Abstract
Community-based participatory research (CBPR) has emerged to bridge the gap between research and primary-care practice through community engagement and social action to increase health equity. It is widely acknowledged that access to high-quality primary care services is important to the overall health of a community. Here, CBPR studies in a primary care setting are reviewed to assess the use of CBPR associated with common health problems seen in primary care such as access to care and disparities in chronic disease management across vulnerable populations. CBPR involves building relationships with local communities, determining areas of need and establishing priorities for health concerns. Studies showing improved access to care for a Hispanic population, reduced asthma symptoms and weight loss are highlighted.
Keywords: CBPR, community-based, participatory research, community engagement, primary care delivery
Community-based participatory research (CBPR) is a widely accepted collaborative approach to research that works to understand and protect public health by involving all partners in the research process [1]. CBPR has emerged in the last decades to bridge the gap between science and practice through community engagement and social action to increase health equity [2]. The NIH definition of CBPR emphasizes that key stakeholders are fully involved in each stage of the research, from the study's conception to its design, analysis and communication of results [3]. Additionally, new efforts in funding patient-centered research through the Patient-Centered Outcomes Research Institute emphasize stakeholder engagement in research. CBPR can be especially useful in a local context by allowing the participation of community members throughout the research process. Evidence generated through CBPR can be fed-back to community partners. Tangible evidence can be used to design new interventions and maintain community engagement. As a result, CBPR methodologies have become increasingly popular in a primary care research setting [3–5]. In addition, CBPR has become a way to blur the traditional social relationships between communities and health providers, enabling them to work together for a common mission.
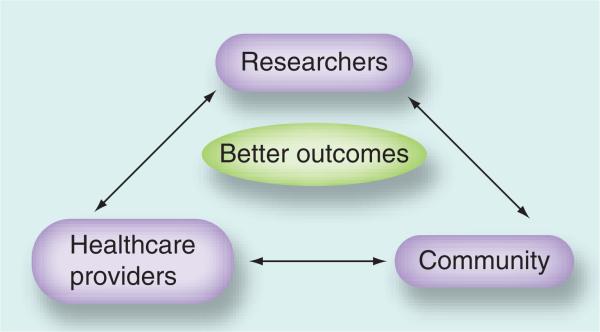
Participative Action Research (PAR) can be described as a family of research methodologies that pursue action (or change) and research (or understanding) at the same time. Action research is a way of generating research about a social system while simultaneously attempting to change that system. PAR is participative because change is usually easier to achieve when those affected by the change are involved in the research. CBPR is typically thought of as a type of PAR that is collaborative between researchers and community members. Here we also describe research that includes healthcare providers as part of the CBPR process (Figure 1).
Figure 1.
Using community-based participatory research to bring together researchers, healthcare providers and community stakeholders to improve health outcomes.
It is widely acknowledged that access to high-quality primary care services is imperative to the overall health of a community. Health benefits from an increased primary care physician supply include improved health outcomes in cancer, heart disease, stroke, infant mortality and life expectancy, among others [6,7]. Studies have shown that those using a primary care physician as their regular source of care have lower 5-year mortality rates than those using a specialist, controlling for all other factors [8]. In addition, populations served by a community health center are healthier than comparable populations receiving other types of care and receive more preventive services [9,10]. The chronic care model and adoption of this model by primary care as part of the Patient-Centered Medical Home has the potential to improve health outcomes and reduce overall medical costs [11]. Adoption of the elements of the chronic care model including an integrated approach to care by leveraging providers and community resources has been shown to impact patients with chronic diseases such as diabetes, asthma and congestive heart failure [12]. For example, with respect to integrated pest management, cockroaches are common asthma triggers. Prevention and reduction of asthma exacerbations are key to reducing mortality associated with asthma. Although most asthma exacerbations are treated in an outpatient setting, they present considerable difficulty for patients, including increased healthcare utilization, lost work productivity, school absences and increased healthcare costs. The implications of reducing trigger exposure to improve asthma care or the increased use of walking trails to limit diabetes and obesity have important implications for primary care physicians. While primary care physicians probably recommend exercise for patients as a matter of prevention for several chronic conditions, studies such as that by Zoellner et al. [13] examine the realities of patient's real-world experiences that promote or inhibit exercise in the community. The results from these CBPR projects guide primary care providers to more fully impact the health of the community it serves.
Using CBPR to study a community's access to primary care and the health problems commonly addressed in a primary care setting can help set the stage for real policy change on a local level to tackle health disparities and deficiencies. Analyses of the usefulness of CBPR have shown that collaboration among community members, researchers, providers and patients can lead to improvement in the overall health of a variety of communities and lessen health disparities [14]. Recently, CBPR has begun to be adapted in primary care settings, such as practice-based research networks (PBRNs) where groups of primary care practices come together not only to address the primary care of patients, but also with a mission to investigate questions related to community-based practice and to improve the quality of primary care [15–17]. Typical overlap topics of PBRN and CBPR research are health-care disparities, prevention, chronic disease management and mental health.
In the following review, CBPR studies in a primary care setting are reviewed to assess the use of CBPR to improve access to care and reduce health disparities. Topics explored are using CBPR to evaluate access to primary care services, as well as using CBPR to target common health problems and disparities primarily treated by primary care physicians (Table 1). In this review, we aim to demonstrate and detail the various applications of CBPR to clinical situations common in primary care. Later, challenges inherent in CBPR primary care research are addressed. This review was based on a search of PubMed, Ovid and Google using search terms around Community-Based Participatory Research and Primary Care. CBPR, primary care and participatory research were used as MeSH terms within PubMed, and related links were also examined. This literature search was not intended to represent an exhaustive literature survey or systematic review, but rather was based on identifying key research papers that demonstrated the use of CBPR in primary care applicable scenarios.
Table 1.
Community-based participatory research in primary care.
