Brief Summary
We propose that complex (nonlinear) fluctuations of hemodynamic variables (including systemic blood pressure parameters) during cardiovascular surgery contain information relevant to risk assessment and intraoperative management. Preliminary analysis of a pilot study supports the feasibility and potential merits of performing a larger, prospective study to assess the clinical utility of such new dynamical measures and to evaluate their potential role in enhancing contemporary approaches to risk assessment of major adverse events.
Introduction
As the population ages, increasing numbers of elderly patients with multiple co-morbid conditions are presenting for high-risk cardiovascular surgical procedures. The commensurate increase in perioperative major adverse events (MAEs) increases mortality by 1.4 to 8-fold,1 with an estimated 1 billion dollars annually spent on managing these complications.2 Current MAE risk prediction indexes3,4 are typically based on static or “snapshot” measures, such as the presence or absence of a co-morbid condition like hypertension. Unfortunately, these indexes have failed to adequately predict which high-risk patients will have MAEs5–7 possibly, at least in part, because they do not take into consideration the complex (nonlinear), time-varying features of physiological hemodynamic signals. Furthermore, a “one-size-fits-all” risk prediction model approach is unlikely to accurately identify patients at high risk5–7 particularly at extremes of age and predicted risk.8–13
A major motivation for the program outlined here is that current risk prediction tools may be improved by incorporating dynamical properties of physiologic signals, thereby enhancing: (a) individual patient risk assessment and counseling, (b) design of timely interventions to prevent disabling or fatal complications (e.g., stroke, renal failure, atrial fibrillation and myocardial infarction), and (c) the accuracy of comparisons of provider and hospital performances. Toward this end, our goal is to develop a real-time blood pressure variability (BP variability) index or set of indexes incorporating a patient's own baseline and evolving pathophysiologic characteristics into current “snapshot” scoring systems.4,5,14
One of the most important physiologic signals obtained in the perioperative period is the continuously recorded systemic BP signal.15 While the optimization of BP is a major perioperative target there is no universally accepted guideline for defining hypotension. Furthermore, hypotensive episodes, are dynamic, not static phenomena and not only vary from patient to patient but also within a patient at different surgical stages.
Therefore, measures of BP variability, quantified using different metrics, have been the focus of considerable interest. For example, in one study,16 BP variability was defined as the time spent above or below a target systolic blood pressure range of 95–135 mm of Hg, and an increased BP variability value was associated with higher 30-day mortality. In another study, BP variability was defined as the root mean successive square difference of a moving 5 second time period. In this investigation17, decreased intracranial pressure and BP variability were shown to predict long-term adverse outcome after aneurysmal subarachnoid hemorrhage.
An intuitive limitation of traditional measures of variability is the fact that they do not take into consideration the temporal structure of a sequence of measurements. For example, the following two sequences: A = {1 2 3 2 1 2 3 2 1 2 3 2 1} and B ={1111222222333}16, have the same variability, as measured by amplitude of range and standard deviation, but completely different structures. In fact, while sequence A defines a triangular wave, sequence B is a step function. Measures that are sensitive to the temporal organization of a signal have been essential in characterizing and discriminating different dynamical systems.
Here we assess BP fluctuation (variability) dynamics via two complementary metrics: 1) traditional standard deviation of BP time series and 2) the degree of complexity of their dynamics. The motivating framework for quantifying the degree of complexity of nonlinear physiologic signals, such as BP, is that complexity reflects the degree of robustness/resilience of the underlying control mechanisms, and it decreases with aging and pathology (http://physionet.org/tutorials/cv/, accessed Oct 21, 2013).
The term nonlinear may be unfamiliar to readers of physiologic and clinical journals. Linear systems exhibit two properties: proportionality and superposition. Proportionality, as implied by the term, means that there is a straight-line relationship between input and output. Superposition indicates that one can completely understand the system (e.g., a Rube Goldberg-type device) by breaking it down into multiple sub-components. In contrast, the sub-components of a non-linear system do not “add up” to the whole because of either “constructive” or “destructive” interactions between those sub-components. In these cases, reductionist strategies will fail to provide full understanding of a given system.18,19 Furthermore, in nonlinear systems, unanticipated (“off-target”) effects are likely since small input changes may induce major changes in the output (the “so-called “butterfly effect”).
