Abstract
Purpose
To quantify the number of required hours of nutrition education at U.S. medical schools and the types of courses in which the instruction was offered, and to compare these results with results from previous surveys.
Method
The authors distributed to all 127 accredited U.S. medical schools (that were matriculating students at the time of this study) a two-page online survey devised by the Nutrition in Medicine Project at the University of North Carolina at Chapel Hill. From August 2008 through July 2009, the authors asked their contacts, most of whom were nutrition educators, to report the nutrition contact hours that were required for their medical students and whether those actual hours of nutrition education occurred in a designated nutrition course, within another course, or during clinical rotations.
Results
Respondents from 109 (86%) of the targeted medical schools completed some part of the survey. Most schools (103/109) required some form of nutrition education. Of the 105 schools answering questions about courses and contact hours, only 26 (25%) required a dedicated nutrition course; in 2004, 32 (30%) of 106 schools did. Overall, medical students received 19.6 contact hours of nutrition instruction during their medical school careers (range: 0–70 hours); the average in 2004 was 22.3 hours. Only 28 (27%) of the 105 schools met the minimum 25 required hours set by the National Academy of Sciences; in 2004, 40 (38%) of 104 schools did so.
Conclusions
The amount of nutrition education that medical students receive continues to be inadequate.
Over the past three decades, numerous professional groups, scientific publications, and a congressional mandate have highlighted the need to improve the medical nutrition education that future physicians receive.1–4 Student groups have attempted to define the goals related to incorporating essential nutrition-related teaching into the curriculum,5 and a major funding initiative by the National Heart, Lung, and Blood Institute created the Nutrition Academic Award.6,7
There is little dispute that a patient’s dietary habits can influence chronic disease risk and treatment outcomes. Consumer surveys show that physicians are considered credible sources of nutrition information.8 However, more than half of graduating medical students still rate their nutrition knowledge as “inadequate,”9 and physicians report that they have not received adequate training to counsel their patients on appropriate nutrition.10–13 Surveys of medical students and physicians alike have found suboptimal knowledge with respect to nutrition facts.13–15
It has been nearly a quarter-century since the National Academy of Sciences published its groundbreaking report highlighting the insufficiency of nutrition education in the medical school curriculum.3 Our study attempted to answer two questions about that topic in the intervening 25 years. First, have medical schools responded to the challenge by improving nutrition knowledge and practice skills of future physicians? And, second, do most schools meet the minimum of 25 hours of nutrition education recommended by this landmark report on medical nutrition education?
Since 1995, the Nutrition in Medicine (NIM) Project at the University of North Carolina at Chapel Hill has developed a free, interactive, comprehensive nutrition curriculum for medical students.16 As part of the NIM mission, the NIM team surveys nutrition instructors at U.S. medical schools every few years. This effort aids the project in tracking trends related to the provision of nutrition instruction in medical school curricula and gives the team feedback that will help improve content and outreach. The existence of the data from these surveys provides the opportunity to compare newly collected data with data from previous surveys dating back to 2000.
The NIM team uses a survey methodology that goes deeper than usual by assessing more than the simple existence of a nutrition course for medical students. With the proliferation of integrated curricula and problembased learning paradigms, much of the nutrition instruction at medical schools currently is occurring outside of dedicated nutrition courses. The NIM Project’s 2008–2009 survey is designed to capture and quantify the instruction that occurs in different types of courses across the four years of the undergraduate medical curriculum. An important facet of the methodology is that the NIM database of medical school contacts contains the names of the nutrition educators themselves—those who are actually providing the instruction— rather than the names of administrators, who would be reporting secondhand information.
Method
The NIM Project has administered similar types of surveys several times since 2000. In developing the 2008–2009 survey, we retained the wording of key questions from the 2000–2001 and 2004 surveys to allow direct comparison of the results through the years. Identical questions had to do with the type and total hours of nutrition education across the medical school curriculum. New questions pertained to the use of the online curriculum of the NIM Project, the ways in which it has influenced nutrition education, and whether the respondent is responsible for teaching residents and other physicians.
In August and September 2008, we emailed the online survey link to the NIM database contacts at 127 of the 130 U.S. medical schools accredited by the Association of American Medical Colleges (AAMC).17 The three U.S. medical schools not included in this survey would not be matriculating students until the fall of 2009, and thus the survey could not include them. The NIM database of medical school contacts is unique in that, in most cases, NIM Project staff members are in direct contact with the instructor, the person who is actually providing nutrition education to medical students. The NIM team continued to contact instructors via phone, fax, and e-mail through July 2009 to encourage them to complete the survey. Participation was voluntary.
