Abstract
Nerve injury-induced central sensitization can manifest as an increase in excitatory synaptic transmission and/or as a decrease in inhibitory synaptic transmission in spinal dorsal horn neurons. Cytokines such as tumor necrosis factor-α (TNF-α) are induced in the spinal cord under various injury conditions and contribute to neuropathic pain. In this study we examined the effect of TNF-α in modulating excitatory and inhibitory synaptic input to spinal substantia gelatinosa (SG) neurons over time in mice following chronic constriction injury (CCI) of the sciatic nerve. Whole cell patch-clamp studies from SG neurons showed that TNF-α enhanced overall excitability of the spinal cord early in time following nerve injury 3 days after CCI compared with that in sham control mice. In contrast, the effects of TNF were blunted 14 days after CCI in nerve-injured mice compared with sham surgery mice. Immunohistochemical staining showed that the expression of TNF-α receptor 1 (TNFR1) was increased at 3 days but decreased at 14 days following CCI in the ipsilateral vs. the contralateral spinal cord dorsal horn. These results suggest that TNF-α acting at TNFR1 is important in the development of neuropathic pain by facilitating excitatory synaptic signaling in the acute phases after nerve injury but has a reduced effect on spinal neuron signaling in the later phases of nerve injury-induced pain. Failure of the facilatory effects of TNF-α on excitatory synaptic signaling in the dorsal horn to resolve following nerve injury may be an important component in the transition between acute and chronic pain conditions.
Keywords: CCI, hyperalgesia, substantia gelatinosa, spinal synaptic transmission
nerve injury caused by trauma or surgery can produce persistent neuropathic pain, a chronic condition that is often resistant to conventional analgesics (Sindrup and Jensen 1999; Woolf and Mannion 1999). Allodynia and hyperalgesia are not only the result of peripheral sensitization at the site of injury but also a consequence of hyperactivity or sensitization of neurons in the spinal dorsal horn (Matzner and Devor 1994; Woolf and Mannion 1999). Several mechanisms have been proposed as contributing to central sensitization in neuropathic pain. These include increased excitatory neuronal processes in the spinal cord, parallel decreases in the activity of spinal neuronal inhibitory processes (Costigan et al. 2009; Sandkuhler 2009), and changes in the regulation of the spinal microenvironment by spinal astrocytes and microglia (Gao and Ji 2010; Milligan and Watkins 2009).
Tumor necrosis factor-α (TNF-α) is among the proinflammatory cytokines expressed by a variety of cell types, including immune cells and glial cells (Mannel 1986; Ohtori et al. 2004; Xu et al. 2006), that play a critical role in inflammatory and neuropathic pain in the peripheral as well as the central nervous system (Cunha et al. 1992; Ferreira et al. 1993; Schafers et al. 2003a, 2003c; Schäfers et al. 2003; Sommer et al. 1998, 2001; Watkins et al. 1995; Woolf et al. 1997; Xu et al. 2006). TNF-α is increased at the injury site following chronic constriction injury (CCI) of the sciatic nerve in rats (George et al. 1999, 2004; Shubayev and Myers 2000), and intrasciatic injection of TNF-α in rats reproduces CCI-like pain hypersensitivity (Sorkin and Doom 2000; Wagner and Myers 1996). Conversely, CCI-induced hypersensitivity is reversed with peripheral administration of neutralizing antibodies to TNF-α or to TNF receptors (TNFRs), in particular TNFR1 (Sommer et al. 1998; Sorkin and Doom 2000). Similarly, intraperitoneal injection of the TNF-α inhibitor etanercept suppresses hypersensitivity after nerve injury (Iwatsuki et al. 2013), and mice lacking TNF-α or TNFR1 show reduced nociceptive sensitivity compared with wild-type littermates after nerve injury (Nadeau et al. 2011).
TNF-α also has an important role within the central nervous system (CNS) in generating neuropathic pain. For example, intrathecal injection of TNF-α induces mechanical allodynia and heat hyperalgesia (Gao et al. 2009; Narita et al. 2008), and TNF-α among other cytokines is released by spinal glial cells (both microglia and astrocytes) that are activated following nerve injury or inflammation (Gao and Ji 2010; Milligan and Watkins 2009). Suppression of this response of spinal glial cells similarly suppresses behavioral hypersensitivity to peripheral stimuli normally observed following nerve injury (Gao and Ji 2010; Milligan and Watkins 2009). Yet, the specific mechanisms underlying the effects of TNF-α within the CNS are not well understood. Previous experiments showed that acute application of TNF-α significantly reduced the frequency of spontaneous inhibitory synaptic currents (sIPSCs) and also produced an increase in the frequency of spontaneous excitatory postsynaptic currents (sEPSCs) in spinal substantia gelatinosa (SG) neurons isolated from naive mice (Zhang et al. 2010). Acute application of TNF-α directly inhibits the excitability of a subset of spinal GABAergic neurons (Zhang and Dougherty 2011). However, the functional changes of TNF-α on synaptic input to spinal neurons in neuropathic pain conditions have not been tested. This gap in knowledge was addressed in this study.
MATERIALS AND METHODS
Animals.
Sixty-nine C57BL/6 mice of either sex weighing 20–25 g were used. All the surgical and experimental protocols were approved by the Animal Care and Use Committee of MD Anderson Cancer Center and conformed to the NIH guidelines for the ethical use of animals. All efforts were made to minimize the number of animals used and their suffering.
CCI model and behavioral test.
Mice were deeply anesthetized with 2–3% isoflurane. The left sciatic nerve was exposed at the mid-thigh level proximal to the trifurcation and freed from adhering tissue. Three ligatures (chromic gut, 6-0) were tied around the nerve with about 1-mm spacing in between, similar to procedures previously used on rats (Carlton et al. 1991; Dougherty et al. 1992; Palecek et al. 1992). The muscle and skin incisions were then closed. In sham animals, the left sciatic nerve was exposed and freed from the connective tissue as in the CCI mice but not surrounded with suture. The response of mice to mechanical stimulation of both hindpaws was evaluated daily beginning 3 days before CCI and then at 1, 3, 7, and 14 days after surgery. Animals were placed under acrylic boxes that were atop wire mesh floors and allowed to habituate for 1 h. Von Frey filaments were applied to the plantar surface of paw, and the withdrawal threshold was measured using an up-down method beginning with a 0.6-g filament (Chaplan et al. 1994). Mice with confirmed mechanical hypersensitivity in the ipsilateral paw (compared with the contralateral paw) and mice with sham CCI exited the behavioral studies to the terminal electrophysiological or immunohistochemical experiments at either day 3 or day 14 after surgery.
Spinal cord slice preparation.
Mice were anesthetized with 2–3% isoflurane, and lumbar segments 4 to 6 of the spinal cord were rapidly removed through laminectomy. The mice were then killed by inhalation of 5% isoflurane and exsanguination. The spinal cord was immediately placed in ice-cold sucrose artificial cerebrospinal fluid (ACSF) saturated with 95% O2 and 5% CO2. The sucrose ACSF contained 234 mM sucrose, 3.6 mM KCl, 1.2 mM MgCl2, 2.5 mM CaCl2, 1.2 mM NaH2PO4, 12.0 mM glucose, and 25.0 mM NaHCO3. The tissue was then placed in a shallow groove formed in a gelatin block and glued onto the stage of a Vibratome (Products International, St. Louis, MO). Transverse spinal cord slices (300 μm) through the L5 segment were cut in the ice-cold sucrose ACSF and then transferred and incubated in Krebs solution bubbled with 95% O2 and 5% CO2 at 34°C for at least 1 h before further use. The Krebs solution contained 117.0 mM NaCl, 3.6 mM KCl, 1.2 mM MgCl2, 1.5 mM CaCl2, 1.2 mM NaH2PO4, 11.0 mM glucose, and 25.0 mM NaHCO3. Slices for study were placed in a glass-bottom recording chamber (Warner Instruments, Hamden, CT) and fixed with parallel nylon threads supported by a U-shaped stainless steel weight. The slice was continuously perfused with Krebs solution at 3.0 ml/min at 34°C, maintained by an in-line solution heater and a temperature controller (TC-344B; Warner Instruments).