Pilot Study: Overview
In this pilot study, we tested the feasibility of: i) acquiring BP waveform data of sufficient length and quality for nonlinear complexity analyses, and ii) converting the data from a proprietary to an open-source format. Our specific hypothesis is that the complexity of the dynamics of systolic arterial (SAP), diastolic arterial (DAP) and pulse pressure (PP) from the post-bypass period is lower for the group of patients with MAEs (cases) than for a control group with comparable risk but no MAEs. We included pulse pressure dynamics in light of evidence that abnormalities in pulse pressure has been independently associated with up to 3-fold increase in MAEs following cardiac surgery.20
Methods
Pilot Study Population
Our institution collaborates in the Multiparameter Intelligent Monitoring in Intensive Care II (MIMIC II) data collection program with the Massachusetts Institute of Technology (MIT).21 The MIMIC II project involves collection of all clinical and bedside monitoring data from patients in critical care bed and has been approved by the Institutional Review Boards of Beth Israel Deaconess Medical Center and MIT. Recently, we expanded the MIMIC II project to the operating room (OR) by collecting all monitoring data during cardiovascular surgery.
Metadata including type and duration of surgery, preoperative medications, intraoperative anesthetic, and surgical events (anesthetic induction, surgical incision, bypass time, post bypass period, chest closure, and surgery end) were collected from the Anesthetic Information Management Systems (AIMS; Philips CompuRecord). Time-stamped data reporting the anesthetic dosage (end-tidal agent concentration, minimal alveolar concentration of anesthetic) and details of circulatory support were collected from the hospital's AIMS systems. The deidentified metadata were then integrated into the STS system which also served as the source of preoperative ontology definitions, including demographic data, comorbid conditions, inotropic support, STS predictive risk index for morbidity and 30-day mortality, surgery type and postoperative adverse outcome information. Standard STS definitions were used to adjudicate endpoints (http://www.sts.org/doc/4862; Accessed Sep 25, 2010) and to report the postoperative outcome.
Twenty patients with MAEs admitted for cardiac surgery at the Beth Israel Deaconess Medical Center between the months of November 2009 and Feb 2010 were chosen for the pilot study. Twenty controls, without MAEs, matched for age, gender and body surface area were chosen from the same period.
Data Acquisition and Pre-processing
The monitoring data from the ORs are streamed at 125 Hz and 12-bit amplitude resolution to a dedicated, data-archiving server located within the secure environment of the Beth Israel Deaconess ORs. The data are retrieved from the server after completion of surgery and translated from a commercial system's (Philips, Andover, MA) proprietary data format to an open-source (WFDB) waveform data format. After data conversion, signal quality assessment is performed by visual inspection. We then used an open-source software algorithm22 to identify and annotate the onset of the arterial BP waveforms. We derived the beat-to-beat systolic and diastolic sequences of values that constitute the systolic and diastolic time series by determining the minimum and the maximum values of the BP waveforms in a neighborhood of the previously identified onsets.
Finally, for each beat, we coded and archived the stage to which the surgical procedure had progressed (pre-induction, induction, vessel harvesting, bypass, post-bypass). These procedure-specific hemodynamic data were integrated with the intraoperative surgical events and postoperative STS database.
For the pilot study presented here, we focused on the analysis of post-bypass SAP, DAP, and PP time series segments with a minimum of 95% usable data. The selection of data from this time period was based on the assumption that the period of time during which chest closure is being performed is likely to be a hemodynamically stable phase of surgery and relatively comparable between subjects.
Such segments (one per subject, Fig. 1) were available in 12 cases (one in-hospital death, two patients with post-operative renal failure and nine patients with new onset post-operative atrial fibrillation) and 11 control subjects. Segment length varied between 12 and 30 minutes (Table 1).
