Abstract
Introduction
The pathologic relevance of Demodex infestation in blepharitis is still controversial. The aim of the study was to determine the prevalence of Demodex spp. in eyelash follicles and its relationship to eye symptoms.
Material and methods
A total of 290 individuals were studied for the presence of Demodex folliculorum and Demodex brevis within eyelash follicles. Participants belonged to one of four groups: inpatients, drug abusers, health professionals, and medical students. Ten eyelashes were epilated from each subject, placed on microscope slides and examined for parasites. The sample was defined as positive if at least one parasite or parasite's ova were present. The presence of parasites was analyzed according to age, gender, place of living, reported eye problems, and use of contact lenses or glasses.
Results
The prevalence of Demodex spp. infestation among all studied subjects was 41%, with the highest infestation rate among inpatients (p < 0.01) and elderly people (p < 0.001). No difference regarding the presence of Demodex was found between women and men (p = 0.76). Demodex folliculorum was about 2.4 times more frequent than D. brevis. The prevalence of Demodex spp. in subjects with and without eye complaints suggesting blepharitis was similar (41.6% vs. 40.2%, respectively, p = 0.9). On the other hand, wearing glasses was linked to Demodex infestation (48.4% vs. 32.3%, p < 0.01).
Conclusions
Demodex is a common saprophyte found in human eyelash follicles. Its presence might be related to some ocular discomfort; however, in the vast majority of cases the infestation seems to be asymptomatic.
Keywords: blepharitis, Demodex, demodicosis, mites, prevalence
Introduction
Demodex mites (class Arachnida, subclass Acarina) are common ectoparasites found in the human skin of different ethnic groups, including but not limited to Aborigines, Caucasians, Inuits, Maoris and Nigerians [1, 2]. Two parasitic species have been described in humans: Demodex folliculorum and D. brevis [3]. Demodex mites inhabit follicles with or without hair with a predilection for areas of high sebum production. They can be observed in the skin of almost the entire body, namely on the head, the outer ear, the upper chest, mons pubis and buttocks. To a greater extent they are found in the facial T-zone (forehead, cheeks, nose and nose-labial folds) and are also frequently located in meibomian glands and follicles of eyelashes [2–4].
Demodex folliculorum occurs more frequently than D. brevis and is usually found within the follicle infundibulum. The adult individuals have a length of 279–294 µm, and arrowhead shaped ova are 104 µm × 41 µm in size. Parasites isolated from eyelashes are usually longer than mites isolated from the skin. Demodex brevis is smaller (165–208 µm), penetrates deeper into sebaceous ducts and meibomian glands and has fusiform ova (60 µm × 34 µm). The life cycle of these parasites is completed within 14–18 days from the egg through the larval stage, protonymph, deutonymph and finally to the adult mite [4, 5]. Demodex feeds on sebum, and follicular and glandular epithelial cells, and may induce inflammation of the skin and lid margin [3, 6, 7]. In the skin, Demodex mites are believed to be a causative agent of rosacea-like demodicosis, pityriasis folliculorum, pustular folliculitis, perioral granulomatous dermatitis, and hyperpigmented patches of the face. It is also believed that they may be important etiological factors of chronic blepharitis. Demodicosis of the margins of the eyelids could be related to the blockage of the ostia of hair follicles and sebaceous ducts and may induce epithelial hyperplasia and hyperkeratosis, follicular distension, cylindrical cuffs of keratin, and an inflammatory response to the mite's chitinous skeleton and its products of metabolism. Demodex mites occupying deeper regions of hair follicles cause dislocation of the base of the hair. These changes may lead to excessive loss of eyelashes and eyebrows [3, 6, 7]. Infested follicles usually contain 2–6 parasites, but they may sometimes be even more numerous [8]. Demodex mites also serve as a vector for bacteria, such as Streptococci, Staphylococci or Bacillus oleronius. Bacterial antigens on the mite surface can trigger a host inflammatory response, while bacteria present in the parasite intestine (B. oleronius) may stimulate proliferation of mononuclear cells in the peripheral blood of infected persons. Demodex mites can also transmit viruses and fungi [1, 3]. However, the relevance of Demodex spp. in blepharitis remains controversial and inconclusive, as some authors were unable to demonstrate higher prevalence of these mites in eyelash follicles of patients with blepharitis compared to healthy controls [9–11].
