Abstract
Ultrasound is a unique and exciting theranostic modality that can be used to track drug carriers, trigger drug release and improve drug deposition with high spatial precision. In this review, we briefly describe the mechanisms of interaction between drug carriers and ultrasound waves, including cavitation, streaming and hyperthermia, and how those interactions can promote drug release and tissue uptake. We then discuss the rational design of some state-of-the-art materials for ultrasound-triggered drug delivery and review recent progress for each drug carrier, focusing on the delivery of chemotherapeutic agents such as doxorubicin. These materials include nanocarrier formulations, such as liposomes and micelles, designed specifically for ultrasound-triggered drug release, as well as microbubbles, microbubble-nanocarrier hybrids, microbubble-seeded hydrogels and phase-change agents.
Rational Design of Ultrasound-Triggered Drug Carriers
Early reports in the field of ultrasonic drug delivery demonstrated that the application of ultrasound energy alone may facilitate intracellular delivery of molecules [1–7]. Therefore, it stands to reason that ultrasound with ultrasound-responsive materials can be an effective tool for enhancing the therapeutic efficacy of a drug during therapy. In this review, we cast a selection of recent innovative materials for ultrasound-triggered drug delivery into the rational design paradigm in order to identify general design rules that scientists and engineers can use in their quest for more potent drug carriers. Our main focus is on ultrasound-targeted drug delivery; gene therapy has been recently reviewed elsewhere [8].
We start by defining the general rational design paradigm: that materials can be engineered for a specific application by understanding the key interrelationships between composition, processing, structure, property and performance. In drug delivery, the main performance criterion is the therapeutic index (TI), defined as the drug dose that produces a toxicity in 50% of the population (TD50) divided by the minimum effective dose for 50% of the population (ED50).
| (1) |
Targeting increases TI by simultaneously increasing the dose required for toxicity and decreasing that for effective therapy. This is achieved by delivering a greater percentage of the drug to the target tissue and avoiding healthy tissue. For ultrasound-triggered drug delivery, the main properties that are necessary to achieve a significant increase in TI are (1) stable encapsulation of the drug compound prior to application of ultrasound, (2) release of the drug by ultrasound stimulation and (3) the ability to image the carrier and monitor delivery of the drug cargo. The adoption of the third criterion provides theranostic control capabilities to the drug delivery system and is ideally suited for ultrasound, which is widely used for both imaging and therapy.
Several types of nano, micro and macro structures have been developed with these properties in mind. These include microbubbles, liposomes, micelles, phase-change emulsions, microbubble-loaded hydrogels and other interesting structures. In this review, we illustrate a few promising structures by focusing on how they were synthesized and characterized, how they interact with ultrasound, and how they performed at ultrasound-triggered drug delivery.
Ultrasound Triggers
As an ultrasound wave propagates through tissue in the body, several physical effects occur which can be used as triggers for ultrasound-mediated drug release. These physical effects include simple pressure variation, acoustic fluid streaming, cavitation and local hyperthermia. Rational design of an ultrasound-triggered drug carrier typically involves designing the material to respond to one or more of these triggers.
Pressure Variation
In medical ultrasound, transducers are used to generate longitudinal pressure waves, which are transmitted into the body at varying frequency and amplitude. The broad range of biomedical ultrasound frequencies are 0.1–50 MHz and peak negative pressures are 0.01–10 MPa [9][10]. The acoustic waves are attenuated as they pass through tissue owing to absorption and scatter of the acoustic energy, and this effect typically increases with increasing transmit frequency. Near 1 MHz, however, this attenuation is minimal and deep-tissue imaging/therapy is possible. Ultrasound is also characterized by pulse length and shape, as well as pulse repetition frequency. For imaging, the reflections and scatter of acoustic waves are detected and used to generate an image. For drug delivery, on the other hand, acoustic waves are used to stimulate the carrier to release its cargo, and/or provide other bioeffects such as enhanced vascular permeability. The key mechanisms of drug carrier interactions with acoustic waves are cavitation, acoustic streaming and hyperthermia.
Cavitation
Compressible objects, such as microbubbles, contract and expand as they experience the compression and rarefaction cycles of passing acoustic waves. These volumetric oscillations can facilitate drug release, increased drug uptake and strong backscattered echoes that can be used for imaging. The type of cavitation depends highly on the amplitude and frequency of the ultrasound wave, as well as the size and material properties of the bubble. In many cases, the bubble activity can be divided into “stable” or “inertial” cavitation regimes depending on the mechanical index (MI) [11]. The MI is defined as the derated in situ peak negative pressure (PnP) divided by the center frequency (Fc) [11,12]:
| (2) |
where the units of PnP and Fc are MPa and MHz respectively. The MI is by no means a perfect measure or predictor of biological consequence and does not account well for the presence of ultrasound-sensitive materials in the body, which are discussed in this review. In general, diagnostic imaging occurs at MI levels below 1.9, which is the maximum allowable MI for clinical imaging applications without microbubbles [12]. A maximum MI of 1.9 would likely apply for imaging incompressible drug carriers, such as micelles and liposomes. Microbubbles, on the other hand, interact strongly with ultrasound by acting as “cavitation nuclei”[13], and the maximum allowable MI when using microbubbles is 0.8[14]. Below an MI of 0.8, microbubbles undergo stable cavitation, in which the microbubble is stable over many acoustic cycles, and which is often characterized as a backscattered signal centered at the fundamental and harmonic frequencies. It is unclear what the maximum allowable MI would be for imaging phase-change agents.
Therapeutic ultrasound, in which biological effects are desired, uses higher MI values. High MI ultrasound can result in the violent collapse of gas bubbles, a phenomenon known as “inertial cavitation” [15]. This high energy event is associated with extreme, localized pressures and temperatures that can disrupt the drug carrier and enhance drug uptake. In addition to acting on preformed microbubbles, inertial cavitation can be nucleated in the aqueous phase adjacent to a drug carrier. Alternatively, cavitation can be nucleated within the hydrophobic portion of a drug carrier, such as within the lipid bilayer of a liposome, due to weaker intermolecular cohesive forces compared to water. These latter mechanisms are important for drug targeting using micelles and liposomes. The biological consequences from acoustic phenomena are discussed in detail elsewhere [12,16–19]. For comprehensive reviews on the physical effects of ultrasound on compressible microbubbles, please see articles by Qin et al. [20] and Postema et al. [21].
Acoustic Streaming
Radiation forces experienced by reflectors and scatterers in the ultrasound field can lead to localized particle displacements and fluid currents, termed “acoustic streaming” [15]. Acoustic streaming may involve “bulk streaming”, where fluid is moved in the direction of the propagating sound wave, or “microstreaming” wherein localized eddies or currents are generated next to cavitating bodies [22]. Bulk streaming produces a “radiation force” that can move particles in the direction of the propagating ultrasound wave. For stably cavitating microbubbles, radiation forces are maximal at driving frequencies near the microbubble resonance frequency. Radiation forces can be used to displace particles in blood [23], to facilitate adhesion between circulating agents and the endothelium, and to drive particles into target tissue [24,25]. Microstreaming is another effect of cavitation that can increase the local mass transfer coefficient through enhanced convection, and it can induce shear stresses that destabilize drug carriers and permeabilize cell membranes and vascular endothelia. The effects of microstreaming around cavitation bubbles can be modeled in exquisite detail [26], and the overall phenomenon may be exploited to promote extravasation and delivery of circulating agents to target tissue.
Hyperthermia
Ultrasound energy is dissipated to thermal energy as the acoustic waves propagate through tissue and generate friction. Focused ultrasound can lead to localized tissue heating [27], which may be monitored and guided by magnetic resonance imaging (MRI) and other thermometric imaging techniques [28–30]. Studies have shown that cavitation bubbles can enhance ultrasonic heating [31–33]. Tissue hyperthermia can be used to release drugs from thermo-sensitive carriers designed to destabilize above specific temperatures. Specific examples of thermo-sensitive micelle and liposome carriers are discussed in this review.
Nanocarriers
Nanocarriers are smaller than one micron in size and typically have the advantages of longer persistence in systemic circulation and greater diffusivity through tissue. By virtue of their small size, one or more nanocarriers can be taken up by a single cell to deliver the drug payload. These advantages are often tempered, however, by relatively low ultrasound responsiveness and, as will be discussed later in this review, recent innovations have combined nanocarriers with larger, more ultrasound-responsive microbubble structures.
Micelles
Composition and Structure
Micelles are formed by amphiphilic molecules, such as lipids or amphiphilic di-block or tri-block copolymers. The amphiphlic molecules self-assemble when exposed to aqueous media to form a hydrophobic core surrounded by a hydrophilic corona (Fig. 1). Association of molecules typically is mediated through hydrophobic forces, although electrostatic attractive forces may also lead to self-assembly. Micelles are typically 10–100 nm in diameter, depending on material composition, and are capable of storing hydrophobic drugs within their core to form so-called “swollen micelles” [34].
Figure 1.
Micelles comprise amphiphilic molecules that self-assemble to form a hydrophobic core, amenable to loading of hydrophobic drugs, and a hydrophilic corona. A) Micelles can be composed of PEGylated phospholipids, such as 1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-[polyethylene oxide] (DSPE-PEO). B) Other micelles are commonly composed of amphiphilic di-block and tri-block copolymers with hydrophobic units, such as poly(lactic acid) (PLA), linked to hydrophilic units, such as poly(ethylene oxide) (PEO).
The main advantage of micelles is their relative ease of fabrication. Above the critical micelle concentration (CMC), they self-assemble in aqueous solution, often with the hydrophobic drug spontaneously partitioning into the nonpolar environment of the micelle core. Micelles also beak apart and release the drug when diluted below the CMC. The CMC is a complex property that depends not only on the structure of the amphiphile, but also the local microenvironment. In blood, other amphiphiles, association colloids and biomembranes are present that may alter the chemical potential gradient between monomers in the micelles and those in the milieu, thus shifting the CMC to a higher value. Consequently, micelles that are stable in saline may be found to be unstable when introduced into the bloodstream, where they disassemble and prematurely release their cargo drug.
One may avoid premature micelle disassembly by the use of highly hydrophobic amphiphiles that have a very low CMC, even in blood and tissue. Micelles made from low-CMC compounds may be difficult to generate by simple film hydration and sonication methods. Instead, one may start with an organic co-solvent, which dissolves the drug and amphiphiles as monomers, and then add water in a controlled fashion to promote self-assembly of drug-loaded micelles that then become kinetically trapped as the co-solvent is exchanged with water. This process can be done with remarkable precision using techniques such as “nano-flash precipitation” [35].
Interactions with Ultrasound
Micelles have been shown in numerous studies to release their drug cargo when exposed to ultrasound [36–39]. Experimental studies have correlated drug release with the onset of ultrasound-induced cavitation. Husseini et al. [40] demonstrated that lower ultrasound frequencies (20 kHz) achieved the highest levels of release of the anti-cancer agent doxorubicin (DOX), and the efficiency of drug release decreased with increasing frequency up to 90 kHz. Similar results were achieved using pluronic micelles stabilized by an interpenetrating network of poly(N,N-diethylacrylamide) that prevented destabilization upon dilution [41]. Husseini et al. [42] provided further evidence for the role of cavitation by correlating micelle drug release with subharmonic acoustic emissions. Marin et al. [43] found that low-frequency ultrasound (20–100 kHz) was more effective at releasing DOX from micelles. For example, 10% release required only 0.05 W/cm2 and 20 kHz, but as much as 2.4 W/cm2 at 67 kHz, and 7.2 W/cm2 at 1 MHz. More recently, DOX release was monitored in pluronic micelles during 70-kHz ultrasound exposure by measurement of the fluorescence emission, which becomes quenched when the DOX molecules enter the aqueous medium [44]. Interestingly, rapid DOX re-uptake into micelles was observed immediately following ultrasound exposure, indicating that drug release is a reversible process [44] (Fig 2). Enhanced micellar delivery at lower frequency, and hence higher MI, indicates that inertial cavitation is an important mechanism in ultrasound-triggered release.
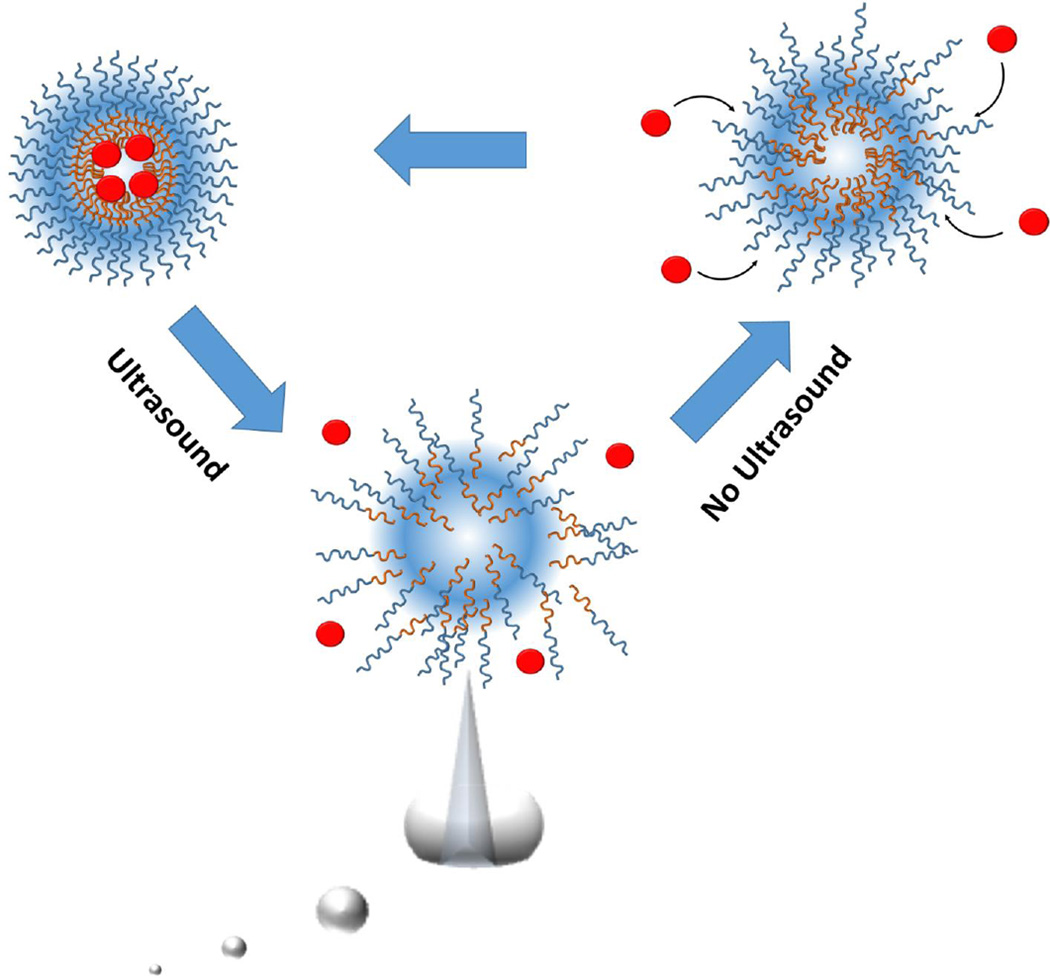
Figure 2.
Ultrasound-induced cavitation can facilitate micelle disassembly and drug release. After ultrasound is removed, rapid reincorporation of the drug may occur as the micelles reform.
Mohan et al. [45] demonstrated that ultrasound can trigger the release of DOX from micelles taken up into the cell cytoplasm. Deprotonated DOX (characterized by increased hydrophobicity and more efficient micellar encapsulation) used in this study demonstrated poor nuclear localization following intracellular uptake in cultured cells. The application of ultrasound (2 W/cm2 at 3 MHz) increased both intracellular uptake and nuclear localization of micelle-loaded DOX, as determined by fluorescence intensities in the cytosol and nuclear structures from confocal imaging.
Hasanzadeh et al. [46] used a novel dual-frequency sonication approach to release encapsulated DOX from pluronic P-105 based micelles. In this study, low frequency (27.7 kHz at 0.02 and 0.04 W/cm2) ultrasound was used in combination with higher frequency ultrasound (3 MHz at 1 and 2 W/cm2). Hasanzadeh et al. also demonstrated significantly higher (~1.5-fold) levels of DOX release using simultaneous dual frequency application compared to either frequency alone, suggesting the mechanisms of release using high and low frequency ultrasound are synergistic. Sonication also demonstrated improved intra-tumoral DOX uptake in vivo compared to free DOX and micelle-encapsulated DOX without ultrasound. However, single frequency sonications were not performed as comparison. It should be noted that dual-frequency sonication resulted in increased local mild-hyperthermia (albeit below 42° C) during sonication, and thermal mechanisms may have also been at play.
Recent Progress
Recent work has focused on combining biochemical (ligand-receptor) cell targeting techniques with ultrasound-mediated drug release in order to maximize the TI. For example, Husseini et al. [44] recently explored the effects of cavitation on DOX release from folate-conjugated micelles. This approach is promising, but more in vitro and in vivo studies must be done to further explore the advantages of receptor-targeted micelles with ultrasound.
Recent progress has also been made by exploring new ultrasound-cleavable micelle compositions and structures. Wang et al. [47] utilized a novel poly(ethylene oxide)-block-poly(2-tetrahydropyranyl methacrylate) (PEO-b-PTHPMA) copolymer to form ultrasound responsive micelles with weaker chemical bonds meant to be more sensitive to both pH and temperature. The thermo-sensitivity of PEO-b-PTHPMA polymers was explored previously by Pelletier et al. [48], who demonstrated that PEO-b-PTHPMA micelles are disrupted following thermally induced hydrolysis of the 2-tetrahydropyranyl methacrylate (THPMA) side chains, converting PTHPMA to poly(methacrylic acid) PMAA and increasing the overall polarity (and hydrophilicity) of the polymer. The resulting PMAA-PEO diblock polymers were more soluble, leading to rapid micellar destabilization. Wang et al. [47] used the same micelle formulation to demonstrate that hydrolysis and disruption of the side chains could be achieved efficiently with higher frequency ultrasound exposure (1.1 MHz).
Liposomes
Composition and Structure
Liposomes are one of the most commonly used carriers for in vivo drug delivery due to their inherent biocompatibility and versatility [49]. These drug carriers are typically 100–200 nm in diameter and contain an aqueous core surrounded by a self-assembled lipid bilayer membrane. The phospholipid bilayer of the liposome mimics the cell membrane and is amenable to loading of lipophilic drugs. Alternatively, hydrophilic molecules can be loaded into the aqueous core. Liposomal nanocarries have been used for over five decades as drug delivery systems [49] and are particularly useful in cancer therapies for the delivery of insoluble drugs, such as DOX [50]. Encapsulation of drugs into liposomes increases TI by increasing blood circulation half-life, thus taking advantage of passive targeting through the enhanced permeability and retention (EPR) effect of solid tumors with leaky vasculature [51]. Current research is focused on further increasing TI by the use of ultrasound targeting, which can stimulate liposomes that have accumulated in the tumor and are passing through tumor vasculature to release their drug cargo.
Interactions with Ultrasound
Numerous studies have demonstrated that ultrasound can trigger release of drugs from liposomes [52], although the predominant underlying mechanism of drug release is not completely understood. It is likely that several mechanisms are at play, and the dominant mechanism of drug release depends on the particular ultrasound parameters and the chemical composition of the liposomes. Potential mechanisms for drug release from liposomes include cavitation, thermal effects and acoustic streaming, and these mechanisms may not be completely independent (Fig. 3).
Figure 3.
Liposomes for ultrasound-triggered drug delivery. A) Liposomes comprise a phospholipid bilayer membrane and an aqueous core. Drugs, such as doxorubicin, can be loaded into the hydrophobic bilayer and then released through several ultrasound mechanisms: B) Drug release can be achieved by ultrasound-induced cavitation, which involves the generation and violent collapse of one or more gas bodies near the liposome. Microbubble nucleation and growth may also occur within the lipid bilayer of the liposome due to lower energies required to disrupt intermolecular van der Waals forces between lipid chains. C) Focused ultrasound can be used to increase the local fluid temperature to promote drug release from temperature-sensitive liposomes. D) Acoustic radiation-force streaming can increase the frequency of particle collisions and thus facilitate material transfer.
Cavitation involves the generation and sudden collapse of a vapor cavity at or near the lipid bilayer membrane of the liposome. For drug delivery, the cavitation event must be sufficiently violent to disrupt the membrane and release the liposomal contents. Recently, Krasovitski et al. [53] described how cavitation could nucleate in the bilayer membrane owing to the lower intermolecular cohesion forces between lipid acyl chains, which have relatively weak dispersion forces in comparison to the strong hydrogen-bonding forces of water.
Experimental research has suggested that cavitation induced by low-frequency ultrasound can destabilize liposomes to promote release of internal cargo [54]. Schroeder et al. [55] used low-frequency (20 kHz) ultrasound exposure to demonstrate triggered release of three different encapsulated drugs (methylprednisolone hemisuccinate, doxorubicin and cisplatin). Ultrasound exposure periods up to 180 seconds demonstrated efficient release (~80%) of drug from liposomes, independent of the drug or method of drug loading. This result was attributed to permanent destabilization of ~20% of liposomes and the formation of transient pores in the remainder. Somaglino et al. [56] recently demonstrated that cavitation plays a strong role in the release of DOX from liposomes. In order to avoid significant temperature changes from the ultrasound exposure and isolate the effects of cavitation, the authors utilized high-frequency (1 MHz) pulsed ultrasound to sonicate DOX-carrying liposomes. The inertial cavitation dose (CD) was measured from a broadband acoustic signal and free radical formation. DOX release was tested from two different liposome formulations (Caelyx® and Epi® liposomes), and both showed a high correlation between %DOX release and CD. The findings implied that CD was a better predictor of drug release than total exposure time, although follow-up studies demonstrated that this technique is more complicated in vivo 57]. Research by Evejen et al. demonstrated that controlling CD in vivo can facilitate drug release from intra-tumorally injected liposomes via non-thermal mechanisms [58].
While cavitation is thought to be the dominant mechanism of liposomal drug release, several reports have illustrated that thermal effects could also play a role. The original liposomal carriers (e.g., Doxil™) were not designed with ultrasound-triggered release in mind. However, novel liposome materials have been developed to exploit the thermal effects of focused ultrasound in order to promote a less violent mechanism of drug release. The permeability of liposomes can be enhanced by increasing local temperature above the lipid main phase transition temperature (Tm) [59,60]. Needham et al. [61] developed a temperature-sensitive liposome (TSL) formulation wherein the Tm was just above physiological temperature, producing drug release with mild hyperthermia. In this study, the authors demonstrated more efficient DOX release as phospholipids in the bilayer transitioned from the gel-like (ordered packing) condensed state to the more fluidic (disordered packing) state. The proposed mechanism was attributed to highly permeable boundary defects arising during the phase transition. The authors found highly efficient and reproducible xenograft tumor regression compared to traditional temperature-insensitive liposomes.
An investigation of the efficacy of TSLs was recently performed by Gasselhubber et al. [62], who developed a multi-compartment mathematical model describing intracellular accumulation of DOX in tumors with respect to time and release rates from TSLs. The model was used to determine the optimal release rate constants of DOX from TSLs (and non-TSLs) in order to maximize intracellular DOX uptake in tumors while minimizing systemic exposure of the drug. Intracellular uptake and biodistribution of highly responsive TSLs with rapid release rates in response to hyperthermia (minutes) and less responsive TSLs (hours) were compared with commercially available stealth liposomes (Doxil™, with release rate constants on the order of weeks) and free DOX. The optimal release rate constant was estimated to be ~45 min to achieve maximum intracellular uptake and drug efficacy. This study demonstrated that control over drug release timing is a critical aspect of drug delivery and is a necessary part of a rational design approach to optimize chemotherapeutic treatments. While this study did not contain in vivo work, validation of the model was based on data from a preceding in vivo study by Kong et al. [63. Hyperthermia was not induced by ultrasound in these studies, but several subsequent studies have demonstrated that ultrasound-induced hyperthermia can effectively cause release of DOX from TSLs. For example, Dromi et al. [64] used pulsed high-intensity focused ultrasound (HIFU) to demonstrate that TSLs, similar to those used by Needham et al., produce more rapid drug release and local DOX delivery to tumors compared to traditional temperature-insensitive liposomes. Paoli et al. [65] showed the importance of tracking biodistribution of both the lipid shell and drug contents in determining the most effective lipid formulation. These studies indicated that local ultrasound-induced hypothermia is an effective method for controlling drug release.
Although the mechanisms governing ultrasound-mediated release have been largely attributed to cavitation and thermal effects [66], more recent research has demonstrated that acoustic streaming can also achieve efficient drug release from liposomes. Oerlemenas et al. [67] encapsulated hydrophilic (fluorescein) and hydrophobic (Nile Red) dyes into TSLs and traditional liposomes and evaluated the release kinetics under 1.5-MHz focused ultrasound. Interestingly, the authors did not observe release of Nile Red dye from the liposomes for either TSLs or traditional liposomes when they were subjected to increased temperature above the lipid Tm. However, Nile Red release was observed in both liposome formulations when exposed to high-intensity focused ultrasound. Release of Nile Red in this case was attributed to non-cavitational and non-thermal effects of ultrasound. The authors speculated that radiation force induced collisions of particles during ultrasound exposure could be responsible for the release of Nile Red from the lipid bilayer. This latest study provides new insight into the mechanisms of hydrophobic drug release from lipid bilayers.
Overall, ultrasound-triggered drug release of chemotherapeutic compounds from liposomes has been clearly established as feasible, although the dominant mechanisms remain unclear. It is likely that several mechanisms are simultaneously at play, making it difficult to isolate and study the specific phenomena in vivo. Still, the development of novel ultrasound-responsive liposomes holds great promise in targeted therapy and will likely be of great importance in future clinical work.
Recent Progress
Research elucidating the mechanism of drug release from liposomes has led to the development of so-called “sonosensitive” materials that could be utilized for more efficient release of drugs during ultrasound exposure. Evjen et al. [68] demonstrated that sono-sensitivity of liposomes could be enhanced by incorporating 1,2-distearoyl-sn-glycero-3-phosphatidylethanolamine (DSPE) into the lipid bilayer. The authors speculated that the inclusion of DSPE lipids promotes the induction on local defects and polymorphic rafts, thus decreasing their stability under ultrasound application. The results of the study demonstrated that increasing DPSE concentration could improve the efficiency of DOX release by 7-fold compared to a more traditional liposomal DOX formulation.
Summary
Polymeric and lipid nanocarriers have shown great promise in research and clinical settings for the treatment of cancer. Thermo-responsive and shear-responsive drug carriers have been developed and shown to effectively trigger drug release and improve therapeutic efficiency. The drawback to this approach is that systemic targeting of the drug carriers to the desired tissue cannot be easily achieved. Ultrasound-responsive drug carriers are by their nature less stable than conventional nanocarriers, and they may easily lose their contents en route to the target tissue. Those circulating agents that retain their cargo only remain in the focal region of ultrasound for short periods of time (seconds), whereas as the typical exposure times required for ultrasound-triggered release are much longer (minutes). Thus, the main mechanism of tissue targeting in vivo is still passive extravasation of the circulating agents into desired tissue, namely the EPR effect in tumor targeting. Alternate methods of drug release from circulating agents are required for more advanced drug targeting. In the following section of this review, we discuss how this can be achieved using microbubbles.
Microbubbles
Composition and Structure
Microbubbles are commonly used as vascular probes for ultrasound imaging, and they can be used as drug carriers as well [8,18,20,69]. Microbubbles comprise a gas-filled core and stabilizing shell of lipid, polymer and/or protein [70]. Unlike lipid and polymer based nanocarriers, microbubbles are on the micron scale, ranging 1–10 µm in diameter. Due to their larger size, systemically delivered microbubbles do not passively extravasate. Instead, they remain in circulation until they dissolve or are actively cleared by the mononuclear phagocyte system (MPS), with most uptake in the lung, liver and spleen [71,72].
Interactions with Ultrasound
Microbubbles are uniquely suited for ultrasound-triggered drug delivery. The compressible nature of the gas core allows the microbubble to volumetrically oscillate in response to the compression and rarefaction portions of the ultrasound wave [20]. Microbubble oscillation causes an acoustic backscatter that can be detected by clinical ultrasound scanners, which makes them excellent ultrasound probes for monitoring blood perfusion by ultrasound imaging. Due to their ability to generate a micro-scale mechanical response in a millimeter-scale ultrasound field, the bioeffects of ultrasound exposure are greatly focused and magnified by the presence of microbubbles. For example, the energy required to generate cavitation is lowered by microbubbles, which themselves act as cavitation nuclei [16,73]. Microbubbles facilitate cavitation-related phenomena, such as temperature rise and free radical formation [16,18]. Additionally, microbubble volumetric oscillations enhance the generation of shear forces and acoustic streaming [20]. The mechanical response of microbubbles to ultrasound can also promote physiological changes that improve extravasation of circulating drugs into target cells and tissues [8,18,70,74]. The mechanisms of microbubble permeabilization of the endothelial vasculature have been recently reviewed in more detail [8]. The mechanisms include increased permeability of the cell membrane by violent collapse of the microbubbles (inertial cavitation) or mechanical agitation of a stably oscillating microbubble (stable cavitation) near the boundary of the cell or vessel wall [20] (Fig. 4). Ultrasound can also translate microbubbles in the direction of the propagating ultrasound wave through enhanced acoustic radiation forces [21,24]. Such radiation forces can be applied using a clinical ultrasound scanner [75]. Through acoustic radiation forces, microbubbles may also squeeze through the endothelium and tunnel through soft tissue [76,77], possibly increasing the deposition of shell-loaded materials beyond the vasculature.
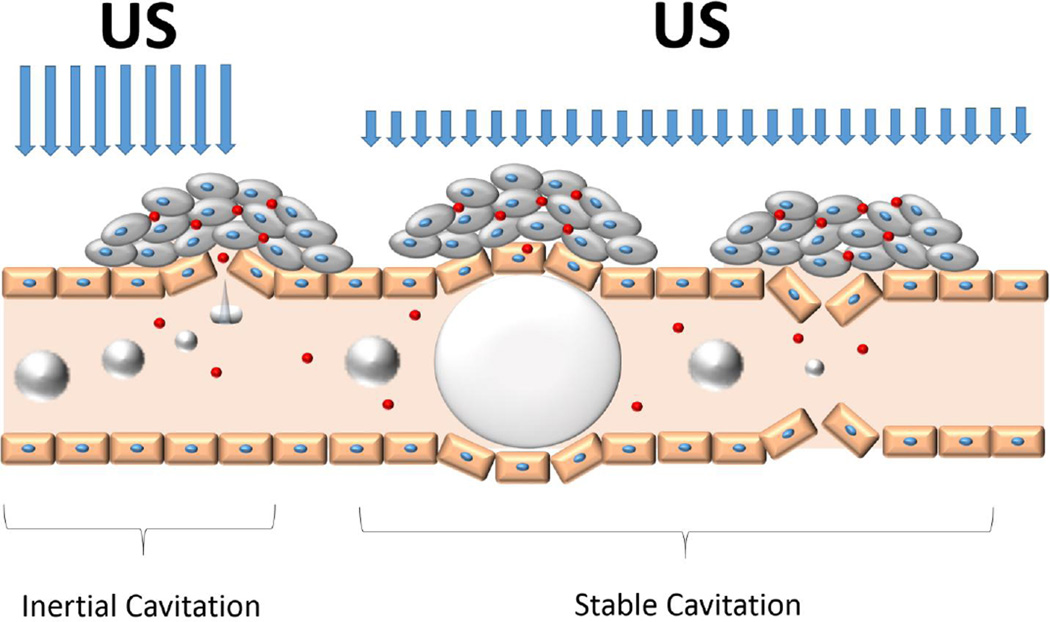
Figure 4.
Microbubble interactions with ultrasound. Extravasastion of circulating drugs may occur through inertial cavitation events at high mechanical index, causing disruption of the endothelial lining. At lower ultrasound pressures, volumetric oscillations of the microbubble can stretch or distend of the blood vessel [124,125], which also may facilitate endothelial disruption and drug extravasation. A more detailed description of microbubble interactions with blood vessels can be found in Sirsi et al. [19].
Recent Progress
Microbubbles were originally designed for ultrasound imaging applications. Even without physically attaching drugs to the surface, numerous studies have demonstrated that the mechanical response of microbubbles to ultrasound can promote extravasation and localized delivery of circulating agents [78,79]. However, it is generally accepted that incorporation of a drug payload onto the microbubble will provide greater control over drug release and deposition and therefore an increased TI. Here, we discuss microbubble formulations developed to improve hydrophobic drug loading. Two distinct classes of microbubbles will be discussed, namely soft-shelled and hard-shelled microbubbles. Both classes have distinct advantages and disadvantages in targeted drug delivery.
Soft-Shelled Microbubbles
The term “soft-shelled microbubbles” refers to microbubbles comprising a thin surfactant shell material, such phospholipids or proteins. The thin, flexible shell makes the microbubble highly sensitive to acoustic waves. At low amplitudes, the microbubbles stably oscillate in volume (stable cavitation). At high amplitudes, microbubbles undergo rapid expansion and contraction, which results in violent microbubble destruction (inertial cavitation) that has sufficient energy to permeabilize surrounding tissue. Because of the thin shell, drug loading in soft-shelled microbubbles is limited. Improved drug loading can be accomplished, however, by physical attachment to the surface, and several research groups have used this approach to generate drug-loaded, phospholipid-coated microbubbles [69] (Fig. 5).
Figure 5.
Loading of lipophilic drugs onto phospholipid microbubbles. Drug loading can be achieved by A) incorporating a thin layer of hydrophobic oil beneath the phospholipid monolayer shell, B) intercalating the drug between phospholipids within the monolayer, C) tethering the drug to the phospholipid head group, or D) loading the drug into nanocarriers (such as liposomes) tethered to the microbubble surface.
The earliest work on drug-loaded soft-shelled microbubbles was described by Unger et al. [80], in what the authors called “acoustically active lipospheres” (AALs). AALs were formulated by mechanical agitation of liposomes, paclitaxel-carrying emulsion and a fluorocarbon gas. The paclitaxel was emulsified in soybean oil, which putatively became trapped beneath the phospholipid monolayer at the gas-liquid interface. Shielding the paclitaxel in this way reduced drug exposure to the plasma serum. Targeting AALs with RGD peptides was later described by Tartis et al. [81]. This study was one of the first to combine the use of drug-loaded microbubbles with both biochemical targeting and ultrasound targeting. The authors used acoustic radiation force to promote vascular adhesion and “break” pulses (high intensity ultrasound pulses) in order to destroy the microbubbles and release the shell-encapsulated drug in the region of ultrasound application.
More recent work on DOX loading onto microbubbles was described by Tinkov et al. [82]. Instead of encapsulating an oil layer beneath the shell, loading was achieved by simply re-suspending a dried mixture of phospholipids in an aqueous suspension containing DOX. The liposome suspensions were emulsified with a hydrophobic gas to form DOX-loaded microbubbles. Based on previous literature detailing the interactions between lipophilic (and slightly positive) DOX molecules with anionic lipids [83,84], the authors reasoned that DOX would be incorporated into the phospholipid shell of the microbubble. An interesting result from this study was that DOX loading in the shell caused a fluidizing effect that lowered the Tm of the lipids. Targeting with DOX-loaded microbubbles showed a 12-fold increase in DOX uptake by tumor tissue with the application of ultrasound [82]. Ultrasound-triggered drug release of DOX slowed tumor growth significantly without showing signs of toxicity.
Instead of relying on electrostatic uptake of DOX in the microbubble shell, Wu et al. [85] chemically combined DOX to pluronic F68 triblock polymers, a process described earlier by Zhao et al. [86], and formulated Tween-based microbubbles along with a lipid-conjugated bFGF targeting peptide, which were developed by Terada et al. [87]. The authors claimed 95% incorporation of the loaded DOX into the microbubble shell. Preliminary in vivo data demonstrated that bFGF-labeled, DOX-loaded microbubbles under ultrasound exposure slowed the growth of xenograft tumors by ~25% compared to untreated controls, thus demonstrating that DOX conjugation to pluronic F68 is an effective method of incorporating DOX into a microbubble shell.
Recently, our research group described the use of natural lung surfactant extract (Survanta®, Abbott Nutrition) as a microbubble shell material to improve drug payload and delivery [88]. Pulmonary surfactant extracts such as Survanta® contain hydrophobic surfactant proteins (SP-B and SP-C) that facilitate lipid folding and retention on lipid monolayers [89]. In this study, we showed that Survanta-based microbubbles exhibit wrinkles and increased lipid retention on the microbubble surface in the form of surface-associated aggregates (Fig 6). Consequently, drug payload was increased by over 2-fold compared to synthetic lipid-coated microbubbles lacking SP-B and SP-C. Survanta-based microbubbles were found to be highly echogenic and demonstrated improved targeted deposition of a model lipophilic drug in vitro.
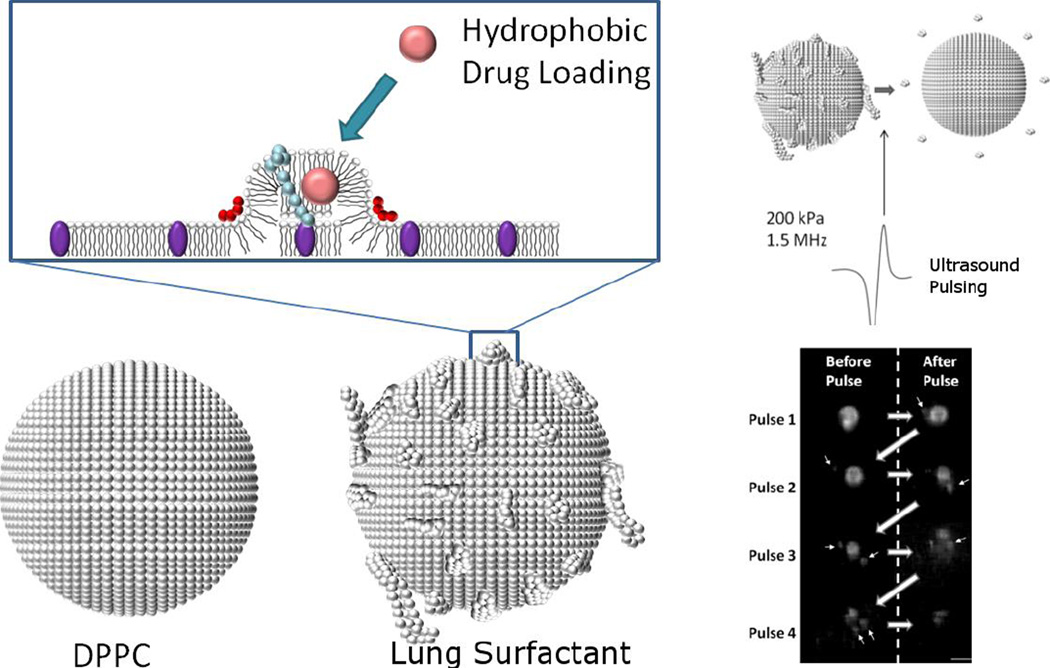
Figure 6.
A) Lung surfactant microbubbles with excess surface lipid buildup are more amenable to hydrophobic drug loading compared to synthetic microbubble formulations (such as DPPC:DSPE-PEG) that do not exhibit surface lipid retention. B) Fluorescence imaging demonstrating that excess lipid bulk can be shed by single acoustic pulses (shed lipid marked by arrows) to release model lipophilic drug (DiO) from the microbubble shell. Reprinted with permission [88].
Hard-Shelled Microbubbles
The term “hard-shelled microbubbles” refers to the use of cross-linked or entangled polymers that from a thicker and less compliant microbubble shell. The thicker shells provide higher stability and drug payload in comparison to soft-shelled microbubbles. However, hard-shelled microbubbles also show lower ultrasound responsiveness in comparison to lipid or protein-shelled microbubbles [90]. At low ultrasound pressures (<1 MPa), hard-shelled microbubbles typically do not oscillate due to a dampened acoustic response. At high acoustic pressures (>1 MPa), however, the microbubble shell cracks, and the encapsulated gas extrudes and escapes into the surroundings. Gas escaping rapidly from a fractured microbubble shell could potentially propel the microbubble towards the vasculature wall or allow extravasation of the contrast agent, as suggested by Mehier-Humbert et al. [91].
Eisenbrey et al. [92] were the first to evaluate the potential of hard-shelled poly(lacticacid) microbubbles for the encapsulation and delivery of DOX. In this study, three different methods of DOX loading were evaluated to determine payload and release kinetics, namely 1) DOX loading into the microbubble shell, 2) DOX loading by surface adsorption onto pre-fabricated microbubbles, and 3) DOX loading by absorption during microbubble fabrication. The authors showed a high loading efficiency of DOX when absorbed into the shell during microbubble fabrication, presumably while the microbubble shell was still hardening. However, a rapid, burst release of DOX was observed for these microbubbles prior to ultrasound triggering. Loading of DOX into the microbubble shell showed high loading efficiency and better retention of DOX in solution, and was thus chosen as the preferred method of loading in follow-up experiments. Eisenbrey et al. [93] recently reported that increasing the ultrasound exposure time dramatically reduced the size of the particles, presumably due to fragmentation of the shell and release of the gas core. Cochran et al. [94] utilized the same DOX-loaded microbubbles to demonstrate significantly higher DOX accumulation in hepatocellular carcinoma tumors implanted in rats, compared to free DOX alone. The authors attributed the improved DOX delivery to the formation of small polymer “shards” created during ultrasound fragmentation of the shell.
Recently, Dicker et al. [95] described a method of encapsulating soft-shelled lipid microbubbles within polymer microcapsules for improved microbubble stability in contrast imaging applications. In this study, the authors demonstrated that multiple small 1–2 µm lipid bubbles could be loaded into larger 3–5 µm poly(lactic acid)-based microcapsules. This dual polymer and lipid system combines the advantages of high drug payloads with echogenic properties of soft-shelled microbubbles. The authors of this study demonstrated more effective release of calcein from the microbubbles-loaded capsules compared to unloaded capsules using ultrasound as a trigger. This study showed that co-encapsualtion techniques may be beneficial for maximizing drug payloads in therapeutic drug delivery applications.
Nanocarrier-Microbubble Hybrids
Several research groups have proposed the development of nanocarrier-microbubble hybrids, wherein drug-containing liposomes, micelles or other nanoparticles are physically attached to the microbubble surface. These hybrids take full advantage of the high drug loading capacity of the nanocarriers and the systemic targeting capability and vascular permeabilizing effect of microbubbles. For example, Kheirolomoom et al. [96] used biotin-avidin linkage to attach liposomes to the surface of microbubbles. Liposomes containing a hydrophobic dye were loaded at high efficiencies (103 to 104 liposomes per bubble for 200-nm and 100-nm liposomes, respectively). The calculated increase in available surface area for drug loading would be 34-fold higher, without significantly increasing the diameter of the microbubble drug carrier. This study utilized fluorescent cholesterol as a model drug to demonstrate higher drug deposition from liposome-loaded microbubbles in vitro, compared to fluorescent cholesterol loaded directly in the microbubble shell. Lentacker et al. [97] used a similar biotin-avidin linkage system to investigate the mechanism of release and intracellular uptake of DOX-loaded liposomes attached to microbubbles.
Recently, Fan et al. [98] developed a novel DOX-loaded microbubble containing super-paramagnetic iron oxide (SPIO) nanoparticles for dual modality imaging and improved image-guided drug delivery. DOX was loaded into the microbubble shell prior to microbubble formulation, using the same procedure described by Tinkov et al. [82]. Hydrophobic SPIO nanoparticles, which are used as MRI probes, were loaded into the shell during microbubble formulation. The authors successfully used focused ultrasound to trigger DOX and SPIO release from circulating microbubbles to brain glioma tumors. The authors also demonstrated that the delivery of SPIO to brain tumors was improved using magnetic targeting in combination with focused ultrasound. However, the improvement in DOX delivery using magnetic targeting was not measured. The same group also developed hard-shelled PLA microbubbles for the encapsulation of DOX and iron oxide [99], and they demonstrated a higher rate of apoptosis in tumor lymph models with exposure to ultrasound.
One very promising application of magnetic nanoparticle-loaded microbubbles was recently demonstrated Stride et al. [100,101], who showed that targeting in flow can be significantly increased by simultaneous application of a magnetic field and ultrasound. Interestingly, their magnetic microbubbles experienced a force toward the magnetic source that was stronger than estimated in a free-body analysis, suggesting a coupling mechanism that may be utilized to enhance the targeting capability of this system [102,103]. Our research group recently showed that coupling of plasmonic gold nanoparticles onto microbubbles can enhance the photoacoustic signal compared to the nanoparticles alone, thus opening the possibility of dual modality ultrasound/photoacoustic imaging and photothermal therapy [104].
Microbubble-loaded hydrogels for targeted drug delivery
The field of ultrasound-triggered drug release has focused mainly on targeting of systemically circulating agents. However, methods have been developed for implantable drug release systems that can be triggered using ultrasound [105–107] (Fig 7.). For example, Epstein-Barash et al. [108] developed an ultrasound-triggerable hydrogel for in vivo drug release. This system comprised a novel injectable Dextran-based hydrogel with dye-loaded liposomes and microbubbles. This material was used as an implant for on-demand, localized drug delivery via pulsed ultrasound application. The putative mechanism for this system involves enhanced convection and shear forces owing to the mechanical response of microbubbles in the ultrasound field, which promotes drug release. In vivo experiments using trypan blue dye demonstrated a 2-fold increase of dye release into the mouse skin with the application of a single ultrasound pulse. Microbubble-loaded hydrogels are a unique implantable material capable of serial applications of ultrasound-targeted drug delivery.
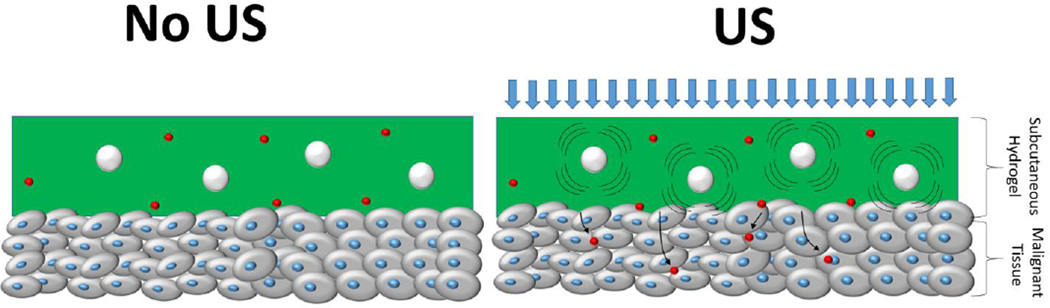
Figure 7.
Schematic of a microbubble-loaded hydrogel. Microbubble volumetric oscillations in the hydrogel facilitate release of liposomal drugs by increasing local convection and shear forces.
Phase-Change Agents
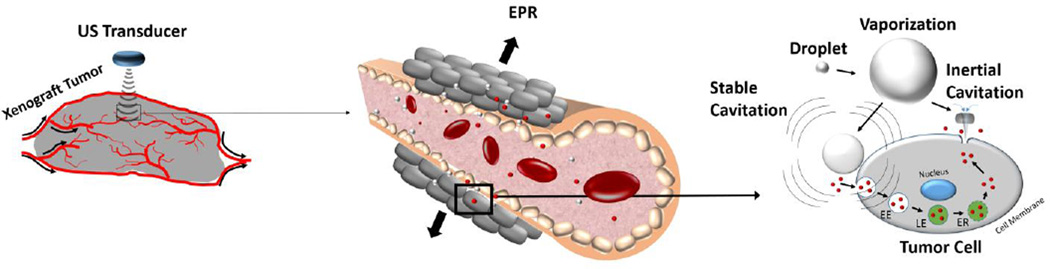
Microbubble contrast agents are orders of magnitude more responsive to ultrasound stimuli than nanocarriers. However, one of the main drawbacks is that microbubbles are too large to extravasate and reach tissue beyond the vasculature. Phase-change agents represent a novel class of materials that have been developed to combine the advantage of small size for nanocarriers to penetrate into tissue and cells with the excellent acoustic properties of microbubbles. Phase-change agents use fluorocarbons that remain liquid at room temperature and body temperature, and then spontaneously vaporize upon application of ultrasound. Thus, the particles can be introduced systemically on the nanoscale, where they extravasate into tissue adjacent to leaky vasculature. They can then be vaporized to form microbubbles that are acoustically active to enhance drug delivery (Fig. 8) or enhance tissue ablation in HIFU therapies [109,110]. Importantly, the droplet cores can be loaded with hydrophobic drugs, such as DOX or hydrophilic compounds for drug delivery [111]. These materials have been developed as theranostic agents that have shown excellent potential as systemic drug carriers. For recent reviews on phase-change agents in imaging and therapy, see Rapoport [112] and Sheehan and Dayton [113].
Figure 8.
Schematic of a phase-change agent mediated drug delivery to tumor tissue. Circulating phase-change agents (white) and drugs (red) are small enough to extravasate into tumor tissue via the EPR effect. Following extravasation into tumor tissue, phase-change agents can vaporize into microbubbles and promote intracellular uptake of drugs through inertial cavitation (sonoporation of the membrane) or stable cavitation (e.g., stimulation of endocytosis).
The concept of phase-change agents as drug carriers was pioneered by Rapoport et al. [114], who used polymeric micelles in order to encapsulate liquid perfluoropentane (PFP) containing DOX. Polymer composition (PEG-PLLA or PEG-PCL) and polymer-to-liquid ratio were varied to control nanoemulsion size. For this system, increasing the temperature to 37°C caused the PFP nanodrops to vaporize into larger bubbles (mm size). Interestingly, heating and cooling cycles showed rapid growth of larger bubbles by coalescence. It was proposed that hypothermia targeted to the tumor region could generate larger microbubbles formed by coalescence of the vaporized nanodrops. The authors demonstrated feasibility of using polymer-stabilized PFP nanodroplets to deliver DOX to xenograft tumors, and they showed that tumor growth could be arrested by this method. This study was the first to demonstrate the potential of phase-change agents as effective ultrasound-triggered drug delivery vehicles. A follow-up study by Gao et al. [115] demonstrated that cavitation of the microbubbles following intra-tumoral uptake could effectively enhance intracellular DOX uptake into tumor cells as well.
This earlier work on phase-change agents for chemotherapeutic drug delivery was highly innovative, but difficulties in controlling the onset and rate of vaporization, microbubble size and subsequent coalescence have complicated clinical translation. More recent work by Rapoport et al. [112,116] has focused on novel echogenic perfluoro-15-crown-5-ether (PFCE) nanodrops that exhibit long circulation lifetimes and greater control over vaporization and microbubble formation. In this system, droplet structures are maintained at body temperature allowing them to extravasate into tumor tissue. Ultrasound is then used to trigger nanodrop vaporization following accumulation into tumor tissue. PFCE nanodrops can also be used as MRI contrast agents for dual modality imaging. In the most recent work, tumor regression was achieved with paclitaxel-loaded PFCE droplets [116]. Due to the acoustic impedance mismatch between PFCE and surrounding tissue, the droplets could be imaged with ultrasound in circulation, allowing for the development of image-guided drug delivery. Similar approaches to dual modality imaging and therapy are being explored with vaporizable nanodrops, such as the development of Gd-coated PFC nanodrops for MR imaging and ultrasound-mediated tissue ablation [117], and image-guided tagging of tissue with fluorescent markers [118].
A similar study was reported by Phillips et al. [119], who used perfluorocarbon (PFC) nanodrops made from a mixture of volatile decafluorobutane and less-volatile dodecafluoropentane at a 1:1 ratio. The mixture of PFCs was stable at room temperature for storage and required low energies of high-intensity focused ultrasound to cause droplet vaporization in the body. Additionally, the droplet sizes were reported to be 100–300 nm in size, small enough to extravasate into tumor tissue. The droplets were reported to be stable up to 48 hours.
Lin et al. demonstrated that PFC nanodrops (~100 nm) could be incorporated within liposomes (~200 nm) to form liposome-droplet hybrids (termed eLiposomes) with high DOX loading and effective DOX release [120]. DOX release from the eLipososmes was evaluated using low-frequency ultrasound application (20 kHz at 1 W/cm2) and high-frequency ultrasound application (1–3 MHz at 1–5 W/cm2). The release of DOX from eLiposomes at both low and high-frequencies was higher compared to liposomal DOX without PFC, although DOX release was far more rapid with low-frequency vs. high-frequency sonication (80% vs. 15% release after 60 seconds). The results from this study show that PFC nanodrop loading into liposomal DOX may be an effective tool for ultrasound triggered release, but effective phase transition of the PFC may require low-frequency sonication.
Kagan et al. [121] demonstrated that phase-change agents can be utilized as an ultrasound-triggered propulsion system to direct payload delivery in vivo at high velocities deep within the tissue. By loading perfluorocarbon nanodrops into conically shaped micron-sized structures, the authors demonstrated that ultrasound-triggered vaporization of the droplets could cause linearly directed propulsion (similar to the firing of a bullet through a barrel of a gun) at high velocities (>6 m/s). This method of ultrasound triggered drug delivery utilizes vaporization of droplets as a propulsion system that could be useful in a wide variety of in vivo applications that might require payloads to be delivered well beyond the vascular space.
Innovations have also been made regarding methods of formulating phase-change agents. Sheeran et al. [122] recently described two methods for generating low-boiling point fluorocarbon nanodrops. In the first method, perfluorobutane (PFB), which is normally a gas at room temperature, was liquefied and emulsified to form lipid-coated microbubbles. Remarkably, these lipid-coated PFB nanodrops were stable and did not vaporize upon heating to room temperature and body temperature. This hysteretic behavior has yet to be fully explained. Sheeran et al. [122,123] also showed how to generate nanodrops by condensing gas-filled microbubbles through cooling and pressurization. This elegant method allows one to tailor the composition and size distribution of the nanodrops by first tailoring these properties in the precursor microbubbles. Once again, these nanodrops remained in the liquid form at room temperature and body temperature, but were converted to microbubbles by sonication with a relatively low mechanical index. Nanodrop formation by microbubble condensation offers a fountain of opportunities for new formulations and applications.
Conclusions
Ultrasonic drug targeting of chemotherapeutic agents has the potential to alter current clinical paradigms of cancer treatment to significantly improve therapeutic outcomes and the quality of life of patients undergoing chemotherapeutic treatment. In this review, we have discussed several state-of-the-art materials that are currently being developed for ultrasound-triggered drug release. Although many of these materials are in the early stage of development, they have strong potential for the use in clinical drug delivery treatments as well as for image-guided drug delivery.
Acknowledgements
Funding for this work was provided to SRS by NIH 1R21EB015040-01A1 and to MAB by NSF grants CBET-1133687 and CBET-1059726.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Loverock P, ter Haar G, Ormerod MG, Imrie PR. The effect of ultrasound on the cytotoxicity of adriamycin. Br. J. Radiol. 1990;63:542–546. doi: 10.1259/0007-1285-63-751-542. [DOI] [PubMed] [Google Scholar]
- 2.Bao S, Thrall BD, Miller DL. Transfection of a reporter plasmid into cultured cells by sonoporation in vitro. Ultrasound Med. Biol. 1997;23:953–959. doi: 10.1016/s0301-5629(97)00025-2. [DOI] [PubMed] [Google Scholar]
- 3.Tachibana K, Uchida T, Tamura K, Eguchi H, Yamashita N, Ogawa K. Enhanced cytotoxic effect of Ara-C by low intensity ultrasound to HL-60 cells. Cancer Lett. 2000;149:189–194. doi: 10.1016/s0304-3835(99)00358-4. [DOI] [PubMed] [Google Scholar]
- 4.Tachibana K, Uchida T, Ogawa K, Yamashita N, Tamura K. Induction of cell-membrane porosity by ultrasound. Lancet. 1999;353:1409. doi: 10.1016/S0140-6736(99)01244-1. [DOI] [PubMed] [Google Scholar]
- 5.Saito K, Miyake K, McNeil PL, Kato K, Yago K, Sugai N. Plasma membrane disruption underlies injury of the corneal endothelium by ultrasound. Exp. Eye Res. 1999;68:431–437. doi: 10.1006/exer.1998.0626. [DOI] [PubMed] [Google Scholar]
- 6.Domenici F, Giliberti C, Bedini A, Palomba R, Luongo F, Sennato S, et al. Ultrasound well below the intensity threshold of cavitation can promote efficient uptake of small drug model molecules in fibroblast cells. Drug Deliv. 2013;20:285–295. doi: 10.3109/10717544.2013.836620. [DOI] [PubMed] [Google Scholar]
- 7.Rapoport NY, Herron JN, Pitt WG, Pitina L. Micellar delivery of doxorubicin and its paramagnetic analog, ruboxyl, to HL-60 cells: effect of micelle structure and ultrasound on the intracellular drug uptake. J. Control. Release Off. J. Control. Release Soc. 1999;58:153–162. doi: 10.1016/s0168-3659(98)00149-7. [DOI] [PubMed] [Google Scholar]
- 8.Sirsi SR, Borden MA. Advances in ultrasound mediated gene therapy using microbubble contrast agents. Theranostics. 2012;2:1208–1222. doi: 10.7150/thno.4306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Halliwell M. A tutorial on ultrasonic physics and imaging techniques. Proc. Inst. Mech. Eng. [H] 2010;224:127–142. doi: 10.1243/09544119JEIM656. [DOI] [PubMed] [Google Scholar]
- 10.Azhari H. Basics of biomedical ultrasound for engineers. Hoboken, N.J: Wiley: IEEE; 2010. [Google Scholar]
- 11.Abbott JG. Rationale and derivation of MI and TI--a review. Ultrasound Med. Biol. 1999;25:431–441. doi: 10.1016/s0301-5629(98)00172-0. [DOI] [PubMed] [Google Scholar]
- 12.Dalecki D. Mechanical bioeffects of ultrasound. Annu. Rev. Biomed. Eng. 2004;6:229–248. doi: 10.1146/annurev.bioeng.6.040803.140126. [DOI] [PubMed] [Google Scholar]
- 13.Leighton TG. The acoustic bubble. London: Academic Press; 1994. [Google Scholar]
- 14.Lantheus Medical Imaging. How to Use DEFINITY®: System Optimization. 2013. [Google Scholar]
- 15.Coussios CC, Roy RA. Applications of Acoustics and Cavitation to Noninvasive Therapy and Drug Delivery. Annu. Rev. Fluid Mech. 2008;40:395–420. [Google Scholar]
- 16.Miller DL. Overview of experimental studies of biological effects of medical ultrasound caused by gas body activation and inertial cavitation. Prog. Biophys. Mol. Biol. 2007;93:314–330. doi: 10.1016/j.pbiomolbio.2006.07.027. [DOI] [PubMed] [Google Scholar]
- 17.Miller DL, Smith NB, Bailey MR, Czarnota GJ, Hynynen K, Makin IRS, et al. Overview of therapeutic ultrasound applications and safety considerations. J. Ultrasound Med. Off. J. Am. Inst. Ultrasound Med. 2012;31:623–634. doi: 10.7863/jum.2012.31.4.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pitt WG, Husseini GA, Staples BJ. Ultrasonic drug delivery--a general review. Expert Opin. Drug Deliv. 2004;1:37–56. doi: 10.1517/17425247.1.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sirsi SR, Borden MA. Advances in ultrasound mediated gene therapy using microbubble contrast agents. Theranostics. 2012;2:1208–1222. doi: 10.7150/thno.4306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qin S, Caskey CF, Ferrara KW. Ultrasound contrast microbubbles in imaging and therapy: physical principles and engineering. Phys. Med. Biol. 2009;54:R27–R57. doi: 10.1088/0031-9155/54/6/R01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Postema M, Schmitz G. Bubble dynamics involved in ultrasonic imaging. Expert Rev. Mol. Diagn. 2006;6:493–502. doi: 10.1586/14737159.6.3.493. [DOI] [PubMed] [Google Scholar]
- 22.Baker KG, Robertson VJ, Duck FA. A review of therapeutic ultrasound: biophysical effects. Phys. Ther. 2001;81:1351–1358. [PubMed] [Google Scholar]
- 23.Shi X, Martin RW, Vaezy S, Crum LA. Quantitative investigation of acoustic streaming in blood. J. Acoust. Soc. Am. 2002;111:1110–1121. doi: 10.1121/1.1428544. [DOI] [PubMed] [Google Scholar]
- 24.Dayton PA, Allen JS, Ferrara KW. The magnitude of radiation force on ultrasound contrast agents. J. Acoust. Soc. Am. 2002;112:2183–2192. doi: 10.1121/1.1509428. [DOI] [PubMed] [Google Scholar]
- 25.Shortencarier MJ, Dayton PA, Bloch SH, Schumann PA, Matsunaga TO, Ferrara KW. A method for radiation-force localized drug delivery using gas-filled lipospheres. IEEE Trans. Ultrason. Ferroelectr. Freq. Control. 2004;51:822–831. doi: 10.1109/tuffc.2004.1320741. [DOI] [PubMed] [Google Scholar]
- 26.Doinikov AA, Bouakaz A. Acoustic microstreaming around an encapsulated particle. J. Acoust. Soc. Am. 2010;127:1218–1227. doi: 10.1121/1.3290997. [DOI] [PubMed] [Google Scholar]
- 27.Diederich CJ, Hynynen K. Ultrasound technology for hyperthermia. Ultrasound Med. Biol. 1999;25:871–887. doi: 10.1016/s0301-5629(99)00048-4. [DOI] [PubMed] [Google Scholar]
- 28.Diederich CJ. Thermal ablation and high-temperature thermal therapy: overview of technology and clinical implementation. Int. J. Hyperth. Off. J. Eur. Soc. Hyperthermic Oncol. North Am. Hyperth. Group. 2005;21:745–753. doi: 10.1080/02656730500271692. [DOI] [PubMed] [Google Scholar]
- 29.Quesson B, de Zwart JA, Moonen CT. Magnetic resonance temperature imaging for guidance of thermotherapy. J. Magn. Reson. Imaging JMRI. 2000;12:525–533. doi: 10.1002/1522-2586(200010)12:4<525::aid-jmri3>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 30.Partanen A, Tillander M, Yarmolenko PS, Wood BJ, Dreher MR, Kohler MO. Reduction of peak acoustic pressure and shaping of heated region by use of multifoci sonications in MR-guided high-intensity focused ultrasound mediated mild hyperthermia. Med. Phys. 2013;40:013301. doi: 10.1118/1.4769116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaneko Y, Maruyama T, Takegami K, Watanabe T, Mitsui H, Hanajiri K, et al. Use of a microbubble agent to increase the effects of high intensity focused ultrasound on liver tissue. Eur. Radiol. 2005;15:1415–1420. doi: 10.1007/s00330-005-2663-7. [DOI] [PubMed] [Google Scholar]
- 32.Yu T, Wang G, Hu K, Ma P, Bai J, Wang Z. A microbubble agent improves the therapeutic efficiency of high intensity focused ultrasound: a rabbit kidney study. Urol. Res. 2004;32:14–19. doi: 10.1007/s00240-003-0362-x. [DOI] [PubMed] [Google Scholar]
- 33.Yu T, Xiong S, Mason TJ, Wang Z. The use of a micro-bubble agent to enhance rabbit liver destruction using high intensity focused ultrasound. Ultrason. Sonochem. 2006;13:143–149. doi: 10.1016/j.ultsonch.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 34.Lu Y, Park K. Polymeric micelles and alternative nanonized delivery vehicles for poorly soluble drugs. Int. J. Pharm. 2013;453:198–214. doi: 10.1016/j.ijpharm.2012.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.D’Addio SM, Prud’homme RK. Controlling drug nanoparticle formation by rapid precipitation. Adv. Drug Deliv. Rev. 2011;63:417–426. doi: 10.1016/j.addr.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 36.Husseini GA, Pitt WG. The use of ultrasound and micelles in cancer treatment. J. Nanosci. Nanotechnol. 2008;8:2205–2215. doi: 10.1166/jnn.2008.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Munshi N, Rapoport N, Pitt WG. Ultrasonic activated drug delivery from Pluronic P-105 micelles. Cancer Lett. 1997;118:13–19. doi: 10.1016/s0304-3835(97)00218-8. [DOI] [PubMed] [Google Scholar]
- 38.Rapoport N. Stabilization and activation of Pluronic micelles for tumor-targeted drug delivery. Colloids Surf. B Biointerfaces. 1999;16:93–111. [Google Scholar]
- 39.Rapoport N. Ultrasound-mediated micellar drug delivery. Int. J. Hyperth. Off. J. Eur. Soc. Hyperthermic Oncol. North Am. Hyperth. Group. 2012;28:374–385. doi: 10.3109/02656736.2012.665567. [DOI] [PubMed] [Google Scholar]
- 40.Husseini GA, Myrup GD, Pitt WG, Christensen DA, Rapoport NY. Factors affecting acoustically triggered release of drugs from polymeric micelles. J. Control. Release Off. J. Control. Release Soc. 2000;69:43–52. doi: 10.1016/s0168-3659(00)00278-9. [DOI] [PubMed] [Google Scholar]
- 41.Husseini GA, Christensen DA, Rapoport NY, Pitt WG. Ultrasonic release of doxorubicin from Pluronic P105 micelles stabilized with an interpenetrating network of N,N-diethylacrylamide. J. Control. Release Off. J. Control. Release Soc. 2002;83:303–305. doi: 10.1016/s0168-3659(02)00203-1. [DOI] [PubMed] [Google Scholar]
- 42.Husseini GA, Diaz de la Rosa MA, Richardson ES, Christensen DA, Pitt WG. The role of cavitation in acoustically activated drug delivery. J. Control. Release Off. J. Control. Release Soc. 2005;107:253–261. doi: 10.1016/j.jconrel.2005.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Marin A, Sun H, Husseini GA, Pitt WG, Christensen DA, Rapoport NY. Drug delivery in pluronic micelles: effect of high-frequency ultrasound on drug release from micelles and intracellular uptake. J. Control. Release Off. J. Control. Release Soc. 2002;84:39–47. doi: 10.1016/s0168-3659(02)00262-6. [DOI] [PubMed] [Google Scholar]
- 44.Husseini GA, Velluto D, Kherbeck L, Pitt WG, Hubbell JA, Christensen DA. Investigating the acoustic release of doxorubicin from targeted micelles. Colloids Surf. B Biointerfaces. 2013;101:153–155. doi: 10.1016/j.colsurfb.2012.05.025. [DOI] [PubMed] [Google Scholar]
- 45.Mohan P, Rapoport N. Doxorubicin as a molecular nanotheranostic agent: effect of doxorubicin encapsulation in micelles or nanoemulsions on the ultrasound-mediated intracellular delivery and nuclear trafficking. Mol. Pharm. 2010;7:1959–1973. doi: 10.1021/mp100269f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hasanzadeh H, Mokhtari-Dizaji M, Bathaie SZ, Hassan ZM. Effect of local dual frequency sonication on drug distribution from polymeric nanomicelles. Ultrason. Sonochem. 2011;18:1165–1171. doi: 10.1016/j.ultsonch.2011.03.018. [DOI] [PubMed] [Google Scholar]
- 47.Wang J, Pelletier M, Zhang H, Xia H, Zhao Y. High-frequency ultrasound-responsive block copolymer micelle. Langmuir ACS J. Surf. Colloids. 2009;25:13201–13205. doi: 10.1021/la9018794. [DOI] [PubMed] [Google Scholar]
- 48.Pelletier M, Babin J, Tremblay L, Zhao Y. Investigation of a New Thermosensitive Block Copolymer Micelle: Hydrolysis, Disruption, and Release. Langmuir. 2008;24:12664–12670. doi: 10.1021/la802522b. [DOI] [PubMed] [Google Scholar]
- 49.Allen TM, Cullis PR. Liposomal drug delivery systems: from concept to clinical applications. Adv. Drug Deliv. Rev. 2013;65:36–48. doi: 10.1016/j.addr.2012.09.037. [DOI] [PubMed] [Google Scholar]
- 50.Gabizon AA. Pegylated liposomal doxorubicin: metamorphosis of an old drug into a new form of chemotherapy. Cancer Invest. 2001;19:424–436. doi: 10.1081/cnv-100103136. [DOI] [PubMed] [Google Scholar]
- 51.Fang J, Nakamura H, Maeda H. The EPR effect: Unique features of tumor blood vessels for drug delivery, factors involved, and limitations and augmentation of the effect. Adv. Drug Deliv. Rev. 2011;63:136–151. doi: 10.1016/j.addr.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 52.Schroeder A, Kost J, Barenholz Y. Ultrasound, liposomes, and drug delivery: principles for using ultrasound to control the release of drugs from liposomes. Chem. Phys. Lipids. 2009;162:1–16. doi: 10.1016/j.chemphyslip.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 53.Krasovitski B, Frenkel V, Shoham S, Kimmel E. Intramembrane cavitation as a unifying mechanism for ultrasound-induced bioeffects. Proc. Natl. Acad. Sci. U. S. A. 2011;108:3258–3263. doi: 10.1073/pnas.1015771108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lin HY, Thomas JL. Factors affecting responsivity of unilamellar liposomes to 20 kHz ultrasound. Langmuir ACS J. Surf. Colloids. 2004;20:6100–6106. doi: 10.1021/la049866z. [DOI] [PubMed] [Google Scholar]
- 55.Schroeder A, Avnir Y, Weisman S, Najajreh Y, Gabizon A, Talmon Y, et al. Controlling liposomal drug release with low frequency ultrasound: mechanism and feasibility. Langmuir ACS J. Surf. Colloids. 2007;23:4019–4025. doi: 10.1021/la0631668. [DOI] [PubMed] [Google Scholar]
- 56.Somaglino L, Bouchoux G, Mestas JL, Lafon C. Validation of an acoustic cavitation dose with hydroxyl radical production generated by inertial cavitation in pulsed mode: application to in vitro drug release from liposomes. Ultrason. Sonochem. 2011;18:577–588. doi: 10.1016/j.ultsonch.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 57.Lafon C, Somaglino L, Bouchoux G, Mari JM, Chesnais S, Ngo J, et al. Feasibility study of cavitation-induced liposomal doxorubicin release in an AT2 Dunning rat tumor model. J. Drug Target. 2012;20:691–702. doi: 10.3109/1061186X.2012.712129. [DOI] [PubMed] [Google Scholar]
- 58.Evjen TJ, Hagtvet E, Moussatov A, Røgnvaldsson S, Mestas J-L, Fowler RA, et al. In vivo monitoring of liposomal release in tumours following ultrasound stimulation. Eur. J. Pharm. Biopharm. doi: 10.1016/j.ejpb.2012.12.007. (n.d.). [DOI] [PubMed] [Google Scholar]
- 59.Weinstein JN, Magin RL, Yatvin MB, Zaharko DS. Liposomes and local hyperthermia: selective delivery of methotrexate to heated tumors. Science. 1979;204:188–191. doi: 10.1126/science.432641. [DOI] [PubMed] [Google Scholar]
- 60.Tacker JR, Anderson RU. Delivery of antitumor drug to bladder cancer by use of phase transition liposomes and hyperthermia. J. Urol. 1982;127:1211–1214. doi: 10.1016/s0022-5347(17)54299-8. [DOI] [PubMed] [Google Scholar]
- 61.Needham D, Anyarambhatla G, Kong G, Dewhirst MW. A new temperature-sensitive liposome for use with mild hyperthermia: characterization and testing in a human tumor xenograft model. Cancer Res. 2000;60:1197–1201. [PubMed] [Google Scholar]
- 62.Gasselhuber A, Dreher MR, Rattay F, Wood BJ, Haemmerich D. Comparison of conventional chemotherapy, stealth liposomes and temperature-sensitive liposomes in a mathematical model. PloS One. 2012;7:e47453. doi: 10.1371/journal.pone.0047453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kong G, Anyarambhatla G, Petros WP, Braun RD, Colvin OM, Needham D, et al. Efficacy of liposomes and hyperthermia in a human tumor xenograft model: importance of triggered drug release. Cancer Res. 2000;60:6950–6957. [PubMed] [Google Scholar]
- 64.Dromi S, Frenkel V, Luk A, Traughber B, Angstadt M, Bur M, et al. Pulsed-high intensity focused ultrasound and low temperature-sensitive liposomes for enhanced targeted drug delivery and antitumor effect. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2007;13:2722–2727. doi: 10.1158/1078-0432.CCR-06-2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Paoli EE, Kruse DE, Seo JW, Zhang H, Kheirolomoom A, Watson KD, et al. An optical and microPET assessment of thermally-sensitive liposome biodistribution in the Met-1 tumor model: Importance of formulation. J. Control. Release Off. J. Control. Release Soc. 2010;143:13–22. doi: 10.1016/j.jconrel.2009.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ning S, Macleod K, Abra RM, Huang AH, Hahn GM. Hyperthermia induces doxorubicin release from long-circulating liposomes and enhances their anti-tumor efficacy. Int. J. Radiat. Oncol. Biol. Phys. 1994;29:827–834. doi: 10.1016/0360-3016(94)90572-x. [DOI] [PubMed] [Google Scholar]
- 67.Oerlemans C, Deckers R, Storm G, Hennink WE, Nijsen JFW. Evidence for a new mechanism behind HIFU-triggered release from liposomes. J. Controlled Release. 2013;168:327–333. doi: 10.1016/j.jconrel.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 68.Evjen TJ, Nilssen EA, Rognvaldsson S, Brandl M, Fossheim SL. Distearoylphosphatidylethanolamine-based liposomes for ultrasound-mediated drug delivery. Eur. J. Pharm. Biopharm. Off. J. Arbeitsgemeinschaft Pharm. Verfahrenstechnik EV. 2010;75:327–333. doi: 10.1016/j.ejpb.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 69.Lentacker I, De Smedt SC, Sanders NN. Drug loaded microbubble design for ultrasound triggered delivery. Soft Matter. 2009;5:2161–2170. [Google Scholar]
- 70.Sirsi S, Borden M. Microbubble Compositions, Properties and Biomedical Applications. Bubble Sci. Eng. Technol. 2009;1:3–17. doi: 10.1179/175889709X446507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kabalnov A, Klein D, Pelura T, Schutt E, Weers J. Dissolution of multicomponent microbubbles in the bloodstream: 1. Theory. Ultrasound Med. Biol. 1998;24:739–749. doi: 10.1016/s0301-5629(98)00034-9. [DOI] [PubMed] [Google Scholar]
- 72.Tartis MS, Kruse DE, Zheng H, Zhang H, Kheirolomoom A, Marik J, et al. Dynamic microPET imaging of ultrasound contrast agents and lipid delivery. J. Control. Release Off. J. Control. Release Soc. 2008;131:160–166. doi: 10.1016/j.jconrel.2008.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Crum L. Nucleation and stabilization of microbubbles in liquids. Appl. Sci. Res. 1982;38:101–115. [Google Scholar]
- 74.Wu J, Nyborg WL. Ultrasound, cavitation bubbles and their interaction with cells. Adv. Drug Deliv. Rev. 2008;60:1103–1116. doi: 10.1016/j.addr.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 75.Borden MA, Streeter JE, Dayton PA, Sirsi SR. In Vivo Demonstration of Cancer Molecular Imaging with Ultrasound Radiation Force and Buried-ligand Microbubbles. Mol Imaging. 2013;12:1. [PMC free article] [PubMed] [Google Scholar]
- 76.Caskey CF, Qin S, Dayton PA, Ferrara KW. Microbubble tunneling in gel phantoms. J. Acoust. Soc. Am. 2009;125:EL183–EL189. doi: 10.1121/1.3097679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Arvanitis CD, Bazan-Peregrino M, Rifai B, Seymour LW, Coussios CC. Cavitation-enhanced extravasation for drug delivery. Ultrasound Med. Biol. 2011;37:1838–1852. doi: 10.1016/j.ultrasmedbio.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 78.Korpanty G, Chen S, Shohet RV, Ding J, Yang B, Frenkel PA, et al. Targeting of VEGF-mediated angiogenesis to rat myocardium using ultrasonic destruction of microbubbles. Gene Ther. 2005;12:1305–1312. doi: 10.1038/sj.gt.3302532. [DOI] [PubMed] [Google Scholar]
- 79.Tsunoda S, Mazda O, Oda Y, Iida Y, Akabame S, Kishida T, et al. Sonoporation using microbubble BR14 promotes pDNA/siRNA transduction to murine heart. Biochem. Biophys. Res. Commun. 2005;336:118–127. doi: 10.1016/j.bbrc.2005.08.052. [DOI] [PubMed] [Google Scholar]
- 80.Unger EC, McCreery TP, Sweitzer RH, Caldwell VE, Wu Y. Acoustically active lipospheres containing paclitaxel: a new therapeutic ultrasound contrast agent. Invest. Radiol. 1998;33:886–892. doi: 10.1097/00004424-199812000-00007. [DOI] [PubMed] [Google Scholar]
- 81.Tartis MS, McCallan J, Lum AF, LaBell R, Stieger SM, Matsunaga TO, et al. Therapeutic effects of paclitaxel-containing ultrasound contrast agents. Ultrasound Med. Biol. 2006;32:1771–1780. doi: 10.1016/j.ultrasmedbio.2006.03.017. [DOI] [PubMed] [Google Scholar]
- 82.Tinkov S, Coester C, Serba S, Geis NA, Katus HA, Winter G, et al. New doxorubicin-loaded phospholipid microbubbles for targeted tumor therapy: in-vivo characterization. J. Control. Release Off. J. Control. Release Soc. 2010;148:368–372. doi: 10.1016/j.jconrel.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 83.de Wolf FA, Maliepaard M, van Dorsten F, Berghuis I, Nicolay K, de Kruijff B. Comparable interaction of doxorubicin with various acidic phospholipids results in changes of lipid order and dynamics. Biochim. Biophys. Acta. 1990;1096:67–80. doi: 10.1016/0925-4439(90)90014-g. [DOI] [PubMed] [Google Scholar]
- 84.Nicolay K, Sautereau AM, Tocanne JF, Brasseur R, Huart P, Ruysschaert JM, et al. A comparative model membrane study on structural effects of membrane-active positively charged anti-tumor drugs. Biochim. Biophys. Acta. 1988;940:197–208. doi: 10.1016/0005-2736(88)90195-2. [DOI] [PubMed] [Google Scholar]
- 85.Wu Y, Lu C, Li W, Sun C, Yang W, Zhang Y, et al. Preparation and antitumor activity of bFGF-mediated active targeting doxorubicin microbubbles. Drug Dev. Ind. Pharm. 2012:1–8. doi: 10.3109/03639045.2012.730527. [DOI] [PubMed] [Google Scholar]
