Abstract
Tetracyclines are administered to cure Japanese spotted fever (JSF) and tsutsugamushi disease (TD). It is generally said that the clinical course of JSF is worse than that of TD despite antibiotic treatment. The precise mechanism underlying the more severe clinical course of JSF is not fully understood. We therefore examined whether the differential cytokine profile between these two infectious diseases contributes to the difference in clinical severity. The serum concentrations of various cytokines (tumor necrosis factor alpha [TNF-α], interleukin-6 [IL-6], and gamma interferon [IFN-γ]) and chemokines (IL-8, interferon-inducible protein 10 [IP-10], monocyte chemoattractant protein 1 [MCP-1], macrophage inflammatory protein 1α [MIP-1α], MIP-1β, and eotaxin) were measured in 32 TD and 21 JSF patients. The results showed that serum levels of TNF-α in the acute phases of TD and JSF were significantly increased, with a higher concentration of TNF-α in patients with JSF (mean, 39.9 pg/ml) than in those with TD (mean, 13.8 pg/ml). Comparatively higher levels of other cytokines and chemokines (IL-6, IFN-γ, IL-8, IP-10, MCP-1, MIP-1α, and MIP-1β) were also observed in the acute phase of JSF. The clinical severity score (3.67 ± 1.71) of JSF patients was higher than that of TD patients (1.47 ± 0.77). Our findings revealed that the cytokine and chemokine levels in the acute phase of JSF were significantly higher than those in the acute phase of TD. The differential cytokine levels may be related to the difference in clinical severity between JSF and TD.
INTRODUCTION
Scrub typhus, also known as tsutsugamushi disease (TD), is a mite-borne infection caused by Orientia tsutsugamushi that occurs frequently in Southeast Asia. The vector of this disease is the trombiculid mite, also known as tsutsugamushi, which resides in mountainous areas and around rivers throughout Southeast Asia. In Japan, the number of cases of TD is approaching 500 per year (1, 2). TD is characterized by fever, rash, and eschar (3). Both minocycline and doxycycline are effective for treating TD and eradicating O. tsutsugamushi, and marked defervescence is observed in the majority of patients within 24 h after commencement of tetracyclines (4, 5).
Japanese spotted fever (JSF), caused by Rickettsia japonica, was first reported in Japan in 1984 (6–9). Areas where JSF is endemic are located along the southwestern and central coastal areas of Japan, which have a warmer climate (9). The clinical manifestations (high fever, rash, and tick bite eschar) of JSF are similar to those of TD (3, 10). Tetracyclines are recommended for clinically suspected cases of JSF (5), and complications like pneumonia, meningitis, disseminated intravascular coagulation, and systemic inflammatory response syndrome (SIRS) leading to multiple organ failure may result if tetracyclines are not administered early (11, 12).
It is generally said that the clinical course of JSF is worse than that of TD despite antibiotic treatment. The mortality rate of TD was reported to be 7% in untreated classical cases, while the mortality rate of Rocky Mountain spotted fever in the preantibiotic era was 20% to 25%, and the recent mortality rate, due to delay in diagnosis and therapy, was reported to be 5% (13). Compared with these mortality rates, it is important to recognize that the mortality rate of JSF may be similar to that in patients with Rocky Mountain spotted fever, which is the most lethal rickettsiosis. The precise mechanism underlying the more severe clinical course of JSF is not fully understood, and in the future, a larger number of patients should be investigated. It has been hypothesized that fatal JSF is associated with hypercytokinemia (14); however, no studies that elaborate cytokine levels in the acute phase of JSF exist.
In the present study, we measured the concentrations of several cytokines and chemokines in patients with TD and JSF before and after the administration of minocycline and compared the levels in the acute phases of JSF and TD. We believe our study is of great interest to physicians involved in the treatment of patients with rickettsial infection.
MATERIALS AND METHODS
Patient characteristics and diagnosis.
This prospective study was approved by the Institutional Review Board of the Faculty of Medical Science of the University of Fukui. Serum cytokine and chemokine levels were examined in 53 Japanese patients (25 males and 28 females; age range, 13 to 86 years) with confirmed rickettsial disease, which included 32 patients with confirmed O. tsutsugamushi infection diagnosed between 2003 and 2009 in Tanabe City, Wakayama Prefecture, Japan, and 21 patients with confirmed R. japonica infection diagnosed between 2007 and 2008 in the mountainous region of Misen, Shimane Prefecture, Japan. Detailed history taking and a physical examination for rash and eschar were performed in all patients (Table 1). The diagnosis of rickettsiosis was based on a rise in serum IgM antibody titer or a 4-fold rise in serum IgG antibody titer to strains of O. tsutsugamushi or R. japonica using an indirect immunoperoxidase antibody test performed on paired serum samples collected during the acute (1 to 7 days after disease onset) and convalescent phases (14 to 21 days after onset). Its sensitivity was 99.1% and specificity was 98.9% for reactivity to IgM and IgG (15, 16).