The survey contained 13 items. As in previous surveys, the first question asked for the number of first-year medical students at that school, and the second question asked instructors to specify whether nutrition instruction was required, optional, or not offered at their medical schools. The third question asked them to estimate the total number of required nutrition contact hours, specifying in which years the instruction was provided (first and second years or third and fourth years). The fourth question asked respondents to indicate the type of course in which the nutrition content was taught (e.g., nutrition, physiology/pathophysiology, biochemistry, or an integrated curriculum). The fifth question asked them to specify whether they felt that the amount of instruction was sufficient.
Questions 6 through 9 had to do with the use and impact of the NIM Project curriculum at the respondent’s medical school. The survey concluded with questions 10 through 12, which inquired whether the respondent’s responsibilities included teaching preclinical students, clinical students, or residents. The final question, number 13, was an open field for comments.
All but one recipient used the online interface to fill out the survey. The remaining survey was completed over the telephone, and one of us (K.M.A.) manually entered those responses into the online form. The institutional review board at the University of North Carolina at Chapel Hill made the determination that this project was exempt.
When the data collection was complete, an NIM staff member produced a dataset from all of the entries, and we used a spreadsheet software program (Excel 2003; Microsoft Corp., Seattle, Washington) to carry out all calculations. We calculated means and standard errors for the current survey and for all previous survey years by using the same categories and procedures.
In performing computations related to the hours of required nutrition instruction, we coded optional hours as zero hours of required nutrition education. If the respondent estimated a range of hours (e.g., 15–20 hours), we used the midpoint of the range (e.g., 17.5 hours) in calculations. We reanalyzed all numbers from previous years’ surveys by using the same criteria.
We determined the total number of hours in the four years of medical school by adding the required hours of nutrition instruction in the first and second years to the hours occurring in the third and fourth years. In nine cases, a respondent indicated the number of hours of required instruction in the first and second years but was unable to estimate the number of hours of required instruction in the third and fourth years. In these cases, the analysis used zero hours for the third and fourth years.
Results
Surveys were returned from 109 of 127 U.S. medical schools, for an 86% response rate. Of these 109 schools, 103 (94%) reported that nutrition instruction was required. Four schools (4%) offered optional instruction only; one school (1%) reported that it did not offer any nutrition instruction, and the respondent for one school (1%) did not know the answer to the question.