Electrophysiological recordings.
Recordings of postsynaptic currents were performed using whole cell voltage-clamp as described previously (Zhang et al. 2010). All recordings were conducted in randomly selected lamina II neurons ipsilateral to the surgery side (CCI or sham). Lamina II was identified by its distinctive translucent appearance, and neurons were located using a fixed-stage microscope (BX51WI; Olympus, Tokyo, Japan) with infrared differential interference contrast (DIC) illumination. Electrodes for the whole cell recordings were triple-pulled from borosilicate glass capillary tubes using a horizontal electrode puller (P-97; Sutter Instrument, Novato, CA). The impedance of the pipette was 4–7 MΩ when filled with internal solution containing 110.0 mM Cs2SO4, 5.0 mM KCl, 2.0 mM MgCl2, 0.5 mM CaCl2, 5.0 mM HEPES, 5.0 mM EGTA, 5.0 mM ATP-Mg, and 0.5 mM Na-GTP, adjusted to pH 7.2–7.4 with 1 M CsOH (290–320 mosM). QX314, a sodium channel blocker, was added to the internal solution to suppress action potentials in targeted neurons. Recordings of postsynaptic currents began ∼5 min after whole cell access was established and the current reached a steady state. Input resistance was monitored and recording was abandoned if this changed by more than 15%. Signals were amplified using an MultiClamp700B (Molecular Devices Cellular Neurosciences, Foster City, CA) at a holding potential of 0 mV for sIPSCs and −70 mV for sEPSCs, filtered at 2 kHz, digitized at 10 kHz (Digidata 1322A; Molecular Devices Cellular Neurosciences), and stored on a personal computer for later analysis.
Immunohistochemistry.
CCI and sham mice (n = 4 per group, per time point) were deeply anesthetized with pentobarbital sodium (Nembutal; 100 mg/kg ip) and perfused through the ascending aorta with warm saline, followed by cold 4% paraformaldehyde in 0.1 M phosphate buffer. The L5 spinal cord segment was removed, postfixed in 4% paraformaldehyde for 4 h, and then cryoprotected in 30% sucrose solution at 4°C for at least one night. Transverse free-floating spinal cord sections (20 μm) were cut in a cryostat and processed for immunofluorescent staining. All of the sections were first blocked with 10% normal donkey serum (NDS) and 0.2% Triton X-100 in phosphate-buffered saline (PBS) for 1 h at room temperature. The sections were then incubated over two nights at 4°C in 5% NDS and 0.2% Triton X-100 in PBS containing the primary antibodies for TNFR1 (rabbit, 1:1,000; Abcam) and glial fibrillary acidic protein (GFAP; mouse, 1:1,000; Cell Signaling Technology). The sections were then incubated with cyanine 3 (Cy3)- and FITC-conjugated secondary antibodies in 5% NDS and 0.2% Triton X-100 overnight at 4°C. To test the specificity of the TNFR1 antibody, a preabsorption experiment was conducted by incubating TNFR1 antibody (1 μg/ml; Abcam) with TNFR1 peptide (5 μg/ml) for 1 h at room temperature before incubating with spinal cord slices.
Chemicals.
Recombinant mouse TNF-α was purchased from R&D Systems and prepared as stock solutions at 10 μg/ml in PBS with 0.1% bovine serum albumin. Bicuculline and strychnine were obtained from Sigma (St. Louis, MO).
Data analysis: electrophysiology.
Data are means ± SE. The sIPSCs and sEPSCs were analyzed off-line. Amplitude and frequency of sIPSCs and sEPSCs were analyzed from 1-min segments collected 30 s before, following 2-min application, and then 10–15 min after application of TNF-α. The sIPSCs and sEPSCs were detected as a signal with fast rise time (<200 μs) achieving an amplitude two times threshold above the background noise (MiniAnalysis; Synaptosoft, Decatur, GA). The interevent intervals of sIPSCs or sEPSCs of each cell (CCI or sham) were then analyzed using the Kolmogorov-Smirnov test to determine and categorize each cell as either responsive or not to TNF-α (MiniAnalysis; Synaptosoft). Further statistical analyses of grouped responses were carried out using GraphPad Prism 5.0 software. Fisher's exact test was used to compare the proportion of cells responsive to TNF-α in the CCI or sham groups. Within-group (CCI or sham) differences in responses before and after drug application were evaluated with a paired t-test. Finally, differences in baseline and post-TNF responses between CCI and sham groups were evaluated with one-way analysis of variance (ANOVA). P < 0.05 was considered in all analyses to indicate statistical significance.
Data analysis: immunohistochemistry.
Ten slices were randomly selected from each animal for analysis using NIS Elements imaging software (Nikon) as previously described (Zhang et al. 2011). The area of translucent lamina II both ipsilateral and contralateral to CCI (or sham) was determined and outlined from images captured while viewed under DIC. Fluorescence images from the same orientation first had background subtracted, and then the relative brightness of TNFR1 or GFAP immunoreactivity for the whole of lamina II on both sides was measured for each slice. The exposure times and illumination intensities were identical for all images in a given experiment. Side-to-side differences in fluorescence intensity within the CCI and sham treatment groups were determined using paired t-tests.
RESULTS
CCI induced prominent mechanical hypersensitivity in mice.
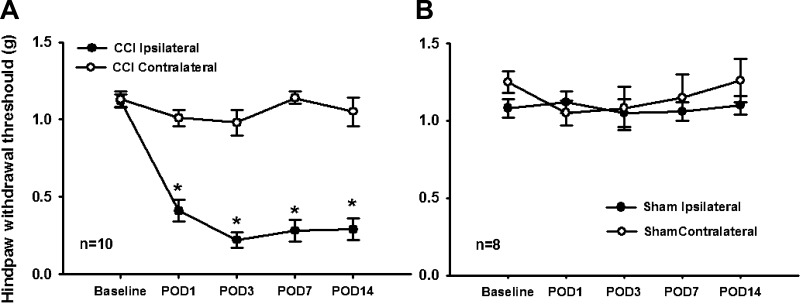
The withdrawal threshold to mechanical stimulation showed a decrease in the ipsilateral compared with the contralateral paw in CCI mice by 1 day after surgery, and this difference lasted at least 14 days. The mechanical threshold significantly decreased in the ipsilateral paw from 1.12 ± 0.04 to 0.27 ± 0.07 g in CCI mice by 14 days after surgery, whereas the withdrawal threshold in the contralateral paw remained at 1.18 ± 0.04 g (Fig. 1A). Mechanical withdrawal threshold was not altered significantly in sham surgery mice (from 1.24 ± 0.07 to 1.11 ± 0.07 g) through 14 days after surgery (Fig. 1B).
Fig. 1.
