Abstract
Objective
Health literacy and numeracy are necessary to understand health information and to make informed medical decisions. This study explored the relationships among health literacy, numeracy, and ability to accurately interpret graphical representations of breast cancer risk.
Methods
Participants (N = 120) were recruited from the Facing Our Risk of Cancer Empowered (FORCE) membership. Health literacy and numeracy were assessed. Participants interpreted graphs depicting breast cancer risk, made hypothetical treatment decisions, and rated preference of graphs.
Results
Most participants were Caucasian (98%) and had completed at least one year of college (93%). Fifty-two percent had breast cancer, 86% had a family history of breast cancer, and 57% had a deleterious BRCA gene mutation. Mean health literacy score was 65/66; mean numeracy score was 4/6; and mean graphicacy score was 9/12. Education and numeracy were significantly associated with accurate graph interpretation (r = 0.42, p < 0.001 and r = 0.65, p < 0.001, respectively). However, after adjusting for numeracy in multivariate linear regression, education added little to the prediction of graphicacy (r2 = 0.41 versus 0.42, respectively).
Conclusion
In our highly health-literate population, numeracy was predictive of graphicacy.
Practice implications
Effective risk communication strategies should consider the impact of numeracy on graphicacy and patient understanding.
Keywords: Health literacy, Numeracy, Graphicacy, Breast cancer, Risk communication
1. Introduction
1.1. Effectual health communication supports informed decision-making
Essential to informed patient decision-making is the ability to understand numerically and graphically presented health information. Previous studies have shown that health literacy [1,2], numeracy [2,3], and graph design [4,5] may influence patient understanding of health communications. Comprehension of prevention and risk information is important in decision-making for women who carry a BRCA mutation given the magnitude of the associated risks of breast and ovarian cancer. BRCA mutations confer an 85% lifetime of breast cancer [6,7] and a second primary breast cancer risk of approximately 50% [8] as well as a lifetime risk for ovarian cancer of about 15–50% [6,7,9]. Women who carry a BRCA mutation may consider bilateral mastectomy and/or bilateral salpingo-oophorectomy as risk-reduction strategies [10]. In order to make a fully informed decision regarding risk management, it is important that these women understand their cancer risks as well as the risk-reduction impact and quality of life outcomes of each surgical intervention. No studies to date have explored the ability of BRCA+ women to interpret graphically presented risk information.
1.2. Health literacy and numeracy affect cancer prevention and treatment compliance
The United States Department of Health and Human Services has defined health literacy as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” [11]. As such, health literacy has been shown to be a critical component of meaningful cancer risk communication, treatment and screening compliance, informed consent, and overall patient health [1,12–16]. Individuals with low health literacy scores often do not understand basic cancer prevention, or diagnosis and treatment terminology such as screening, colon, tumor, lesion, and cure, which may contribute to a lack of adherence to potentially lifesaving screening recommendations [17].
Numeracy has been defined as, “the degree to which individuals have the capacity to access, process, interpret, communicate, and act on numerical, quantitative, graphical, biostatistical, and probabilistic health information needed to make effective health decisions” [18]. Until recently, numeracy was considered and often measured as a component of health literacy. However, several studies have shown that numeracy is a separate proficiency from literacy and that health numeracy is a significant and distinctive aspect of health knowledge and communication [2,18–21].
Patient numeracy and the presentation of probabilistic health outcome information impact health care in diverse areas from prevention to treatment [22–25]. Although patients report higher trust and comfort with their health care provider when numerical data are included [26], they may not always understand the given data. In a study of 463 highly educated participants, about 40% could not solve a basic probability problem or convert a percentage to a proportion [27]. Therefore, health care providers cannot assume that well-educated patients are numerate when discussing treatment decisions and risk. In another study, less numerate women were less likely to accurately assess the reduction in breast cancer death from screening mammography [28]. Additionally, studies suggest that innumerate individuals are more likely than their numerate peers to inaccurately understand their health risks [3] and are more likely to have inaccurate perceptions of the health consequences of cancer screening, surveillance, and treatment choices [19,29].
1.3. Graphicacy is a complex skill utilized to understand personal cancer risk
Graphicacy has been defined as “the ability to understand and present information in the form of sketches, photographs, diagrams, maps, plans, charts, graphs, and other non-textual, two-dimensional formats” [30]. Graphical representations of risk have been shown to improve patient understanding, informed consent, and decision-making accuracy [5,31], particularly for those individuals with low levels of numeracy [28,32].