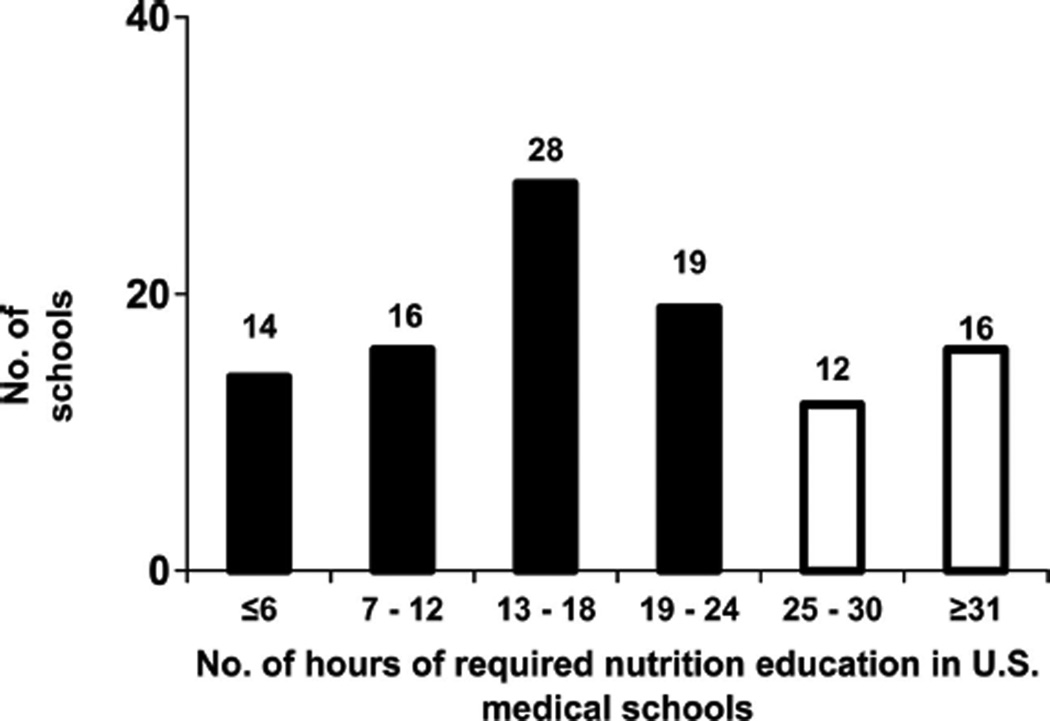
A total of 105 schools completed the portion of the survey regarding the number of nutrition contact hours. According to these responses, U.S. medical schools provided an average of 19.6 hours of required nutrition teaching (range: 0–70 contact hours). Only 27% (28/105) of U.S. medical schools responding to this question indicated that they provided the minimum of 25 hours recommended by the National Academy of Sciences in 1985.3 Thirty medical schools (29%) reported requiring 12 or fewer hours of nutrition instruction (Figure 1). Most of these contact hours took place during the first two years of medical training when students received an average (standard error of the mean [SEM]) of 15.4 (1.0) hours of required nutrition instruction. The third and fourth years provided an average (SEM) of only 4.2 (0.6) additional hours.
Figure 1.
Distribution of the total hours of required nutrition instruction at U.S. medical schools. Representatives from 109 U.S. medical schools responded to the 2008–2009 Nutrition in Medicine survey (105 schools provided data in response to this question; 4 schools did not). The graph compares the number of schools meeting the recommended minimum of 25 hours of required nutrition education (white bars) with the number of schools providing less than the minimum number of required hours (black bars). The number of schools at each level of required nutrition instruction is indicated above each bar.
Twenty-six schools specified that they had a course dedicated to nutrition. In 10 of those institutions, this course represented all of the available nutrition instruction. These dedicated nutrition courses provided an average of 16.4 nutrition contact hours (Table 1). Fifty-five schools provided some nutrition instruction within basic science courses (physiology or biochemistry); on average, each of these courses accounted for 6.2 hours or less.
Table 1.
Course Distribution of Required Nutrition Contact Hours in U.S. Medical Schools During 2008–2009*
| Type of course | Schools providing part of their required nutrition instruction in this format, no. |
No. of hours of nutrition teaching provided in this format, mean (SEM) |
|---|---|---|
| Nutrition | 26 | 16.4 (1.7) |
| Physiology, pathophysiology, or pathology | 36 | 5.7 (0.6) |
| Biochemistry | 48 | 6.2 (0.6) |
| Integrated curriculum | 62 | 11.9 (1.1) |
| Clinical practice | 49 | 6.4 (0.7) |
| Other† | 11 | 10.0 (3.1) |
One hundred nine U.S. medical schools responded to a survey conducted in 2008–2009; 100 schools responded to the question about the course distribution of their required nutrition education (three schools requiring nutrition education did not indicate the number of hours). Note that schools could offer nutrition education in more than one type of course. SEM indicates standard error of the mean.
Includes clerkships and clinical rotation lectures, clinical foundations, problem-based learning, nutrition selective, and organ-based modules.
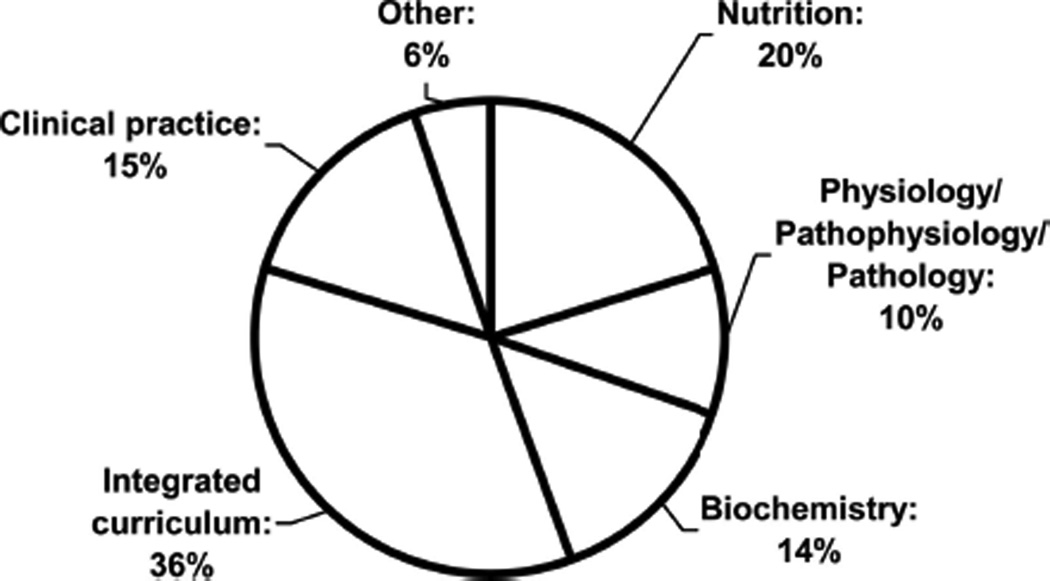
At U.S. medical schools, 80% of the nutrition instruction took place outside of designated nutrition courses (Figure 2). During the third and fourth years, 35 (33%) of the 105 schools answering this question offered five or more hours of nutrition instruction.
Figure 2.
Distribution of the required nutrition contact hours (i.e., the actual number of hours of nutrition education) among the various types of medical school courses. Representatives from 109 U.S. medical schools responded to the 2008–2009 Nutrition in Medicine survey (100 schools provided data in response to this question; 9 schools did not). The chart shows the distribution of required nutrition instruction throughout medical school curricula, whether in a designated nutrition course (20%) or integrated into other courses or learning environments (80%).
More than three-quarters of the medical school instructors (84/107, or 79%) surveyed indicated that students at their institution need more nutrition instruction, whereas 16 (15%) of them said that the students did not need more nutrition instruction. Only 8 of these 16 instructors were at schools offering more than the national average number of hours of nutrition instruction. The remaining 7% of instructors said that they did not know whether their students needed more nutrition education. (The total percentage exceeds 100% because of rounding of individual percentages.)
Table 2 more clearly illustrates the current situation by presenting a comparison of key data points from this survey and of those from surveys of previous years18,19; all three surveys used the same methodology and (with one exception in the 2000–2001 survey) asked the same core questions. Of the three national surveys, the most recent survey found the lowest number of schools that require a nutrition course, the lowest percentage of schools that provide a total of at least 25 hours of nutrition education, and the lowest average number of required nutrition contact hours. None of these differences reached statistical significance, however.
Table 2.
Comparisons Over Time of Selected Survey Data From U.S. Medical Schools With Respect to Nutrition Education*
| Item | 2000–2001 survey | 2004 survey | 2008–2009 survey |
|---|---|---|---|
| Average required nutrition contact hours, no.*† | 20.4 | 22.3 | 19.6 |
| Schools with required nutrition course, % (no./total) | 35 (39/112) | 30 (32/106) | 25 (26/105) |
| Schools requiring ≥25 hours of nutrition education, % (no./total) | 32 (36/112) | 38 (40/104)‡ | 27 (28/105) |
| Instructors who think more nutrition education is needed, % | — | 88 | 79 |
All U.S. medical schools were surveyed at three distinct times: 2000–2001, 2004, and 2008–2009 (the current survey). The surveys used identically worded core questions (the only exception is that the question reflected in the bottom row was not asked on the 2000–2001 survey). The response rates from the three surveys were 89%, 84%, and 86% from 2000–2001, 2004, and 2008–2009, respectively.
The averages represent data from all schools providing quantifiable responses. Schools reporting only optional nutrition instruction were coded as having zero hours of required nutrition instruction.
Two schools did not provide a response to this survey question.
Discussion
Our study shows that nutrition education continues to be very limited in most medical schools, a situation that casts doubt on the readiness of future physicians to effectively counsel their patients about appropriate nutrition. How did we determine that the current amount of nutrition education is “inadequate?” There are two major recommendations in the literature about this topic. One is the 1985 National Academy of Sciences report that suggests 25 hours of nutrition instruction as a minimum,3 and the other is the 1989 American Society of Clinical Nutrition recommendation that 37 to 44 hours be dedicated to nutrition instruction during medical school.20 By either standard, medical schools are falling far short of providing adequate training.
There are many medical schools, however, that manage to incorporate at least 25 hours of nutrition education into their curricula in any given year. We examined the 86 medical schools from which we had data for all three NIM Project surveys over the past 10 years. In each survey, a total of 28 of those schools met or exceeded this minimum standard, but they were not the same 28 institutions in every survey. Only nine schools provided at least 25 hours of nutrition instruction in all three surveys, which attests to the persistently tenuous state of nutrition education at most medical schools. There seems to be a great deal of flux from year to year in the number of hours of nutrition instruction offered, as indicated by the periodic NIM Project surveys.
According to the 2008–2009 survey, most instructors still believe that the amount of nutrition education in the curriculum is inadequate. A small majority of students share this view. AAMC last included a nutrition question in its graduation questionnaire in 2005. At that time, 51.1% of all U.S. medical students reported that the time devoted to nutrition in the curriculum was inadequate.9 So it seems that, overall, graduating medical students and instructors alike continue to be dissatisfied with the amount of nutrition education in U.S. medical schools.
It is important to note that 80% of the nutrition instruction in medical schools is not specifically identified as such in the curriculum. Nutrition instruction provided outside of designated courses could be considered diluted in importance—presented as an aside, instead of being given the emphasis it deserves as a core component of modern medical practice.
In addition, it still appears that most of the nutrition instruction that does occur in medical schools takes place during the preclinical years—the first two years of medical training. It may be more beneficial, however, to emphasize nutrition during the later clinical years, when the student can see the direct correlation between nutrition principles and medical treatment.
Several reports suggest that recent medical school graduates feel unprepared to intervene in their patients’ care with regard to nutrition.9,11,21,22 Recent surveys of residents and practicing physicians support this view,10,13 especially with regard to the growing problem of obesity.22–25 This deficit in preparation is rather alarming, considering the importance of nutrition in obesity prevention and the critical role of diet in the energy balance equation.
There are many challenges to bringing more nutrition education into medical schools’ curricula. In the past, its absence or scarcity seemed to be a consequence of a lack of expert nutrition faculty who could advocate for incorporating nutrition into the undergraduate and residency curricula and who could serve as role models in demonstrating how nutrition can be applied to modern medical practice.26,27 Another, more recent barrier is the lack of time for new courses or additional lectures.27 The NIM Project has developed an online curriculum that addresses both of these challenges.16 Through this online resource, fully developed content is available to supplement the curriculum when a faculty member trained in nutrition is not available, and the individual online modules contain units that can be customized for the amount of time available to any instructor. Even though this resource can be used at no cost by any medical school instructor wishing to incorporate nutrition into existing courses or clerkships, the amount of nutrition instruction at medical schools is still not where it should be.
Strengths
Some strengths of the current survey administration must be noted. One of these strengths is that identical questions have been used for three consecutive survey administrations, a practice that allows direct comparisons across time. Before 2000, the NIM Project administered several similar surveys, so there were multiple chances to improve and refine the wording of the questions. We obtained response rates of 86% in the 2008 –2009 survey, 84% in the 2004 survey, and 89% in the 2000 –2001 survey—rates much higher than those in many surveys reported in the literature. Another of these strengths is that the method we used targets the person at each medical school who is likely to be the most knowledgeable about the nutrition curriculum. All but eight respondents are actually involved in nutrition teaching of first- and second-year medical students at their schools (and six of those eight teach more advanced students, which leaves only two respondents who claimed to be knowledgeable about the curriculum but were not actually teaching nutrition). Thus, the responses to this survey came from faculty who are contributing directly to nutrition education, and we did not rely on reports from administrators or other faculty. Despite the difficulties in quantifying an entity as diverse as nutrition instruction across a four-year curriculum, we present these results with confidence.
Limitations
The survey methodology had some limitations. Respondent self-selection bias was possible, because the survey was voluntary. If anything, however, we feel that this bias might overestimate the amount of nutrition education, because nutrition educators, with whom we have an established relationship, may feel more compelled to answer the survey. With a response rate of 86%, however, this bias should not be so pronounced. There is an inherent uncertainty about how different instructors estimated the hours of nutrition, given that nutrition is a broad topic that is not always clearly defined. It is possible that different instructors at the same institution would use different definitions and, thus, give different answers.