Scatter and line plots show the mechanical withdrawal threshold (y-axis, in g) of the ipsilateral (filled circles) and contralateral paws (open circles) in mice with either a chronic constriction injury (CCI) of the sciatic nerve (A) or sham sciatic nerve injury (B) over time (x-axis, in days). The mechanical withdrawal threshold of the paw ipsilateral to the CCI was significantly reduced at postoperative day (POD) 1, and this remained across the time interval observed (A). The threshold of hindpaw withdrawal showed no change in sham mice (B).
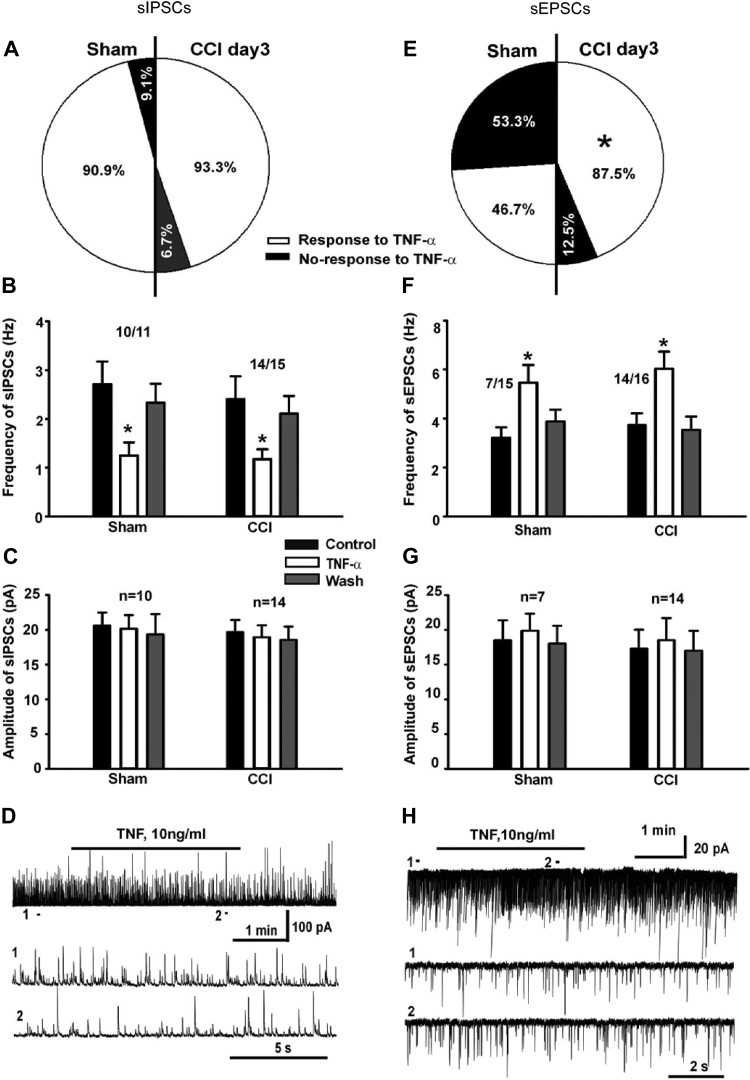
Effect of TNF-α on inhibitory and excitatory synaptic input to spinal cord SG neurons 3 days after CCI.
TNF-α inhibits inhibitory inputs (disinhibits) spinal SG neurons in naive mice, resulting in an increased magnitude of excitatory inputs to these cells (Zhang et al. 2010). To test whether peripheral nerve injury induces plasticity in these effects, the effect of TNF-α (10 ng/ml, 3 min) on the frequency and amplitude of sIPSCs and sEPSCs of spinal SG neurons was determined in sham and CCI mice 3 days after surgery.
There was no significant difference between the baseline sIPSC frequencies between the CCI and sham surgery groups. The baseline frequency of sIPSCs in sham mice was 2.41 ± 0.46 Hz (n = 11), and the baseline frequency of sIPSCs in CCI mice was 2.71 ± 0.46 Hz (n = 15). The proportions of neurons showing response to TNF-α also were not changed given that 10 of 11 (90.9%) SG neurons responded to TNF-α in sham mice and 14 of 15 (93.3%) SG neurons responded to TNF-α in CCI mice based on analysis of interevent intervals of sIPSCs before and after drug application (Fig. 2A). TNF-α significantly reduced the frequency of sIPSCs in both sham (from 2.41 ± 0.47 to 1.17 ± 0.20 Hz, n = 10, P < 0.05) and CCI mice (from 2.71 ± 0.46 to 1.25 ± 0.27 Hz, n = 14, P < 0.05; Fig. 2, B and D). There was no significant difference in the magnitude of inhibition between sham (51.45%) and CCI mice (53.87%). TNF-α had no effect on the amplitude of sIPSCs in either sham or CCI mice (Fig. 2, C and D). These results indicate that the effect of TNF-α on inhibitory synaptic transmission to SG neurons was not changed at 3 days following peripheral nerve injury.
Fig. 2.
Pie charts, bar graphs, and representative whole cell recordings summarize the effect of tumor necrosis factor-α (TNF-α) on synaptic transmission in spinal substantia gelatinosa (SG) neurons in mice at 3 days following CCI compared with sham sciatic nerve injury in mice. Pie charts show the percentages of cells that responded to TNF-α with a change in frequency of spontaneous inhibitory synaptic currents (sIPSCs; A) and spontaneous excitatory synaptic currents (sEPSCs; E) in sham (left side of each pie chart) and CCI mice (right side of each pie chart). A significantly larger proportion of SG neurons in CCI mice showed a change in sEPSC frequency than in sham mice (E). Bar graphs in B and F summarize the mean (and SE) change in frequency of sIPSCs (B) and sEPSCs (F) before (control; solid bars), after 10-min application of TNF-α (open bars), and after washout (shaded bars) for those cells showing response in sham and CCI mice. The number of SG neurons responding to TNF-α out of the total number of neurons is indicated above bars for sham and CCI mice. Bar graphs in C and G show the mean (and SE) amplitude of sIPSCs (C) and sEPSCs (G) before (solid bars), after 10-min application of TNF-α (open bars), and after washout (shaded bars) in sham and CCI mice (n is the number of neurons responding to TNF-α). *P < 0.05, significant difference compared with the baseline control recording. Finally, representative examples of analog whole cell recordings for SG neurons before (1; expanded time base in 2nd row) and then following application of TNF-α (2; expanded time base in 3rd row) for cells showing suppression of sIPSCs (D) and increase of sEPSCs (H) are shown. The washout segment is not shown.
On the other hand, the effect of TNF-α on sEPSCs was increased in CCI 3 days after injury compared with sham-operated mice. A total of 15 neurons in sham and 16 neurons in CCI mice were recorded in SG 3 days after injury. There was no significant difference between the baseline sEPSC frequency between sham and CCI mice, with the mean baseline frequency of sEPSCs in sham mice at 4.14 ± 0.55 Hz (n = 15) and the baseline frequency of sEPSCs in CCI mice at 3.73 ± 0.48 Hz (n = 16). TNF-α significantly increased the frequency of sEPSCs of in 7 of 15 (46.7%) SG neurons from 3.21 ± 0.43 to 5.47 ± 0.72 Hz (n = 7, P < 0.05; Fig. 2, E, F, and H) in sham mice but increased the frequency of sEPSCs in 14 of 16 SG neurons (87.5%) from 3.45 ± 0.51 to 6.03 ± 0.70 Hz (n = 14, P < 0.05; Fig. 2, E and F) in CCI mice. Although the effect on sEPSC rate was not significantly different, with sham rats showing an increase of 170.4% and CCI rats showing an increase to 174.8% of the baseline rate, the overall percentage of neurons responding to TNF was significantly greater in CCI mice than in sham mice (Fig. 2E). TNF-α again had no effect on the amplitude of sEPSCs (Fig. 2G) in either sham or CCI mice. These results indicate that in contrast to the effects on sIPSCs, TNF-α had an augmented effect on excitatory synaptic transmission of spinal SG neurons at 3 days after CCI.