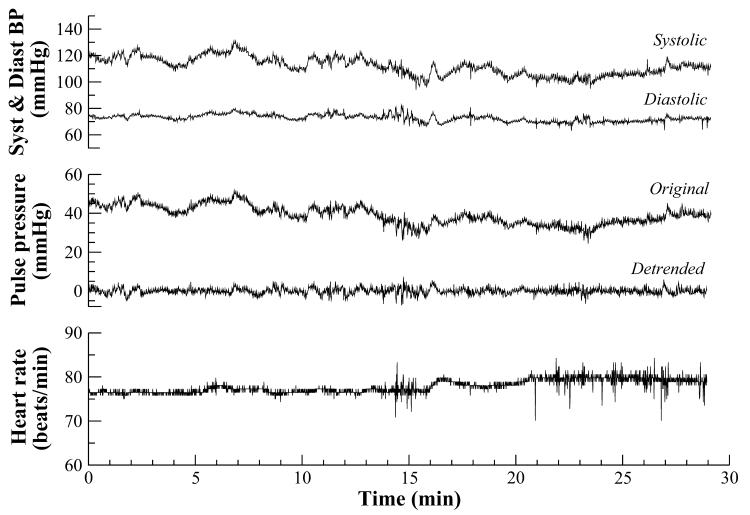
Figure 1.
Systolic, diastolic, pulse pressure and heart rate fluctuation time series from a control subject. Note: the heart rate time series were not analyzed because most patients had sustained electronic pacing that confounds heart rate variability analyses.
Table 1.
Demographic data for cases and controls
| Cases (n=12) | Controls (n=11) | `p' value | |
|---|---|---|---|
| Age (years) Mean±SD | 72 ± 10 | 62 ± 15 | 0.400 |
| Gender (male/female) | 7/5 | 6/5 | 1.000 |
| BSA (m2) Mean ± SD | 1.9 ± 0.3 | 1.9 ± 0.2 | 0.950 |
| Diabetes | 7 | 3 | 0.214 |
| Hypertension | 12 | 7 | 0.037* |
| Lung disease | 1 | 2 | 0.590 |
| Dialysis | 0 | 0 | 1.000 |
| Preoperative CHF | 3 | 2 | 1.000 |
| Preoperative CVA | 1 | 1 | 1.000 |
| Previous MI | 3 | 0 | 0.217 |
BSA-Body Surface Area, CHF-Congestive Heart Failure, CVA-Cerebrovascular accident, MI-Myocardial Infarction.
p value < 0.05 was considered significant
An automated algorithm, used to eliminate artifacts, excluded SAP values < 50 mm Hg and > 250 mm Hg; DAP values < 20 mm Hg and > 150 mm Hg; DAP ≥ SAP, and SAP – DAP < 10 mm Hg.
Signal analysis
For each of SAP, DAP and PP signals we calculated: 1) the mean, 2) the standard deviation for the entire length of the time series, a measure of the amount of variability around the mean value, and 3) a complexity index, computed using the multiscale entropy (MSE) method, which quantifies the information content of the signal over a range of scales (~1 – 10 seconds). Table 3 presents the group mean and standard deviation values for each of these measures.
Table 3.
Traditional and Complexity measures of Blood Pressure time series
| Cases (n=12) | Controls (n=11) | p value | |
|---|---|---|---|
| Mean (mm Hg) | |||
| Systolic | 117.71 ± 8.47 | 115.98 ± 6.09 | 0.603 |
| Diastolic | 67.75 ± 7.89 | 70.85 ± 4.53 | 0.064 |
| Pulse pressure | 49.99 ± 9.83 | 45.18 ± 8.34 | 0.280 |
| Standard Deviation (mm Hg) | |||
| Original time series | |||
| Systolic | 11.32 ± 4.07 | 10.89 ± 2.79 | 0.976 |
| Diastolic | 5.44 ± 2.47 | 7.97 ± 7.13 | 0.516 |
| Pulse pressure | 9.83 ± 2.78 | 8.34 ± 2.08 | 0.170 |
| Detrended time series | |||
| Systolic | 4.48 ± 1.31 | 3.61 ± 2.11 | 0.060 |
| Diastolic | 1.59 ± 0.48 | 1.84 ± 0.65 | 0.207 |
| Pulse pressure | 3.54 ± 0.96 | 3.02 ± 2.32 | 0.069 |
| Complexity index (unitless) | |||
| Systolic | 12.52 ± 2.72 | 15.50 ± 2.02 | 0.004 |
| Diastolic | 13.81 ± 1.98 | 15.45 ± 1.59 | 0.034 |
| Pulse pressure | 12.38 ± 2.97 | 15.60 ± 2.13 | 0.004 |
In addition to the original data segments, we also analyzed detrended time series, since non-stationarities, due to factors such as slow drifts of the baseline of a time series, can lead to misleadingly low complexity values. For an example of the type of non-stationarity (drift) that we removed, see the PP signal (original and detrended) shown in the middle plot of Fig. 1. For detrended, we employed an adaptive data decomposition method, called empirical mode decomposition.23 We preserved the first 4 components of the decomposed signals, which is equivalent to eliminating frequencies < 0.07 Hz. For the detrended signals, we also calculated the standard deviation values (the mean is approximately zero).