The amount of nutrition education required during the third and fourth years of medical school is difficult to estimate, given that much of this instruction occurs during clerkships under different instructors. Because many more instructors in medical schools are involved in clinical teaching than are involved in basic sciences curricula, it is plausible that an instructor familiar with the basic sciences curriculum may underestimate the amount of instruction provided in the second half of the medical curriculum. To further examine this possibility, we conducted a separate analysis comparing responses of clinicians with those of basic science instructors. The schools of respondents who self-identified as “clinical” instructors provide a similar number of nutrition education hours as do the schools of instructors with basic science orientation.
Future surveys of this type, with additional resources, could include multiple instructors at the same institution in an attempt to confirm and complete the responses provided. In addition, if attempts were made to systematically survey clinical instructors, the information gained would add to the understanding of the depth and breadth of nutrition instruction during the third and fourth years of medical school.
Conclusions
The teaching of nutrition in U.S. medical schools still appears to be in a precarious position, lacking a firm, secure place in the medical curriculum of most medical schools. Concerns remain that many future physicians will lack adequate preparation in this essential component of modern medical practice. Despite these challenges, a minority of medical schools still manage to provide substantial nutrition training for their students. Medical school faculty should encourage administrators to retain the nutrition education currently offered and expand it to provide, at a minimum, the 25 nutrition education hours needed to properly train physicians.
Acknowledgments
The authors gratefully acknowledge all of the medical school faculty members who completed surveys and express appreciation to the Nutrition in Medicine Project advisory board.
Funding/Support: The Nutrition in Medicine Project was supported in part by grant no. R25 CA65474 from the National Cancer Institute and the Office of Dietary Supplements, National Institutes of Health, and by grant no. DK56350 from the University of North Carolina Clinical Nutrition Research Unit.
Footnotes
Other disclosures: None.
Ethical approval: The institutional review board at the University of North Carolina at Chapel Hill made the determination that this project was exempt.
Contributor Information
Kelly M. Adams, Department of Nutrition, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
Martin Kohlmeier, Department of Nutrition, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
Steven H. Zeisel, Department of Nutrition, and director, Nutrition Research Institute, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
References
- 1.Bruer RA, Schmidt RE, Chapel T. Nutrition Education for Physicians: Alternative Federal Roles for Creating an Improved System. Bethesda, Md: Richard Schmidt Associates. Ltd.; 1993. [Google Scholar]
- 2.Davis CH. The report to Congress on the appropriate federal role in assuring access by medical students, residents, and practicing physicians to adequate training in nutrition. Public Health Rep. 1994;109:824–826. [PMC free article] [PubMed] [Google Scholar]
- 3.National Research Council Committee on Nutrition in Medical Education. Nutrition Education in U.S. Medical Schools. Washington, DC: National Academy Press; 1985. [Google Scholar]
- 4.National Nutrition Monitoring and Related Research Act of 1990. Pub L No. 1101-445/HR1608, Section 302(1990). [Google Scholar]
- 5.Report of the American Medical Student Association’s Nutrition Curriculum Project. Essentials of nutrition education in medical schools: A national consensus. Am J Clin Nutr. 1997;65:1559–1561. doi: 10.1093/ajcn/65.5.1559. [DOI] [PubMed] [Google Scholar]
- 6.Pearson TA, Stone EJ, Grundy SM, McBride PE, Van Horn L, Tobin BW NAA Collaborative Group. Translation of nutritional sciences into medical education: The Nutrition Academic Award Program. Am J Clin Nutr. 2001;74:164–170. doi: 10.1093/ajcn/74.2.164. [DOI] [PubMed] [Google Scholar]
- 7.Walker WA. Innovative teaching strategies for training physicians in clinical nutrition: An overview. J Nutr. 2003;133(suppl):541S–543S. doi: 10.1093/jn/133.2.541S. [DOI] [PubMed] [Google Scholar]
- 8.American Dietetic Association. Summary of findings: American Dietetic Association’s public opinion survey Nutrition and You: Trends 2008. [Accessed May 10, 2010]; Available at: http://www.eatright.org/WorkArea/DownloadAsset.aspx?id=6442451351. [Google Scholar]
- 9.Association of American Medical Colleges. 2005 Medical School Graduation Questionnaire. [Accessed May 10, 2010];All Schools Report. Available at: http://www.aamc. org/data/gq/allschoolsreports/2005.pdf. [Google Scholar]
- 10.Darer JD, Hwang W, Pham HH, Bass EB, Anderson G. More training needed in chronic care: A survey of US physicians. Acad Med. 2004;79:541–548. doi: 10.1097/00001888-200406000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Kushner RF. Barriers to providing nutrition counseling by physicians: A survey of primary care practitioners. Prev Med. 1995;24:546–552. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 12.Levine BS, Wigren MM, Chapman DS, Kerner JF, Bergman RL, Rivlin RS. A national survey of attitudes and practices of primary-care physicians relating to nutrition: Strategies for enhancing the use of clinical nutrition in medical practice. Am J Clin Nutr. 1993;57:115–119. doi: 10.1093/ajcn/57.2.115. [DOI] [PubMed] [Google Scholar]
- 13.Vetter ML, Herring SJ, Sood M, Shah NR, Kalet AL. What do resident physicians know about nutrition? An evaluation of attitudes, self-perceived proficiency and knowledge. J Am Coll Nutr. 2008;27:287–298. doi: 10.1080/07315724.2008.10719702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Makowske M, Feinman RD. Nutrition education: A questionnaire for assessment and teaching. Nutr J. 2005;4:2. doi: 10.1186/1475-2891-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flynn M, Sciamanna C, Vigilante K. Inadequate physician knowledge of the effects of diet on blood lipids and lipoproteins. Nutr J. 2003;2:19. doi: 10.1186/1475-2891-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lindell KC, Adams KM, Kohlmeier M, Zeisel SH. The evolution of Nutrition in Medicine, a computer-assisted nutrition curriculum. Am J Clin Nutr. 2006;83(suppl):956S–962S. doi: 10.1093/ajcn/83.4.956S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Association of American Medical Colleges. Member medical schools. [Accessed May 10, 2010]; Available at: http:// www.aamc.org/medicalschools.htm. [Google Scholar]
- 18.Adams KM, Kohlmeier M, Zeisel SH. 2000–2001 Nutrition in Medicine survey of nutrition education at U.S. medical schools. Data file available from author at nimprof@unc.edu.. [Google Scholar]
- 19.Adams KM, Lindell KC, Kohlmeier M, Zeisel SH. Status of nutrition education in medical schools. Am J Clin Nutr. 2006;83(suppl):941S–944S. doi: 10.1093/ajcn/83.4.941S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weinsier RL, Boker JR, Brooks CM, et al. Priorities for nutrition content in a medical school curriculum: A national consensus of medical educators. Am J Clin Nutr. 1989;50:707–712. doi: 10.1093/ajcn/50.4.707. [DOI] [PubMed] [Google Scholar]
- 21.Mihalynuk TV, Scott CS, Coombs JB. Self-reported nutrition proficiency is positively correlated with the perceived quality of nutrition training of family physicians in Washington State. Am J Clin Nutr. 2003;77:1330–1336. doi: 10.1093/ajcn/77.5.1330. [DOI] [PubMed] [Google Scholar]
- 22.Mihalynuk TV, Knopp RH, Scott CS, Coombs JB. Physician informational needs in providing nutritional guidance to patients. Fam Med. 2004;36:722–726. [PubMed] [Google Scholar]
- 23.Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: Attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110(1 pt 2):210–214. [PubMed] [Google Scholar]
- 24.Stettler N. The global epidemic of childhood obesity: Is there a role for the paediatrician? Obes Rev. 2004;5:91–92. doi: 10.1111/j.1467-789X.2004.00138.x. [DOI] [PubMed] [Google Scholar]
- 25.Jay M, Gillespie C, Ark T, et al. Do internists, pediatricians, and psychiatrists feel competent in obesity care? Using a needs assessment to drive curriculum design. J Gen Intern Med. 2008;23:1066–1070. doi: 10.1007/s11606-008-0519-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bringing physician nutrition specialists into the mainstream: Rationale for the Intersociety Professional Nutrition Education Consortium. Am J Clin Nutr. 1998;68:894–898. doi: 10.1093/ajcn/68.4.894. [DOI] [PubMed] [Google Scholar]
- 27.Kohlmeier M, Zeisel SH. Teaching preventive nutrition in medical schools. In: Bendich A, Deckelbaum RJ, editors. Preventive Nutrition: The Comprehensive Guide for Health Professionals. 3rd ed. Totowa, NJ: Humana Press, Inc.; 2005. pp. 889–899. [Google Scholar]