Abstract
We systematically evaluated 5 methods for testing daptomycin versus 48 Enterococcus faecalis, 51 Enterococcus faecium, and 50 Staphylococcus aureus isolates using (i and ii) broth microdilution (BMD) with 50-mg/liter calcium medium supplementation (reference method) and 30-mg/liter calcium medium supplementation (BMD30 method), (iii) Etest, and (iv and v) MicroScan panel 33 using 2 methods to prepare the bacterial inoculum (MicroScan turbidity and MicroScan Prompt). Isolates were categorized as susceptible (S) or nonsusceptible (NS) based on measured MICs. Essential (±1 dilution) agreement (EA) and categorical (S/NS) agreement (CA) for each method were compared to the reference method. For E. faecium, categorical agreement was poor between the reference method and BMD30 as well as with the three commercial methods, with frequent false-NS results (30 for BMD30, 18 for Etest, 22 for MicroScan Prompt, and 25 for MicroScan turbidity). All E. faecalis isolates were judged to be S by the reference method; two of these isolates were categorized as NS using the BMD30 method, and one was categorized as NS by all three commercial methods. All S. aureus isolates were judged to be S using all five methods. MIC values determined by the comparator methods tended to be higher than those for the reference method, especially for E. faecium isolates. EAs between the reference BMD and BMD30, Etest, MicroScan Prompt, and MicroScan turbidity were 63%, 63%, 63%, and 56%, respectively, for E. faecium, 87%, 83%, 98%, and 80%, respectively, for E. faecalis, and all 100% for S. aureus.
INTRODUCTION
Daptomycin is a cyclic lipopeptide with activity against Gram-positive organisms. It was approved by the Food and Drug Administration initially in 2003 for the treatment of complicated skin and skin structure infections caused by Staphylococcus aureus, vancomycin-susceptible Enterococcus faecalis, and some streptococcal species. Subsequently, in 2006, it was approved for the treatment of S. aureus bacteremia and right-sided endocarditis. It is one of the few antibiotics that exhibits in vitro bactericidal activity against enterococci (1).
An evaluation of daptomycin activity trends against methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci (VRE) during a 6-year period (2005 to 2010) in 32 U.S. medical centers showed that daptomycin exhibited sustained activity against an extensive collection of clinical isolates of MRSA and VRE from numerous U.S. medical centers over the last 6 monitored years (2). However, daptomycin-nonsusceptible (NS) enterococcal isolates have been reported and multiple mechanisms of resistance have been described (3–7).
Currently, daptomycin is frequently used to treat infections caused by MRSA and VRE. In 2009, the clinical microbiology laboratory at Robert Wood Johnson University Hospital (RWJUH) (New Brunswick, NJ) began routinely testing Staphylococcus aureus and enterococci for daptomycin susceptibility using the MicroScan Pos Combo panel type 33 (PC33) MIC plate (Siemens Healthcare Diagnostics, Tarrytown, NY) instead of the epsilometer test (Etest) (bioMérieux, Durham, NC). Following this change in methodology, we noted an increase in enterococci NS to daptomycin when tested using the MicroScan system. We suspected that the MicroScan method itself, rather than a change in prevalence of truly NS isolates, was responsible for this antibiogram trend. To address our concerns, we tested 11 Enterococcus spp. isolates in parallel using the MicroScan Pos combo type 33 panel microtiter plate method, the reference broth microdilution (BMD) method, and the Etest. The results of this pilot investigation revealed numerous discrepancies between the reference method, the MicroScan susceptibility method, and the Etest. Although the MICs determined for the discrepant isolates were typically within one dilution of each other, the MicroScan method resulted in NS interpretations in 5 isolates, whereas the reference method results were interpreted as susceptible (S).
Others have reported that isolates judged to be NS to daptomycin using MicroScan methods were frequently characterized as susceptible (S) when tested by Etest or BMD (8–10). Palavecino and Burnell compared daptomycin MIC results obtained by MicroScan and by Etest for S. aureus and enterococci and found that the MicroScan method demonstrated a rate of false nonsusceptible results as high as 88% for Enterococcus faecium, 90% for E. faecalis, and 87% for S. aureus (10). Bryant et al. evaluated 150 enterococcal isolates judged to be NS to daptomycin using an automated commercial method (MicroScan) by repeat testing with a variety of methods and demonstrated that only 20% were confirmed as NS (9). In both of these studies, enterococcal isolates were initially selected because they were judged to be NS to daptomycin using the routine testing methodology in the laboratory.
In vitro susceptibility testing of daptomycin attempts to approximate physiologic levels of 50 mg/liter Ca2+ in the broth. Changes in the calcium concentration have been shown to affect the MIC determinations by a variety of methods, leading to higher- or lower-than-expected MIC determinations (11, 12). For this reason, CLSI guidelines specify supplementation of CA-MHB with calcium to a final concentration of 50 mg/liter when the BMD method is used to determine daptomycin MICs (13, 14). We suspected that the tight Ca2+ concentration tolerances required for accurate MIC determinations of daptomycin might partially explain the differences in categorization between methods.
To more rigorously explore our initial observations, we systematically evaluated five methods for testing enterococci and S. aureus susceptibility to daptomycin, which included a reference BMD method along with a BMD method using suboptimal concentrations of calcium.
MATERIALS AND METHODS
Isolate selection.
Fifty S. aureus, 48 E. faecalis, and 51 E. faecium blood culture isolates collected between January 2009 and April 2011 were selected from our frozen stock collection. Our collection consists of bacterial isolates from all positive blood cultures (except coagulase-negative staphylococci) identified at Robert Wood Johnson University Hospital and is limited to one isolate per episode of bacteremia. To minimize clonality, the first two isolates from each month of the study period were selected, with the exception of January and March of each calendar year, during which only the first isolate was selected.
Media and antimicrobial susceptibility testing.
All isolates were tested for daptomycin susceptibility in triplicate using the MicroScan Pos Combo panel type 33 (PC33) MIC microtiter panel on the MicroScan instrument, the Etest, and the manual broth microdilution methods. In each case, the replicates were performed from a single inoculum. Clinical and Laboratory Standards Institute (CLSI) guidelines were used to categorize isolates as susceptible (S) or NS (14). For S. aureus, the S category includes isolates with MICs of ≤1 μg/ml and for enterococci, it includes isolates with MICs of ≤4 μg/ml. Organisms with MICs greater than these breakpoints are considered NS. For the MicroScan method, the turbidity and proprietary inoculation (Prompt) methods were performed for all isolates.
The reference broth microdilution method was performed in-house using 2-fold dilutions of daptomycin between 0.25 μg/ml and 64 μg/ml in BBL cation-adjusted Mueller-Hinton broth II (CA-MHB) (BD, Sparks, MD) supplemented to either 30 or 50 mg/liter Ca2+. CA-MHB mixtures with final Ca2+ concentrations of 30 mg/liter and 50 mg/liter were prepared by adding 0.1 M CaCl2-2H2O. The amounts of 0.1 M CaCl2-2H2O added to the CA-MHB mixtures to achieve the desired final Ca2+ concentrations were empirically determined (Ca2+ measurements performed at Laboratory Specialists, Inc., Westlake, OH) for the specific lot of CA-MHB used in the study. Cubist Pharmaceuticals (Lexington, MA) provided the daptomycin used in this study, and a single vial was used to prepare dilutions for all BMD assays. Aliquots of daptomycin diluted to a concentration of 1,280 μg/ml were stored at −70°C. The CLSI-specified control organism (E. faecalis ATCC 29212) was included on each BMD plate.
The PC33 microtiter panels were inoculated according to the manufacturer's protocol using either the Prompt method or using a standardized turbidity-based method. The Prompt method employs the use of a collared inoculating wand that is touched to three isolated colonies. Retraction of the wand through the collar results in the suspension of the bacteria in 30 ml of stabilized 0.1% pluronic D solution. This solution is then transferred to the microtiter plate. Inoculation of the microtiter plate using the turbidity method entailed transferring 100 μl of Tryptic soy broth adjusted to a 0.5 McFarland standard to a tube containing 0.1% pluronic D. The mixture was then transferred to an inoculating tray and a Renok inoculator (Siemens) was used to transfer the suspension to the microtiter plate. MicroScan plates were incubated and read on a MicroScan Walkaway instrument (Siemens). One control plate inoculated with the CLSI-specified control organism (E. faecalis ATCC 29212) was included on each run.
Etest strips (bioMérieux, Marcy l'Etoile, France) were placed on inoculated cation-adjusted Mueller-Hinton II agar (MHA) plates (BD, Sparks, MD) and incubated according to the package insert. A control plate inoculated with the CLSI-specified control organism (E. faecalis ATCC 29212) was included each day Etests were done.
Data analysis.
Reproducibility of the BMD, MicroScan, and Etest assays was assessed by comparing the susceptibility results of the isolates tested in triplicate using each of these methods. CLSI breakpoints were used to categorize S and NS isolates based on measured MICs. When the MIC was outside the upper or lower limit of the testing method, the MIC was assigned as the next higher or lower dilution. We assigned BMD using broth supplemented with 50 mg/liter Ca2+ as the reference method and calculated essential (±1 dilution) agreement (EA) and categorical (S/NS) agreement (CA) for each commercial method compared to the reference method.
Patient privacy.
The study protocol was reviewed by the Institutional Review Board (IRB) at Rutgers-Robert Wood Johnson Medical School, which determined that this study did not meet the regulatory definition of human subjects research provided in 45 CFR 46.102 and thus did not require IRB approval.
RESULTS
MIC distributions.
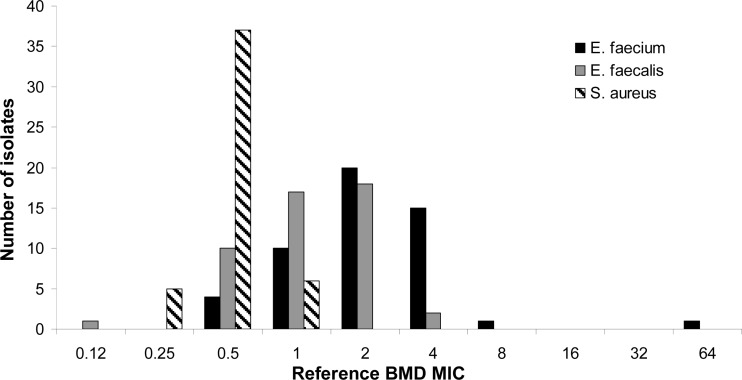
Figure 1 depicts the range of distributions of MICs obtained for each species tested using the reference BMD method. It is evident that the E. faecium isolates tended to exhibit higher daptomycin MICs than did the E. faecalis and S. aureus isolates. Notably, a significant number of the E. faecium isolates (15/51) exhibited an MIC that was at the S/NS breakpoint (4 μg/ml).
FIG 1.
Daptomycin MIC distributions determined for all isolates using the reference broth microdilution technique.
Reproducibility.
Overall, excellent intrarun reproducibility was observed for all methods and all species. In most cases, the triplicate measurements were identical (data not shown). When rare deviations from identical triplicate measurements of MICs were observed, the differences were never >2-fold (1 dilution).
Categorical agreement.
Categorical agreement between the reference BMD method, the BMD method using suboptimal calcium supplementation, and each of the commercial methods is depicted in Table 1. Categorical agreement between the reference method and the comparator methods for E. faecium was poor; 30 isolates were miscategorized using the BMD method with 30 mg/liter calcium supplementation, 18 by Etest, 22 by MicroScan Prompt, and 23 by MicroScan turbidity. Categorical agreement levels for E. faecium using each of these four comparator methods were 41%, 66%, 57%, and 52%, respectively. Conversely, agreement was excellent for E. faecalis, for which only 2 isolates were miscategorized as NS using the suboptimally calcium-supplemented BMD method and 1 was miscategorized as NS using the commercial methods. Similarly, categorical agreement for S. aureus was 100% for all comparator methods relative to the reference BMD method. Method-specific quality control results were within acceptable limits for each isolate tested by all five methods. Figure 2 demonstrates that, with the exception of 1 plate, BMD control tests, as specified by CLSI guidelines (E. faecalis ATCC 29212), were routinely within the specified range (MICs, 1 to 4 μg/ml) regardless of whether or not the Ca2+ concentration was optimal (50 mg/liter) or suboptimal (30 mg/liter) (14).
TABLE 1.
Categorical agreement between reference BMD method and BMD supplemented with 30 mg/liter calcium, Etest, MicroScan Prompt, and MicroScan turbidity methods
| Organism (no. of isolates), method used, and result | Reference BMD result (no. of isolates) |
% Agreement | |
|---|---|---|---|
| S | NS | ||
| E. faecium (51) | |||
| BMD 30 mg/liter calcium | |||
| S | 19 | 0 | 41 |
| NS | 30 | 2 | |
| Etest | |||
| S | 31 | 0 | 66 |
| NS | 18 | 2 | |
| MicroScan Prompt | |||
| S | 27 | 0 | 57 |
| NS | 22 | 2 | |
| MicroScan turbidity | |||
| S | 24 | 0 | 52 |
| NS | 25 | 2 | |
| E. faecalis (48) | |||
| BMD 30 mg/liter calcium | |||
| S | 46 | 0 | 96 |
| NS | 2 | 0 | |
| Etest | |||
| S | 47 | 0 | 98 |
| NS | 1 | 0 | |
| MicroScan Prompt | |||
| S | 47 | 0 | 98 |
| NS | 1 | 0 | |
| MicroScan turbidity | |||
| S | 47 | 0 | 98 |
| NS | 1 | 0 | |
| S. aureus (50) | |||
| BMD 30 mg/liter calcium | |||
| S | 50 | 0 | 100 |
| NS | 0 | 0 | |
| Etest | |||
| S | 50 | 0 | 100 |
| NS | 0 | 0 | |
| MicroScan Prompt | |||
| S | 50 | 0 | 100 |
| NS | 0 | 0 | |
| MicroScan turbidity | |||
| S | 50 | 0 | 100 |
| NS | 0 | 0 | |
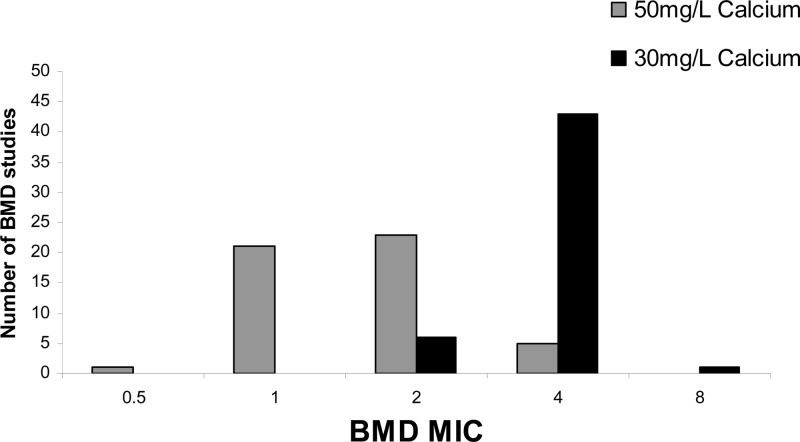
FIG 2.
Daptomycin MICs observed for the CLSI-recommended enterococcal (ATCC 29212) control organism in each BMD run with either suboptimal (30 mg/liter) Ca2+ supplementation or reference (50 mg/liter) Ca2+ supplementation.
Essential agreement.
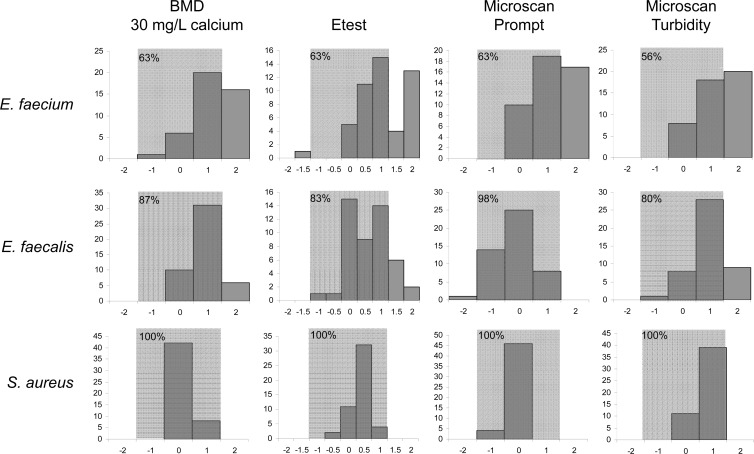
Essential agreement (EA) between the reference BMD method, the suboptimally supplemented BMD method, and the three commercial methods varied widely among species (Fig. 3). Consistent with the observations for CA, EA between the BMD reference method, the suboptimally calcium-supplemented BMD method, and all three commercial methods was poor for E. faecium but substantially better for E. faecalis and S. aureus. A trend toward higher MIC determinations, most pronounced for E. faecium but also present for E. faecalis, was evident when MICs were determined using the BMD method with suboptimal calcium supplementation, the Etest, and the MicroScan turbidity methods. For E. faecium, EA was 63% for BMD with suboptimal calcium supplementation, Etest, and MicroScan Prompt and 56% for MicroScan turbidity. For E. faecalis, EA was 87% for BMD with suboptimal calcium supplementation, 83% for Etest, 98% for MicroScan Prompt, and 80% for MicroScan turbidity compared to the reference method. Finally, for S. aureus isolates, EA was 100% for all four comparator methods.
FIG 3.
Differences (number of dilutions) in daptomycin MIC determinations between the reference method (BMD with 50 mg/liter Ca2+ supplementation), BMD with 30 mg/liter calcium supplementation, and three commercial methods. The y axes represent the number of organisms, and the x axes represent the number of dilutions of difference between the reference method and the comparator methods. Positive differences indicate that the reference method established a lower MIC than the comparator. Shaded areas represent acceptable levels of disagreement (±1 dilution). The percentages of isolates falling within the acceptable range (percent essential agreement) are noted in the upper left corners of the shaded areas.
DISCUSSION
The selection of appropriate antimicrobial therapy for serious bacterial infections is predicated on accurate and timely in vitro antimicrobial susceptibility testing performed in the clinical microbiology laboratory. Daptomycin is increasingly being used to treat S. aureus and enterococcal infections, especially when other antibiotic choices are limited due to resistance to other classes of antibiotics. In the case of VRE infection, daptomycin often represents one of the few therapeutic options available for patients with life-threatening infections. The miscategorization of enterococcal isolates, especially VRE isolates, as NS to daptomycin when they are in fact S may impede timely implementation of effective antibiotic therapy and lead to poor outcomes for some patients.
The effects of media formulations and especially calcium concentrations on the accurate determination of in vitro susceptibility of Gram-positive organisms to daptomycin have been recognized for several decades (15). Consequently, CLSI protocols specify supplementation of CA-MHB with calcium to a final concentration of 50 mg/liter for BMD susceptibility testing (14). However, very few clinical microbiology laboratories perform BMD testing at all and even fewer do so routinely. Instead, most laboratories rely on MIC determinations performed by Etest or automated methods. Etest is typically performed on MHA plates, which may have variable calcium concentrations depending on lot and/or manufacturer (16). Likewise, automated methods may not consistently contain optimal calcium concentrations for daptomycin susceptibility testing and/or may contain other matrix components that could lead to inaccurate daptomycin susceptibility results. Such variability between methods has been demonstrated by numerous investigators (9, 10, 16).
Our study design differs from those of previously reported investigations of false daptomycin NS categorization for enterococci and S. aureus in that we selected isolates from patients with bloodstream infection irrespective of the daptomycin susceptibility determined at the time of isolation. Thus, our analysis is not biased toward isolates that may demonstrate daptomycin MICs close to the S/NS breakpoint and allows us to evaluate the daptomycin MIC distributions for enterococci and S. aureus isolated in our institution. When isolates were tested using the reference broth dilution method as specified by CLSI (50 mg/liter Ca2+ supplementation), very few daptomycin NS isolates were observed, consistent with nationwide and worldwide trends observed previously (17–18). However, when Ca2+ supplementation of CA-MHB in broth microdilution tests was suboptimal (30 mg/liter Ca2+), a significant number of E. faecium isolates with daptomycin MICs that would be interpreted as NS were observed. This is a direct consequence of the fact that a large number of the E. faecium isolates included in our study demonstrated reference BMD MICs that were 4 μg/ml, which is the enterococcal interpretive cutoff for daptomycin. A small change in calcium concentration in the BMD method led to MICs that were just one dilution higher for many isolates but resulted in a significant number of isolates miscategorized as NS. These observations clearly illustrate the care that must be taken to ensure that accurate Ca2+ supplementation is achieved when performing BMD for daptomycin in the clinical laboratory. This is sometimes difficult, however, since preparations of MHB and CA-MHB may vary considerably in Ca2+ concentrations, requiring manufacturer-specific and even lot-specific changes in the amounts of supplementation required to achieve the target final Ca2+ concentrations. In some cases, empirical determination of Ca2+ concentrations using specific reagents may be the only way to ensure accurate final Ca2+ concentrations and thus accurate daptomycin MICs. Obviously, the analytical measurement of calcium in supplemented media is beyond the capacity of most clinical microbiology laboratories, so arrangements with a reference laboratory must be sought. It is also important to note that suboptimal Ca2+ supplementation (at least at levels of ≥30 mg/liter) are not reliably revealed by testing the recommended E. faecalis control strain since, in our study, daptomycin MICs determined for the control strain using BMD with 30 mg/liter Ca2+ supplementation were, with one exception, within the acceptable range specified by CLSI (14).
To our knowledge, our study is the first to compare daptomycin susceptibility testing using Etest and two MicroScan methods to the reference BMD method using randomly selected enterococcal and S. aureus isolates. The results are consistent, however, with those of other studies that have used isolates selected based on daptomycin NS determinations (9–10). Palavecino and Burnell demonstrated that only 11.6% of E. faecium isolates were judged to be daptomycin NS using MicroScan confirmed by Etest (10). Similarly, Bryant et al. showed that of 150 enterococcal isolates judged to be daptomycin NS by MicroScan, only 30 (20%) were confirmed NS by BMD. Using Etest, 45 (30%) of these isolates had MICs of >4 μg/ml (9). Comparatively, in our study of 51 E. faecium isolates, 18, 22, and 25 were judged to be daptomycin NS by Etest, MicroScan Prompt, and MicroScan turbidity, respectively, whereas only 2 were confirmed NS by reference BMD (11%, 9%, and 8%). The lower rate of NS confirmation (and this higher rate of NS miscategorization by commercial methods) may reflect variability in the commercial reagents, especially with regard to calcium content. Unlike Bryant et al., we did not observe the failure of any of the commercial methods to detect NS enterococci or S. aureus (no very major errors).
As also reported by Bryant et al., all of the E. faecium isolates and the single E. faecalis isolate miscategorized as daptomycin NS using the commercial methods had daptomycin MICs of 4 μg/ml as judged by the reference BM method (9). Since a large number of E. faecium isolates exhibited MICs of 4 μg/ml while E. faecalis isolates tended to have lower MICs, it is not surprising that CA for E. faecalis was better than for E. faecium. Interestingly, however, it appears that the fact that the daptomycin population MIC values approach the breakpoint for susceptibility for E. faecium does not completely explain our findings. The bias toward higher MIC determinations using all three commercial methods was greater for E. faecium than E. faecalis. This suggests that whatever influences the method-dependent variability in daptomycin susceptibility testing does not equally impact all species tested. This conclusion is further supported by the fact that the essential agreement between all three commercial methods with reference BMD was 100% for S. aureus.
In summary, we have confirmed the previously reported overestimation of daptomycin NS E. faecium using MicroScan and Etest methods with an unbiased panel of clinical isolates. Additionally, we have systematically studied a large number of E. faecalis and S. aureus isolates and confirmed that this phenomenon is primarily limited to E. faecium isolates. Clearly, daptomycin NS results obtained using the MicroScan should be confirmed. However, the best method for confirmation is unequivocally BMD, which most laboratories do not routinely perform. Furthermore, given the technical complexities associated with Ca2+ supplementation of media used in BMD for daptomycin, many laboratories might find it difficult to employ such testing, especially on a sporadic basis. If laboratories do choose to implement BMD for confirmation of daptomycin NS organisms, calcium supplementation must be very carefully controlled, as suboptimal levels will have significant impacts on MIC determinations and lead to further miscategorization. In the absence of the ability to refer isolates judged to be daptomycin NS by MicroScan for BMD testing or perform it in-house, retesting using the same method or a different inoculation technique is not useful, but Etest may offer a slight increase in accuracy.
ACKNOWLEDGMENTS
This work was supported by an investigator-initiated study grant from Cubist Pharmaceuticals.
We thank Giovanni Divinagracia for expert technical assistance.
Footnotes
Published ahead of print 19 March 2014
REFERENCES
- 1.Eliopoulos GM, Willey S, Reiszner E, Spitzer PG, Caputo G, Moellering RC., Jr 1986. In vitro and in vivo activity of LY 146032, a new cyclic lipopeptide antibiotic. Antimicrob. Agents Chemother. 30:532–535. 10.1128/AAC.30.4.532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sader HS, Moet GJ, Farrell DJ, Jones RN. 2011. Antimicrobial susceptibility of daptomycin and comparator agents tested against methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci: trend analysis of a 6-year period in US medical centers (2005–2010). Diagn. Microbiol. Infect. Dis. 70:412–416. 10.1016/j.diagmicrobio.2011.02.008 [DOI] [PubMed] [Google Scholar]
- 3.Arias CA, Panesso D, McGrath DM, Qin X, Mojica MF, Miller C, Diaz L, Tran TT, Rincon S, Barbu EM, Reyes J, Roh JH, Lobos E, Sodergren E, Pasqualini R, Arap W, Quinn JP, Shamoo Y, Murray BE, Weinstock GM. 2011. Genetic basis for in vivo daptomycin resistance in enterococci. N. Engl. J. Med. 365:892–900. 10.1056/NEJMoa1011138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davlieva M, Zhang W, Arias CA, Shamoo Y. 2013. Biochemical characterization of cardiolipin synthase mutations associated with daptomycin resistance in enterococci. Antimicrob. Agents Chemother. 57:289–296. 10.1128/AAC.01743-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelesidis T. 2013. Transport of daptomycin resistance genes between animals and humans as a possible mechanism for development of de novo daptomycin resistance in enterococci. Epidemiol. Infect. 141:2185–2186. 10.1017/S0950268812002865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mishra NN, Bayer AS, Tran TT, Shamoo Y, Mileykovskaya E, Dowhan W, Guan Z, Arias CA. 2012. Daptomycin resistance in enterococci is associated with distinct alterations of cell membrane phospholipid content. PLoS One 7:e43958. 10.1371/journal.pone.0043958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Palmer KL, Daniel A, Hardy C, Silverman J, Gilmore MS. 2011. Genetic basis for daptomycin resistance in enterococci. Antimicrob. Agents Chemother. 55:3345–3356. 10.1128/AAC.00207-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gomez-Garces JL, Lopez-Fabal F, Burillo A, Gil Y. 2010. Comparative study of the susceptibility to daptomycin and other antimicrobials against Staphylococcus spp. resistant to methicillin and Enterococcus spp. using Wider, E-test, and microdilution methods. Rev. Esp Quimioter 23:87–92 (In Spanish.) [PubMed] [Google Scholar]
- 9.Bryant KA, Roberts AL, Rupp ME, Anderson JR, Lyden ER, Fey PD, Van Schooneveld TC. 2013. Susceptibility of enterococci to daptomycin is dependent upon testing methodology. Diagn. Microbiol. Infect. Dis. 76:497–501. 10.1016/j.diagmicrobio.2013.04.019 [DOI] [PubMed] [Google Scholar]
- 10.Palavecino EL, Burnell JM. 2013. False daptomycin-nonsusceptible MIC results by Microscan panel PC 29 relative to Etest results for Staphylococcus aureus and enterococci. J. Clin. Microbiol. 51:281–283. 10.1128/JCM.01721-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fuchs PC, Barry AL, Brown SD. 2000. Daptomycin susceptibility tests: interpretive criteria, quality control, and effect of calcium on in vitro tests. Diagn. Microbiol. Infect. Dis. 38:51–58. 10.1016/S0732-8893(00)00164-4 [DOI] [PubMed] [Google Scholar]
- 12.Fuchs PC, Barry AL, Brown SD. 2001. Evaluation of daptomycin susceptibility testing by Etest and the effect of different batches of media. J. Antimicrob. Chemother. 48:557–561. 10.1093/jac/48.4.557 [DOI] [PubMed] [Google Scholar]
- 13.Clinical and Laboratory Standards Institute. 2012. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically: approved standard, 7th ed. CLSI document M7–A7. Clinical and Laboratory Standards Institute, Wayne, PA [Google Scholar]
- 14.Clinical and Laboratory Standards Institute. 2013. Performance standards for antimicrobial susceptibility testing; 23rd informational supplement. CLSI M100–S23. Clinical and Laboratory Standards Institute, Wayne, Pa [Google Scholar]
- 15.Andrew JH, Wale MC, Wale LJ, Greenwood D. 1987. The effect of cultural conditions on the activity of LY146032 against staphylococci and streptococci. J. Antimicrob. Chemother. 20:213–221. 10.1093/jac/20.2.213 [DOI] [PubMed] [Google Scholar]
- 16.Nakashima H, Takahashi H, Kameko M, Saito H. 2012. Daptomycin Etest MICs for methicillin-resistant Staphylococcus aureus vary among different media. J. Infect. Chemother. 18:970–972. 10.1007/s10156-012-0424-5 [DOI] [PubMed] [Google Scholar]
- 17.Castanheira M, Jones RN, Sader HS. 2008. Update of the in vitro activity of daptomycin tested against 6710 Gram-positive cocci isolated in North America (2006). Diagn. Microbiol. Infect. Dis. 61:235–239. 10.1016/j.diagmicrobio.2008.01.016 [DOI] [PubMed] [Google Scholar]
- 18.Sader HS, Farrell DJ, Jones RN. 2011. Antimicrobial activity of daptomycin tested against gram-positive strains collected in European hospitals: results from 7 years of resistance surveillance (2003-2009). J. Chemother. 23:200–206. 10.1179/joc.2011.23.4.200 [DOI] [PubMed] [Google Scholar]