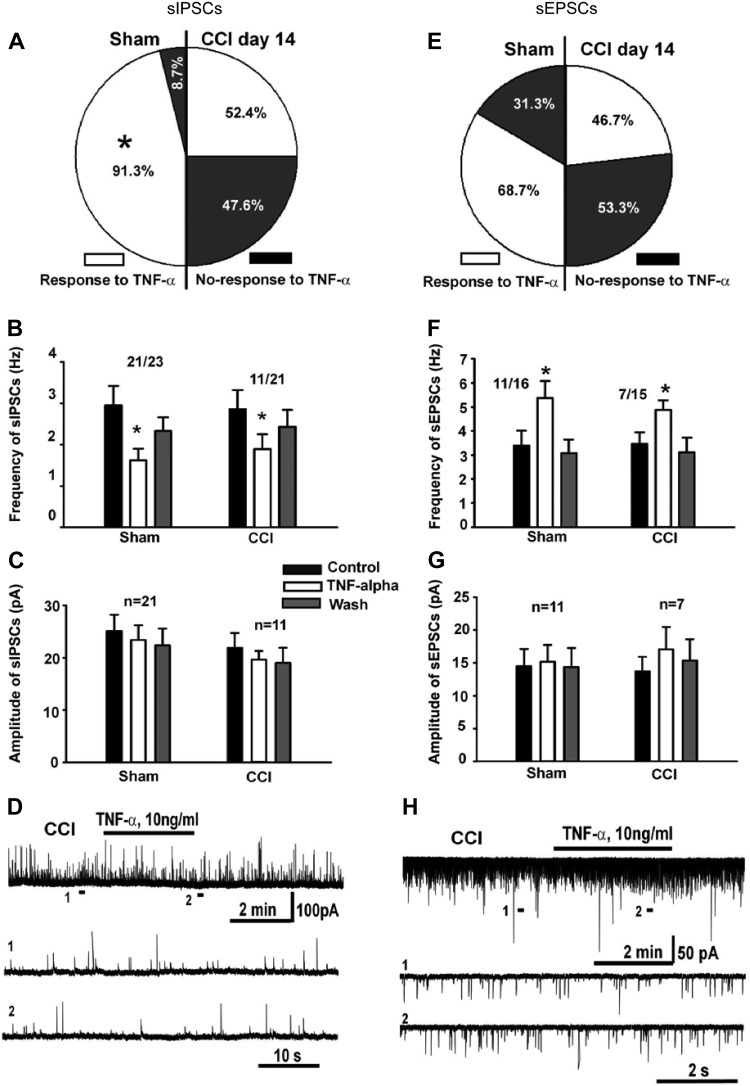
Effect of TNF-α on inhibitory and excitatory synaptic input to spinal cord SG neurons 14 days after CCI.
TNF-α reduced the frequency of sIPSCs in 21 of 23 (91.3%) neurons in sham mice (Fig. 3A) from an average of 2.95 ± 0.47 to 1.62 ± 0.28 Hz (n = 21, P < 0.05; Fig. 3B), a 54.9% reduction from the baseline before TNF-α application. Hence, TNF had the same effect on both the numbers of cells affected and overall decrease in rate at both 3 and 14 days in sham surgery mice. In contrast, only 11 of 21 cells (52.4%) responded to TNF-α in CCI mice, which was significantly lower than the response rate in sham mice (91.3%; Fig. 3A). The effect of TNF-α in those cells that responded was similar with the mean frequency of sIPSCs dropping from 2.85 ± 0.46 to 1.89 ± 0.36 Hz (n = 11, P < 0.05; Fig. 3B), or 66.42 ± 0.53% of baseline. Again, there was no significant effect of TNF-α on the amplitude of sIPSCs of SG neurons in sham mice or CCI mice (Fig. 3C). These results suggest that the effect of TNF-α on inhibitory synaptic transmission of spinal SG neurons is reduced 14 days after CCI.
Fig. 3.
Pie charts, bar graphs, and representative whole cell recordings summarize the effect of TNF-α on synaptic transmission in spinal SG neurons in mice at 14 days following CCI compared with sham sciatic nerve injury in mice. Pie charts show the percentages of cells that responded to TNF-α with a change in frequency of sIPSCs (A) and sEPSCs (B) in sham (left side of each pie chart) and CCI mice (right side of each pie chart). A significantly smaller proportion of SG neurons in CCI mice showed a change in sIPSC frequency than in sham mice (A). Bar graphs in B and F summarize the mean (and SE) change in frequency of sIPSCs (B) and sEPSCs (F) before (solid bars), after 10-min application of TNF-α (open bars), and after washout (shaded bars) for those cells showing response in sham and CCI mice. The number of SG neurons responding to TNF-α out of the total number of neurons is indicated above bars for sham and CCI mice. Bar graphs in C and G show the mean (and SE) amplitude of sIPSCs (C) and sEPSCs (G) before (solid bars), after 10-min application of TNF-α (open bars), and after washout (shaded bars) in sham and CCI mice (n is the number of neurons responding to TNF-α). *P < 0.05, significant difference compared with the baseline control recording. Finally, representative examples of analog whole cell recordings for SG neurons before (1; expanded time base in 2nd row) and then following application of TNF-α (2; expanded time base in 3rd row) for cells showing suppression of sIPSCs (D) and increase of sEPSCs (H) are shown. The washout segment is not shown.
The effect of TNF-α on the sEPSCs was also tested 14 days after nerve injury. TNF-α significantly increased the frequency of sEPSCs in 11 of 16 (68.7%) neurons in sham mice (Fig. 3E) with the mean frequency increasing from 3.39 ± 0.62 to 5.37 ± 0.89 Hz (n = 11, P < 0.05; Fig. 3F), or 164.57 ± 12.66% of baseline, an effect similar to that observed at 3 days after the sham surgery. In CCI mice, sEPSCs were recorded from a total of 15 spinal SG neurons, and 7 cells (46.7%; Fig. 3E) responded to TNF-α where the mean frequency of sEPSCs increased from 3.46 ± 0.37 to 4.88 ± 0.39 Hz (n = 7, P < 0.05; Fig. 3F), or 143.96 ± 6.31% of baseline. Although TNF-α affected a smaller proportion of the neurons from CCI than sham mice, this difference did not achieve statistical significance. Finally, once again, TNF-α had no significant effect on the amplitude of sEPSCs in either sham mice or CCI mice (Fig. 3G).