TABLE 1.
Clinical characterization of TD and JSFa
| Criterion | No. (%) of patients with: |
|
|---|---|---|
| TD (n = 32) | JSF (n = 21) | |
| Eschar | 28 (87.5) | 20 (95.2) |
| Skin rash | 30 (93.8) | 21 (100) |
| Fever (>38°C) | 21 (65.6) | 21 (100) |
| Lymph node swelling | 7 (21.9) | 7 (33.3) |
| Thrombocytopenia (PLT < 50,000/mm3) | 13 (40.6) | 4 (19.0) |
| Liver dysfunction (ALT > 40 IU/liter) | 18 (56.3) | 21 (100) |
| Disseminated intravascular coagulation | 2 (6.3) | 4 (19.0) |
| Central nervous system disorder | 1 (3.1) | 3 (14.3) |
The revised clinical severity scores (mean ± standard deviation) were 1.47 ± 0.77 for TD patients and 3.67 ± 1.71 for JSF patients. ALT, alanine aminotransferase; PLT, platelet.
Modified clinical severity scoring of rickettsial infections.
We used the clinical severity scoring system which was presented by Kern et al. for Mediterranean spotted fever, with minor modifications to adjust it to tsutsugamushi disease (17). Disease severity was evaluated using a modified scoring system based on the clinical scoring system reported by Iwasaki et al. (18). In brief, the score was calculated as the sum of different point values assigned to specific criteria: points were assigned to the clinical manifestations of fever (1 or 2 points), severe myalgia (1 point), lymphadenopathy (1 point), hepatosplenomegaly (1 point), liver dysfunction (1 point), thrombocytopenia (1 or 2 points), disseminated intravascular coagulation (2 points), and central nervous system disorder (3 points) (Table 2). These scores, with total possible points ranging from 0 to 15, were determined on the basis of laboratory data and major symptoms on admission.
TABLE 2.
Revised clinical severity scoring system
| Criteriona | Score |
|---|---|
| Fever of: | |
| >38°C | 1 |
| >39°C | 2 |
| Severe myalgia | 1 |
| Lymph node swelling | 1 |
| Hepatosplenomegaly | 1 |
| Liver dysfunction (ALT > 40 IU/liter) | 1 |
| Thrombocytopenia with PLT counts of: | |
| <100 × 109/liter | 1 |
| <50 × 109/liter | 2 |
| Disseminated intravascular coagulation | 2 |
| Central nervous system disorder | 3 |
ALT, alanine aminotransferase; PLT, platelet.
Cytokines and chemokines in patients with TD and JSF.
Sera taken from patients with TD and JSF were collected at the first clinic visit (acute phase) and 2 weeks after initiation of minocycline therapy (convalescent phase) and were frozen within 8 h of receipt and stored at −80°C until analysis. In our experience, the freezing of sera does not affect the results on retesting (19). All serum cytokine and chemokine levels were measured simultaneously using multiplex bead immunoassays. Multiplex bead immunoassays (Bio-Plex suspension array system; Bio-Rad Laboratories, Inc., CA, USA) were used to quantify cytokines and chemokines simultaneously by following the manufacturer's instructions (20). This novel immunoassay uses color-coded beads and permits the simultaneous detection of up to 100 cytokines and chemokines in a single well of a 96-well microplate in just 3 h (21–23). The serum levels of the following cytokines and chemokines were assessed: tumor necrosis factor alpha (TNF-α), interleukin-6 (IL-6), gamma interferon (IFN-γ), IL-8, interferon-inducible protein 10 (IP-10), monocyte chemoattractant protein 1 (MCP-1), macrophage inflammatory protein 1α (MIP-1α), MIP-1β, and eotaxin. The concentrations of each cytokine and chemokine in the acute and convalescent phases are reported.
Statistical analysis.
All data are presented as the mean ± standard deviation (SD). Student's t test was performed to analyze differences in the data using statistical software (Microsoft Excel 2010; Microsoft Corporation, Redmond, WA, USA). A P value of <0.05 was considered statistically significant.
RESULTS
Clinical features of TD and JSF.
All clinically suspected cases of rickettsial infection underwent indirect immunoperoxidase antibody testing performed on paired serum samples collected during the acute and convalescent phases. The IgM antibody titers were more than 1:640 during the acute phase in each case, and IgG antibody titers also increased more than 1:640 in the convalescent phase (data not shown). The following strains of O. tsutsugamushi were identified: Gilliam (n = 0), Karp (n = 2), Kato (n = 0), Irie/Kawasaki (n = 24), Hirano/Kuroki (n = 6), and Shimokoshi (n = 0). Patient demographics and clinical and laboratory data are summarized in Table 1. O. tsutsugamushi and R. japonica differ in their antigenic determinants, and accordingly, there was no overlap of the serologic assays for TD and JSF. The peak temperatures of fever in patients with JSF were higher than those in patients with TD (39.2 ± 0.7°C versus 38.1 ± 0.7°C) (Fig. 1A). Moreover, patients with JSF had a higher clinical severity score (3.67 ± 1.71) than patients with TD (1.47 ± 0.77) (Fig. 1B). Patients were given 100 to 200 mg/day minocycline intravenously or per os for 3 to 10 days, and all responded well to treatment.
FIG 1.
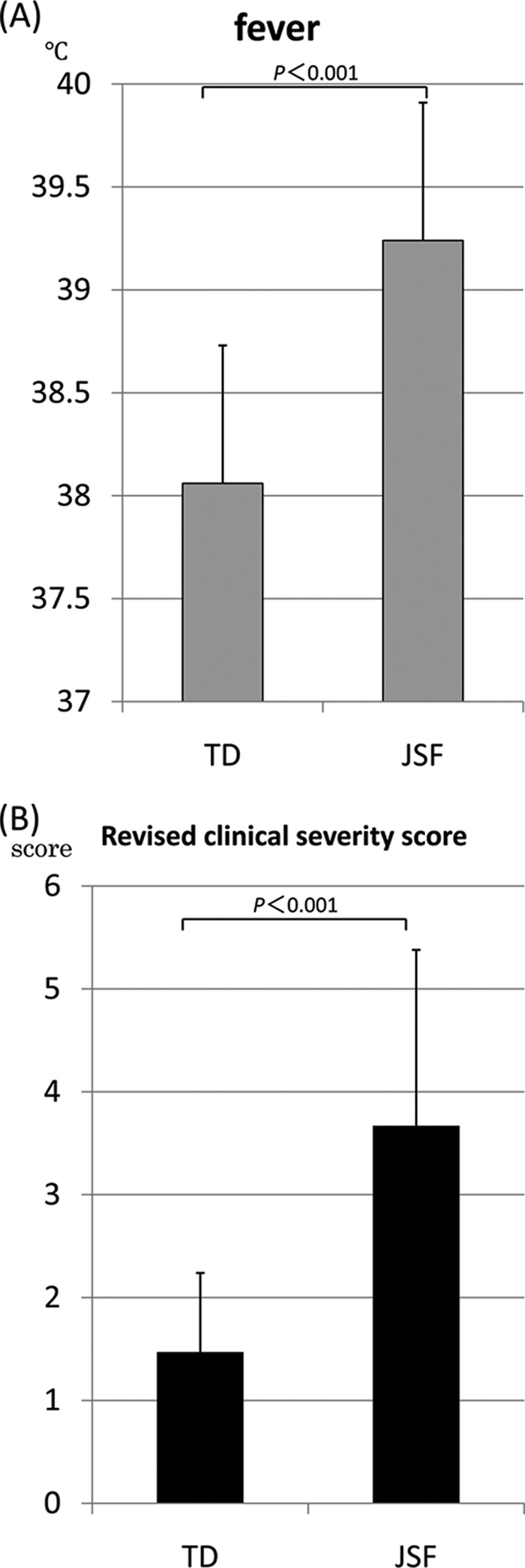
Comparison of the peak temperatures (A) and clinical severity scores (B) of patients with tsutsugamushi disease (TD) and Japanese spotted fever (JSF).
Serum cytokine and chemokine levels during minocycline treatment of TD and JSF.
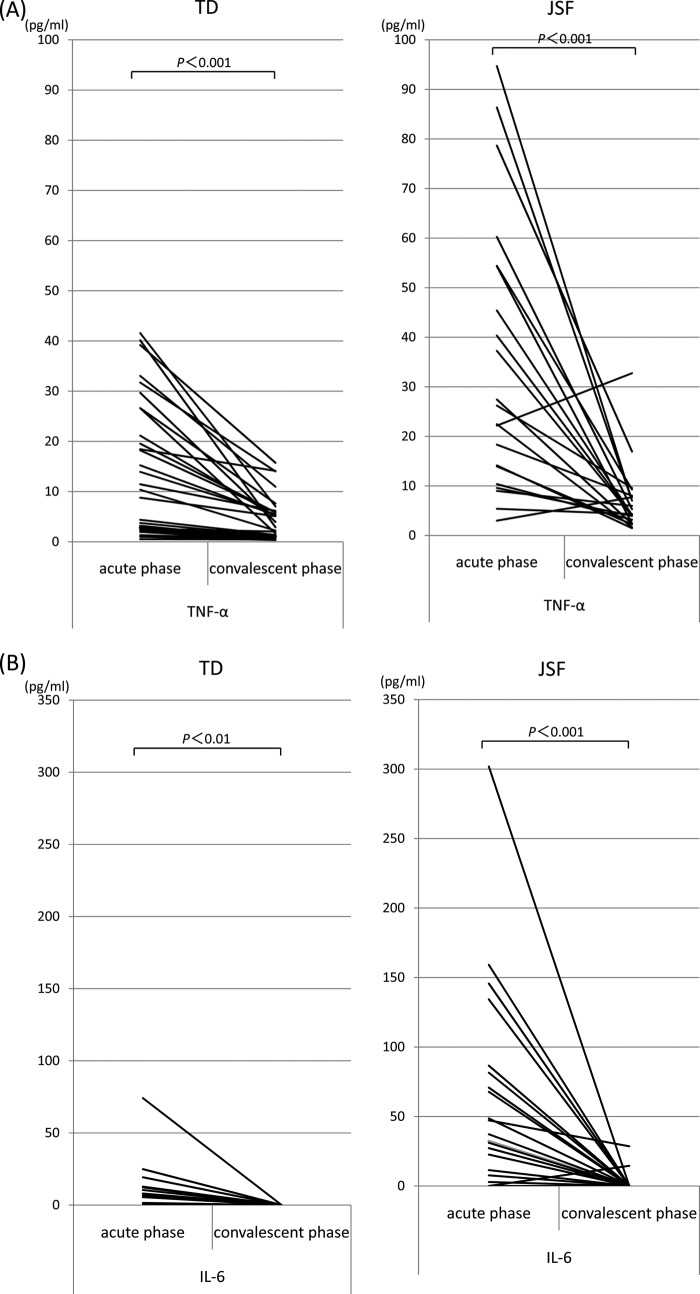
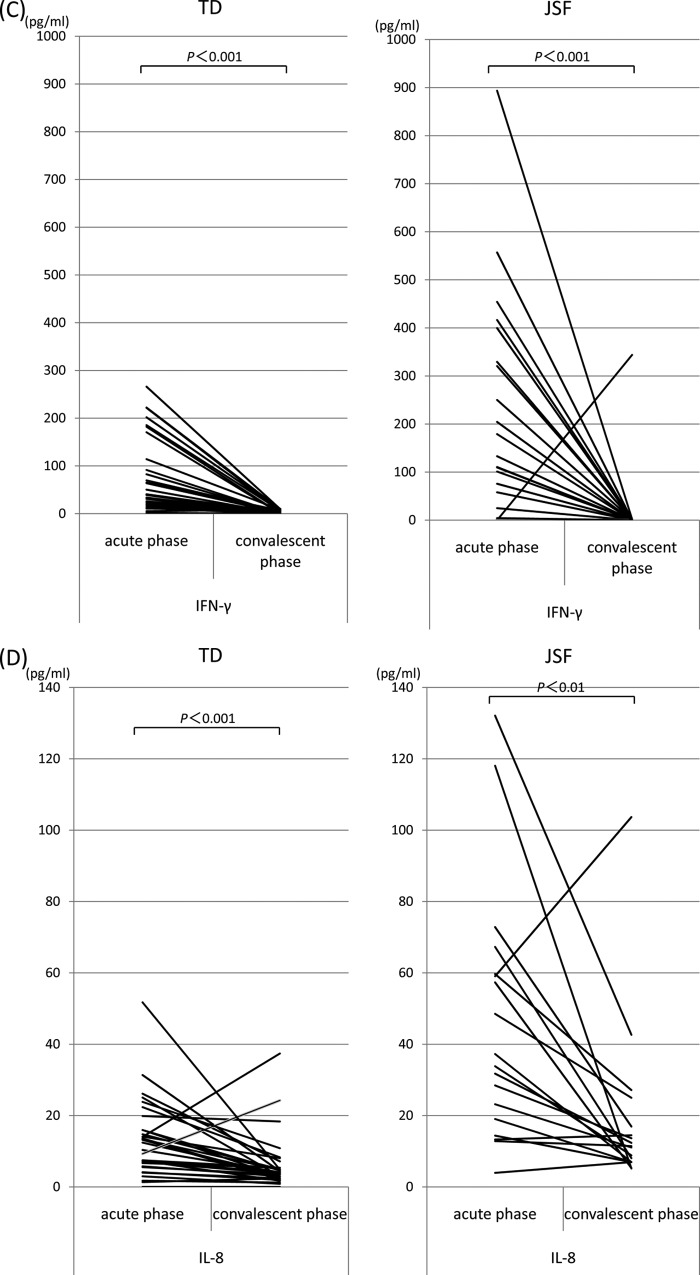
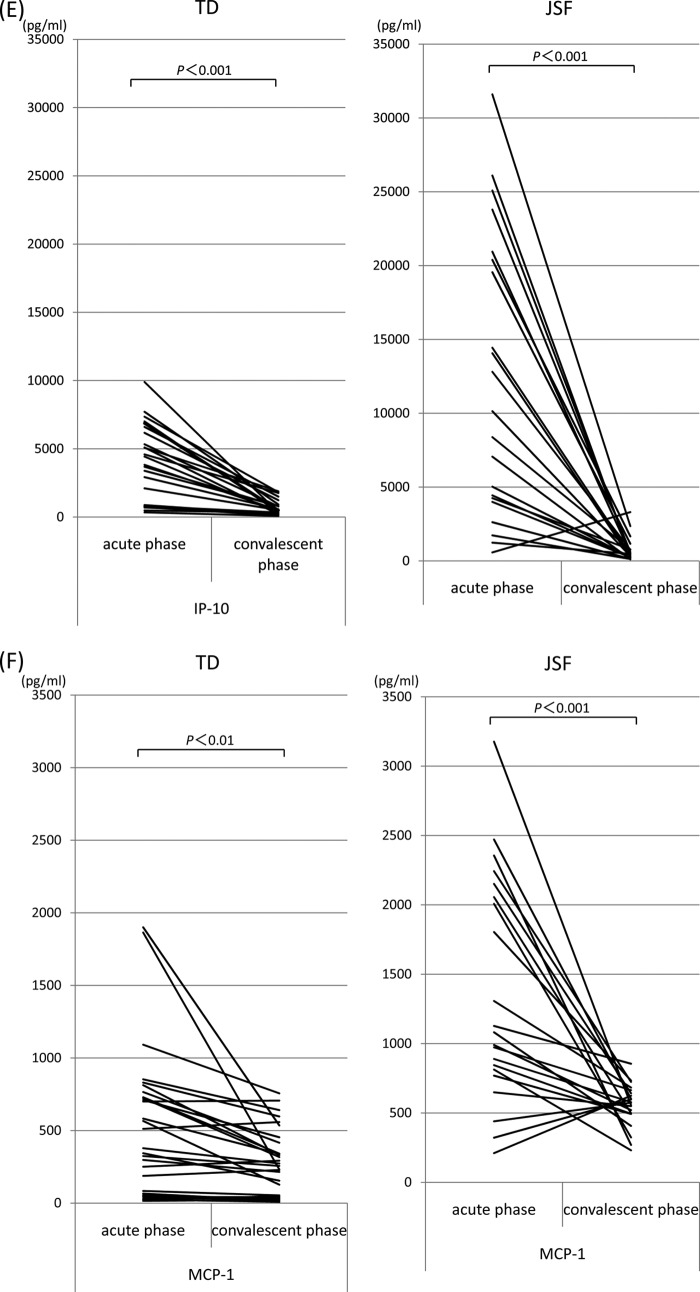
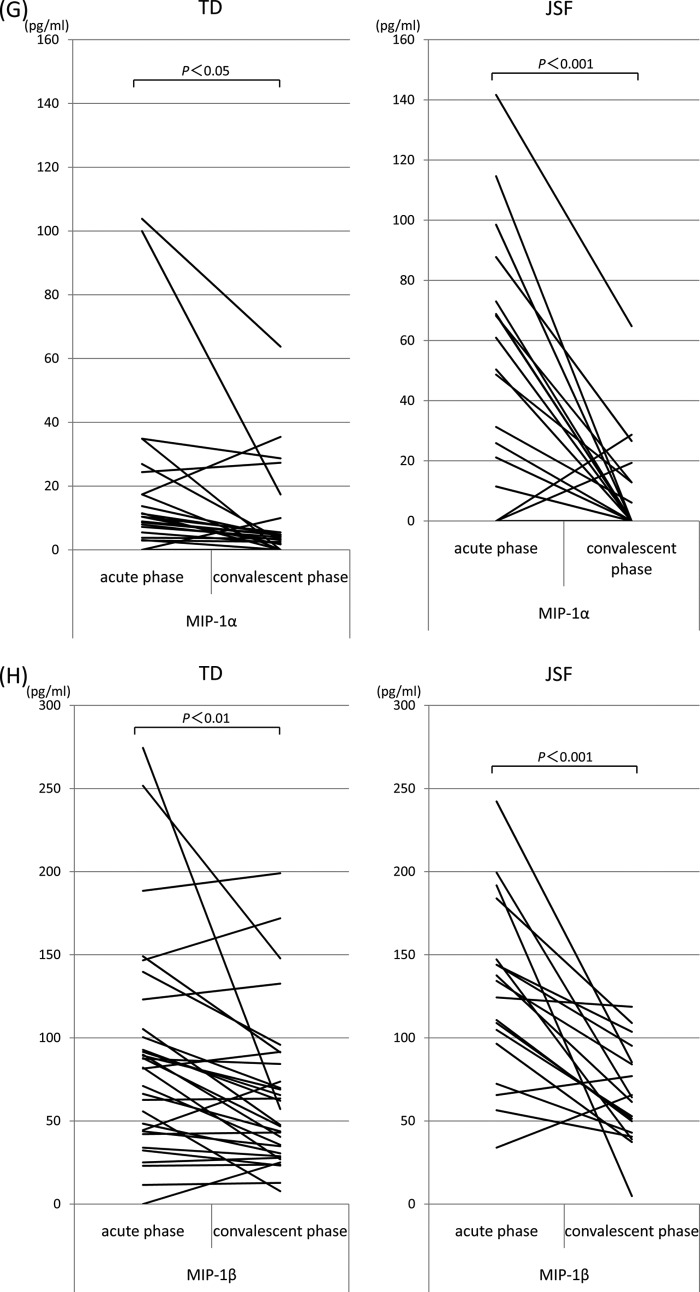
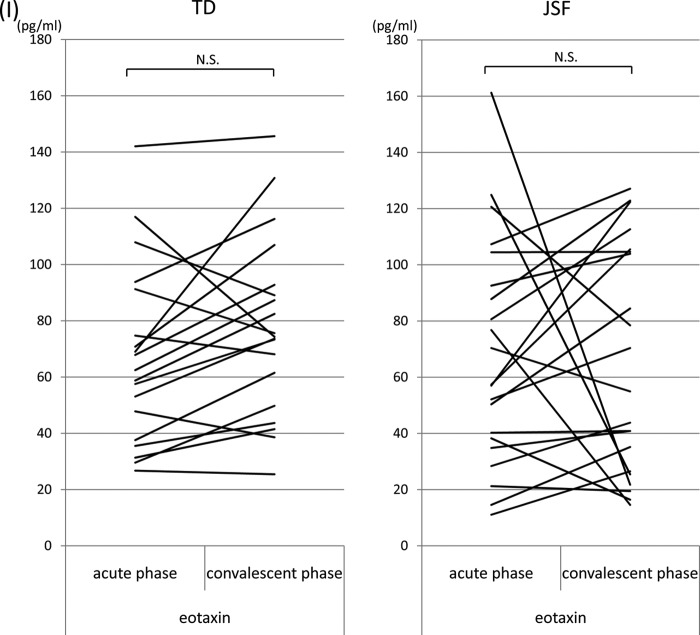
The serum levels of TNF-α, IL-6, IFN-γ, IL-8, IP-10, MCP-1, MIP-1α, and MIP-1β were elevated in almost all patients during the acute phase of rickettsial disease (Fig. 2A to I). Compared with the acute phase, the serum concentrations of these cytokines and chemokines were significantly decreased in the convalescent phase. In contrast, eotaxin levels were unchanged in the acute and convalescent phases. We next examined whether serum levels of cytokines and chemokines were significantly different between TD and JSF in the acute phase. The mean concentrations of cytokines and chemokines in patients infected with O. tsutsugamushi or R. japonica are shown in Table 3. The serum concentrations of TNF-α in patients with JSF (35.0 pg/ml) were significantly higher than those in patients with TD (13.8 pg/ml). Similarly, the serum levels of cytokines IL-6 (65.8 pg/ml versus 11.6 pg/ml) and IFN-γ (220.3 pg/ml versus 73.4 pg/ml) and chemokines IL-8 (46.3 pg/ml versus 13.2 pg/ml), IP-10 (12,298.3 pg/ml versus 3,215.9 pg/ml), MCP-1 (1,365.8 pg/ml versus 467.5 pg/ml), MIP-1α (53.9 pg/ml versus 15.0 pg/ml), and MIP-1β (127.7 pg/ml versus 88.5 pg/ml) in JSF patients were significantly higher than those in TD patients. However, there was no significant difference in the concentration of eotaxin between the acute phases of TD and JSF (67.1 pg/ml versus 68.2 pg/ml). On the other hand, in the convalescent phase, the serum levels of TNF-α, IL-8, and MCP-1 in JSF patients were significantly higher than those in TD patients, and there were no significant differences in other cytokines and chemokines between TD and JSF patients (Table 3).
FIG 2.
Serum cytokine and chemokine levels during the acute and convalescent phases of TD and JSF. Serum cytokines TNF-α (A), IL-6 (B), and IFN-γ (C) and chemokines IL-8 (D), IP-10 (E), MCP-1 (F), MIP-1α (G), MIP-1β (H), and eotaxin (I) were measured using multiplex bead immunoassays. The concentrations of cytokines and chemokines in the acute and convalescent phases are shown. N.S., not significant.
TABLE 3.
Differences in cytokine and chemokine levels between TD and JSF patients
| Disease phase and cytokine or chemokinea | Avg level ± SD (pg/ml) in patients with: |
P valueb | |
|---|---|---|---|
| TD (n = 32) | JSF (n = 21) | ||
| Acute | |||
| TNF-α | 13.8 ± 13.5 | 35.0 ± 27.5 | <0.001 |
| IL-6 | 11.6 ± 17.2 | 65.8 ± 73.4 | <0.01 |
| IFN-γ | 73.4 ± 78.1 | 220.3 ± 228.0 | <0.001 |
| IL-8 | 13.2 ± 10.5 | 46.3 ± 35.3 | <0.001 |
| IP-10 | 3,215.9 ± 2,786.1 | 12,298.3 ± 9,539.4 | <0.001 |
| MCP-1 | 467.5 ± 492.0 | 1,365.8 ± 816.7 | <0.001 |
| MIP-1α | 15.0 ± 25.3 | 53.9 ± 41.0 | <0.001 |
| MIP-1β | 88.5 ± 63.5 | 127.7 ± 54.0 | <0.05 |
| Eotaxin | 67.1 ± 31.7 | 68.2 ± 40.1 | NS |
| Convalescent | |||
| TNF-α | 4.1 ± 4.4 | 6.8 ± 6.9 | <0.05 |
| IL-6 | 0 ± 0 | 2.2 ± 7.0 | NS |
| IFN-γ | 3.5 ± 3.7 | 16.7 ± 7.5 | NS |
| IL-8 | 6.1 ± 7.5 | 18.5 ± 23.3 | <0.01 |
| IP-10 | 550.8 ± 534.2 | 730.9 ± 805.2 | NS |
| MCP-1 | 253.9 ± 229.1 | 553.3 ± 153.3 | <0.001 |
| MIP-1α | 7.3 ± 13.9 | 9.5 ± 16.9 | NS |
| MIP-1β | 63.7 ± 46.2 | 65.7 ± 29.6 | NS |
| Eotaxin | 77.7 ± 31.8 | 65.3 ± 40.4 | NS |
Normal levels: TNF-α, <2.3 pg/ml; IL-6, <3.0 pg/ml; IFN-γ, <7.3 pg/ml; IL-8, <3.0 pg/ml; IP-10, MCP-1, MIP-1α and MIP-1β, normal levels not determined.
P values were determined by t test. NS, not significant.
Positive correlations exist between TNF-α and IL-8 (r = 0.876) (Fig. 3A) and between TNF-α and IP-10 (r = 0.704) (Fig. 3B) in the acute phase of JSF. In contrast, no significant correlation was observed between TNF-α and other cytokines and chemokines in the acute phase of TD.
FIG 3.
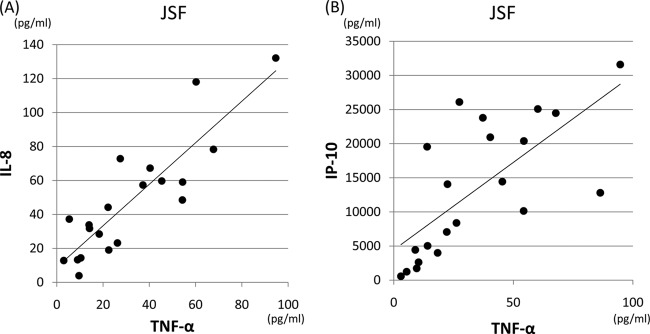
Relationships between TNF-α and IL-8 (A) (r = 0.876) and between TNF-α and IP-10 (r = 0.704) (B) in the acute phase of JSF.
DISCUSSION
In the present study, the levels of cytokines and chemokines were significantly higher in the acute phase of JSF than in the acute phase of TD. Consistent with this, a positive correlation between TNF-α and IL-8 (r = 0.876), as well as between TNF-α and IP-10 (r = 0.704), was observed in the acute phase of JSF. We speculate that the severity of JSF is related to hypercytokinemia. Systemic inflammatory reactions are regulated by a complicated cytokine network, and the production of proinflammatory cytokines and chemokines is essential in the immune response against pathogens. Regulation of cytokine and chemokine production is necessary for an appropriate host response; however, tissue damage may result from activation of immune cells due to the overproduction of cytokines and chemokines. The unregulated and excessive systemic release of numerous cytokines and chemokines in a life-threatening infection can cause systemic disorders and lead to fatal consequences like septic shock or SIRS (24, 25). We estimate that hypercytokinemia may contribute to the disease severity of rickettsiosis, including JSF. For instance, fulminant TD has been associated with hemophagocytic syndrome (10), and this syndrome may represent a hyperreaction of the immune system mediated by an overactivated cytokine network during the advanced stages of rickettsial infection (19, 26–28). We previously reported that a downregulation of these cytokines and chemokines is observed after the administration of tetracyclines, demonstrated a correlation between the severity of TD and the serum concentration of TNF-α in the acute phase of the disease, and showed that TNF-α levels are predictive of the severity of TD (18, 19, 29, 30). In relation to other spotted fever group infections, it is reported that Mediterranean spotted fever is characterized by a Th1 cytokine profile, and the patient's immune system responds with proinflammatory and immunoregulatory cytokine production (IL-1β, TNF-α, IL-6, IFN-γ, IL-8, IL-10, and IL-12) that accompanies the rickettsial vasculitis and contributes to the healing process (31). The cytokine profiles for JSF and MSF were not much different from each other. No cytokines were characteristic of JSF, in contrast with what was observed for other rickettsioses. It is generally said that the clinical course of JSF is worse than that of TD despite antibiotic treatment, and in cases of severe JSF with complications where monotherapy with either minocycline or doxycycline was not effective, such patients can be successfully treated using tetracyclines combined with quinolones (ciprofloxacin, levofloxacin, etc.) (32). However, in this study, although we examined correlations between the severity of JSF and some cytokine levels, we could not show any significant difference. It is unclear whether the severity of JSF is related to the serum concentrations of cytokines and chemokines in the acute phase of the disease. Although the precise mechanism underlying the disease severity of JSF is not well understood, our study provides insight into the possible contribution of cytokines and chemokines in the pathogenesis of this disease.
In conclusion, the present study showed that the serum cytokine and chemokine levels were significantly higher in JSF than in TD. We suspect that the differences in cytokine and chemokine levels contribute to the difference in disease severity between JSF and TD.
ACKNOWLEDGMENTS
This work was supported by grant H24-Shinkou-Ippan-008 to H.I. for research on emerging and reemerging infectious diseases from the Ministry of Health, Labor and Welfare of Japan and a Grant-in-Aid for Scientific Research (C) KAKENHI 24591478 from the Japan Society for the Promotion of Science.
We thank Seitaro Nasu of Nasu Clinic for provision of serum of rickettsia patients and the colleagues in our laboratory for excellent technical assistance and helpful discussions.
The authors declare no conflict of interest.
Footnotes
Published ahead of print 26 March 2014
REFERENCES
- 1.Iwasaki H, Yano T, Kaneko S, Egi M, Takada N, Ueda T. 2001. Epidemiological analysis on many cases of tsutsugamushi disease found in Hiroshima Prefecture, Japan. Kansenshogaku Zasshi 75:365–370 [DOI] [PubMed] [Google Scholar]
- 2.Tamura A, Ohashi N, Urakami H, Miyamura S. 1995. Classification of rickettsia-tsutsugamushi in a new genus, Orientia gen. nov., as Orientia tsutsugamushi comb. nov. Int. J. Syst. Bacteriol. 45:589–591. 10.1099/00207713-45-3-589 [DOI] [PubMed] [Google Scholar]
- 3.Iwasaki H, Ueda T, Uchida M, Nakamura T, Takada N, Mahara F. 1991. Atypical lymphocytes with a multilobated nucleus from a patient with tsutsugamushi disease (scrub typhus) in Japan. Am. J. Hematol. 36:150–151. 10.1002/ajh.2830360216 [DOI] [PubMed] [Google Scholar]
- 4.Miyamura S, Ohta T, Tamura A. 1989. Comparison of in vitro susceptibilities of Rickettsia prowazekii, R. rickettsii, R. sibirica and R. tsutsugamushi to antimicrobial agents. Nihon Saikingaku Zasshi 44:717–721. 10.3412/jsb.44.717 [DOI] [PubMed] [Google Scholar]
- 5.Suto T, Hatakeyama H, Ito R, Nakamura Y, Mahara F. 1989. In vitro susceptibility of a strain of Rickettsia recently isolated from a case of Japanese spotted fever to chemotherapeutic agents. Kansenshogaku Zasshi 63:35–38 [DOI] [PubMed] [Google Scholar]
- 6.Mahara F, Koga K, Sawada S, Taniguchi T, Shigemi F, Suto T, Tsuboi Y, Ooya A, Koyama H, Uchiyama T. 1985. The first report of the rickettsial infections of spotted fever group in Japan: three clinical cases. Kansenshogaku Zasshi 59:1165–1171 [DOI] [PubMed] [Google Scholar]
- 7.Uchida T, Mahara F, Tsuboi Y, Oya A. 1985. Spotted fever group rickettsiosis in Japan. