A 50-year-old man who had undergone a liver transplantation in 2008 presented with a 2-day history of right upper quadrant tenderness and elevated transaminases; other symptoms included nausea, vomiting, and anorexia. A magnetic resonance angiogram of the liver confirmed common hepatic artery occlusion and an anastomosis biliary stricture.
An endoscopic retrograde cholangiopancreatography revealed duodenitis (likely due to mild ischemia) as well as the anastomosis stricture, which was ultimately treated with sphincterotomy and stent placement. Unfortunately, the patient developed sepsis after the procedure, resulting in a 1-month hospitalization.
Initially, he received broad empirical antimicrobial therapy including vancomycin, meropenem, and micafungin. Continuous fevers prompted collection of blood cultures, and an abdominal magnetic resonance imaging (MRI) scan revealed two areas within the liver parenchyma of high signal intensity suggestive of abscess formation. Four days later, a positive-blood-culture bottle showed long, Gram-negative rods (Fig. 1A). When subcultured to solid medium, the organism grew on blood, chocolate, and brucella agars but failed to grow on MacConkey agar; growth was notable for a distinct, strawberry-like odor. Gram staining of growth from blood agar revealed small, coccobacillary Gram-negative rods (Fig. 1B). Of significance, the same Gram-negative organism was isolated from an aspirate of the liver abscess.
FIG 1.
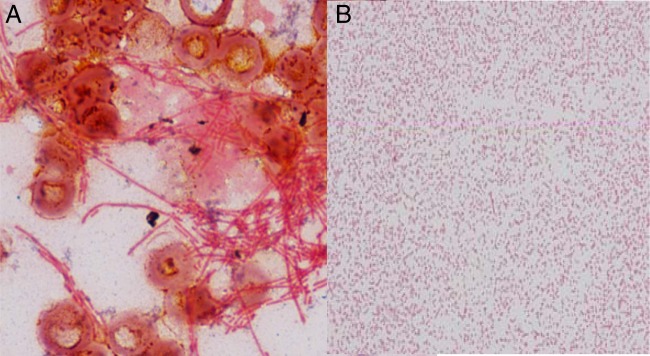
Gram stains of the unknown organism from an aliquot of the positive-blood-culture BacT/Alert SN bottle (A) and a colony grown on blood agar (magnification, ×1,000) (B).
(For answer and discussion, see page 2287 in this issue [doi:10.1128/JCM.00385-13].)