| Study (year) | Approach | Community participation | Results/outcomes | CBPR benefits | Ref. |
|---|---|---|---|---|---|
| Access to care | |||||
| Moreno et al. (2009) | Needs assessment | Conducted door-to-door surveys among community members for needs assessment. Held public hearings with community members to determine the concerns around and best location for a safety net medical clinic | Providers established a community health center on the campus of a local middle school through a partnership with the school district | Collaboration with community resulted in creation of a new community health center, thereby improving access to care | [21] |
| Kruger et al. (2010) | Surveys on health-related behaviors, attitudes and health insurance coverage | Community health surveys before, then both surveys and focus groups after expansion of the county health plan | Survey results used to gain support for the development and expansion of a county health plan that provides basic insurance for all uninsured low-income adults | Enhancement of basic insurance coverage for low-income adults in the community | [22] |
| Tapp et al. (2013) | Assessments of patient service areas and analysis of travel distance and cost | Provider discussion groups and patient surveys | Both patients and providers identified a culturally targeted, patient-centered medical home, with continuity of care as the ideal for receiving care | For each clinic, best practices were identified through discussion groups and surveys | [23] |
| Asthma | |||||
| Martin et al. (2010) | Culturally tailored education modules | Community, academic and medical partners communicated at every stage of the project from conception to results dissemination | Improved asthma disease outcomes. Decreased rates of hospitalizations | Improved asthma disease outcomes. Decreased rates of hospitalizations | [26] |
| Moreno et al. (2009) and Bonilla et al. (2005) | Screening to identify at-risk students. Family intervention to identify environmental and social factors related to asthma | Survey given to students. Results shared with school leaders who then supported and were involved in the development of community asthma intervention | 60% improvements in asthma control after 4 months | Asthma improvement among community members | [21,27] |
| Brenner et al. (2011, 2003) | Intervention trial to test an Integrated Pest Management program | Used existing partnership between researchers, community health centers and East Harlem (NY, USA) community members to design the research project. Together they decided to implement the pest reduction program. Community members suggested that the comparison group had to also receive an intervention of value, and injury prevention education was given to those not receiving an intervention | Decrease in cockroach infestation in low-income households | Not only improved pest management, but also gave injury prevention education to a control group | [5,28] |
| Levy et al. (2006) | Pest management, educational efforts, case management and support from community health advocates | Use of a decision-making committee, which included representation of all members. Included community participation during project conception, design and implementation | Significant reductions in 2-week recall respiratory symptom score and other asthma symptoms, such as wheezing and waking at night, as well as an improved asthma-related quality of life score | Improved respiratory status as a function of better pest management | [20] |
| Diabetes | |||||
| Parikh et al. (2010) | Prediabetes prevention strategy | Created a community action board, 75% of the membership were community members. Board developed methods for interventions to improve diabetes prevention | Sustained weight loss among participants | Sustained weight loss among participants | [34] |
| Jackson (2009) and Mau et al. (2010) | Diabetes Prevention Program – Lifestyle Intervention | Interviews and focus groups to culturally adapt research methods | Modified intervention led to successful weight loss | Modified intervention led to successful weight loss | [35,36] |
| Brown et al. (2010 and 2013) | Modified diabetes prevention program to target disproportionately high Type 2 diabetes rates in an American–Indian population | Formed collaboration with local Northern Plain American–Indian communities initially to seek funding together. Then held regular meetings between academic and community members to discuss study design, recruitment and sustainability | Feasible to implement health behavior and weight loss intervention to reduce risk of Type 2 diabetes in American–Indian youths | Determined feasibility of intervention and reduced rate of BMI increase among participants | [37,38] |
| Obesity/exercise | |||||
| Mabachi et al. (2012) | A community food assessment | Community member survey input used to tailor food access strategy | The survey results showed a desire for a grocery store in the neighborhood to improve food access and address the low frequency of fruit and vegetable consumption. The results were used to create a business plan to address the absence of healthy food access in the neighborhood | Created new food access strategy | [42] |
| Reininger et al. (2010) | Media campaign to reduce health risk | Community advisory boards determine the content and scope of the potential intervention. Also used focus groups to get community input on most important healthcare issues and media channels most often accessed for health information | Campaign to enhance the translation of currently recommended practices for physical activity and healthy food choices to Mexican–American individuals | Modified media campaign to improve health of specific community involved | [44] |
| Zoellner et al. (2012) | Community residents were surveyed to measure their physical activity, trail use and perceptions of the trails | Used community advisory board, and community members were able to participate in development, implementation and evaluation of research project. Some community members were trained to administer the surveys | Found association between trail usage and meeting physical activity recommendations. They found a need for greater invention efforts in areas of low physical activity that focus on residents’ perceptions of walking trail safety, conditions and amenities | Improved perception and usage of walking trails, which could have positive health implications for community members | [13] |
| Moreno et al. (2009) | Intervention to encourage daily physical activity | Initially used focus groups to determine community perceptions of walking groups. Also interviewed 200 families regarding exercise habits and views towards the walking group concept | Involved promotoras to establish a walking plan | Successfully encouraged local families to participate in walking groups, which could have positive health implications for community members | [21] |
| Maternal/child health | |||||
| Foster et al. (2012) | Examined community perceptions of maternal and newborn health services | Based on input from Dominican nurses and midwives, the research question about pregnant women with complications was developed. Researchers trained Dominican nurses and community leaders in CBPR, who then initiated focus groups and interviews | Elucidated a general dissatisfaction with the Dominican Republic's maternal health system, with many mothers and their families feeling disrespected, ignored and afraid | The dissemination of the co-created knowledge has forged new and positive working relationships between community members and healthcare providers | [48] |
| Bermudez-Millan et al. (2011) | Collected community experiences and perspectives regarding stress, discrimination and stressors that affect maternal health | Several focus groups consisting of community members to identify stressors to maternal health | Found significant stressors to maternal health and child health in their community to be poverty, instability of food, lack of quality education and unsafe environments | Future interventions can address the specific stressors found in this study | [51] |
CBPR: Community-based participatory research.
Use of CBPR to evaluate access to care
Existing studies using CBPR often focus on a specific intervention, such as community-based diabetes management [18] or a community intervention trial aimed at reducing asthma exacerbation rates using integrated pest management specifically to remove cockroaches [19,20]. By contrast, some studies focus more broadly on using CBPR to evaluate access to primary care. In a long-term partnership between the University of California, Los Angeles (UCLA; CA, USA) Department of Family Medicine (DFM) and an underserved Los Angeles (LA; CA, USA) community, CBPR was used to not only study prevalent diseases affecting the community, but also to address the lack of access to high-quality primary care clinics [21]. A needs assessment undertaken by medical students found that access to affordable and high-quality medical care was a high priority to the community [21]. As a result, the DFM established a community health center through a partnership with the LA school district. Rather than immediately building the clinic where they thought it would best serve the community, UCLA researchers sought community input for the location decision. Through public hearings, community members expressed concerns about having a clinic in a residential area that would attract ‘drug addicts’ and lower property values. As a result, Sun Valley Middle School (SVMS; CA, USA) was chosen and currently provides free services for students, as well as the entire community.
Increasing access to primary healthcare is not solely achieved through the creation or improvement of physical clinics. Researchers at the University of Michigan (MI, USA) used CBPR to facilitate the development of a county health coverage plan [22]. A Community Board consisting of representatives from academic, community, government and health sectors conducted the study, collecting information via telephone surveys on health-related behaviors, attitudes and status of random households from Genesee County (MI, USA). The survey included questions relating to health insurance coverage and helped bring to light the characteristics of uninsured adults. The authors indicate that in CBPR studies, there is often a gap between data collection/analysis and the actual shaping of policy decisions. However in this case, the CBPR-generated survey data were used to gain support for the development and expansion of a county health plan, the Genesee Health Plan. The Genesee Health Plan is a nonprofit organization that provides primary care services, prescription drugs and other care to uninsured and low-income adults in the county. As a result of the effective and useful partnerships created throughout the CBPR process, Genesee County became one of the first counties in the USA to provide basic healthcare for all uninsured, low-income adults [22].
While many primary care physicians believe themselves to be community oriented, the practice organizations in which they operate are not community oriented [20]. A cross-sectional investigation assessed the community orientation of four primary healthcare models in Ontario (Canada; fee-for-service practices, community health centers, family health networks and health service organizations), finding only the community health center model to be community oriented [9]. Although the study did not use CBPR methodologies, instead relying on provider and patient surveys and chart abstractions, the results suggest the need for improvement in the integration of primary care practices into the communities they serve.