Several studies have tested the effectiveness of various graphical formats. The presentation of health care data in simple forms, such as single line graphs [33], bar graphs [34] or frequency graphs showing highlighted human figures [4], has been shown to improve patient understanding and influence treatment decisions. A bar graph tailored to women's breast cancer risk improved accuracy of self-described risk among women with a family history of breast cancer [34]. Another study found that using a frequency diagram plus a bar graph improved risk perception accuracy more than by using a bar graph alone [35]. A focus group study concluded that frequency graphs are contextual, easy to understand, and meaningful; however, when compared to participants with more formal education, participants with less education more often perceived their risk of breast cancer to be erroneously high when using human figure frequency graphs rather than bar graphs [4]. In addition, some participants found that bar graphs were a more helpful format for the comparison of multiple risks [4]. Another study showed that utilizing two complimentary graphs, a frequency graph along with a bar graph, improved risk perception accuracy more than by using a single graph [35]. In studies considering patient understanding and treatment choice by comparing risk communication formats, researchers identified that graphical format alone influenced risk perception and treatment decisions [36,37].
Thus, graphicacy is considered a key patient skill utilized for breast cancer risk communication [38], yet, little is known about the relationship of graphicacy to health literacy and numeracy. Therefore, the aim of this study was to examine the relationship between literacy, numeracy, and graphicacy, in the context of breast cancer risk communication and decision-making about risk-reducing surgery for high risk patients.
2. Participants and methods
2.1. Study population and recruitment
This study was approved by the University of California Irvine's Institutional Review Board. Participants were recruited between December 2006 and January 2007 by placing a link on the FORCE breast cancer advocacy website at www.facingourrisk.org, and sending an email blast to approximately 4500 registered users. The email blast yielded 205 respondents within 24 h, and the total number of respondents was 219. Eligibility included women with a personal and/or family history of breast cancer. Consecutive respondents (N = 120) who provided adequate contact information were mailed the study information sheet and a sealed envelope containing the survey instruments. Participants were called by the lead investigator (SB) to review the study, obtain informed consent and complete the health literacy, numeracy and graphicacy assessments (described below). Demographic questions were asked including age, education, employment, income, breast cancer history, the type of clinician who provided risk education, BRCA testing history, and mutation status. All personally identifiable health information was anonymized.
2.2. Health literacy measure
Health literacy was assessed by administering the 66-word version of the Rapid Estimate of Adult Literacy in Medicine (REALM) [39]. REALM has been widely accepted and incorporated into medical research assessing health literacy. Participant ability to correctly read the 66-word list of medical/health terms was determined by subtracting one point for every word missed or mispronounced. The scale was scored as follows: 61–66 = high school, 45–60 = 7th to 8th grade, 19–44 = 4th to 6th grade, 0–16 = 3rd grade and below.
2.3. Health numeracy measure
Numeracy was assessed with a 6-question numeracy scale (Fig. 1) by combining two previously validated 3-question numeracy scales developed by Woloshin and Schapira to quickly analyze participant numerical ability [29,40]. Cronbach's alpha were 0.57–0.63 and 0.63, respectively [40,41]. Both scales included a simple coin toss question (Q1). Due to concerns that Internet recruitment would yield a highly educated population [42,43], a more difficult question (Q2) was added to allow for a greater range of numeracy scores.
Fig. 1.
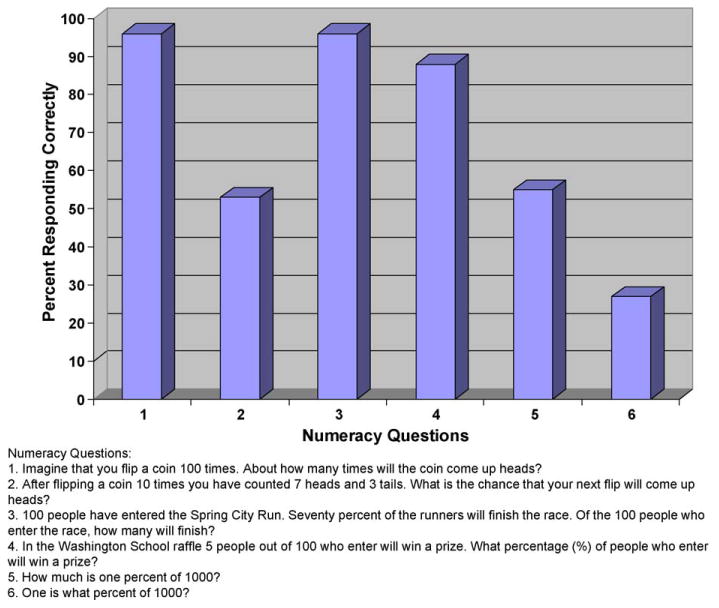
Numeracy assessment: percent correct responses to numeracy questions (N = 120).