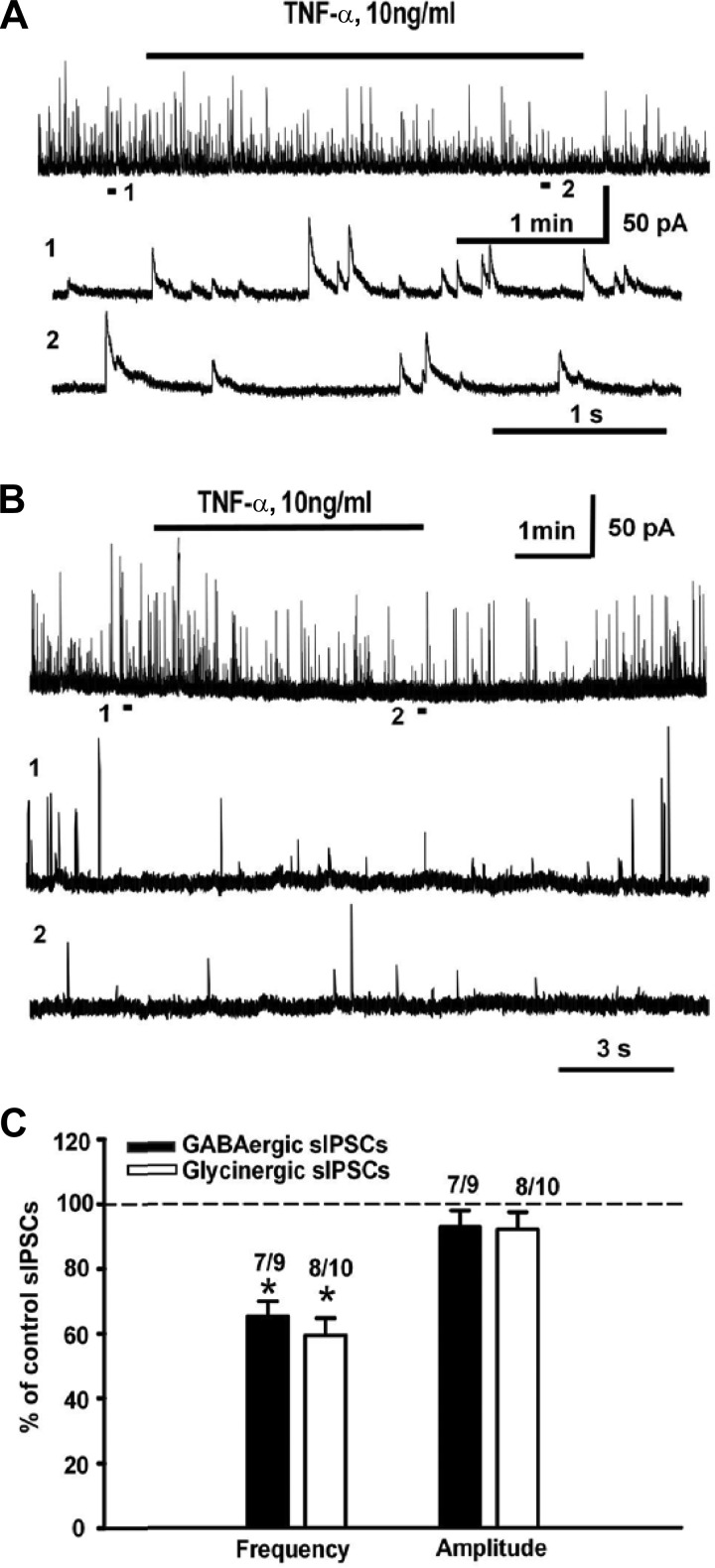
Effect of TNF-α on GABAergic and glycinergic inhibitory input to SG neurons in the spinal cord dorsal horn.
Inhibitory neurotransmission in the spinal cord is primarily mediated by GABA and glycine. The possible differential effect of TNF-α on these inhibitory synaptic processes was examined pharmacologically by adding bicuculline (10 μM) or strychnine (1 μM) in the recording chamber. As shown in Fig. 4A, GABAergic sIPSCs were defined by their characteristic long duration, with a mean rise time of 4.74 ± 0.38 ms and mean decay time of 19.29 ± 1.88 ms. TNF-α significantly decreased the frequency of GABAergic IPSCs by 65.6% (from 1.89 ± 0.61 to 1.19 ± 0.39 Hz, n = 7, P < 0.05; Fig. 4C) in 7 of 9 neurons without changing the amplitude (19.56 ± 3.51 to 17.60 ± 2.69 pA, 92.87% of baseline). As shown in Fig. 4B, glycinergic postsynaptic currents were defined by their characteristic short duration, with a mean rise time of 3.73 ± 0.42 ms and mean decay time of 4.87 ± 0.33 ms. TNF-α also decreased the frequency of glycinergic IPSCs by 59.34% in 8 of 10 neurons (from 1.56 ± 0.67 to 0.86 ± 0.34 Hz, n = 8, P < 0.05; Fig. 4C) without significant effect on the amplitude (from 29.74 ± 4.18 to 27.03 ± 3.88 pA, 92.13% of control). These results suggest that TNF-α indiscriminately inhibits both GABAergic and glycinergic inhibitory inputs to SG neurons.
Fig. 4.
Representative analog recordings and bar graphs summarize the effect of TNF-α on GABAergic (A and solid bars in C) and glycinergic (B and open bars in C) inputs to SG neurons. The representative analog recordings in the top row of A and B show a long time base sample before, during (horizontal line above recording), and after application of TNF-α, whereas the expanded time bases 1 and 2 show samples before and then late during TNF-α application, respectively. *P < 0.05.
Expression of TNFR1 in the spinal cord dorsal horn over time after CCI.
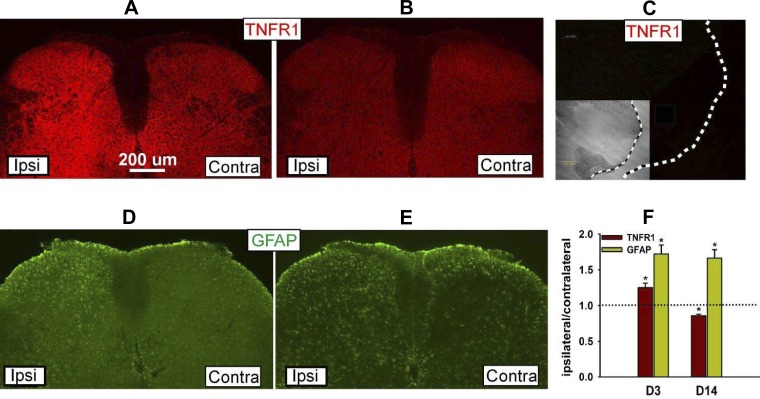
TNF-α receptors are normally expressed in the spinal cord of naive animals (Holmes et al. 2004; Ohtori et al. 2004). Previous work confirmed that TNFR1 is expressed throughout the spinal cord gray matter in both neurons and astrocytes, whereas TNFR2 is expressed only in large ventral horn neurons of naive mice (Zhang et al. 2010). As shown in Fig. 5, the expression of TNFR1 and GFAP was upregulated in the spinal dorsal horn ipsilateral to injury side by 3 days after CCI (Fig. 5, A and D). TNFR1 and GFAP expression specifically in the ipsilateral SG increased to 125 ± 6.3% (n = 24, P < 0.05) and 172.3 ± 12.3% (n = 24, P < 0.05) compared with that in the contralateral SG at 3 days after injury (Fig. 5F). In contrast, at 14 days after CCI, the expression of TNFR1 was downregulated in the ipsilateral dorsal horn (Fig. 5, B and E). The levels in SG specifically were reduced on the ipsilateral side to 85.3 ± 2.3% (n = 32, P < 0.05) of the level on the contralateral side (Fig. 5F). Preincubation of TNFR1 peptide and TNFR1 antibody prevented the specific staining of TNFR1 in spinal cord (Fig. 5C). These data indicate that the expression of TNFR1 ipsilateral to the CCI is upregulated at day 3, consistent with previous reports, but surprisingly downregulated at day 14.
Fig. 5.
Representative immunohistochemical sections show the expression of TNF-α receptor 1 (TNFR1; A and B) and glial fibrillary acidic protein (GFAP; D and E) in the ipsilateral (Ipsi; left side) and contralateral (Contra; right side) spinal dorsal horn 3 (A and D) and 14 days (B and E) after CCI. No signal was detected when an excess of TNFR1 was preincubated with the primary antibody (C; inset is differential interference contrast view of slice for orientation). Bar graph summarizes the grouped quantification data where the ratio of fluorescence in the ipsilateral-to-contralateral SG are compared to indicate downregulation of TNFR1 and activation of GFAP in the ipsilateral compared with contralateral spinal SG at day 3 (D3) and day 14 (D14) following CCI. *P < 0.05.
DISCUSSION
TNF-α has many well-documented roles in promoting inflammatory and nerve injury-related pain, especially in the peripheral nervous system, but less is known concerning the effects TNF-α might have in altering spinal synaptic transmission in promoting nociceptive processing. In the present study, TNF-α was shown to induce a number of changes in spinal inhibitory and excitatory synaptic processes that would be consistent with a net excitatory effect on synaptic transmission, and some of these effects showed plasticity over time in a mouse model of CCI. TNF-α produces a prominent disinhibitory effect through suppression of sIPSCs both in sham mice and in mice 3 days after CCI. Not surprisingly, TNF-α also enhanced excitatory synaptic transmission in sham mice, and this effect was exaggerated in CCI mice 3 days after nerve injury, affecting a larger population of neurons than normally observed in naive mice. In contrast to the net excitatory effect of TNF-α on SG synaptic physiology at 3 days after CCI, these effects were blunted on both inhibitory and excitatory synaptic transmission at 14 days after nerve injury. Parallel to the physiological effects, immunohistochemical staining shows that TNFR1 is upregulated at day 3 but downregulated at day 14 in the ipsilateral vs. contralateral side of the dorsal horn in CCI mice.
A number of behavioral studies have suggested that TNF-α plays a significant role in the development of inflammatory and neuropathic pain. Mice with genetic deletion of TNF-α or TNFR1 show reduced nociceptive sensitivity compared with wild-type littermates after nerve injury (Nadeau et al. 2011); and perineural or intrathecal injection resulted in hyperresponsiveness to peripheral heat and mechanical stimuli (Gao et al. 2009; Narita et al. 2008; Schafers et al. 2008). Conversely, CCI-induced hypersensitivity is reversed with peripheral administration of neutralizing antibodies to TNF-α or TNFRs, in particular TNFR1 (Sommer et al. 1998; Sorkin and Doom 2000). Similarly, intraperitoneal injection of the TNF-α inhibitor etanercept suppresses hypersensitivity after nerve injury (Iwatsuki et al. 2013), and mice lacking TNF-α or TNFR1 show reduced nociceptive sensitivity compared with wild-type littermates after nerve injury (Nadeau et al. 2011). Parallel to these behavioral studies, TNF-α was found to be increased in both dorsal root ganglia (DRG) and spinal cord following nerve injury (Cha et al. 2012; Xu et al. 2006).
The physiological bases underlying the behavioral effects of TNF-α are still to be fully defined. TNF-α directly activates primary afferent fibers when applied along peripheral axons (Schafers et al. 2003a) and modifies synaptic activity of spinal cord neurons in naive mice (Kawasaki et al. 2008; Zhang et al. 2010). More specifically, at the spinal level, acute application of TNF-α suppresses sIPSCs and increases sEPSCs in SG neurons, and this effect appears largely driven by a direct inhibition of the excitability of a subset of spinal GABA neurons (Zhang and Dougherty 2011). The net effect of TNF-α in both the peripheral and central nervous system would be consistent with promoting nociceptive processing and hence contributing to primary and secondary forms of hyperalgesia.
In the present study, TNF-α very similarly suppressed inhibitory synaptic transmission in SG neurons in mice with sham or CCI nerve injury as in naive mice but was found to have an exaggerated effect on the excitatory synaptic transmission in CCI mice as indicated by the larger percentage of neurons showing increases in sEPSCs. In that the increase of sEPSCs in naive mice were entirely accounted for by suppression of sIPSCs (Zhang et al. 2010), the more pronounced increase of sEPSCs in the context of similar levels of suppression of sIPSCs in CCI mice would suggest an acquired direct effect of TNF-α on subsets of excitatory spinal neurons. The idea that under conditions of nerve injury TNF-α might have a preferential effect on a subset of spinal neurons is not without precedent given that brain-derived neurotrophic factor and CCI differentially affect the activities of SG neurons identified by spike-burst properties (Lu et al. 2009, 2012).
On the other hand, at 14 days after CCI, the effect of TNF-α became blunted with reduced percentages of neurons showing either disinhibitory or excitatory effects. Combined, the plasticity in effects of TNF-α on spinal synaptic processes would suggest a role in promoting spinal nociceptive processing (sensitization) early in the time course following CCI of the sciatic nerve but a diminishing role in the longer-term stages following injury. Indeed, failure of the effects of TNF-α to resolve over time following nerve injury may be a key event in the transition between acute and chronic pain conditions. A caveat in these results is that equal samples of neurons were collected at the different time points. The distribution of sexes of the mice in the two samples was equal, so the potential for a differential effect of TNF-α on spinal synaptic processing between male and female mice seems unlikely. The cells that were selected for study were also equal among the regions of the SG, and so it would also seem unlikely that unbalanced populations of excitatory vs. inhibitory neurons were sampled in the day 3 and day 14 CCI mice. Moreover, given that sIPSCs and sEPSCs are reflective of the summation of inputs from large groups of upstream neurons, it seems unlikely that a sampling bias affected the final results.
TNF-α has two receptors, TNFR1 and TNFR2. Activation of TNFR1 triggers the dominant pathway for the major effects of TNF-α (Vandenabeele et al, 1995), and several lines of evidence suggest that TNFR1 is the major receptor promoting pain signal processing by TNF-α after nerve injury or inflammation (Jin and Gereau 2006; Sachs et al. 2002; Sommer et al. 1998). Consistent with these findings, the TNF-α-induced disinhibition of spinal synaptic transmission was also shown to be mediated through TNFR1 but not TNFR2 (Zhang et al. 2010). The expression of TNFR1 was found to show plasticity over time following CCI, which paralleled the changes in physiological responses discussed above. Hence, the expression of TNFR1 was increased at day 3 after CCI when the physiological effects of TNF-α were also exaggerated, but then receptor expression was reduced by day 14, where the physiological effects of TNF-α were also becoming blunted. The dynamic change of the expression of TNFR1 in spinal cord dorsal horn following CCI is intriguing. Several lines of evidence have shown that TNFR1 increases early in time following nerve injury. For example, Schafers et al. (2003b) found that TNFR1 mRNA levels in both DRG and the spinal dorsal horn increased 1 day after spinal nerve ligation and returned to control levels by 7 and 14 days, respectively. Lee et al. (2004) reported the same temporal pattern for the TNFRs as well as TNF-α in DRG and spinal cord with CCI of the sciatic nerve. Finally, TNF-α and TNFR1 immunoreactivity increased in both DRG and spinal cord by 1 day after transection of the L5 ventral root and persisted for about 2 wk (Xu et al. 2006). The observations here that TNFR1 expression in dorsal horn was increased and the effect of TNF-α on the frequency of sEPSCs was enhanced 3 days after CCI is consistent with these previous studies and clearly show that the time course of increased TNFR1 expression is shorter than that of mechanical hyperresponsiveness produced by nerve injury. Thus increased TNFR1 expression and enhanced physiological effects of TNF-α appear to have important roles in increasing the overall excitability of the spinal dorsal horn, contributing to pain in the early stages of nerve injury, but have a reducing influence in maintaining nerve injury pain.
Inhibitory tone in the spinal cord dorsal horn is determined by the output of inhibitory GABA- and glycine-containing interneurons. A recent study showed that GABA neurons are tonically inhibited by glycine or GABA in a regionally distinct fashion (Takazawa and MacDermott 2010). Inhibitory neurons at the lamina II/III border were shown to be under tonic glycine-mediated inhibition, whereas the more dorsal lamina I and IIo inhibitory neurons were primarily under GABAergic inhibition. The present findings did not seem consistent with this differential pattern of inhibitory connections, but rather were more consistent with results reported by others (Labrakakis et al. 2009) in that cells throughout SG showed both GABA- and glycine-mediated IPSCs and these were equally sensitive to TNF-α. Glycine and GABA have a common vesicular transporter (vesicular inhibitory amino acid transporter, VIAAT) and thus can be co-packaged into the same synaptic vesicles and co-released from the same terminals (Wojcik et al. 2006). Thus the pure GABAergic or glycinergic IPSCs are actually dependent on the receptors (GABAA receptor or glycine receptor, respectively), which are expressed in postsynaptic neurons (Jonas et al. 1998; Mitchell et al. 2007). The current study showed TNF-α equally inhibited both GABAergic and glycinergic inputs, indicating that these neurons have both receptors throughout the lamina II regardless of position in the SG. An important caveat, however, is that TNF-α was bath applied and may have activated affected inhibitory inputs to these cells from multiple other dorsal horn areas.
In conclusion, electrophysiology and immunohistochemistry results indicate that the effect of TNF-α on the regulation of overall excitability of spinal dorsal horn is enhanced in the acute phase and attenuated in the late phase of CCI neuropathy. The plasticity in the physiological effects of TNF-α on the excitability of spinal cord neurons following nerve injury appears mediated by plasticity in the expression of its key receptor TNFR1 expression at different phases. These results suggest that TNF-α and TNFR1 are important in the development but may not be as central in the maintenance of nerve injury-related pain.
GRANTS
This work was supported by National Institutes of Health Grants R01 NS046606 and CA124787.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the authors.
AUTHOR CONTRIBUTIONS
H.-M.Z. and P.M.D. conception and design of research; H.-M.Z. performed experiments; H.-M.Z., H.Z., and P.M.D. analyzed data; H.-M.Z., H.Z., and P.M.D. interpreted results of experiments; H.-M.Z. prepared figures; H.-M.Z. drafted manuscript; H.-M.Z., H.Z., and P.M.D. approved final version of manuscript; H.Z. and P.M.D. edited and revised manuscript.
REFERENCES
- Carlton SM, Dougherty PM, Pover CM, Coggeshall RE. Neuroma formation and numbers of axons in an experimental peripheral neuropathy. Neurosci Lett 131: 88–92, 1991 [DOI] [PubMed] [Google Scholar]
- Cha MH, Nam TS, Kwak Y, Lee H, Lee BH. Changes in cytokine expression after electroacupuncture in neuropathic rats. Evid Based Complement Alternat Med 2012: 792765, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods 53: 55–63, 1994 [DOI] [PubMed] [Google Scholar]
- Costigan M, Scholz J, Woolf CJ. Neuropathic pain: a maladaptive response of the nervous system to damage. Annu Rev Neurosci 32: 1–32, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunha FQ, Poole S, Lorenzetti BB, Ferreira SH. The pivotal role of tumor-necrosis-factor-alpha in the development of inflammatory hyperalgesia. Br J Pharmacol 107: 660–664, 1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty PM, Garrison CJ, Carlton SM. Differential influence of local anesthetic upon two models of experimentally-induced peripheral mononeuropathy in the rat. Brain Res 570: 109–115, 1992 [DOI] [PubMed] [Google Scholar]
- Ferreira SH, Lorenzetti BB, Poole S. Bradykinin initiates cytokine-mediated inflammatory hyperalgesia. Br J Pharmacol 110: 1227–1231, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao YJ, Ji RR. Chemokines, neuronal-glial interactions, and central processing of neuropathic pain. Pharmacol Ther 126: 56–68, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao YJ, Zhang L, Samad OA, Suter MR, Yasuhiko K, Xu ZZ, Park JY, Lind AL, Ma Q, Ji RR. JNK-induced MCP-1 production in spinal cord astrocytes contributes to central sensitization and neuropathic pain. J Neurosci 29: 4096–4108, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- George A, Buehl A, Sommer C. Wallerian degeneration after crush injury of rat sciatic nerve increases endo- and epineurial tumor necrosis factor-alpha protein. Neurosci Lett 372: 215–219, 2004 [DOI] [PubMed] [Google Scholar]
- George A, Schmidt C, Weishaupt A, Toyka KV, Sommer C. Serial determination of tumor necrosis factor-alpha content in rat sciatic nerve after chronic constriction injury. Exp Neurol 160: 124–132, 1999 [DOI] [PubMed] [Google Scholar]
- Holmes GM, Hebert SL, Rogers RC, Hermann GE. Immunocytochemical localization of TNF type 1 and type 2 receptors in the rat spinal cord. Brain Res 1025: 210–219, 2004 [DOI] [PubMed] [Google Scholar]
- Iwatsuki K, Arai T, Ota H, Kato S, Natsume T, Kurimoto S, Yamamoto M, Hirata H. Targeting anti-inflammatory treatment can ameliorate injury-induced neuropathic pain. PLoS One 8: e57721, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin XC, Gereau RW. Acute p38-mediated modulation of tetrodotoxin-resistant sodium channels in mouse sensory neurons by tumor necrosis factor-alpha. J Neurosci 26: 246–255, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonas P, Bischofberger J, Sandkuhler J. Corelease of two fast neurotransmitters at a central synapse. Science 281: 419–424, 1998 [DOI] [PubMed] [Google Scholar]
- Kawasaki Y, Zhang L, Cheng JK, Ji RR. Cytokine mechanisms of central sensitization: distinct and overlapping role of interleukin-1beta, interleukin-6, and tumor necrosis factor-alpha in regulating synaptic and neuronal activity in the superficial spinal cord. J Neurosci 28: 5189–5194, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labrakakis C, Lorenzo LE, Bories C, Ribeiro-Da-Silva A, De Koninck Y. Inhibitory coupling between inhibitory interneurons in the spinal cord dorsal horn. Mol Pain 5: 24, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HL, Lee KM, Son SJ, Hwang SH, Cho HJ. Temporal expression of cytokines and their receptors mRNAs in a neuropathic pain model. Neuroreport 15: 2807–2811, 2004 [PubMed] [Google Scholar]
- Lu VB, Colmers WF, Smith PA. Long-term effects of brain-derived neurotrophic factor on the frequency of inhibitory synaptic events in the rat superficial dorsal horn. Neuroscience 161: 1135–1143, 2009 [DOI] [PubMed] [Google Scholar]