The MSE method24 quantifies the information content of a signal over multiple time scales. In practice, the algorithm comprises two steps: (1) a coarse-graining procedure that allows us to look at representations of the system's dynamics at different scales, and (2) the quantification of the degree of irregularity of each coarse-grained time series, which can be accomplished using a measure termed sample entropy.25 The graphical output of the MSE method is the entropy of a signal plotted as a function of scale factor (Fig. 2). The most complex time series have higher entropy values over a range of time scales. The number of scales probed depends on the length of the original time series. Typically, for a time series with N data points, the largest time scale n included in the analysis is such that N/n > 200. The SAP, DAP and PP time series are not evenly sampled because the timing of each value is determined by the cardiac interbeat interval cadence. Let {PP(t1), PP(t2), …PP(tN)} represent the PP time series where PP(ti) represents the value of PP at time ti. For scale 1 of the MSE curve, entropy is calculated for the original time series. For scale 2, entropy is calculated for the sequence of values obtained by averaging 2 consecutive data points of the original time series, that is, for the following sequence: (PP(t1) + PP(t2))/2, (PP(t3) + PP(t4))/2, (PP(t5) + PP(t6))/2, …). For scale 3, entropy is calculated for the sequence of values obtained by averaging 3 consecutive data points, [(PP(t1) + PP(t2) + PP(t3)]/3, [(PP(t4) + PP(t5) + PP(t6)]/3, …), and so forth.
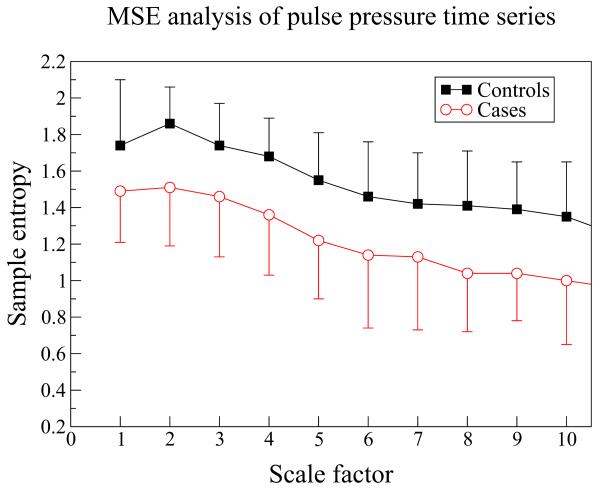
Figure 2.
Multiscale entropy (MSE) analysis of the detrended pulse pressure time series from the post-bypass period for the case and control groups. Symbols and error bars represent group means and standard deviation values.
In the general case, scale n, the entropy is calculated for the following sequence: (PP(t1) + ..+ PP(tn))/n, (PP(tn+1) + … + PP(t2n))/n, (PP(t2n+1) + … + PP(t3n))/n, …). In summary, to derive the coarse-grained time series for scale n, we divide the original signal into non-overlapping segments of length n and then take the average of each of these segments. The scale factor is the number of data points in each of these segments.