One of the validated 3-question numeracy scales had been designed and used to produce a continuous numeracy variable [29], while the other produced a categorical variable [40] that resulted in the dichotomous categorization of individuals as numerate or innumerate. Because another study suggested the potential utility of further stratifying results to produce a moderately numerate category [44] and for ease of presentation, we chose to analyze numeracy as a continuous variable coded 1–6, with 1 point for each correct answer, and also to examine numeracy as a categorical variable (low: 1–2 points, moderate: 3–4 points, or high: 5–6 points).
2.4. Health graphicacy measure
Four hypothetical graphical representations of breast cancer risk were developed by the investigators to measure graph interpretation: vertical bar, horizontal bar, line, and iconic (Fig. 2). Each graph illustrated the chance of a second primary breast cancer for a supposed patient given four surgical options: no surgery, bilateral mastectomy, bilateral oophorectomy, and bilateral mastectomy plus oophorectomy. The graphs were not individualized for each participant and the actual absolute risks were chosen for convenience and were not exactly what would have been expected after the proposed intervention. Participants were asked to review each graph and respond to question A, which required basic interpretation of the risk remaining after a surgical option, and to two related questions B and C, which required surgical decision-making based on the hypothetical patient and an interpretation of the resulting risk, respectively. The decision-making questions (B and C) for graphs 1 and 3 involved identifying two surgical options and comparing the difference in risk, and for graphs 2 and 4, involved identifying a single surgical option and the remaining risk. Correctly answering question C was dependent on correctly answering question B, therefore the percent who answered question C correctly is based on a smaller sample size. One point was given for each correct answer. Graphicacy was measured as the total number of correct answers from all four graphs and resulted in a total graph interpretation score of between 0 and 12 possible points. For ease of presentation, graphicacy was also analyzed as a categorical variable with four categories of 0–3, 4–6, 7–9, and 10–12.
Fig. 2.

Survey instrument: graph formats showing breast cancer risk for hypothetical cases.
2.5. Graph preference measure
Participants were asked to rate their preference for each graph based on a 6-point Likert scale, where 1 equaled a poor graph and 6 equaled a good graph.
2.6. Statistical analysis
Psychometric characteristics of the combined validated numeracy scales were assessed. Frequency and percentage distributions were determined for all variables and were analyzed in relation to numeracy and graphicacy. Categorical variables were tested for association with numeracy and with graphicacy using the Pearson chi-square test. Associations between continuous variables were assessed using Pearson correlations. The univariate relationship between graphicacy and numeracy and other independent variables was investigated using analysis of variance (ANOVA) and linear regression methods. Multiple linear regression was used to investigate the relationship between graphicacy (dependent variable) and health literacy, numeracy, age, years of college, income, personal and family breast cancer history, and BRCA status (independent variables). Statistical analysis was performed with the SYSTAT 11 program. Significance was set at the 0.05 level.
3. Results
3.1. Demographics
Participant-reported demographic characteristics, cancer history, and BRCA status of the 120 participants are shown in Table 1. The mean age of participants was 45.6 years (SD = 8.7). Participants were primarily European American (98%) who had completed at least some college (92%), had a personal (52%) and/or family history (86%) of breast and/or ovarian cancer, and carried a BRCA mutation (58%). Their reported average total household income of $123,410 (SD = $82,500) is more than double the national average of $48,000. [45] Participant addresses were distributed over 30 continental U.S. states.
Table 1.
Socio-demographic and breast cancer history/genetic characteristics of study participants (N = 120).
| Characteristic | N (%) |
|---|---|
| Age in years (range 24–69) | |
| Less than or equal to 50 years | 90 (75) |
| Greater than 50 years | 30 (25) |
| Race/ethnicity | |
| Caucasian, Non-Hispanic | 118 (98) |
| African American | 1 (1) |
| Hispanic | 1 (1) |
| Education | |
| High School | 9 (8) |
| Some College | 17 (14) |
| Bachelor degree | 50 (42) |
| Master degree | 37 (31) |
| MD and/or PhD | 7 (6) |
| Occupation | |
| Home-maker, retired, student | 30 (25) |
| Laborer | 3 (3) |
| Administrator | 15 (13) |
| Science/medicine | 30 (25) |
| Other professional | 42 (35) |
| Total household income (N = 117)a | |
| Less than $50,000 | 11 (9) |
| $50,000–99,999 | 35 (30) |
| $100,000–149,999 | 33 (28) |
| $150,000 or higher | 38 (33) |
| Breast (or ovarian) cancer | |
| Family history | 103 (86) |
| Personal history | 62 (52) |
| BRCA testing | |
| Tested | 94 (78) |
| Mutation positive | 69 (58) |
Three participants declined to state their total household income.
3.2. Health literacy scores
All REALM scores fell within the highest literacy range. The average REALM score out of 66 possible points was 65.06 (SD = 1.04, range 61–66). Each participant read and attempted to pronounce each word; however, very few words (impetigo, colitis, and anemia) were occasionally mispronounced.
3.3. Numeracy scores
Fig. 1 shows the six numeracy questions and the percentage of participants responding correctly to each question. Psychometric analyses indicated that the resulting two 3-question numeracy scores were significantly correlated with each other (r = 0.34) and highly correlated with the 6 question assessment (r = 0.58 and 0.82), supporting the validity of the 6-question numeracy scale. Out of 6 questions, the mean number of correct answers was 4.11 (SD = 1.17, range 1–6). When categorized, 8% of the participants were low numerate (1–2 points), 53% were moderately numerate (3–4 points), and 40% were highly numerate (5–6 points). Completed years of college showed significant and strong association with numeracy (r = 0.44, p < 0.001). Participants who had not attended college never scored within the high numeracy range and none of those with a medical and/or doctorate degree scored within the low numeracy range. Health literacy was moderately associated with numeracy (r = 0.27, p < 0.01).
3.4. Graphicacy scores
The mean graphicacy score was 8.84 points (SD = 2.23, range 4–12). When categorized, 17% of the participants had a low graph score (4–6 points), 42% had a moderate score (7–9 points), and 42% had a high score (10–12 points).
Fig. 3 shows the graph assessment questions and the percentage of participants responding correctly to each question. Graph question A(1–4), which asked participants to interpret the breast cancer risk following a preventive surgery choice, was answered correctly the majority of the time for all four graphs. However, a higher percentage of participants answered correctly when viewing the horizontal (96%) or vertical (93%) bar graphs compared to the line (72%) or iconic (84%) graphs. In contrast, question B(1–4), which asked participants to use the graph to make a surgical decision was answered correctly less often for the vertical bar graph (45%) than for the horizontal bar graph (73%), line graph (96%), and iconic graph (93%). Questions C1 and C3 asked participants to compare the difference in remaining risks after two preventive surgical options. The percent correctly answering C1 and C3 was similar (65% and 63%, respectively). Questions C2 and C4 asked participants to state the remaining risk after a single preventive surgery. The percent correctly answering C2 and C4 was the same (87%).
Fig. 3.
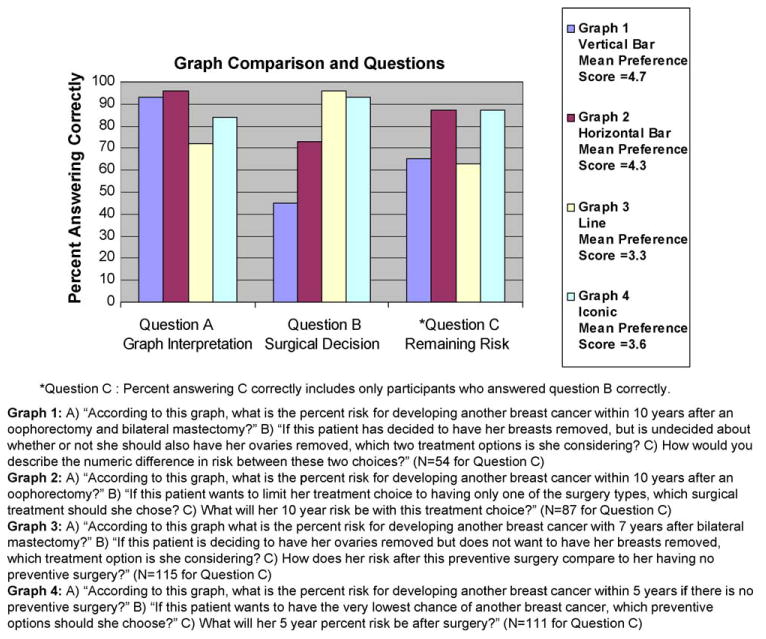
Graphicacy assessment: percent correct responses to survey instrument (N = 120).
Respondents found it more difficult to compare the risk-reduction values between two surgeries than to determine the risk after a single preventive surgery, independent of graph format. Overall, participants answered the questions correctly more often when using the iconic graph (88%) compared to the horizontal bar (85%), line (77%), or vertical bar (68%) graphs.
The mean preference score for each graph is shown in the legend of Fig. 3. Study participants reported the highest preference for the graph with the lowest percent answering correctly (vertical bar graph) and a lower preference for the graph with the highest percent answering correctly (iconic graph). On a scale of 1–6, the participants preferred the vertical bar graph (4.7), compared to the horizontal bar graph (4.3), the iconic graph (3.6), or the line graph (3.3).
3.5. Relating the independent variables to graph interpretation
Fig. 4 illustrates the mean graphicacy score for each numeracy level. The correlation between numeracy and graphicacy was positive and significant (r = 0.64, p < 0.001).
Fig. 4.
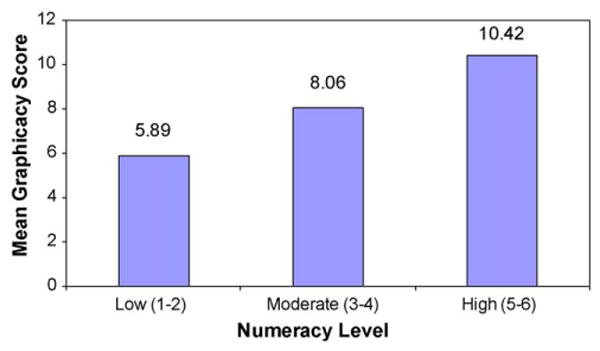
Relationship of numeracy to graphicacy (N = 120).
Both numeracy and education (completed years of college) were significantly associated with graphicacy score in univariate analyses (r = 0.64, p < 0.001 and r = 0.37, p < 0.001, respectively). However, after adjusting for numeracy in multiple linear regression, education added little to the prediction of graphicacy (r2 = 0.41 versus 0.42, respectively) (Table 2). In stepwise linear regression, no other covariates studied were significant predictors of graphicacy after adjusting for numeracy.
Table 2.
Prediction of graphicacy: multivariate regression.
| Independent variables | Effect | Coefficient | SE | t | p (2 tail) | Multiple r2 |
|---|---|---|---|---|---|---|
| Numeracy | Constant | 3.843 | 0.575 | 6.684 | <0.0005 | |
| Numeracy | 1.217 | 0.135 | 9.040 | <0.0005 | 0.409 | |
| Numeracy + education | Constant | 3.454 | 0.613 | 5.633 | <0.0005 | |
| Numeracy | 1.101 | 0.149 | 7.374 | <0.0005 | ||
| Education | 0.402 | 0.233 | 1.725 | 0.087 | 0.424 |
In stepwise linear regression, after adjusting for numeracy, no covariates were significant predictors of graphicacy. Education added little to the prediction of graphicacy.
4. Discussion and conclusion
4.1. Discussion
The reasons for using graphs to communicate health risks are compelling: patients may gain valuable understanding, develop the judgment needed to compare outcomes, and may achieve improved confidence in decision-making [32]. Decision aids may potentially be developed that incorporate numeracy and graphicacy assessment, tailor for patient preference and understanding, as well as provide individualized risk interpretation tutorials.
While it may seem reasonable for clinicians to presume that health-literate and educated patients will have proficient numerical ability and will correctly interpret graphical risk information, findings from this and other studies profiling subject numeracy indicate that education level does not predict numeracy [2,27,46]. An expert review of visual communication suggests that less numerate individuals may benefit from graphical representation of risk [32]. However, our study found that individuals who had lower numeracy had lower graphicacy levels, suggesting that less numerate individuals may have less ability to interpret the graphs.
Preference for a particular type of graph does not always relate to performance of the graph [41]. Our study found that the vertical bar graph was the most preferred format, while the iconic graph led to the highest graphicacy scores. One reason the iconic graph may have been preferred was because of the ease of understanding the shading in a figure with only ten icons. But it is not possible to express more precise figures (e.g., a 12% risk) in such a format; perhaps the iconic format would be less preferred if a reference group of 100 or 1000 figures were used. Hence, further investigation is needed to determine how to best recognize which individuals may benefit most from different graphical risk formats. Nelson et al. argue that there may be situations in which patients should be able to choose their preferred format because patients may be more likely to use decision aids if graphical formats are customized to their personal preference for numerical presentation.
Several aspects intrinsic to the study design limit generalization of the findings. Participants were female, highly educated, and mostly Caucasian. Conducting this study with a less homogeneous sample and with other populations may clarify the global utility of our findings. In addition, the graphs were presented in the same order for every study participant, therefore, a trend in graph score could be associated with graph order as an artifact of subject learning. Also, the effect of graph format may be due to differences in the questions posed for each format.
4.2. Conclusion
To our knowledge, this report represents the first study to consider the relationship of patient numeracy to graphicacy, independent of health literacy and education. We found that although there was nearly a ceiling effect for health literacy, there was considerable variability in numeracy and graphicacy. In our study, numeracy accounted for 41% of the variation in graph interpretation scores, suggesting that numeracy and graphicacy are strongly linked.
Overall, graphicacy scores varied by graph format; participants scored highest when using the iconic graph. Interestingly, performance and preference did not match; participants answered the fewest questions correctly when using the vertical bar graph but ranked this graph highest in personal preference. Our findings confirm previous studies showing that participants preferred simple bar graphs [47] and that preference was not always associated with accuracy [48]. Consequently, the graphicacy assessment instrument may be an important tool in risk communications research. Further investigation is needed to determine the effect of graph format on risk perception and behavior and to develop formats that target specific communication goals.
4.3. Practice implications
As the direction of patient–clinician communication moves towards shared decision-making and increased patient autonomy, appropriately addressing patient numeracy and graphicacy becomes increasingly important. To improve patients' understanding, compliance, and health outcomes, clinicians should consider these proficiencies when counseling patients about risk, options and outcomes including preventive choices and treatment decisions.
Acknowledgments
The authors thank Virginia Kimonis, MD, Lari Wenzel, PhD, and Susan Neuhausen, PhD from the University of California, Irvine, who assisted in development of the study. We thank Janelle Hilario and Shawntel Payton for technical assistance with the manuscript. This research was supported in part by a grant from the Susan G. Komen Breast Cancer Foundation (Grant #BCTR0600463).
Footnotes
Conflicts of interest: The authors do not have any actual or potential conflicts of interest to disclose.
References
- 1.Paasche-Orlow MK, Schillinger D, Greene SM, Wagner EH. How health care systems can begin to address the challenge of limited literacy. J Gen Intern Med. 2006;8:884–7. doi: 10.1111/j.1525-1497.2006.00544.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Estrada C, Barnes V, Collins C, Byrd JC. Health literacy and numeracy. J Amer Med Assoc. 1999;282:527. doi: 10.1001/jama.282.6.527. [DOI] [PubMed] [Google Scholar]
- 3.Zikmund-Fisher BJ, Smith DM, Ubel PA, Fagerlin A. Validation of the subjective numeracy scale: effects of low numeracy on comprehension of risk communications and utility elicitations. Med Decis Making. 2007;27:663–71. doi: 10.1177/0272989X07303824. [DOI] [PubMed] [Google Scholar]
- 4.Schapira MM, Nattinger AB, McHorney CA. Frequency or probability? A qualitative study of risk communication formats used in health care. Med Decis Making. 2001;21:459–67. doi: 10.1177/0272989X0102100604. [DOI] [PubMed] [Google Scholar]
- 5.Lipkus IM. Numeric, verbal, and visual formats of conveying health risks: suggested best practices and future recommendations. Med Decis Making. 2007;27:696–713. doi: 10.1177/0272989X07307271. [DOI] [PubMed] [Google Scholar]
- 6.Ford D, Easton DF, Stratton M, Narod S, Goldgar D, Devilee P, et al. Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. The breast cancer linkage consortium. Am J Hum Genet. 1998;62:676–89. doi: 10.1086/301749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.King MC, Marks JH, Mandell JB. Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science. 2003;302:643–6. doi: 10.1126/science.1088759. [DOI] [PubMed] [Google Scholar]
- 8.Metcalfe KA, Lynch HT, Ghadirian P, Tung N, Olivotto I, Warner E, et al. Contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2004;22:2328–35. doi: 10.1200/JCO.2004.04.033. [DOI] [PubMed] [Google Scholar]
- 9.Metcalfe KA, Lynch HT, Ghadirian P, Tung N, Olivotto IA, Foulkes WD, et al. The risk of ovarian cancer after breast cancer in BRCA1 and BRCA2 carriers. Gynecol Oncol. 2005;96:222–6. doi: 10.1016/j.ygyno.2004.09.039. [DOI] [PubMed] [Google Scholar]
- 10.Schrag D, Kuntz KM, Garber JE, Weeks JC. Life expectancy gains from cancer prevention strategies for women with breast cancer and BRCA1 or BRCA2 mutations. J Amer Med Assoc. 2000;283:617–24. doi: 10.1001/jama.283.5.617. [DOI] [PubMed] [Google Scholar]
- 11.Healthy people 2010: understanding and improving health. Washington, DC: Department of Health and Human Services; Jan, 2000. [Google Scholar]
- 12.Bennett CL, Ferreira MR, Davis TC, Kaplan J, Weinberger M, Kuzel T, et al. Relation between literacy, race, and stage of presentation among low-income patients with prostate cancer. J Clin Oncol. 1998;16:3101–4. doi: 10.1200/JCO.1998.16.9.3101. [DOI] [PubMed] [Google Scholar]
- 13.Davis TC, Arnold C, Berkel HJ, Nandy I, Jackson RH, Glass J. Knowledge and attitude on screening mammography among low-literate, low-income women. Cancer. 1996;78:1912–20. doi: 10.1002/(sici)1097-0142(19961101)78:9<1912::aid-cncr11>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 14.Davis TC, Michielutte R, Askov EN, Williams MV, Weiss BD. Practical assessment of adult literacy in health care. Health Educ Behav. 1998;25:613–24. doi: 10.1177/109019819802500508. [DOI] [PubMed] [Google Scholar]
- 15.Williams MV, Davis T, Parker RM, Weiss BD. The role of health literacy in patient–physician communication. Fam Med. 2002;34:383–9. [PubMed] [Google Scholar]
- 16.Davis TC, Williams MV, Marin E, Parker RM, Glass J. Health literacy and cancer communication. CA Cancer J Clin. 2002;52:134–49. doi: 10.3322/canjclin.52.3.134. [DOI] [PubMed] [Google Scholar]
- 17.Davis TC, Dolan NC, Ferreira MR, Tomori C, Green KW, Sipler AM, et al. The role of inadequate health literacy skills in colorectal cancer screening. Cancer Invest. 2001;19:193–200. doi: 10.1081/cnv-100000154. [DOI] [PubMed] [Google Scholar]
- 18.Golbeck AL, Ahlers-Schmidt CR, Paschal AM, Dismuke SE. A definition and operational framework for health numeracy. Am J Prev Med. 2005;29:375–6. doi: 10.1016/j.amepre.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 19.Peters E, Vastfjall D, Slovic P, Mertz CK, Mazzocco K, Dickert S. Numeracy and decision making. Psychol Sci. 2006;17:407–13. doi: 10.1111/j.1467-9280.2006.01720.x. [DOI] [PubMed] [Google Scholar]
- 20.Schwartz LM, Woloshin S, Welch HG. Can patients interpret health information? An assessment of the medical data interpretation test. Med Decis Making. 2005;25:290–300. doi: 10.1177/0272989X05276860. [DOI] [PubMed] [Google Scholar]
- 21.Woloshin S, Schwartz LM, Welch HG. Patients and medical statistics. Interest, confidence, and ability. J Gen Intern Med. 2005;20:996–1000. doi: 10.1111/j.1525-1497.2005.00179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Armstrong K, Schwartz JS, Fitzgerald G, Putt M, Ubel PA. Effect of framing as gain versus loss on understanding and hypothetical treatment choices: survival and mortality curves. Med Decis Making. 2002;22:76–83. doi: 10.1177/0272989X0202200108. [DOI] [PubMed] [Google Scholar]
- 23.Chao C, Studts JL, Abell T, Hadley T, Roetzer L, Dineen S, et al. Adjuvant chemotherapy for breast cancer: how presentation of recurrence risk influences decision-making. J Clin Oncol. 2003;21:4299–305. doi: 10.1200/JCO.2003.06.025. [DOI] [PubMed] [Google Scholar]
- 24.Waters EA, Weinstein ND, Colditz GA, Emmons K. Formats for improving risk communication in medical tradeoff decisions. J Health Commun. 2006;11:167–82. doi: 10.1080/10810730500526695. [DOI] [PubMed] [Google Scholar]
- 25.Weinstein ND. What does it mean to understand a risk? Evaluating risk comprehension. J Natl Cancer Inst Monogr. 1999;25:15–20. doi: 10.1093/oxfordjournals.jncimonographs.a024192. [DOI] [PubMed] [Google Scholar]
- 26.Gurmankin AD, Baron J, Armstrong K. The effect of numerical statements of risk on trust and comfort with hypothetical physician risk communication. Med Decis Making. 2004;24:265–71. doi: 10.1177/0272989X04265482. [DOI] [PubMed] [Google Scholar]
- 27.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 28.Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med. 1997;127:966–72. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- 29.Woloshin S, Schwartz LM, Moncur M, Gabriel S, Tosteson AN. Assessing values for health: numeracy matters. Med Decis Making. 2001;21:382–90. doi: 10.1177/0272989X0102100505. [DOI] [PubMed] [Google Scholar]
- 30.Aldrich FK, Sheppard L. Graphicacy: the fourth ‘R’? Prim Sci Rev. 2000;64:8–11. [Google Scholar]
- 31.Bogardus ST, Jr, Holmboe E, Jekel JF. Perils, pitfalls, and possibilities in talking about medical risk. J Amer Med Assoc. 1999;281:1037–41. doi: 10.1001/jama.281.11.1037. [DOI] [PubMed] [Google Scholar]
- 32.Lipkus IM, Hollands JG. The visual communication of risk. J Natl Cancer Inst Monogr. 1999;25:149–63. doi: 10.1093/oxfordjournals.jncimonographs.a024191. [DOI] [PubMed] [Google Scholar]
- 33.Brundage M, Feldman-Stewart D, Leis A, Bezjak A, Degner L, Velji K, et al. Communicating quality of life information to cancer patients: a study of six presentation formats. J Clin Oncol. 2005;23:6949–56. doi: 10.1200/JCO.2005.12.514. [DOI] [PubMed] [Google Scholar]
- 34.Burke W, Culver JO, Bowen D, Lowry D, Durfy S, McTiernan A, et al. Genetic counseling for women with an intermediate family history of breast cancer. Am J Med Genet. 2000;90:361–8. doi: 10.1002/(sici)1096-8628(20000228)90:5<361::aid-ajmg4>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 35.Ghosh K, Crawford BJ, Pruthi S, Williams CI, Neal L, Sandhu NP, et al. Frequency format diagram and probability chart for breast cancer risk communication: a prospective, randomized trial. BMC Womens Health. 2008;8:18. doi: 10.1186/1472-6874-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Timmermans D, Molewijk B, Stiggelbout A, Kievit J. Different formats for communicating surgical risks to patients and the effect on choice of treatment. Patient Educ Couns. 2004;54:255–63. doi: 10.1016/S0738-3991(03)00238-6. [DOI] [PubMed] [Google Scholar]
- 37.Timmermans DR, Ockhuysen-Vermey CF, Henneman L. Presenting health risk information in different formats: the effect on participants' cognitive and emotional evaluation and decisions. Patient Educ Couns. 2008;73:443–7. doi: 10.1016/j.pec.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 38.Schapira MM, Nattinger AB, McAuliffe TL. The influence of graphic format on breast cancer risk communication. J Health Commun. 2006;11:569–82. doi: 10.1080/10810730600829916. [DOI] [PubMed] [Google Scholar]
- 39.Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–5. [PubMed] [Google Scholar]
- 40.Schapira MM, Davids SL, McAuliffe TL, Nattinger AB. Agreement between scales in the measurement of breast cancer risk perceptions. Risk Anal. 2004;24:665–73. doi: 10.1111/j.0272-4332.2004.00466.x. [DOI] [PubMed] [Google Scholar]
- 41.Nelson W, Reyna VF, Fagerlin A, Lipkus I, Peters E. Clinical implications of numeracy: theory and practice. Ann Behav Med. 2008;35:261–74. doi: 10.1007/s12160-008-9037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Im EO, Chee W. Recruitment of research participants through the Internet. Comput Inform Nurs. 2004;22:289–97. doi: 10.1097/00024665-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 43.Lenert L, Skoczen S. The Internet as a research tool: worth the price of admission? Ann Behav Med. 2002;24:251–6. doi: 10.1207/S15324796ABM2404_01. [DOI] [PubMed] [Google Scholar]
- 44.Schwartz SR, McDowell J, Yueh B. Numeracy and the shortcomings of utility assessment in head and neck cancer patients. Head Neck. 2004;26:401–7. doi: 10.1002/hed.10383. [DOI] [PubMed] [Google Scholar]
- 45.DeNavas-Walt C, Proctor BD, Smith J. In: Income, poverty, and health insurance coverage in the United States: 2006. Bureau UC, editor. Washington, DC: U.S. Government Printing Office; 2007. pp. P60–233. [Google Scholar]
- 46.Sheridan SL, Pignone M. Numeracy and the medical student's ability to interpret data. Eff Clin Pract. 2002;5:35–40. [PubMed] [Google Scholar]
- 47.Fortin JM, Hirota LK, Bond BE, O'Connor AM, Col NF. Identifying patient preferences for communicating risk estimates: a descriptive pilot study. BMC Med Inform Decis Making. 2001;1:2. doi: 10.1186/1472-6947-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ancker JS, Senathirajah Y, Kukafka R, Starren JB. Design features of graphs in health risk communication: a systematic review. J Am Med Inform Assoc. 2006;13:608–18. doi: 10.1197/jamia.M2115. [DOI] [PMC free article] [PubMed] [Google Scholar]