Tapp et al. evaluated primary care delivery in an uninsured Hispanic immigrant population [23]. The research investigated key factors in primary care access using assessments of patient service areas, provider discussion groups, patient surveys and analysis of travel distance and cost. The research team selected four distinct primary healthcare delivery sites frequented by the target community – a community free clinic, low-overhead bilingual clinic, emergency department and hospital-affiliated clinic. Out of all the clinics, the low-overhead bilingual clinic demonstrated the greatest patient satisfaction and was also the clinic the patients traveled the longest distance to reach (an average of 8.3 miles) [23]. CBPR methods allowed the research team to qualitatively understand the nuances of transportation to the clinics and their affordability, as well as what the patients liked most about the care at the clinic they used and the factors influencing clinic selection.
This type of locally focused study offers deeper insights into healthcare access concerns within the specific target community. The traditional approach to this type of research often uses more aggregate data collected on a national or regional level [3]. However, research findings on a local scale are more likely to influence local health policy and lessen health disparities within the community. For example, through discussion groups and analysis of maps and travel distance, Tapp et al. were able to determine that there were large areas of the Hispanic population with no clinic representation. The results indicate provider interest in using the research to determine the locations of future satellite clinics to reach out into new or underserved communities. The relationships established between the researchers, patients, providers and Hispanic community members have created an infrastructure for changes that create a more efficient and streamlined healthcare delivery system.
CBPR & asthma
The severity and prevalence of asthma disproportionately affects vulnerable populations such as certain socioeconomic status and ethnic minority groups [24]. The disparities in asthma treatment and care can be attributed to a multitude of factors such as language barriers, environmental triggers, cultural beliefs, insurance and genetic factors [25]. Several CBPR studies aim to minimize these disparities through culturally tailored approaches to treatment and increased understanding of the environmental obstacles that asthma patients face within their communities.
In Puerto Rico, a culturally tailored asthma management intervention was created for pediatric patients [26]. The program, CALMA (a Spanish acronym for Take Control, Empower Yourself and Achieve Asthma Management), consisted of educational modules delivered by counselors in the homes of these children. During the development and implementation of the intervention, the authors specifically adhered to the principles of CBPR in order to create a culturally adapted program with substantial community buy-in. The intervention was successful; children in the experimental CALMA group experienced three-times greater control of their asthma symptoms, had 37% fewer visits to the emergency room and 68% fewer hospitalizations [26]. The research team also involved the families in the study; caregivers reported increased confidence in their ability to manage their child's asthma after taking part in the modules.
The previously mentioned UCLA DFM team used CBPR methods to implement a school-based asthma-screening program. After carrying out a community needs assessment, the team identified asthma as a major concern among the community's residents. In LA, asthma has been associated with school absenteeism and could jeopardize school funding based on attendance [21,27]. By collaborating with the LA school district and SVMS, the DFM began a screening process to identify at-risk students. Those identified as having asthma were able to take part in a ‘family session’ intervention to identify and address environmental and social factors related to their asthma, which was very successful. Out of the 102 family sessions, 60% of the students with uncontrolled asthma demonstrated controlled asthma 4 months later [21]. In this case study, the UCLA research team adapted their original plans to provide early asthma treatment to the children with positive screens. Because of overlap with an existing local organization already involved in providing asthma treatment within LA schools, the DFM team compromised by focusing on the screening portion of the program. This adaptable approach is crucial in carrying out a CBPR study, as the nature of the approach makes interactions and possible tensions with existing organizations commonplace.
A community-based approach to research is especially useful in the context of environmental toxicants. Given the impact that these toxicants can have on asthma control, and that it may be difficult to access pest management strategies during a primary care visit, these studies provide a vital insight into the community members’ living conditions. The problem of early childhood exposure to cockroach pesticides cannot be adequately studied and solved by a single group; rather, it must be confronted in tandem by environmental scientists, pediatricians and other healthcare professionals, and community members. From this coalition, Growing Up Healthy was created to set up a community intervention trial to test an Integrated Pest Management (IPM) program in East Harlem (NY, USA) [5,28]. An IPM approach consisted of a bilingual team – a health educator, community outreach worker, handyman and consultant – teaching the household IPM methods, which include sealing cracks and using low toxicity gels to kill the cockroaches and eggs. The results of the IPM intervention demonstrated a decrease in cockroach infestation in low-income households. In addition, the tenants were no longer exposed to the toxic pesticides common in low-income housing projects. After a cost assessment indicating IPM to be comparable to the traditional chemical pest control, New York City Council began requiring alternatives to pesticide sprays in all city-owned schools and other properties [28]. In this study, community partners were vital in their role as a bridge between the researchers and the diverse population of East Harlem. After the investigation, they helped translate the results into community education programs to affect change, a vital component to any CBPR approach [5].
While Brenner and colleagues used the reduction of cockroach infestation as a measure of the IPM intervention's success, a CBPR longitudinal study in Boston (MA, USA) measured asthma symptoms among 50 asthmatic children pre- and post-IPM [5,28]. The intervention included IPM as well as educational efforts, case management and support from community health advocates. Postintervention, the research team found significant reductions in 2-week recall respiratory symptom score and other asthma symptoms, such as wheezing and waking at night, as well as an improved asthma-related quality of life score [20]. Because of the multifactorial nature of asthma and the environmental and social triggers, the study further elucidates the need for community partnerships and involvement in asthma intervention programs. This is not a disease that can be solved simply by visits to a primary care physician.
CBPR in diabetes & obesity
Nearly 2 million Americans are diagnosed with diabetes each year and the total percentage of the US population with diabetes is 8.3% [28–31]. Diabetes disproportionately affects black and Latino individuals, with these groups experiencing double the prevalence and mortality rates as whites [30]. Crucial to slowing the rise of diabetes is adequate preventive measures, such as weight loss and increase in physical activity [31]. However, traditional prevention interventions are often financially unfeasible for many communities affected by prediabetes, as they rely on more expensive individualized weight loss interventions [32,33]. A CBPR approach in East Harlem has been successful in developing an effective prediabetes prevention strategy that led to sustained weight loss among participants [34]. The study was developed among a team of community leaders and academic partners who formed to address health disparities and develop and pilot an intervention in the East Harlem community. After reviewing common local health problems, they selected diabetes prevention as their focus, owing to the lack of existing resources and awareness in the community.
Although the efficacy of lifestyle interventions such as the Diabetes Prevention Program Lifestyle Intervention (DPP-LI) has been supported by clinical trials among all ethnic groups [35], less research has been carried out on using CBPR approaches to evaluate the translation of such interventions into public health practice. In one example, the Partnerships for Improving Lifestyle Interventions (PILI) Ohana Pilot Project aimed to shape the DPP-LI for the native Hawaiian and other Pacific Islander populations, using interviews and focus groups to create a culturally adapted program. The modified intervention was proven to be effective; participants who went to all eight lessons lost an average of 1.8 kg, while participants who completed less than eight lessons lost an average of 0.7 kg [36].