The coarse-graining of the time series allows us to quantify the structure of the signal on different time scales. Effectively, the coarse-graining procedure works as a low-pass filter. As an example consider an SAP time series. The timing of each SAP value is determined by the cardiac interbeat interval cadence. If heart rate is 60 bpm, then the SAP time series will be sampled at 1Hz and the coarse-grained SAP time series for scale 10 will be sampled at 0.1 Hz. Thus, by the Nyquist sampling theorem, the duration of the fastest oscillatory component of the coarse-grained SAP time series for scale 10 will be 20 seconds. MSE analyses encompassing scale factors 1 to 10 quantify the entropy of time series fluctuation patterns whose minimum duration range from 2 to 20 seconds and whose maximum duration range from 6 to 60 seconds. These values are also determined taking into consideration the value of a parameter (m=2) of the entropy algorithm that sets the length of the template vectors (see Costa et al. ref. 24–26 for details).
Statistical Analysis
Continuous data was analyzed with Wilcoxon rank sum test. Proportions were analyzed with Chi-square test. SPSS 18.0 (Chicago, IL) was used for analysis. P value < 0.05 was considered significant.
Results
The demographics and preoperative co-morbid conditions (excepting the history of hypertension) of cases and controls were comparable (Table 1). While preoperative medications, intraoperative cross clamp time, and bypass time were also comparable between the two groups, statin use was more common in cases than in controls (Table 2).
Table 2.
Preoperative medications, type of surgery and bypass times
| Cases (n=12) | Controls (n=11) | `p' value | |
|---|---|---|---|
| N (%) or Mean ± SD | N (%) or Mean ± SD | ||
| Beta blockade | 9 (75) | 8 (73) | 1.000 |
| ACE inhibitors | 10 (83) | 5 (45) | 0.089 |
| Aspirin | 10 (83) | 8 (73) | 0.640 |
| Statins | 12 (100) | 5 (45) | 0.005* |
| Type of surgery CABG ± valve Valve | 0.214 | ||
| 9 (75) | 5 (45) | ||
| 3 (25) | 6 (55) | ||
| Cross clamp time (min) | 70 ± 25 | 87 ± 24 | 0.100 |
| Bypass time (min) | 91 ± 27 | 114 ± 32 | 0.110 |
| STS Morbidity mortality (% Risk) | 18 ± 11 | 14 ± 11 | 0.390 |
ACE-Angiotensin Converting Enzyme Inhibitors
CABG-Coronary Artery Bypass Grafting surgery
STS-Society of Thoracic Surgery
p<0.05 is significant
The mean values of post-bypass SAP, DAP and PP were not significantly different between cases and controls. BP variability, defined as the standard deviations of the BP waveform derived time series, that is, the standard deviations of SAP, DAP and PP, were also not significantly different between the two groups. In contrast, the complexity indexes of SAP, DAP and PP were significantly lower for the groups of patients with MAEs than for controls. These differences cannot be attributed to differences in the magnitude of the fluctuations of the signals analyzed, since there were no significant differences between the standard deviation of the SAP, DAP and PP detrended time series used for the computation of the complexity index.
We note that oscillatory patterns in the systolic, diastolic and pulse pressure time series due to breathing will influence the values of the standard deviation of these time series as well as the entropy values for scale factors < 6. For scales 6 and above, the oscillatory patterns that could be due to breathing will have been filtered out through the coarse-graining procedure. Furthermore, Figure 2 clearly shows that the level of separation between the case and control groups remains approximately the same for all scales. Since in this study the complexity index was defined as the summation of the entropy values from scales 1 to 10, this index will be affected by oscillatory patterns due to breathing. However, when we calculate the complexity index for scales 1 to 5 (influenced by breathing) and for scales 6 to 10 (not influenced by breathing) separately, the same statistically significant degree of separation between the two groups was observed.
Discussion
Our preliminary findings are notable from the following three major perspectives. First, we established the feasibility of: i) acquiring BP waveform data of sufficient length and quality for nonlinear complexity analyses and, ii) converting the data from a proprietary to an open-source format. Second, we showed that the complexity of systolic, diastolic and pulse pressure time series derived from blood pressure waveform signals obtained during the post-bypass period were significantly lower in patients who had MAEs compared to those who did not. These results are consistent with our general underlying hypothesis that loss of signal complexity is associated with decreased physiologic adaptiveness and functional integrity. Support for this hypothesis derives from previous studies showing complexity loss with aging and a variety of pathologic conditions in multiple signals26, including heart rate in chronic heart failure and in trauma victims with increased mortality27, electroencephalograms in dementia28, body sway motions in older vs. younger subjects29 and heart rate of fetuses with intrauterine growth retardation vs. normally developing fetuses.30 Furthermore, to our knowledge, this pilot study is the first to use multiscale entropy to analyze intraoperative BP dynamics.