- Lu VB, Colmers WF, Smith PA. Long-term actions of BDNF on inhibitory synaptic transmission in identified neurons of the rat substantia gelatinosa. J Neurophysiol 108: 441–452, 2012 [DOI] [PubMed] [Google Scholar]
- Mannel DN. Biological aspects of tumor necrosis factor. Immunobiology 172: 283–290, 1986 [DOI] [PubMed] [Google Scholar]
- Matzner O, Devor M. Hyperexcitability at sites of nerve injury depends on voltage-sensitive Na+ channels. J Neurophysiol 72: 349–359, 1994 [DOI] [PubMed] [Google Scholar]
- Milligan ED, Watkins LR. Pathological and protective roles of glia in chronic pain. Nat Rev Neurosci 10: 23–36, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell EA, Gentet LJ, Dempster J, Belelli D. GABAA and glycine receptor-mediated transmission in rat lamina II neurones: relevance to the analgesic actions of neuroactive steroids. J Physiol 583: 1021–1040, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadeau S, Filali M, Zhang J, Kerr BJ, Rivest S, Soulet D, Iwakura Y, de Rivero Vaccari JP, Keane RW, Lacroix S. Functional recovery after peripheral nerve injury is dependent on the pro-inflammatory cytokines IL-1beta and TNF: implications for neuropathic pain. J Neurosci 31: 12533–12542, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narita M, Shimamura M, Imai S, Kubota C, Yajima Y, Takagi T, Shiokawa M, Inoue T, Suzuki M, Suzuki T. Role of interleukin-1 beta and tumor necrosis factor-alpha-dependent expression of cyclooxygenase-2 mRNA in thermal hyperalgesia induced by chronic inflammation in mice. Neuroscience 152: 477–486, 2008 [DOI] [PubMed] [Google Scholar]
- Ohtori S, Takahashi K, Moriya H, Myers RR. TNF-alpha and TNF-alpha receptor type 1 upregulation in glia and neurons after peripheral nerve injury: studies in murine DRG and spinal cord. Spine 29: 1082–1088, 2004 [DOI] [PubMed] [Google Scholar]
- Palecek J, Paleckova V, Dougherty PM, Carlton SM, Willis WD. Responses of spinothalamic tract cells to mechanical and thermal stimulation of the skin in rats with an experimental peripheral neuropathy. J Neurophysiol 67: 1562–1573, 1992 [DOI] [PubMed] [Google Scholar]
- Sachs D, Cunha FQ, Poole S, Ferreira SH. Tumour necrosis factor-α, interleukin-1β and interleukin-8 induce persistent mechanical nociceptor hypersensitivity. Pain 96: 89–97, 2002 [DOI] [PubMed] [Google Scholar]
- Sandkuhler J. Models and mechanisms of hyperalgesia and allodynia. Physiol Rev 89: 707–758, 2009 [DOI] [PubMed] [Google Scholar]
- Schafers M, Lee DH, Brors D, Yaksh TL, Sorkin LS. Increased sensitivity of injured and adjacent uninjured rat primary sensory neurons to exogenous tumor necrosis factor-alpha after spinal nerve ligation. J Neurosci 23: 3028–3038, 2003a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafers M, Sommer C, Geis C, Hagenacker T, Vandenabeele P, Sorkin LS. Selective stimulation of either tumor necrosis factor receptor differentially induces pain behavior in vivo and ectopic activity in sensory neurons in vitro. Neuroscience 157: 414–423, 2008 [DOI] [PubMed] [Google Scholar]
- Schafers M, Sorkin LS, Geis C, Shubayev VI. Spinal nerve ligation induces transient upregulation of tumor necrosis factor receptors 1 and 2 in injured and adjacent uninjured dorsal root ganglia in the rat. Neurosci Lett 347: 179–182, 2003b [DOI] [PubMed] [Google Scholar]
- Schafers M, Sorkin LS, Sommer C. Intramuscular injection of tumor necrosis factor-alpha induces muscle hyperalgesia in rats. Pain 104: 579–588, 2003c [DOI] [PubMed] [Google Scholar]
- Schäfers M, Svensson CI, Sommer C, Sorkin LS. Tumor necrosis factor-α induces mechanical allodynia after spinal nerve ligation by activation of p38 MAPK in primary sensory neurons. J Neurosci 23: 2517–2521, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shubayev VI, Myers RR. Upregulation and interaction of TNFalpha and gelatinases A and B in painful peripheral nerve injury. Brain Res 855: 83–89, 2000 [DOI] [PubMed] [Google Scholar]
- Sindrup SH, Jensen TS. Efficacy of pharmacological treatments of neuropathic pain: an update and effect related to mechanism of drug action. Pain 83: 389–400, 1999 [DOI] [PubMed] [Google Scholar]
- Sommer C, Lindenlaub T, Teuteberg P, Schafers M, Hartung T, Toyka KV. Anti-TNF-antibodies reduce pain-related behavior in two different mouse models of painful mononeuropathy. Brain Res 913: 86–89, 2001 [DOI] [PubMed] [Google Scholar]
- Sommer C, Schmidt C, George A. Hyperalgesia in experimental neuropathy is dependent on the TNF receptor 1. Exp Neurol 151: 138–142, 1998 [DOI] [PubMed] [Google Scholar]
- Sorkin LS, Doom CM. Epineurial application of TNF elicits an acute mechanical hyperalgesia in the awake rat. J Peripher Nerv Syst 5: 96–100, 2000 [DOI] [PubMed] [Google Scholar]
- Takazawa T, MacDermott AB. Glycinergic and GABAergic tonic inhibition fine tune inhibitory control in regionally distinct subpopulations of dorsal horn neurons. J Physiol 588: 2571–2587, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenabeele P, Declercq W, Beyaert R, Fiers W. Two tumour necrosis factor receptors: structure and function. Trends Cell Biol 5: 392–399, 1995 [DOI] [PubMed] [Google Scholar]
- Wagner R, Myers RR. Endoneurial injection of TNF-α produces neuropathic pain behaviors. Neuroreport 7: 2897–2901, 1996 [DOI] [PubMed] [Google Scholar]
- Watkins LR, Maier SF, Goehler LE. Immune activation: the role of pro-inflammatory cytokines in inflammation, illness responses and pathological pain states. Pain 63: 289–302, 1995 [DOI] [PubMed] [Google Scholar]
- Wojcik SM, Katsurabayashi S, Guillemin I, Friauf E, Rosenmund C, Brose N, Rhee JS. A shared vesicular carrier allows synaptic corelease of GABA and glycine. Neuron 50: 575–587, 2006 [DOI] [PubMed] [Google Scholar]
- Woolf CJ, Allchorne A, Safieh-Garabedian B, Poole S. Cytokines, nerve growth factor and inflammatory hyperalgesia: the contribution of tumor necrosis factor α. Br J Pharmacol 121: 417–424, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf CJ, Mannion RJ. Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet 353: 1959–1964, 1999 [DOI] [PubMed] [Google Scholar]
- Xu JT, Xin WJ, Zang Y, Wu CY, Liu XG. The role of tumor necrosis factor-alpha in the neuropathic pain induced by lumbar 5 ventral root transection in rat. Pain 123: 306–321, 2006 [DOI] [PubMed] [Google Scholar]
- Zhang H, Dougherty PM. Acute inhibition of signaling phenotype of spinal GABAergic neurons by tumour necrosis factor-alpha. J Physiol 589: 4511–4521, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H, Nei H, Dougherty PM. A p38 mitogen-activated protein kinase-dependent mechanism of disinhibition in spinal synaptic transmission induced by tumor necrosis factor-alpha. J Neurosci 30: 12844–12855, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]