Another CBPR study used a modified DPPLI to target disproportionately high Type 2 diabetes (T2D) rates in an American–Indian population [37,38]. Previously gathered data demonstrated a two- to four-fold increase in obesity rates among American–Indian children in the Northern Plains region of the USA when compared with the national average [39]. Obesity and being overweight are major risk factors for T2D. In this study, academic researchers and tribal and nontribal members worked together to identify culturally relevant behavioral and environmental factors that influence the consumption of healthy foods, physical activity levels and diabetes prevention awareness. One factor found to be associated with physical activity was the difficulties presented by the physical environment, such as harsh weather, toxic rivers, snakes and lack of sidewalks. Many cited a desire for more group and community activities for healthier eating and physical activities. Through the focus groups, researchers found that the community valued the inclusion of cultural components in any DPP-LI; for instance, having “community elders teaching youth to put up traditional sweat lodges and facilitate group sessions for harvesting native ceremonial grasses and berries, drying meat and tanning hides” [38]. Similarly, the participants also emphasized the importance of having adult role models to mentor them towards healthier lifestyle choices. Other studies demonstrate the importance of social support and communal ties in the reinforcement of diabetes-preventing behaviors [40].
Obesity is an epidemic that is correlated with lack of community access to food retailers with healthier options. The rise of ‘food deserts’ filled with high-calorie, low-nutrient foods has been found to contribute to poor dietary patterns leading to obesity and other chronic diseases [41,42]. A CBPR study in the Argentine neighborhood of Kansas City (KS, USA) explored the food needs of low-income and minority residents. Because individual behavior is affected by a complex interaction of environmental and sociocultural factors, individually focused food interventions only have limited success [43]. Thus, CBPR principles were used to form collaborative partnerships among various community, academic and building associations in the neighborhood [42]. A Community Food Assessment survey was conducted, which provided in-depth information about the food needs of the community. The survey results indicated an overwhelming desire for a grocery store in the neighborhood to improve food access, as well as address low frequency of fruit and vegetable consumption. The results were presented in a town-hall-type meeting and used to create a business plan to address the absence of healthy food access in the neighborhood.
Community level interventions, particularly theory-based media campaigns that are planned and operationalized in a culturally appropriate manner, can help to reduce health risk and, eventually, eliminate health disparities. The TuSaludSíCuenta! community-wide media campaign was designed and implemented with a community-based participatory approach that included healthcare providers as well as community members in the design. The campaign was specifically designed to enhance the translation of currently recommended practices for physical activity and healthy food choices to Mexican–American individuals residing along the Texas–Mexico border. In particular, researchers wanted to determine the content and scope of the potential intervention, and used community partnerships effectively to meet this goal [44].
CBPR & exercise
Racial and ethnic minorities and persons with limited incomes, have disproportionately high rates of T2D, obesity, cardiovascular disease and cancer compared with white individuals [45]. Using CBPR, Zoellner et al. aimed to explore socio-ecological forces behind the target low-income minority study community [13]. The researchers analyzed the 21 walking trails within the community and found them to be relatively safe with few incidences of incivilities. While primary care physicians probably recommend exercise for patients as a matter of prevention for several chronic conditions, studies such as Zoellner et al. examine the factors that promote or inhibit exercise in the community. Community residents were surveyed to measure their physical activity, trail use and perceptions of the trails. The research demonstrated a significant association between trail usage and meeting physical activity recommendations, participant proximity to trails, perceptions of trail safety, trail amenities and neighborhood pedestrian safety. The study found a need for greater intervention efforts in areas of low physical activity that focus on residents’ perceptions of walking trail safety, conditions and amenities.
Similarly, in LA walking interventions were implemented as part of the long-term partnership between UCLA DFM and a LA community [21]. After screening children for asthma, results showed that two-thirds of the children are over-weight and half are obese. These data, as well as the growing prevalence of diabetes among Latino individuals in LA County, sparked the creation of an intervention to encourage daily physical activity. Before beginning an intervention, the research team hosted multiple focus groups and interviews with SVMS families to explore community perceptions of walking groups and exercise habits. They also asked for input from local religious leaders, politicians and a Rotary Club. The responses led the team to establish the Sun Valley Saludable (Healthy Sun Valley) program, which had over 1,600 participants during its first year and continues to grow. This project could not have experienced such success without the role of the promotoras, or healthcare professionals in the community who educate families and serve as a bridge between the community residents and health professionals. The promotoras mention some intangible variables that add to the walking intervention's success, such as the participants’ willingness to participate due to their familiarity with UCLA's involvement in SVMS and the social support they find during the walks [21]. Culturally sensitive interventions aimed at reducing obesity in Latino and other minority groups have shown that adjusting education material to different ethnic/nativity groups, and utilizing Spanish-speaking researchers who were of similar cultures to the participant groups positively impacts health outcomes [46]. Community focused approaches including group exercise, nutrition education and personal counseling have also been shown to yield positive outcomes.
CBPR & maternal/child health
CBPR methods have the potential to be useful in the context of improving maternal health, which has a marked effect not only on mothers’ health but also on the reduction of poverty and inequity [47]. A study of maternal care in the Dominican Republic used CBPR principles to examine community perceptions of maternal and newborn health services. The research team included academically trained researchers, Dominican maternity nurses and community leaders from each of the four targeted neighborhoods of study [48–50]. Male and female participants from the neighborhoods were recruited to participate in individual interviews and focus groups. In addition, community leaders accompanied the eligible participants to prenatal appointments to document their experiences. The study was able to elucidate a general dissatisfaction with the Dominican Republic's maternal health system, with many mothers and their families feeling disrespected, ignored and afraid [48–50].
Another CBPR study explored the social determinants of maternal health among Puerto Rican women living in the two Connecticut (USA) cities with the highest rates of premature birth [51]. Through focus groups in English and Spanish, researchers collected community experiences and perspectives regarding stress, discrimination and stressors that affect maternal health. The women indicated stress to be a conglomeration of many social and environmental factors that affect their wellbeing. The most significant stressors to maternal health and child health in their community were found to be poverty, instability of food, lack of quality education and unsafe environments. The study findings suggest that in order to improve birth outcomes, socioeconomic determinants of health must be acknowledged and targeted for improvement [51].
Many CBPR studies focus on marginalized adult populations, but a recent literature review focused on improving child health through direct collaboration with children and youths [52,53]. Including youths throughout various phases of a CBPR study brings a traditionally marginalized and overlooked population directly into the research process, potentially leading to more sustainable interventions. Because children and adolescents are particularly vulnerable to environmental and sociocultural factors affecting the diseases categorized above, CBPR approaches can be valuable [54]. CBPR methods allow children and adolescents to have a voice in the health issues that most affect them and their communities. A total of 34 CBPR studies focused on child health, with most focusing on obesity/diabetes and health needs assessments in communities with high-risk minority youths. It was found that youth involvement across multiple phases of the research led to higher commitment rates when compared with the rates when youths only participated as informants. It was also found that participation increased when barriers to participation were reduced, such as scheduling the projects directly after school, or when incentives were provided, such as scholarships, money, employment or skill development. The review found a strong anecdotal connection between CBPR studies with more meaningful youth involvement and increased youth empowerment, leadership skills and an increased desire to participate in the research and subsequent community health interventions [54].
CBPR challenges
Limitations of CBPR in the papers discussed above include the challenges of sustainability: funding for long-term interventions, such as those inherent to CBPR, can be difficult to obtain [5,21]. A major challenge is often differing goals between the community and researchers in results dissemination. The community is eager to disseminate preliminary results, while researchers are concerned with premature dissemination of results that may contaminate study findings [5]. Additionally, study results are often limited to the specific community in which the research took place and as such may not be translatable to other groups [36,38].
Moreover, limitations of CBPR in primary care can include an inherent disconnection between academics, providers and community members. This gap can lead to a lack of trust, divergent perspectives and research priorities, differences in the sharing of power and resources, and difficul-ties balancing scientific rigor with physician needs and community acceptability [15]. Ideally, projects involving CBPR are a negotiated process between the community, providers and researchers, and when conflicts arise researchers should be open to reframing the research question through the partnership, and working collaboratively through the advisory board to deal with conflict [55]. Effective strategies include building collaboration between the community and providers through formation of an advisory board [56,57]. Indeed, the relationships between all key stakeholders are at the foundation of the success for CBPR projects, and time must be allocated for relationship building such as participation in community events, and sharing power and resources [58]. To maximize the chance that CBPR will lead to tangible, lasting health benefits for communities, researchers are faced with a goal of balancing scientific rigor and healthcare providers and community members acceptability, in practice this is not easily accomplished [55].
Ensuring that a CBPR study is truly an academic/provider/community partnership is an important challenge. The traditional model has been research ‘on’ communities and subjects rather than ‘with’ them, and the clarification of intentions and establishment of trust is crucial to overcome possible negative preconceptions [19,59,60]. Often, an academic research team conceives the studies and the community partners feel that they must constantly advocate for the abidance of community-based principles (which may be overlooked in the interests of time or funding guidelines). In addition, bidirectional stereotypes can also impede a successful partnership. Stereotypes of both academic researchers and community partners must be overcome to ensure the minimization of tension and potential power disparities. Another challenge implicit in CBPR is the “[reconciliation of] the different cultures of the community-based organization and the academic institution and the way in which research is viewed and conducted” [19]. In order to create a fair and equitable partnership, the traditional model of a single primary investigator must be abandoned in favor of a more collegial ‘coinvestigator’ approach.
CBPR has great potential for helping to address mental health issues through partnership with primary care. However, we were unable to find any CBPR mental health initiatives involving the primary care setting. CBPR research within mental health is still considered to be a relatively new approach within the arena [61–64]. Given the comorbidity of mental health disorders with several chronic conditions [65], it is important to consider CBPR in the primary care setting for certain psychosocial disorders.
Another challenge is ensuring that participants feel completely comfortable disclosing sensitive information during the intensive interview sessions or focus groups used in many CBPR studies. The interviewers or focus group leaders are often members of the community themselves, which may create a more comfortable environment in which the participants can feel at ease to share their experiences and opinions. However, perhaps the leader or interviewer has a certain standing within the community or relationship with the academic research team that makes participants hesitant to disclose information [60,66]. In addition, many participants in CBPR studies related to primary care are receiving services for free or at a reduced cost. This fact may create a methodological bias when participants are asked about their opinions of the services, possibly influencing the participants to rate the service higher than they would have otherwise.
Ensuring compliance with federal regulations related to the protection of human subjects can get complicated. One component of CBPR is the need for review by the Institutional Review Board. Institutional Review Boards must ensure that, “When appropriate, there are adequate provisions to protect the privacy of subjects and to maintain the confidentiality of data.” [67]. These provisions can be complicated in CBPR because of the access healthcare- and community-based researchers might have to confidential research information about subjects within their health-care system and/or community. The research protocol must address the likelihood for this situation to occur, the sensitivity of the data available to the research staff and the measures that will be taken to minimize these risks. Training of researchers must include education about how to deal with real life confidentiality challenges and a discussion about the obligation of staff to not discuss the knowledge they have about particular participants outside the research. In some instances, researchers will have access to research information that is subject to the Health Insurance Portability and Accountability Act (HIPPA) Privacy Rule, requiring HIPPA training.
While CBPR has the ability to empower communities to make themselves healthier, it is not always feasible owing to the large amount of time required to develop and cultivate trusting partnerships [19,59,60]. This time constraint may limit progress for CBPR to demonstrate improved healthcare outcomes [68–71]. In addition, and perhaps related to problems inherent in CBPR, a limited number of studies use rigorous scientific research design (such as a randomized controlled trial) in community-based methods of research, making results less easy to be seen as evidence [14]. An earlier review sponsored by Viswanathan et al. was not able to definitively determine whether CBPR efforts result in their intended health outcomes due to large variability in study designs and intervention approaches, as well as the small number of studies with completed interventions that qualified [72]. However, the researchers discovered an association between ‘higher quality research designs’ and more consistently positive health outcomes. According to Viswanathan et al., “the ultimate benefit to emerge from such collaborations is a deeper understanding of a community’s unique circumstances, and a more accurate framework for testing and adapting best practices to the community’s needs” [72].
Many studies spend months or years establishing collaborations and building trust even before beginning the funding application process. Often, this large amount of time building a coalition necessary for the success of a CBPR project is not possible owing to the timing of due dates and grant announcements. Another challenge of CBPR is overcoming the damage done by previous researchers who may not have kept their promises after collecting data, leaving the community wary of further academic studies. Establishing trust in the wake of such challenges is essential if the subsequent CBPR study is to realize its full potential [60,73].
Study authors may be reluctant to publish negative results. It is important that these results be disseminated so that others can learn from these methods and outcomes. In our review, the majority of the work indicated at least partially positive results or outcomes. Brown et al., however, did indicate that there was no overall change in BMI in their study, possibly due to the short intervention time [37].
From a provider perspective engaging in CBPR can be extremely beneficial. In one study, healthcare providers reported that while conducting a CBPR project, it was found that the core principles of CBPR apply not only to the development of intergroup relationships between academia and community members, but also improve relationships within the research team [74]. The unique contribution of service providers as practice professionals, cultural brokers and experts in working in communities is a vital resource in CBPR [75]. Service providers can benefit by obtaining research-based knowledge to help the communities they serve, gaining research skills, building professional relationships, professional development and new programs. They contribute by informing research aims, designing interventions, conducting recruitment, informing overall study design and dissemination. Challenges include time, resources, organizational factors and disconnections between researchers, patients and service providers [75].
Conclusion
This article advances our understanding of the role of CBPR within primary care. By describing the use of CBPR to improve access and reduce health disparities, as well as using CBPR to target common primary care health problems, and discussing challenges in CBPR primary care research, we have provided an overview and synthesis of the current literature on the topic. We hope that future research will focus on how to promote CBPR within primary care with a goal of enhancing primary care, community e ngagement and improved health outcomes.
Future perspective
Expansion of primary care and increased prevalence of obesity, diabetes and other chronic diseases opens the door to increasing need for community provider partnerships. At the same time, the need to overcome barriers to the translation of research findings from bench to bedside, will reinforce the need for CBPR to further engage with primary care to address the needs of vulnerable populations. In recent years, NIH funding for Clinical and Translational Science Awards has been reduced for community engagement, while the Patient-Centered Outcomes Research Institute is now leading the way with emphasis on funding patient-centered approaches using participatory research methods. Patients and community members are increasingly serving as community and/or patient advisory board members, research advisors and reviewers so that their priorities and needs will continue to drive the future of CBPR in improving healthcare outcomes and addressing disparities.
