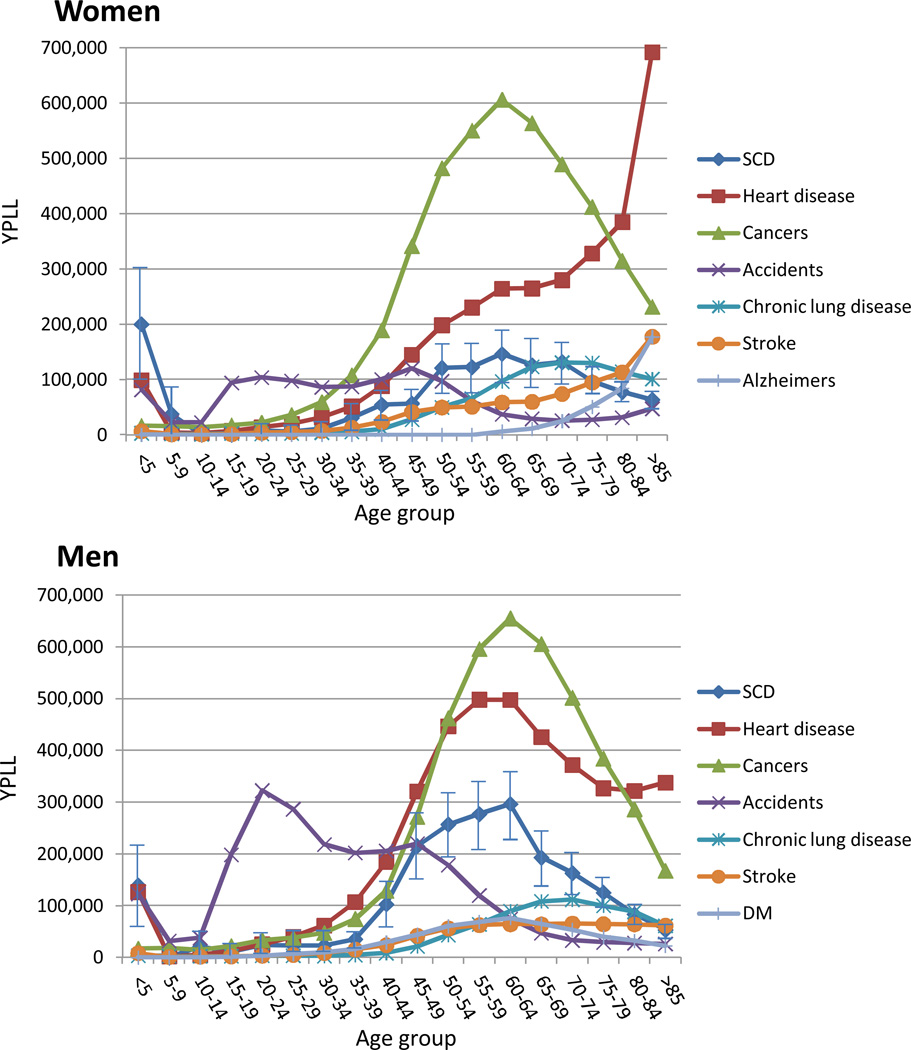
For men, the burden of YPLL for SCD and most major diseases began rising between ages 35 and 45, while that of accidental death was most pronounced between ages 10 and 60 years (Figure 1). For women, there was a similar early peak of YPLL from accidental death, though of smaller magnitude. Heart disease and SCD premature death burdens began rising more slowly with lower peaks relative to overall cancer. Unlike heart disease in men and unlike cancer in both genders, YPLL from heart disease in women continued to climb in old age.
Figure 1.