Transmission of Demodex is a result of close or direct contact with infested skin (containing larvae or adult mites) or by dust containing eggs. The exact prevalence of Demodex infestation, especially regarding eyelashes, is poorly characterized. It seems that certain populations, such as medical staff or students, having multiple contacts with different patients, may represent a higher risk group in respect of Demodex infestation. In addition, immunocompromised subjects, such as human immunodeficiency virus (HIV) infected subjects, may be another risk group [9, 10]. Based on that assumption we performed a study to analyze the prevalence of Demodex spp. in selected groups of people.
The aim of the study was to determine the prevalence of Demodex spp. in eyelash follicles of different populations and its relationship to eye symptoms.
Material and methods
Participants and procedure
A total of 290 individuals were studied for the presence of D. folliculorum and D. brevis within the eyelash follicles. The study group included 130 (45.0%) men and 159 (55.0%) women aged from 16 to 89 years (Table I). Participants belonged to one of four groups: inpatients of the Centre for Orthopedics and Rehabilitation or Regional Hospital admitted for hip joint replacement or for the treatment of bone fractures (n = 95), health professionals (physicians, physiotherapists, nurses) (n = 75), drug abusers from the Addiction Treatment Center MONAR (n = 34) and medical students of the Wroclaw Medical University (n = 86). According to the rules of the Addiction Treatment Center MONAR, drug abusers were abstinent at the time of examination and received appropriate treatment and psychological care. All analyzed subjects were recruited between January and July of 2011. None of the surveyed individuals was previously diagnosed with demodicosis. Based on the anamnesis and medical data, 30 out of 34 (88.2%) drug abusers were diagnosed to be infected with HIV and received anti-retroviral therapy. None of the remaining subjects was aware of being infected with HIV.
Table I.
Characteristics of the studied sample
| Variable | RH, n (%) | ATC, n (%) | HP, n (%) | MS, n (%) | Total, n (%) |
|---|---|---|---|---|---|
| Gender: | |||||
| Females | 43 (45.3) | 4 (12.1) | 63 (84.0) | 49 (57.0) | 159 (55.0) |
| Males | 52 (54.7) | 30 (88.2) | 12 (16.0) | 37 (43.0) | 130 (45.0) |
| χ2 = 54.9, p < 0.001 | |||||
| Age [years]: | |||||
| ≤ 19 | 3 (3.1) | 2 (5.9) | – | – | 5 (1.7) |
| 20–29 | 7 (7.4) | 8 (23.5) | 8 (10.7) | 86 (100) | 109 (37.6) |
| 30–39 | 11 (11.6) | 15 (44.1) | 23 (30.7) | – | 49 (17.0) |
| 40–49 | 6 (6.3) | 7 (20.6) | 26 (34.6) | – | 39 (13.5) |
| 50–59 | 26 (27.4) | 2 (5.9) | 18 (24.0) | – | 46 (15.9) |
| 60–69 | 15 (15.8) | – | – | – | 15 (5.2) |
| 70–79 | 20 (21.0) | – | – | – | 20 (6.9) |
| ≥ 80 | 7 (7.4) | – | – | – | 7 (2.4) |
| χ2 = 329.8, p < 0.001 | |||||
| Place of living: | |||||
| Old building | 39 (41.1) | 26 (76.5) | 21 (28) | 29 (33.7) | 115 (39.7) |
| New building | 56 (58.9) | 8 (23.5) | 54 (72) | 57 (66.3) | 175 (60.3) |
| χ2 = 24.9, p < 0.001 | |||||
| Total | 95 | 34 | 75 | 86 | 290 (100) |
RH – patients of the Regional Hospital in Wroclaw, ATC – drug abusers from Addiction Treatment Centre MONAR, HP – health professionals, MS – medical students
The study was approved by the Ethics Committee of Wroclaw Medical University. Prior to any study procedures each subject was asked to provide written informed consent.
Methods
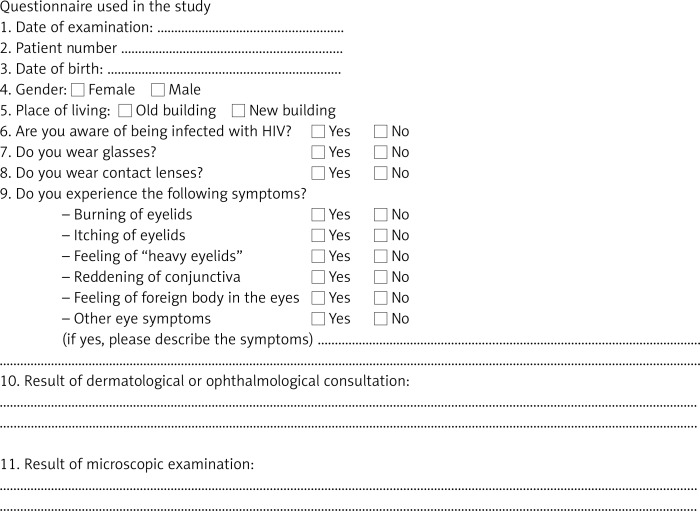
A specially designed questionnaire containing demographic (age, gender, job or faculty, place of residence) and clinical data (use of glasses or contact lenses, history of ocular diseases or problems such as redness or burning of conjunctiva, feeling of eye discomfort, having itchy eyelids or foreign body-like sensation) was completed for each participant based on the anamnesis (Appendix 1). Participants reporting symptoms suggesting blepharitis were consulted by a dermatologist (A.R.) or an ophthalmologist (M.M.-H.) to confirm or exclude the diagnosis.
Then, two drops of Hoyer's medium were placed on the basic slides, and ten eyelashes were epilated from each participant at the place of patient stay, put on a slide and covered with a cover slip. The samples were secured in a transport box and transferred to the laboratory. Slides were examined by M.W. and D.B. for parasites using light microscopy at a magnification of 100×, 200× and 400×. A sample was considered positive if at least one parasite was found [11].
Statistical analysis
Statistical analysis was performed with Statistica 9.0 (StatSoft, Cracow, Poland). Data were analyzed statistically using χ2 test and multiple regression analysis. Statistical significance was set at p < 0.05 for all parameters.
Results
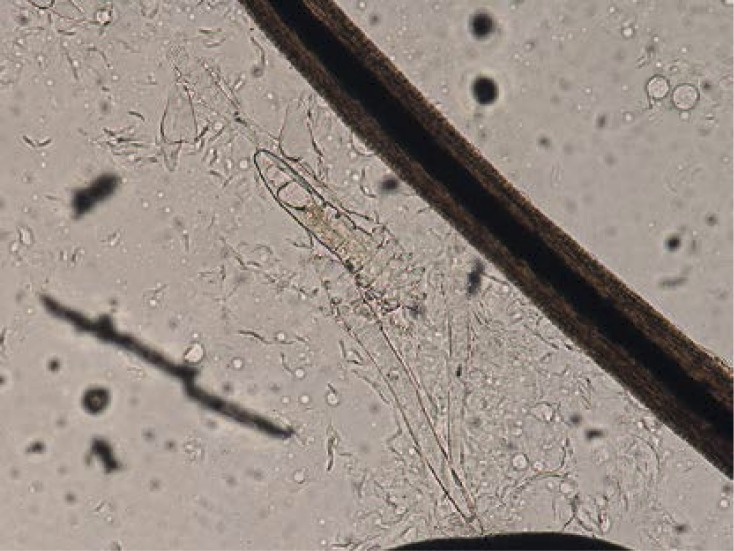
The prevalence of Demodex spp. infestation was found to be 41.0% of all studied participants (Table I). The highest infestation rate (54.7%) was observed among inpatients followed by health professionals (40.0%) (p < 0.01 regarding the comparison of all groups) (Table II). Our study revealed that D. folliculorum seems to be more frequent within eyelash follicles than D. brevis. We found 81.5% and 34.5% of positive cases for respective parasites. In 15.1% of assessed subjects coexistence of both species was noted (Figure 1).
Table II.
Ocular symptoms and prevalence of Demodex spp. in the analyzed subsamples
| Variable | RH, n (%) | ATC, n (%) | HP, n (%) | MS, n (%) | Statistics |
|---|---|---|---|---|---|
| Ocular symptoms: | |||||
| Burning of eyelids | 32 (33.7) | 9 (26.5) | 24 (32.0) | 24 (27.9) | χ2 = 1.1, p = 0.79 |
| Itching of eyelids | 42 (44.2) | 14 (41.2) | 30 (40.0) | 25 (29.1) | χ2 = 4.7, p = 0.19 |
| “Heavy eyelids” | 6 (6.3) | 7 (20.6) | 12 (16.0) | 18 (20.9) | χ2 = 9.0, p = 0.02 |
| Conjunctiva reddening | 12 (12.6) | 9 (26.5) | 24 (32.0) | 11 (12.8) | χ2 = 13.9, p < 0.01 |
| Foreign body feeling in eyes | 6 (6.3) | 6 (17.6) | 9 (12.0) | 1 (1.2) | χ2 = 12.3, p < 0.01 |
| Other | 21 (22.1) | 1 (2.9) | 5 (6.7) | 11 (12.8) | χ2 = 12.6, p < 0.01 |
| Blepharitis: | |||||
| Yes | 57 (60.0) | 19 (55.9) | 46 (61.3) | 51 (59.3) | χ2 = 29.8, p = 0.96 |
| No | 38 (40.0) | 15 (44.1) | 29 (38.7) | 35 (40.7) | |
| Wearing glasses: | |||||
| Yes | 63 (66.3) | 7 (20.6) | 46 (61.3) | 44 (51.2) | χ2 = 22.9, p < 0.001 |
| No | 32 (33.7) | 27 (79.4) | 29 (38.7) | 42 (48.8) | |
| Wearing lenses: | |||||
| Yes | 2 (2.1) | 0 (0) | 4 (5.3) | 14 (16.3) | χ2 = 18.0, p < 0.001 |
| No | 93 (97.9) | 34 (100) | 71 (94.7) | 72 (83.7) | |
| Demodex spp. prevalence | 52 (54.7) | 8 (23.5) | 30 (40.0) | 29 (33.7) | χ2 = 13.6, p < 0.01 |
Figure 1.
An example of infestation of eyelash follicle with Demodex folliculorum
No significant differences regarding Demodex spp. prevalence were noted between women and men (42.1% and 39.7% respectively) (χ2 = 0.09, p = 0.7). Evaluation of the relationship between the frequency of infestation and age was carried out without medical students, as this group only consisted of subjects aged between 20 and 29 years. It was revealed that presence of Demodex mites was significantly associated with age: the frequency of infestation markedly increased among persons older than 50 years (p = 0.005). This difference was even more pronounced if medical students were included in the analysis (χ2 = 28.0, p < 0.001) (Table III). Analyzing the place of living, persons residing in old buildings (> 30 years old) demonstrated slightly more common presence of Demodex spp. (43.5%) than people living in new houses (39.4%); however, the difference was not statistically significant (χ2 = 0.3, p = 0.57).
Table III.
Prevalence of Demodex spp. in relation to studied variables
| Parameter | Prevalence of Demodex spp. | Statistics |
|---|---|---|
| Gender: | ||
| Females | 67 (42.1%) | χ2 = 0.1, p = 0.76 |
| Males | 52 (39.7%) | |
| Age [years]: | ||
| < 20 | 0 (0.0%) | χ2 = 28.0, p < 0.001 |
| 20–29 | 36 (33.0%) | |
| 30–39 | 17 (34.7%) | |
| 40–49 | 12 (30.8%) | |
| 50–59 | 24 (52.2%) | |
| 60–69 | 11 (73.3%) | |
| 70–79 | 15 (75.0%) | |
| > 80 years | 4 (57.1%) | |
| Place of living: | ||
| Old building | 50 (43.5%) | χ2 = 0.3, p = 0.57 |
| New building | 69 (39.4%) | |
| Wearing glasses: | ||
| Yes | 77 (48.1%) | χ2 = 6.8, p < 0.01 |
| No | 42 (32.3%) | |
| Wearing lenses: | ||
| Yes | 8 (40.0%) | χ2 = 0.02, p = 0.9 |
| No | 111 (41.1%) | |
| Symptoms of blepharitis: | ||
| Yes | 72 (41.6%) | χ2 = 0.02, p = 0.9 |
| No | 47 (40.2%) |
Another aspect analyzed in the current study was the association between the presence of Demodex mites and ocular symptoms reported by participants such as redness or burning of conjunctiva, feeling of discomfort, having itchy eyelids and foreign body-like sensation. Presence of at least one symptom suggesting chronic blepharitis was noted in 59.7% of respondents. The most frequently reported symptoms were itching (38.3%) and burning (30.7%). Within individuals reporting such symptoms, 41.6% were infested with Demodex mites. The frequency of positive results in subjects showing no eye complaints was quite similar (40.2%) (χ2 = 0.02, p = 0.9).
Within the studied sample, 55.0% of subjects wore glasses, and 48.4% of them had Demodex mites. The study showed that infestation with Demodex spp. occurs more commonly in people wearing glasses (48.1%) than in those having no glasses (32.3%) (χ2 = 6.8, p < 0.01). Remarkably, no relationship was found between having contact lenses and presence of Demodex spp. (8/20 positivity in participants with contact lenses vs. 111/269 in subjects without contact lenses, χ2 = 0.02, p = 0.9).
Multiple regression analysis revealed that age and the fact of wearing eye glasses were the only parameters among analyzed variables which were significantly associated with the presence of Demodex spp. in eyelash follicles (β = 0.27 ±0.06, p < 0.001 and β = 0.16 ±0.06, p < 0.01, respectively).
Discussion
Demodex mite is a widespread parasite of hair follicles and the pilosebaceous units of human eyelids. Most studies on demodicosis have been focused on the skin, but there is little information in the literature on the prevalence of Demodex in eyelashes of the general human population. Some authors consider Demodex to be an innocuous organism living in the skin, while others believe that it may play a role as an important pathogen in the development of demodicosis, rosacea or chronic blepharitis and contribute to ocular surface irritation [5, 6, 12]. As the pathologic relevance of Demodex infestation in blepharitis is still controversial [13, 14], we would like to share our data on this subject, hoping that they will add further information on this interesting topic.
We found Demodex spp. in about 40% of analyzed subjects. Remarkably, we did not observe a higher prevalence of parasites among subjects with ocular discomfort or symptoms compared to the rest of studied individuals. Our findings are in accordance with the study by Kemal et al. [10], who also did not observe any significant differences of Demodex infestation between subjects with and without blepharitis. Thus, based on these data the relevance of Demodex in blepharitis might be questioned. On the other hand, there are other studies showing some relationships between presence of Demodex and blepharitis [15, 16]. Probably not only the presence, but also the density of parasites plays an important role during disease development. Interestingly, we observed that Demodex was more prevalent in participants having eye glasses, but not in those wearing contact lenses. This observation is difficult to explain. It may be biased by the small number of participants with contact lenses (n = 20) and definitely needs further confirmation.
Higher parasite prevalence was noted in older people, a finding that has been reported previously [15]. It is probable that changes of the sebum composition and increased activity of sebaceous glands which occur with age may facilitate the growth of mites in older people [17]. On the other hand, one may argue that with age the chance of becoming infested is higher as the duration of life is longer. We have also asked our participants about housing, because we suspected that living e.g. in old buildings with wooden ceilings and higher dust density could affect the incidence of infestation. However, we could not confirm our hypothesis as there were no differences between people living in old houses and those living in newer ones.
One of the most important findings of the current study was the observation that prevalence of Demodex spp. in drug abusers, who in the vast majority were infected with HIV, did not differ significantly from the other groups. We believe that HIV positive subjects are not more susceptible to developing demodicosis than other people unless deep immunosuppression occurs. Currently the majority of HIV-infected patients are receiving potent anti-retroviral therapy; thus probably most of them were not immunocompromised enough to facilitate infestation with Demodex spp. It seems that only in severely immunosuppressed cases might Demodex be more prevalent than in the general population [18, 19].
In summary, our results indicate that the role of Demodex as a pathogenic parasite in humans is still controversial. Certainly it may be responsible, at least in some people, for blepharitis and other ocular problems; however, many subjects infested by this mite demonstrate no clinical symptoms related to the infestation. Therefore, further, prospective, probably multicenter studies are needed to gain better insight into the biology, epidemiology and pathology of Demodex spp.
In conclusion, Demodex spp. is a common saprophyte found in human eyelash follicles. Its presence might be related to some ocular discomfort; however, in the vast majority of people the infestation seems to be asymptomatic.
Acknowledgments
We would like to thank Richard Ashcroft for correction of the manuscript.
Appendix 1
References
- 1.Raszeja-Kotelba B, Jenerowicz D, Izdebska JN, Bowszyc-Dmochowska M, Tomczak M, Dembińska M. Some aspects of the skin infestation by Demodex folliculorum. Wiad Parazyt. 2004;50:41–54. [PubMed] [Google Scholar]
- 2.Nutting WB, Green AC. Pathogenesis associated with hair follicle mites (Demodex spp.) in Australian Aborigines. Br J Dermatol. 1976;94:307–12. doi: 10.1111/j.1365-2133.1976.tb04388.x. [DOI] [PubMed] [Google Scholar]
- 3.Lacey N, Kavanagh K, Tseng SC. Under the lash: Demodex mites in human diseases. Biochem (Lond) 2009;31:2–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Desch C, Nutting WB. Demodex folliculorum (Simon) and D. brevis Akbulatova of man: redescription and reevaluation. J Parasitol. 1972;58:169–77. [PubMed] [Google Scholar]
- 5.Rojas M, Riazzo C, Callejón R, Guevara D, Cutillas C. Morphobiometrical and molecular study of two populations of Demodex folliculorum from humans. Parasitol Res. 2012;110:227–33. doi: 10.1007/s00436-011-2476-3. [DOI] [PubMed] [Google Scholar]
- 6.Liu J, Sheha H, Tseng SC. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10:505–10. doi: 10.1097/ACI.0b013e32833df9f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Filho PA, Hazarbassanov RM, Grisolia AB, Pazos HB, Kaiserman I, Gomes JÁ. The efficacy of oral ivermectin for the treatment of chronic blepharitis in patients tested positive for Demodex spp. Br J Ophthalmol. 2011;95:893–5. doi: 10.1136/bjo.2010.201194. [DOI] [PubMed] [Google Scholar]
- 8.Hsu CK, Hsu MM, Lee JY. Demodicosis: a clinicopathological study. J Am Acad Dermatol. 2009;60:453–62. doi: 10.1016/j.jaad.2008.10.058. [DOI] [PubMed] [Google Scholar]
- 9.Elston DM. Demodex mites: facts and controversies. Clin Dermatol. 2010;28:502–4. doi: 10.1016/j.clindermatol.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Kemal M, Sümer Z, Toker MI, Erdoğan H, Topalkara A, Akbulut M. The prevalence of Demodex folliculorum in blepharitis patients and the normal population. Ophthalmic Epidemiol. 2005;12:287–90. doi: 10.1080/092865805910057. [DOI] [PubMed] [Google Scholar]
- 11.Cielecka D, Salamatin R, Garbacewicz A. Usage of the Hoyer's medium for diagnostics and morphological studies of some parasites. Wiad Parazytol. 2009;55:265–70. [PubMed] [Google Scholar]
- 12.Witmanowski H, Lewandowicz E, Sobieszek D, et al. Evaluation of surgical treatment of rhinophyma with tangential shear of the lesion. Postep Derm Alergol. 2012;29:411–6. [Google Scholar]
- 13.Dominey A, Rosen T, Tschen J. Papulonodular demodicidosis associated with acquired immunodeficiency syndrome. J Am Acad Dermatol. 1989;20:197–201. doi: 10.1016/s0190-9622(89)70021-9. [DOI] [PubMed] [Google Scholar]
- 14.Raju VK, Raju LV, Kheirkhah A. Demodex blepharitis. Ophthalmology. 2012;119:200. doi: 10.1016/j.ophtha.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 15.Czepita D, Kuźna-Grygiel W, Kosik-Bogacka D. Investigations on the occurrence as well as the role of Demodex folliculorum and Demodex brevis in the pathogenesis of blepharitis. Klin Oczna. 2005;107:80–2. [PubMed] [Google Scholar]
- 16.Lee SH, Chun YS, Kim JH, Kim ES, Kim JC. The relationship between Demodex and ocular discomfort. Invest Ophthalmol Vis Sci. 2010;51:2906–11. doi: 10.1167/iovs.09-4850. [DOI] [PubMed] [Google Scholar]
- 17.Dhingra KK, Saroha V, Gupta P, Khurana N. Demodex-associated dermatologic conditions – A coincidence or an etiological correlate. Review with a report of a rare case of sebaceous adenoma. Pathol Res Pract. 2009;205:423–6. doi: 10.1016/j.prp.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 18.Clyti E, Sayavong K, Chanthavisouk K. Demodecidosis in a patient infected by HIV: successful treatment with ivermectin. Ann Dermatol Venereol. 2005;132:459–61. doi: 10.1016/s0151-9638(05)79308-x. [DOI] [PubMed] [Google Scholar]
- 19.Sarro RA, Hong JJ, Elgart ML. An unusual demodicidosis manifestation in a patient with AIDS. J Am Acad Dermatol. 1998;38:120–1. doi: 10.1016/s0190-9622(98)70554-7. [DOI] [PubMed] [Google Scholar]