Executive summary.
Background
■ Community-based participatory research (CBPR) has emerged in the last decades to bridge the gap between research and practice through community engagement and social action to increase health equity.
CBPR uses
■ Using CBPR to study a community's access to primary care and the health problems commonly addressed in a primary care setting can help set the stage for real policy change on a local level to tackle health disparities and deficiencies.
■ Disparities in asthma treatment across vulnerable populations and care can be attributed to a multitude of factors such as language barriers, environmental triggers, cultural beliefs, insurance and genetic factors. CBPR studies aim to minimize disparities in asthma care through culturally-tailored approaches to treatment and increased understanding of the environmental obstacles asthma patients face within their communities.
■ Crucial to slowing the rise of diabetes and obesity are adequate preventive measures, such as weight loss, an increase in physical activity and access to affordable healthy foods. Traditional prevention interventions are often financially unfeasible for vulnerable populations, as they rely on more expensive individualized weight loss interventions. CBPR methods allow partnerships to identify culturally relevant behavioral and environmental factors that influence diet and activity.
■ Using CBPR can be especially useful in the context of improving maternal and child health, which has a marked effect not only on health, but also on the reduction of poverty and inequity. CBPR methods allow children and adolescents to have a voice in the health issues that most affect them and their communities. Findings suggest that in order to improve birth outcomes, socio-economic determinants of health must be acknowledged and targeted for improvement.
Challenges
■ CBPR faces many challenges in partnering with primary care. While CBPR has the ability to empower primary care/community partnerships and improve health outcomes, it is not always feasible owing to the large amount of time and effort involved.
Conclusion
■ CBPR can be used to increase access to care by building relationships with community partners that can determine geographical areas of need, establish community priorities for health concerns and ultimately create a more efficient and streamlined healthcare delivery system.
■ CBPR can be used to design sustainable community specific interventions with the potential to produce specific improvements in several chronic conditions.
Footnotes
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pe nding, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
■ of interest
■■ of considerable interest
- 1.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Ann. Rev. Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 2.Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am. J. Public Health. 2010;100(Suppl. 1):S40–S46. doi: 10.2105/AJPH.2009.184036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Brien MJ, Whitaker RC. The role of community-based participatory research to inform local health policy: a case study. J. Gen. Intern. Med. 2011;26(12):1498–1501. doi: 10.1007/s11606-011-1878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horowitz CR, Arniella A, James S, Bickell NA. Using community-based participatory research to reduce health disparities in East and Central Harlem. Mt Sinai J. Med. 2004;71(6):368–374. [PMC free article] [PubMed] [Google Scholar]
- 5■■.Brenner B, Manice M. Community engagement in children's environmental health research. Mt Sinai J. Med. 2011;78(1):85–97. doi: 10.1002/msj.20231. [Together with community health centers and East Harlem (NY, USA) residents, researchers decided to implement a pest reduction program with an aim to reduce the impact of pests and pesticides as asthma triggers. Community members suggested that the comparison group should also receive an intervention of value, and injury prevention education was given to those not receiving integrated pest management.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Macinko J, Starfield B, Shi L. Quantifying the health benefits of primary care physician supply in the United States. Int. J. Health Serv. 2007;37(1):111–126. doi: 10.2190/3431-G6T7-37M8-P224. [DOI] [PubMed] [Google Scholar]
- 8.Franks P, Fiscella K. Primary care physicians and specialists as personal physicians. Health care expenditures and mortality experience. J. Fam. Pract. 1998;47(2):105–109. [PubMed] [Google Scholar]
- 9.O'Malley AS, Forrest CB, Politzer RM, Wulu JT, Shi L. Health center trends, 1994–2001: what do they portend for the federal growth initiative? Health Aff. (Millwood) 2005;24(2):465–472. doi: 10.1377/hlthaff.24.2.465. [DOI] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality. National Healthcare Disparities Report. 2006 [Google Scholar]
- 11.McWilliams A, Tapp H, Barker J, Dulin M. Cost analysis of the use of emergency departments for primary care services in Charlotte, North Carolina. NC Med. J. 2011;72(4):265–271. [PubMed] [Google Scholar]
- 12.Louis MR. Surprise and sense making: what newcomers experience in entering unfamiliar organizational settings. Adm. Sci. Q. 1980;25:226–251. [PubMed] [Google Scholar]
- 13.Zoellner J, Hill JL, Zynda K, Sample AD, Yadrick K. Environmental perceptions and objective walking trail audits inform a community-based participatory research walking intervention. Int. J. Behav. Nutr. Phys. Act. 2012;9:6. doi: 10.1186/1479-5868-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salimi Y, Shahandeh K, Malekafzali H, et al. Is community-based participatory research (CBPR) useful? A systematic review on papers in a decade. Int. J. Prev. Med. 2012;3(6):386–393. [PMC free article] [PubMed] [Google Scholar]
- 15.Tapp H, Dulin M. The science of primary health-care improvement: potential and use of community-based participatory research by practice-based research networks for translation of research into practice. Exp. Biol. Med. (Maywood) 2010;235(3):290–299. doi: 10.1258/ebm.2009.009265. [DOI] [PubMed] [Google Scholar]
- 16.Tierney WM, Oppenheimer CC, Hudson BL, et al. A national survey of primary care practice-based research networks. Ann. Fam. Med. 2007;5(3):242–250. doi: 10.1370/afm.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Westfall JM, Vanvorst RF, Main DS, Herbert C. Community-based participatory research in practice-based research networks. Ann. Fam. Med. 2006;4(1):8–14. doi: 10.1370/afm.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pylypchuk G, Vincent L, Wentworth J, et al. Diabetes risk evaluation and microalbuminuria (DREAM) studies: ten years of participatory research with a First Nation's home and community model for Type 2 diabetes care in Northern Saskatchewan. Int. J. Circumpolar Health. 2008;67(2–3):190–202. doi: 10.3402/ijch.v67i2-3.18264. [DOI] [PubMed] [Google Scholar]
- 19.Freeman ER, Brugge D, Bennett-Bradley WM, Levy JI, Carrasco ER. Challenges of conducting community-based participatory research in Boston's neighborhoods to reduce disparities in asthma. J. Urban Health. 2006;83(6):1013–1021. doi: 10.1007/s11524-006-9111-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levy JI, Brugge D, Peters JL, Clougherty JE, Saddler SS. A community-based participatory research study of multifaceted in-home environmental interventions for pediatric asthmatics in public housing. Soc. Sci. Med. 2006;63(8):2191–2203. doi: 10.1016/j.socscimed.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 21■■.Moreno G, Rodriguez MA, Lopez GA, Bholat MA, Dowling PT. Eight years of building community partnerships and trust: the UCLA family medicine community-based participatory research experience. Acad. Med. 2009;84(10):1426–1433. doi: 10.1097/ACM.0b013e3181b6c16a. [Describes three community-based participatory research (CBPR) intervention case studies in asthma, diabetes and primary care access. Compared common lessons learned across all three case studies and discussed the importance of long-term community relationships.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kruger DJ, Hamacher L, Strugar-Fritsch D, Shirey L, Renda E, Zimmerman MA. Facilitating the development of a county health coverage plan with data from a community-based health survey. J. Public Health Policy. 2010;31(2):199–211. doi: 10.1057/jphp.2010.8. [DOI] [PubMed] [Google Scholar]
- 23■.Tapp H, Smith HA, Dixon JT, Ludden T, Dulin M. Evaluating primary care delivery systems for an uninsured Hispanic immigrant population. Fam. Comm. Health. 2013;36(1):19–33. doi: 10.1097/FCH.0b013e31826d7562. [Evaluated disparities in a Hispanic population. Using CBPR principles, the authors determined patient and provider best practices in this community.] [DOI] [PubMed] [Google Scholar]
- 24.Forno E, Celedon JC. Asthma and ethnic minorities: socioeconomic status and beyond. Curr. Opin. Allergy Clin. Immunol. 2009;9(2):154–160. doi: 10.1097/aci.0b013e3283292207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Canino G, Mcquaid EL, Rand CS. Addressing asthma health disparities: a multilevel challenge. J. Allergy Clin. Immunol. 2009;123(6):1209–1217. doi: 10.1016/j.jaci.2009.02.043. quiz 1218–1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26■.Martin CG, Andrade AA, Vila D, Acosta-Perez E, Canino G. The development of a community-based family asthma management intervention for Puerto Rican children. Prog. Community Health Partnersh. 2010;4(4):315–324. doi: 10.1353/cpr.2010.0025. [Developed culturally tailored asthma education models using CBPR methods within a community, academic and provider partnership.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bonilla S, Kehl S, Kwong KY, Morphew T, Kachru R, Jones CA. School absenteeism in children with asthma in a Los Angeles inner city school. J. Pediatr. 2005;147(6):802–806. doi: 10.1016/j.jpeds.2005.06.041. [DOI] [PubMed] [Google Scholar]
- 28.Brenner BL, Markowitz S, Rivera M, et al. Integrated pest management in an urban community: a successful partnership for prevention. Environ. Health Perspect. 2003;111(13):1649–1653. doi: 10.1289/ehp.6069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Center for Disease Control (CDC) National Diabetes Fact Sheet. 2011 [Google Scholar]
- 30.Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999–2002. Diabetes Care. 2006;29(6):1263–1268. doi: 10.2337/dc06-0062. [DOI] [PubMed] [Google Scholar]
- 31.Genuth S, Alberti KG, Bennett P, et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26(11):3160–3167. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- 32.Horowitz CR, Eckhardt S, Talavera S, Goytia C, Lorig K. Effectively translating diabetes prevention: a successful model in a historically underserved community. Transl. Behav. Med. 2011;1(3):443–452. doi: 10.1007/s13142-011-0067-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Herman WH, Hoerger TJ, Hicks K, et al. Managing people at high risk for diabetes. Ann. Intern. Med. 2006;144(1):66–67. doi: 10.7326/0003-4819-144-1-200601030-00018. author reply 67–68. [DOI] [PubMed] [Google Scholar]
- 34.Parikh P, Simon EP, Fei K, Looker H, Goytia C, Horowitz CR. Results of a pilot diabetes prevention intervention in East Harlem, New York City: Project HEED. Am. J. Public Health. 2010;100(Suppl. 1):S232–S239. doi: 10.2105/AJPH.2009.170910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jackson L. Translating the Diabetes Prevention Program into practice: a review of community interventions. Diabetes Educ. 2009;35(2):309–320. doi: 10.1177/0145721708330153. [DOI] [PubMed] [Google Scholar]
- 36■.Mau MK, Keawe'aimoku Kaholokula J, West MR, et al. Translating diabetes prevention into native Hawaiian and Pacific Islander communities: the PILI ‘Ohana Pilot project. Prog. Community Health Partnersh. 2010;4(1):7–16. doi: 10.1353/cpr.0.0111. [Culturally adapted diabetes prevention and weight-loss intervention with ongoing community partnership in a native Hawaiian and other Pacific Islander population.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37■.Brown B, Noonan C, Harris KJ, et al. Developing and piloting the journey to native youth health program in northern plains Indian communities. Diabetes Educ. 2013;39(1):109–118. doi: 10.1177/0145721712465343. [Researchers leveraged partnership with local Northern Plains Indian communities to seek funding, then were able to maintain ongoing discussion in order to collaboratively design a health behavior and weight-loss strategy.] [DOI] [PubMed] [Google Scholar]
- 38.Brown BD, Harris KJ, Harris JL, Parker M, Ricci C, Noonan C. Translating the diabetes prevention program for Northern Plains Indian youth through community-based participatory research methods. Diabetes Educ. 2010;36(6):924–935. doi: 10.1177/0145721710382582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Noonan CW, Brown BD, Bentley B, et al. Variability in childhood asthma and body mass index across Northern Plains American Indian communities. J. Asthma. 2010;47(5):496–500. doi: 10.3109/02770901003759436. [DOI] [PubMed] [Google Scholar]
- 40.Bisset S, Cargo M, Delormier T, Macaulay AC, Potvin L. Legitimizing diabetes as a community health issue: a case analysis of an Aboriginal community in Canada. Health Promot. Int. 2004;19(3):317–326. doi: 10.1093/heapro/dah305. [DOI] [PubMed] [Google Scholar]
- 41.Mead MN. The sprawl of food deserts. Environ. Health Perspect. 2008;116(8):A335. doi: 10.1289/ehp.116-a335a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mabachi NM, Kimminau KS. Leveraging community-academic partnerships to improve healthy food access in an urban, Kansas City, Kansas, community. Prog. Community Health Partnersh. 2012;6(3):279–288. doi: 10.1353/cpr.2012.0046. [DOI] [PubMed] [Google Scholar]
- 43.Cummins S, Macintyre S. Food environments and obesity--neighbourhood or nation? Int. J. Epidemiol. 2006;35(1):100–104. doi: 10.1093/ije/dyi276. [DOI] [PubMed] [Google Scholar]
- 44.Reininger BM, Barroso CS, Mitchell-Bennett L, et al. Process evaluation and participatory methods in an obesity-prevention media campaign for Mexican Americans. Health Promot. Pract. 2010;11(3):347–357. doi: 10.1177/1524839908321486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gebel K, Bauman AE, Petticrew M. The physical environment and physical activity: a critical appraisal of review articles. Am. J. Prev. Med. 2007;32(5):361–369. doi: 10.1016/j.amepre.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 46.Morrison SD, Haldeman L, Sudha S, Gruber KJ, Bailey R. Cultural adaptation resources for nutrition and health in new immigrants in central North Carolina. J. Immigr. Minor. Health. 2007;9(3):205–212. doi: 10.1007/s10903-006-9031-9. [DOI] [PubMed] [Google Scholar]
- 47.Sachs J. The End of Poverty. Penguin Press; NY, USA: 2005. [Google Scholar]