Years of potential life lost among women and men from sudden cardiac arrest and other leading causes of death
DM diabetes mellitus; SCD – sudden cardiac death; YPLL – years of potential life lost. 95% uncertainty intervals in each age group shown for SCD
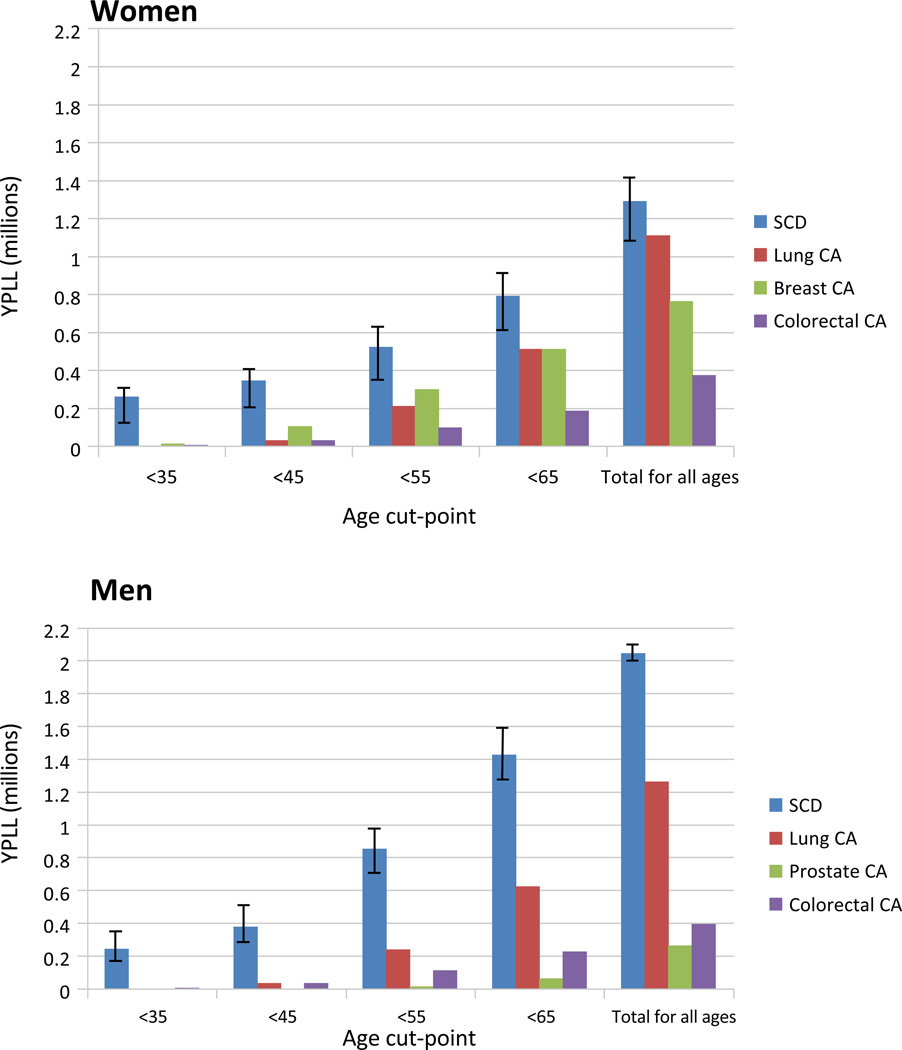
Sudden cardiac death was responsible for a greater burden of premature death than all individual cancers for each gender (Figure 2). Among men less than 65 years old, YPLL from SCD was more than double any individual cancer.
Figure 2.
Years of potential life lost among women and men from sudden cardiac arrest versus top three individual cancers by different age cut-points.
CA – cancer; SCD – sudden cardiac death; YPLL – years of potential life lost. 95% uncertainty intervals in each age cut-off shown for SCD
Discussion
This study demonstrates the large public health burden of SCD, which is responsible for 40% to 50% of YPLL from heart disease. The incidence and premature death burden from SCD exceeded that of any individual cancer for both men and women. Among women, SCD exceeded all non-cardiac causes of premature death except overall cancer. Among men, SCD exceeded all except overall cancer and accidents. The estimated annual national incidence of SCD using standard age and gender adjustment was 183,000 (95% uncertainty interval = 164,000 to 203,000). The point estimate for national SCD incidence after adding cardiac-death-risk adjustment increased to 213,000. This study not only adds to prior reports of SCD incidence,3 but also places the problem of SCD in broader societal perspective by comparing it to other causes of death. Because of lower population-based rates of SCD in Oregon, the actual national burden of premature death from SCD is likely even greater than we have reported in our base case estimate. Adjusting for regional differences in SCD rates resulted in a 15% higher burden of YPLL from SCD for both men and women.