Third, we showed that traditional measures of BP variability, namely, the standard deviation of systolic, diastolic and pulse pressure time series, were not statistically different between cases and controls, in this pilot study. This result suggests that the difference between the BP dynamics of cases and controls is in encoded in the temporal sequence of BP values to which traditional measures of variability are insensitive.
We emphasize that we chose to study BP instead of HR fluctuations for a number of reasons. BP regulation determines organ perfusion and complex variability may be a surrogate measure of the cardiopulmonary reserve (adaptability) of a given patient. Furthermore, a substantial proportion of patients undergoing cardiac surgery have electronically paced rhythms in the perioperative period, obviating the utility of heart rate variability analyses.
Limitations
Not all relevant intraoperative data may get collected and stored due to electronic failures or the presence of electrical or mechanical artifacts.31 To overcome this potential limitation, important events such as induction, incision, as well as sternotomy, cannulation, and bypass times, were time-stamped and obtained from AIMS to examine the influence of these confounders on outcome by multivariate analyses. Major methodological challenges include the intrinsic nonstationarity of the data, extrinsic perturbations induced by surgical and anesthetic interventions, artifacts in the data, and missing data points.
Future directions
As a follow-up we are now performing a larger (n=600) NIH funded study to further assess the utility of complexity-related and other proposed measures32,33 of BP fluctuations in predicting MAEs. Our study will also help understand the mechanistic factors that influence BP fluctuations. To the extent that automated assessment of BP dynamics can be incorporated into real-time monitoring systems, this project has the potential to help identify modifiable “dynamical targets” and improve perioperative decision-making, management strategy, and resource allocation. Finally, BP dynamics can potentially be obtained preoperatively using continuous noninvasive monitors to assess risk and refine treatment plans.
Acknowledgement
We thank Michelle Doherty, STS data coordinator from the Department of Cardiothoracic Surgery, Beth Israel Deaconess Medical Center, Boston, MA. We thank Priyam Mathur, BS Bioinformatics, Department of Anesthesiology, Beth Israel Deaconess Medical Center, Boston, MA for her help in cleaning up the artifacts and digitizing the waveforms. We thank Dr. Brett A Simon, MD PhD, Beth Israel Deaconess Medical Center, Boston, MA for his incredible support in designing the study.
Work funded by:
We gratefully acknowledge support from the National Institutes of Health [grants R01 GM098406 (BS), K99/R00 AG030677 (MDC), R01GM104987 (ALG), and R01 EB0001659 (TH)], Wyss Institute for Biologically Inspired Engineering (ALG and MDC); the G. Harold and Leila Y. Mathers Charitable Foundation (ALG and MDC); the James S. McDonnell Foundation (MDC)].
Work attributed to Beth Israel Deaconess Medical Center, Boston, MA. 02215.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Glance LG, Osler TM, Mukamel DB, et al. Effect of complications on mortality after coronary artery bypass grafting surgery: evidence from New York State. J Thorac Cardiovasc Surg. 2007;134:53–58. doi: 10.1016/j.jtcvs.2007.02.037. [DOI] [PubMed] [Google Scholar]
- 2.Song HK, Diggs BS, Slater MS, et al. Improved quality and cost-effectiveness of coronary artery bypass grafting in the United States from 1988 to 2005. J Thorac Cardiovasc Surg. 2009;137:65–69. doi: 10.1016/j.jtcvs.2008.09.053. [DOI] [PubMed] [Google Scholar]
- 3.Higgins TL, Estafanous FG, Loop FD, et al. Stratification of morbidity and mortality outcome by preoperative risk factors in coronary artery bypass patients. A clinical severity score. JAMA. 1992;267:2344–2348. [PubMed] [Google Scholar]
- 4.Shahian DM, O'Brien SM, Filardo G, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 1--coronary artery bypass grafting surgery. Ann Thorac Surg. 2009;88:S2–S22. doi: 10.1016/j.athoracsur.2009.05.053. [DOI] [PubMed] [Google Scholar]
- 5.Asimakopoulos G, Al-Ruzzeh S, Ambler G, et al. An evaluation of existing risk stratification models as a tool for comparison of surgical performances for coronary artery bypass grafting between institutions. Eur J Cardiothorac Surg. 2003;23:935–941. doi: 10.1016/s1010-7940(03)00165-9. [DOI] [PubMed] [Google Scholar]
- 6.Pinna-Pintor P, Bobbio M, Colangelo S, et al. Inaccuracy of four coronary surgery risk-adjusted models to predict mortality in individual patients. Eur J Cardiothorac Surg. 2002;21:199–204. doi: 10.1016/s1010-7940(01)01117-4. [DOI] [PubMed] [Google Scholar]
- 7.Geissler HJ, Holzl P, Marohl S, et al. Risk stratification in heart surgery: comparison of six score systems. Eur J Cardiothorac Surg. 2000;17:400–406. doi: 10.1016/s1010-7940(00)00385-7. [DOI] [PubMed] [Google Scholar]
- 8.Constantinides VA, Tekkis PP, Senapati A. Comparison of POSSUM scoring systems and the surgical risk scale in patients undergoing surgery for complicated diverticular disease. Dis Colon Rectum. 2006;49:1322–1331. doi: 10.1007/s10350-006-0522-5. [DOI] [PubMed] [Google Scholar]
- 9.Maslow A, Casey P, Poppas A, et al. Aortic valve replacement with or without coronary artery bypass graft surgery: the risk of surgery in patients > or =80 years old. J Cardiothorac Vasc Anesth. 2010;24:18–24. doi: 10.1053/j.jvca.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 10.Tambyraja AL, Kumar S, Nixon SJ. POSSUM scoring for laparoscopic cholecystectomy in the elderly. ANZ J Surg. 2005;75:550–552. doi: 10.1111/j.1445-2197.2005.03428.x. [DOI] [PubMed] [Google Scholar]
- 11.Tamijmarane A, Bhati CS, Mirza DF, et al. Application of Portsmouth modification of physiological and operative severity scoring system for enumeration of morbidity and mortality (P-POSSUM) in pancreatic surgery. World J Surg Oncol. 2008;6:39. doi: 10.1186/1477-7819-6-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bollschweiler E, Lubke T, Monig SP, et al. Evaluation of POSSUM scoring system in patients with gastric cancer undergoing D2-gastrectomy. BMC Surg. 2005;15:5–8. doi: 10.1186/1471-2482-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burgos E, Gomez-Arnau JI, Diez R, et al. Predictive value of six risk scores for outcome after surgical repair of hip fracture in elderly patients. Acta Anaesthesiol Scand. 2008;52:125–131. doi: 10.1111/j.1399-6576.2007.01473.x. [DOI] [PubMed] [Google Scholar]
- 14.Gawande AA, Kwaan MR, Regenbogen SE, et al. An Apgar score for surgery. J Am Coll Surg. 2007;204:201–208. doi: 10.1016/j.jamcollsurg.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 15.Warner MA, Monk TG. The impact of lack of standardized definitions on the specialty. Anesthesiology. 2007;107:198–199. doi: 10.1097/01.anes.0000271863.20091.60. [DOI] [PubMed] [Google Scholar]
- 16.Aronson S, Stafford-Smith M, Phillips-Bute B, et al. Intraoperative systolic blood pressure variability predicts 30-day mortality in aortocoronary bypass surgery patients. Anesthesiology. 2010;113:305–312. doi: 10.1097/ALN.0b013e3181e07ee9. [DOI] [PubMed] [Google Scholar]
- 17.Kirkness CJ, Burr RL, Mitchell PH. Intracranial and blood pressure variability and long-term outcome after aneurysmal sub-arachnoid hemorrhage. Am J Crit Care. 2009;18:241–251. doi: 10.4037/ajcc2009743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldberger AL. Non-linear dynamics for clinicians: chaos theory, fractals, and complexity at the bedside. Lancet. 1996;347:1312–1314. doi: 10.1016/s0140-6736(96)90948-4. [DOI] [PubMed] [Google Scholar]
- 19.Goldberger AL. Giles f. Filley lecture. Complex systems. Proc Am Thorac Soc. 2006;3:467–471. doi: 10.1513/pats.200603-028MS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fontes ML, Aronson S, Mathew JP, et al. Pulse pressure and risk of adverse outcome in coronary bypass surgery. Anesth Analg. 2008;107:1122–1129. doi: 10.1213/ane.0b013e31816ba404. [DOI] [PubMed] [Google Scholar]
- 21.Saeed M, Villarroel M, Reisner AT, et al. Multiparameter Intelligent Monitoring in Intensive Care II: a public-access intensive care unit database. Crit Care Med. 2011;39:952–960. doi: 10.1097/CCM.0b013e31820a92c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zong W, Heldt T, Moody GB. An open-source algorithm to detect onset of arterial blood pressure pulses. Computers in Cardiology. 2003;30:259–262. [Google Scholar]
- 23.Huang NE, Shen Z, Long SR, et al. The Empirical Mode Decomposition and the Hilbert Spectrum for Nonlinear and Nonstationary Time Series Analysis. Proc R Soc London, Ser A. 1998;454:903–995. [Google Scholar]
- 24.Costa M, Goldberger AL, Peng CK. Multiscale entropy analysis of complex physiologic time series. Phys Rev Lett. 2002;89:68–102. doi: 10.1103/PhysRevLett.89.068102. [DOI] [PubMed] [Google Scholar]
- 25.Richman JS, Moorman JR. Physiological time-series analysis using approximate entropy and sample entropy. Am J Physiol Heart Circ Physiol. 2000;278:H2039–H2049. doi: 10.1152/ajpheart.2000.278.6.H2039. [DOI] [PubMed] [Google Scholar]
- 26.Costa M, Goldberger AL, Peng C-K. Multiscale entropy analysis of biological signals. Phys Rev E. 2005;71:021906-1–18. doi: 10.1103/PhysRevE.71.021906. [DOI] [PubMed] [Google Scholar]
- 27.Riordan WP, Jr, Norris PR, Jenkins JM, et al. Early loss of heart rate complexity predicts mortality regardless of mechanism, anatomic location, or severity of injury in 2178 trauma patients. J Surg Res. 2009;156:283–289. doi: 10.1016/j.jss.2009.03.086. [DOI] [PubMed] [Google Scholar]
- 28.Mizuno T, Takahashi T, Cho RY, et al. Assessment of EEG dynamical complexity in Alzheimer's disease using multiscale entropy. Clin Neurophysiol. 2010;121:1438–1446. doi: 10.1016/j.clinph.2010.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kang HG, Costa MD, Priplata AA, et al. Frailty and the degradation of complex balance dynamics during a dual-task protocol. J Gerontol A Biol Sci Med Sci. 2009;64:1304–1311. doi: 10.1093/gerona/glp113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferrario M, Signorini MG, Magenes G. Complexity analysis of the fetal heart rate variability: early identification of severe intrauterine growth-restricted fetuses. Med Biol Eng Comput. 2009;47:911–919. doi: 10.1007/s11517-009-0502-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reich DL, Wood RK, Jr., Mattar R, et al. Arterial blood pressure and heart rate discrepancies between handwritten and computerized anesthesia records. Anesth Analg. 2000;91:612–616. doi: 10.1097/00000539-200009000-00022. [DOI] [PubMed] [Google Scholar]
- 32.Bishop SM, Yarham SI, Navapurkar VU, et al. Multifractal analysis of hemodynamic behavior: intraoperative instability and its pharmacological manipulation. Anesthesiology. 2012;117:810–821. doi: 10.1097/ALN.0b013e31826a4aa2. [DOI] [PubMed] [Google Scholar]
- 33.Soehle M, Czosnyka M, Chatfield DA, et al. Variability and fractal analysis of middle cerebral artery blood flow velocity and arterial blood pressure in subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2008;28:64–73. doi: 10.1038/sj.jcbfm.9600506. [DOI] [PubMed] [Google Scholar]