- 48■.Foster JW, Chiang F, Burgos RI, et al. Community-based participatory research and the challenges of qualitative analysis enacted by lay, nurse, and academic researchers. Res. Nurs. Health. 2012;35(5):550–559. doi: 10.1002/nur.21494. [In collaboration with Dominican nurses and midwives, the researchers developed a research question about pregnant women with complications. They were able to elucidate a general dissatisfaction with the Dominican Republic's maternal health system.] [DOI] [PubMed] [Google Scholar]
- 49.Foster J, Chiang F, Hillard RC, Hall P, Heath A. Team process in community-based participatory research on maternity care in the Dominican Republic. Nurs. Inq. 2010;17(4):309–316. doi: 10.1111/j.1440-1800.2010.00514.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Foster J, Burgos R, Tejada C, et al. A community-based participatory research approach to explore community perceptions of the quality of maternal-newborn health services in the Dominican Republic. Midwifery. 2010;26(5):504–511. doi: 10.1016/j.midw.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bermudez-Millan A, Damio G, Cruz J, et al. Stress and the social determinants of maternal health among Puerto Rican women: a CBPR approach. J. Health Care Poor Underserved. 2011;22(4):1315–1330. doi: 10.1353/hpu.2011.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vaughn LM, Wagner E, Jacquez F. A review of community-based participatory research in child health. MCN Am. J. Matern. Child Nurs. 2013;38(1):48–53. doi: 10.1097/NMC.0b013e31826591a3. [DOI] [PubMed] [Google Scholar]
- 53.Jacquez F, Vaughn LM, Wagner E. Youth as partners, participants or passive recipients: a review of children and adolescents in community-based participatory research (CBPR). Am. J. Community Psychol. 2012;51(1–2):176–189. doi: 10.1007/s10464-012-9533-7. [DOI] [PubMed] [Google Scholar]
- 54.Earls F, Carlson M. The social ecology of child health and well-being. Ann. Rev. Public Health. 2001;22:143–166. doi: 10.1146/annurev.publhealth.22.1.143. [DOI] [PubMed] [Google Scholar]
- 55.Israel B, Eng E, Schulz A, Parker E. Methods in Community-Based Participatory Research. Jossey-Bass; CA, USA: 2005. [Google Scholar]
- 56.Dancy BL, Wilbur J, Talashek M, Bonner G, Barnes-Boyd C. Community-based research: barriers to recruitment of African Americans. Nurs. Outlook. 2004;52(5):234–240. doi: 10.1016/j.outlook.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 57.Tumiel-Berhalter LM, Mclaughlin-Diaz V, Vena J, Crespo CJ. Building community research capacity: process evaluation of community training and education in a community-based participatory research program serving a predominately puerto rican community. Prog. Community Health Partnersh. 2007;1(1):89–97. doi: 10.1353/cpr.0.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Israel BA, Parker EA, Rowe Z, et al. Community-based participatory research: lessons learned from the Centers for Children's Environmental Health and Disease Prevention Research. Environ. Health Perspect. 2005;113(10):1463–1471. doi: 10.1289/ehp.7675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hirani SS, Karmaliani R, Mcfarlane J, et al. Development of an economic skill building intervention to promote women's safety and child development in Karachi, Pakistan. Issues Ment. Health Nurs. 2010;31(2):82–88. doi: 10.3109/01612840903254859. [DOI] [PubMed] [Google Scholar]
- 60.Karmaliani R, Mcfarlane J, Asad N, et al. Applying community-based participatory research methods to improve maternal and child health in Karachi, Pakistan. Nurs. Outlook. 2009;57(4):204–209. doi: 10.1016/j.outlook.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 61.Mulvaney-Day NE, Rappaport N, Alegria M, Codianne LM. Developing systems interventions in a school setting: an application of community-based participatory research for mental health. Ethn. Dis. 2006;16(1 Suppl. 1):S107–S117. [PubMed] [Google Scholar]
- 62.Minkler M, Blackwell AG, Thompson M, Tamir H. Community-based participatory research: implications for public health funding. Am. J. Public Health. 2003;93(8):1210–1213. doi: 10.2105/ajph.93.8.1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stacciarini JM, Wiens B, Coady M, et al. CBPR: building partnerships with latinos in a rural area for a wellness approach to mental health. Issues Ment. Health Nurs. 2011;32(8):486–492. doi: 10.3109/01612840.2011.576326. [DOI] [PubMed] [Google Scholar]
- 64.Stacciarini JM, Shattell MM, Coady M, Wiens B. Review: community-based participatory research approach to address mental health in minority populations. Community Ment Health J. 2011;47(5):489–497. doi: 10.1007/s10597-010-9319-z. [DOI] [PubMed] [Google Scholar]
- 65.Tapp H, Philips S, Waxman D, Alexander M, Brown R, Hall M. Multidisciplinary team approach to improved chronic care management for diabetic patients in an urban safety net ambulatory care clinic. J. Am. Board Fam. Med. 2012;25(2):245–246. doi: 10.3122/jabfm.2012.02.110243. [DOI] [PubMed] [Google Scholar]
- 66.Tumiel-Berhalter LM, Mclaughlin-Diaz V, Vena J, Crespo CJ. Building community research capacity: process evaluation of community training and education in a community-based participatory research program serving a predominantly Puerto Rican community. Prog. Community Health Partnersh. 2007;1(1):89–97. doi: 10.1353/cpr.0.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Penslar RL. IRB Guidebook. US Department of Health & Human Services; DC, USA: 1993. Basic IRB review. [Google Scholar]
- 68.Macaulay AC, Cross EJ, Delormier T, Potvin L, Paradis G, Mccomber A. Developing a code of research ethics for research with a native community in Canada: a report from the Kahnawake Schools Diabetes Prevention Project. Int. J. Circumpolar Health. 1998;57(Suppl. 1):38–40. [PubMed] [Google Scholar]
- 69.Nevin JE, Gohel MM. Community-oriented primary care. Prim. Care. 1996;23(1):1–15. doi: 10.1016/s0095-4543(05)70257-8. [DOI] [PubMed] [Google Scholar]
- 70.Macaulay AC, Hanusaik N, Beauvais JE. Breastfeeding in the Mohawk community of Kahnawake: revisited and redefined. Arctic Med. Res. 1991;(Suppl.):581–585. [PubMed] [Google Scholar]
- 71.Green LA, Hickner J. A short history of primary care practice-based research networks: from concept to essential research laboratories. J. Am. Board Fam Med. 2006;19(1):1–10. doi: 10.3122/jabfm.19.1.1. [DOI] [PubMed] [Google Scholar]
- 72.Viswanathan M, Ammerman A, Eng E, et al. Community-based participatory research: assessing the evidence. Evid. Rep. Technol. Assess. (Summ.) 2004;99:1–8. [PMC free article] [PubMed] [Google Scholar]
- 73.Green LW, Mercer SL. Can public health researchers and agencies reconcile the push from funding bodies and the pull from communities? Am. J. Public Health. 2001;91(12):1926–1929. doi: 10.2105/ajph.91.12.1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dalal M, Skeete R, Yeo HL, Lucas GI, Rosenthal MS. A physician team's experiences in community-based participatory research: insights into effective group collaborations. Am. J. Prev. Med. 2009;37(6 Suppl. 1):S288–S291. doi: 10.1016/j.amepre.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 75.Spector AY. CBPR with service providers: arguing a case for engaging practitioners in all phases of research. Health Promot. Pract. 2012;13(2):252–258. doi: 10.1177/1524839910382081. [DOI] [PubMed] [Google Scholar]