To our knowledge, this is the first study to estimate national rates of SCD using prospective surveillance systems with rigorously adjudicated cause-of-death information on patients of all ages. This allows for the comparison of premature death between SCD and other causes. The societal burden of premature death is an important factor that should help to guide relative allocation of resources for studying, preventing and treating diseases. The high burden of SCD stands in contrast to the limited scientific knowledge regarding its incidence, etiology and risk factors.1, 3, 16 This may be a manifestation of the modest epidemiologic surveillance efforts dedicated to heart disease overall. Heart disease deaths are tracked nationally only by use of death certificates as part of the CDC’s National Vital Statistics System. This is of limited utility for detailed epidemiologic research, and it has been repeatedly shown to inaccurately reflect the mode of cardiovascular death when compared to detailed clinical review of cases.4–6 Incidence and recurrent event data for heart disease, reported annually in the American Heart Association’s Heart Disease and Stroke Statistics updates, are based on the Framingham Heart Study (FHS), Atherosclerosis Risk in Communities Study (ARIC) and Cardiovascular Health Study (CHS).17 These three studies represent an estimated total population of 1 million (less than 0.5% of the US population). Many of the national inferences of heart disease are derived from 10,333 patients in two cohorts of FHS. There are similarly few efforts worldwide to track SCD burden, and it is not reported as part of the Global Burden of Diseases Study.2
The US approach to cancer epidemiology serves as a contrast and potential model for cardiovascular epidemiology. The Surveillance, Epidemiology and End Result (SEER) registry, established in 1973 as part of the National Cancer Institute (NCI), collects detailed information about patient characteristics, tumor characteristics, clinical treatments and patient outcomes for cancer cases in 20 geographic areas.18 It encompasses 28% of the US population and the registry’s demographics are representative of the nation as a whole. The director of the Division of Cancer Prevention at the NCI has stated that “SEER is a mainstay of the National Cancer Program…rational leadership of NCI would not be possible without SEER.”19 The magnitude of SCD illustrated in the present study, as well as its inherent limitations (see below), both argue for an improved epidemiological surveillance system for cardiovascular death that is akin to SEER. With better knowledge of the nature of SCD, more effective investigation into mechanisms, prevention and treatment can be undertaken. For a disorder like SCD with myriad etiologic pathways, such research is particularly important.
Because no nationally representative epidemiologic studies of SCD currently exist, our estimates based on the Oregon SUDS study provide the most accurate available comparison of the burden of premature death from SCD relative to other diseases. The most important limitation is the use of a single metropolitan area. In lieu of a national cardiovascular epidemiologic registry system, a majority of inferences about incidence and trends of cardiovascular disease have been derived from cohorts much smaller than Multnomah County’s population.17 At this point Multnomah County is the only source of data possessing all of the requisite attributes for this analysis. In particular, cause- and mode-of-death adjudication must be robust to prevent inclusion of cardiac arrests that are not primarily arrhythmic (e.g. primary respiratory failure) or occur in the setting of a known terminal illness (e.g. metastatic cancer) from leading to an overestimation of SCD rates. For example, despite other strengths of the ROC Epistry-Cardiac Arrest study, it appears to have overestimated the rate of SCD in the Portland metropolitan area (60 per 100,000 in Oregon SUDS with detailed clinical mode-of-death adjudication; 71 per 100,000 in ROC Epistry-Cardiac Arrest).20 Another important limitation is that the death certificate data used for non-SCD death are prone to disease miscategorization (though likely to a lesser degree than death-certificate-based SCD data). Nonetheless, these data sources are preferred by CDC for nationwide comparisons and alternative sources are not available. Finally, YPLL estimates in the present study are generally less than those from the US portion of the Global Burden of Diseases Study.21 This is likely due to use of US-specific life expectancy estimates in the present study, whereas the Global Burden of Diseases Study used the lowest death rate across countries for each age group to estimate US life expectancies.
Conclusion
The societal burden of SCD as measured by YPLL is high relative to other major non-cardiac conditions. Creation of a nationwide surveillance system for cardiovascular disease has been recognized as a priority.22–23 As the present study illustrates, the high societal burden of SCD alone could justify such a project. In areas where research collaborations between cardiology and emergency medicine systems are feasible, a network of nationally representative community-based studies of SCD could be developed to measure rates and modes of cardiovascular death and track them over time. Such an effort would facilitate a better understanding of SCD etiologies and a more accurate and timely assessment of the effectiveness of SCD prevention and treatment efforts.
Supplementary Material
Acknowledgments
American Medical Response, Portland/Gresham fire departments and the Oregon State Medical Examiner’s office were essential to the success of this research.
Funding Sources: Funded by NHLBI grants R01 HL088416 and R01 HL105170 to Dr Chugh. Dr Chugh holds the Pauline and Harold Price Endowed Chair in Cardiac Electrophysiology at the Cedars-Sinai Heart Institute, Los Angeles, CA.
Footnotes
Conflict of Interest Disclosures: Dr. Stecker reports research grants from Biotronik and Boston Scientific. All other authors report no competing interests.
References
- 1.Chugh SS, Reinier K, Teodorescu C, Evanado A, Kehr E, Al Samara M, Mariani R, Gunson K, Jui J. Epidemiology of sudden cardiac death: Clinical and research implications. Prog Cardiovasc Dis. 2008;51:213–228. doi: 10.1016/j.pcad.2008.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global Burden of Disease Collaborators.. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions 1990–2010: A systematic analysis for the global burden of disease study 2010. Lancet. 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 3.Kong MH, Fonarow GC, Peterson ED, Curtis AB, Hernandez AF, Sanders GD, Thomas KL, Hayes DL, Al-Khatib SM. Systematic review of the incidence of sudden cardiac death in the united states. J Am Coll Cardiol. 2011;57:794–801. doi: 10.1016/j.jacc.2010.09.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chugh SS, Jui J, Gunson K, Stecker EC, John BT, Thompson B, Ilias N, Vickers C, Dogra V, Daya M, Kron J, Zheng ZJ, Mensah G, McAnulty J. Current burden of sudden cardiac death: Multiple source surveillance versus retrospective death certificate-based review in a large U.S. Community. J Am Coll Cardiol. 2004;44:1268–1275. doi: 10.1016/j.jacc.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 5.Every NR, Parsons L, Hlatky MA, McDonald KM, Thom D, Hallstrom AP, Martin JS, Weaver WD. Use and accuracy of state death certificates for classification of sudden cardiac deaths in high-risk populations. Am Heart J. 1997;134:1129–1132. doi: 10.1016/s0002-8703(97)70035-8. [DOI] [PubMed] [Google Scholar]
- 6.Iribarren C, Crow RS, Hannan PJ, Jacobs DR, Jr, Luepker RV. Validation of death certificate diagnosis of out-of-hospital sudden cardiac death. Am J Cardiol. 1998;82:50–53. doi: 10.1016/s0002-9149(98)00240-9. [DOI] [PubMed] [Google Scholar]
- 7.CDC - National Center for Health Statistics. [Accessed February 12, 2013]; http://www.cdc.gov/nchs/data/dvs/LCWK1_2009.pdf.
- 8.CDC - National Center for Health Statistics. [Accessed May 12, 2013]; http://www.cdc.gov/nchs/data/nvsr/nvsr60/nvsr60_03.pdf.
- 9.CDC and National Program of Cancer Registries. [Accessed May 12, 2013]; http://www.cdc.gov/cancer/npcr/uscs/download_data.htm/uscs_1999_2008_ASCII.zip.
- 10.US Census Bureau Intercensal Data. [Accessed May 12, 2013]; http://www.census.gov/popest/data/intercensal/index.html.
- 11.Havmoeller R, Reinier K, Teodorescu C, Uy-Evanado A, Mariani R, Gunson K, Jui J, Chugh SS. Low rate of secondary prevention icds in the general population: Multiple-year multiple-source surveillance of sudden cardiac death in the Oregon Sudden Unexpected Death Study. J Cardiovasc Electrophysiol. 2013;24:60–65. doi: 10.1111/j.1540-8167.2012.02407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fishman GI, Chugh SS, Dimarco JP, Albert CM, Anderson ME, Bonow RO, Buxton AE, Chen PS, Estes M, Jouven X, Kwong R, Lathrop DA, Mascette AM, Nerbonne JM, O'Rourke B, Page RL, Roden DM, Rosenbaum DS, Sotoodehnia N, Trayanova NA, Zheng ZJ. Sudden cardiac death prediction and prevention: Report from a national heart, lung, and blood institute and heart rhythm society workshop. Circulation. 2010;122:2335–2348. doi: 10.1161/CIRCULATIONAHA.110.976092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.CDC Interactive Atlas of Heart Disease and Stroke. [Accessed February 27, 2013]; http://apps.nccd.cdc.gov/DHDSPAtlas/viewer.aspx?state=OR.
- 14.Fay MP, Feuer EJ. Confidence intervals for directly standardized rates: A method based on the gamma distribution. Stat Med. 1997;16:791–801. doi: 10.1002/(sici)1097-0258(19970415)16:7<791::aid-sim500>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 15.Guidelines for using confidence intervals for public health assessment. Washington State Department of Health. [Acessed June 10, 2013]; www.doh.wa.gov/Documents/5500/ConfIntGuide.pdf.
- 16.Chugh SS. Early identification of risk factors for sudden cardiac death. Nat Rev Cardiol. 2010;7:318–326. doi: 10.1038/nrcardio.2010.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics--2013 update: A report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Cancer Institute's Surveillance. Epidemiology and End Results Program program discription. [Accessed April 18, 2013]; http://seer.cancer.gov/about/factsheets/SEER_brochure.pdf.
- 19.National Cancer Institute's Surveillance. Epidemiology and End Results Program Landmark Studies. [Accessed April 18, 2013]; http://seer.cancer.gov/studies/seer_landmark_studies.pdf.
- 20.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Burden of Disease Collaborators. The state of US health, 1990–2010: Burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sidney S, Rosamond WD, Howard VJ, Luepker RV. The "heart disease and stroke statistics--2013 update" and the need for a national cardiovascular surveillance system. Circulation. 2013;127:21–23. doi: 10.1161/CIRCULATIONAHA.112.155911. [DOI] [PubMed] [Google Scholar]
- 23.IOM (Institute of Medicine) A Nationwide Framework for Surveillance of Cardiovascular and Chronic Lung Diseases. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.