- 86.Zhao YZ, Sun CZ, Lu CT, Dai DD, Lv HF, Wu Y, et al. Characterization and anti-tumor activity of chemical conjugation of doxorubicin in polymeric micelles (DOX-P) in vitro. Cancer Lett. 2011;311:187–194. doi: 10.1016/j.canlet.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 87.Terada T, Mizobata M, Kawakami S, Yamashita F, Hashida M. Optimization of tumor-selective targeting by basic fibroblast growth factor-binding peptide grafted PEGylated liposomes. J. Control. Release Off. J. Control. Release Soc. 2007;119:262–270. doi: 10.1016/j.jconrel.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 88.Sirsi SR, Fung C, Garg S, Tianning MY, Mountford PA, Borden MA. Lung Surfactant Microbubbles Increase Lipophilic Drug Payload for Ultrasound-Targeted Delivery. Theranostics. 2013;3:409. doi: 10.7150/thno.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Perez-Gil J. Lipid-protein interactions of hydrophobic proteins SP-B and SP-C in lung surfactant assembly and dynamics. Pediatr. Pathol. Mol. Med. 2001;20:445–469. doi: 10.1080/pdp.20.6.445.469. [DOI] [PubMed] [Google Scholar]
- 90.Bloch SH, Wan M, Dayton PA, Ferrara KW. Optical observation of lipid- and polymer-shelled ultrasound microbubble contrast agents. Appl. Phys. Lett. 2004;84:631. [Google Scholar]
- 91.Mehier-Humbert S, Yan F, Frinking P, Schneider M, Guy RH, Bettinger T. Ultrasound-mediated gene delivery: influence of contrast agent on transfection. Bioconjug. Chem. 2007;18:652–662. doi: 10.1021/bc0602432. [DOI] [PubMed] [Google Scholar]
- 92.Eisenbrey JR, Burstein OM, Kambhampati R, Forsberg F, Liu JB, Wheatley MA. Development and optimization of a doxorubicin loaded poly(lactic acid) contrast agent for ultrasound directed drug delivery. J. Control. Release Off. J. Control. Release Soc. 2010;143:38–44. doi: 10.1016/j.jconrel.2009.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Eisenbrey JR, Soulen MC, Wheatley MA. Delivery of encapsulated Doxorubicin by ultrasound-mediated size reduction of drug-loaded polymer contrast agents. IEEE Trans. Biomed. Eng. 2010;57:24–28. doi: 10.1109/TBME.2009.2030497. [DOI] [PubMed] [Google Scholar]
- 94.Cochran MC, Eisenbrey JR, Soulen MC, Schultz SM, Ouma RO, White SB, et al. Disposition of ultrasound sensitive polymeric drug carrier in a rat hepatocellular carcinoma model. Acad. Radiol. 2011;18:1341–1348. doi: 10.1016/j.acra.2011.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dicker S, Mleczko M, Hensel K, Bartolomeo A, Schmitz G, Wrenn S. Coencapsulation of lipid microbubbles within polymer microcapsules for contrast applications. Bubble SciEngTechnol. 2011;3:12–19. [Google Scholar]
- 96.Kheirolomoom A, Dayton PA, Lum AF, Little E, Paoli EE, Zheng H, et al. Acoustically-active microbubbles conjugated to liposomes: characterization of a proposed drug delivery vehicle. J. Control. Release Off. J. Control. Release Soc. 2007;118:275–284. doi: 10.1016/j.jconrel.2006.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lentacker I, Geers B, Demeester J, De Smedt SC, Sanders NN. Design and evaluation of doxorubicin-containing microbubbles for ultrasound-triggered doxorubicin delivery: cytotoxicity and mechanisms involved. Mol. Ther. J. Am. Soc. Gene Ther. 2010;18:101–108. doi: 10.1038/mt.2009.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Fan C-H, Ting C-Y, Lin H-J, Wang C-H, Liu H-L, Yen T-C, et al. SPIO-conjugated, doxorubicin-loaded microbubbles for concurrent MRI and focused-ultrasound enhanced brain-tumor drug delivery. Biomaterials. 2013;34:3706–3715. doi: 10.1016/j.biomaterials.2013.01.099. [DOI] [PubMed] [Google Scholar]
- 99.Niu C, Wang Z, Lu G, Krupka TM, Sun Y, You Y, et al. Doxorubicin loaded superparamagnetic PLGA-iron oxide multifunctional microbubbles for dual-mode US/MR imaging and therapy of metastasis in lymph nodes. Biomaterials. 2013;34:2307–2317. doi: 10.1016/j.biomaterials.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 100.Owen J, Pankhurst Q, Stride E. Magnetic targeting and ultrasound mediated drug delivery: Benefits, limitations and combination. Int. J. Hyperth. Off. J. Eur. Soc. Hyperthermic Oncol. North Am. Hyperth. Group. 2012;28:362–373. doi: 10.3109/02656736.2012.668639. [DOI] [PubMed] [Google Scholar]
- 101.Stride E, Porter C, Prieto AG, Pankhurst Q. Enhancement of Microbubble Mediated Gene Delivery by Simultaneous Exposure to Ultrasonic and Magnetic Fields. Ultrasound Med. Biol. 2009;35:861–868. doi: 10.1016/j.ultrasmedbio.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 102.Mulvana H, Eckersley RJ, Tang M-X, Pankhurst Q, Stride E. Theoretical and Experimental Characterisation of Magnetic Microbubbles. Ultrasound Med. Biol. 2012;38:864–875. doi: 10.1016/j.ultrasmedbio.2012.01.027. [DOI] [PubMed] [Google Scholar]
- 103.Owen J, Zhou B, Rademeyer P, Tang MX, Pankhurst Q, Eckersley R, et al. Understanding the structure and mechanism of formation of a new magnetic microbubble formulation. Theranostics. 2012;2:1127–1139. doi: 10.7150/thno.4307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Dove JD, Murray TW, Borden MA. Enhanced photoacoustic response with plasmonic nanoparticle-templated microbubbles. Soft Matter. 2013;9:7743. [Google Scholar]
- 105.Leskinen JTT, Hakulinen MA, Kuosmanen M, Ketolainen J, Abrahmsén-Alami S, Lappalainen R. Monitoring of swelling of hydrophilic polymer matrix tablets by ultrasound techniques. Int. J. Pharm. 2011;404:142–147. doi: 10.1016/j.ijpharm.2010.11.026. [DOI] [PubMed] [Google Scholar]
- 106.Lanting B, Barfett J. Encapsulated calcium carbonate suspensions: a drug delivery vehicle sensitive to ultrasound disruption. McGill J. Med. MJM Int. Forum Adv. Med. Sci. Stud. 2006;9:108–110. [PMC free article] [PubMed] [Google Scholar]
- 107.Bao M, Zhou Q, Dong W, Lou X, Zhang Y. Ultrasound-Modulated Shape Memory and Payload Release Effects in a Biodegradable Cylindrical Rod Made of Chitosan-Functionalized PLGA Microspheres. Biomacromolecules. 2013;14:1971–1979. doi: 10.1021/bm4003464. [DOI] [PubMed] [Google Scholar]
- 108.Epstein-Barash H, Orbey G, Polat BE, Ewoldt RH, Feshitan J, Langer R, et al. A microcomposite hydrogel for repeated on-demand ultrasound-triggered drug delivery. Biomaterials. 2010;31:5208–5217. doi: 10.1016/j.biomaterials.2010.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhang M, Fabiilli ML, Haworth KJ, Padilla F, Swanson SD, Kripfgans OD, et al. Acoustic droplet vaporization for enhancement of thermal ablation by high intensity focused ultrasound. Acad. Radiol. 2011;18:1123–1132. doi: 10.1016/j.acra.2011.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Zhu M, Jiang L, Fabiilli ML, Zhang A, Fowlkes JB, Xu LX. Treatment of murine tumors using acoustic droplet vaporization-enhanced high intensity focused ultrasound. Phys. Med. Biol. 2013;58:6179–6191. doi: 10.1088/0031-9155/58/17/6179. [DOI] [PubMed] [Google Scholar]
- 111.Fabiilli ML, Lee JA, Kripfgans OD, Carson PL, Fowlkes JB. Delivery of water-soluble drugs using acoustically triggered perfluorocarbon double emulsions. Pharm. Res. 2010;27:2753–2765. doi: 10.1007/s11095-010-0277-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Rapoport N. Phase-shift, stimuli-responsive perfluorocarbon nanodroplets for drug delivery to cancer. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2012;4:492–510. doi: 10.1002/wnan.1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sheeran PS, Dayton PA. Phase-change contrast agents for imaging and therapy. Curr. Pharm. Des. 2012;18:2152–2165. doi: 10.2174/138161212800099883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Rapoport N, Gao Z, Kennedy A. Multifunctional nanoparticles for combining ultrasonic tumor imaging and targeted chemotherapy. J. Natl. Cancer Inst. 2007;99:1095–1106. doi: 10.1093/jnci/djm043. [DOI] [PubMed] [Google Scholar]
- 115.Gao Z, Kennedy AM, Christensen DA, Rapoport NY. Drug-loaded nano/microbubbles for combining ultrasonography and targeted chemotherapy. Ultrasonics. 2008;48:260–270. doi: 10.1016/j.ultras.2007.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rapoport N, Nam KH, Gupta R, Gao Z, Mohan P, Payne A, et al. Ultrasound-mediated tumor imaging and nanotherapy using drug loaded, block copolymer stabilized perfluorocarbon nanoemulsions. J. Control. Release Off. J. Control. Release Soc. 2011;153:4–15. doi: 10.1016/j.jconrel.2011.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kopechek JA, Park E, Mei C-S, McDannold NJ, Porter TM. Accumulation of phase-shift nanoemulsions to enhance MR-guided ultrasound-mediated tumor ablation in vivo. J. Healthc. Eng. 2013;4:109–126. doi: 10.1260/2040-2295.4.1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Couture O, Faivre M, Pannacci N, Babataheri A, Servois V, Tabeling P, et al. Ultrasound internal tattooing. Med. Phys. 2011;38:1116–1123. doi: 10.1118/1.3548068. [DOI] [PubMed] [Google Scholar]
- 119.Phillips LC, Puett C, Sheeran PS, Dayton PA, Miller GW, Matsunaga TO. Phase-shift perfluorocarbon agents enhance high intensity focused ultrasound thermal delivery with reduced near-field heating. J. Acoust. Soc. Am. 2013;134:1473–1482. doi: 10.1121/1.4812866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lin C-Y, Javadi M, Belnap DM, Barrow JR, Pitt WG. Ultrasound sensitive eLiposomes containing doxorubicin for drug targeting therapy. Nanomedicine Nanotechnol. Biol. Med. 2013 doi: 10.1016/j.nano.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 121.Kagan D, Benchimol MJ, Claussen JC, Chuluun-Erdene E, Esener S, Wang J. Acoustic Droplet Vaporization and Propulsion of Perfluorocarbon-Loaded Microbullets for Targeted Tissue Penetration and Deformation. Angew. Chem. Int. Ed. 2012;51 doi: 10.1002/anie.201201902. n/a–n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Sheeran PS, Luois S, Dayton PA, Matsunaga TO. Formulation and acoustic studies of a new phase-shift agent for diagnostic and therapeutic ultrasound. Langmuir ACS J. Surf. Colloids. 2011;27:10412–10420. doi: 10.1021/la2013705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sheeran PS, Luois SH, Mullin LB, Matsunaga TO, Dayton PA. Design of ultrasonically-activatable nanoparticles using low boiling point perfluorocarbons. Biomaterials. 2012;33:3262–3269. doi: 10.1016/j.biomaterials.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chen H, Kreider W, Brayman AA, Bailey MR, Matula TJ. Blood vessel deformations on microsecond time scales by ultrasonic cavitation. Phys. Rev. Lett. 2011;106:034301. doi: 10.1103/PhysRevLett.106.034301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Chen H, Brayman AA, Evan AP, Matula TJ. Preliminary Observations on the Spatial Correlation Between Short-Burst Microbubble Oscillations and Vascular Bioeffects. Ultrasound Med. Biol. 2012;38:2151–2162. doi: 10.1016/j.ultrasmedbio.2012.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]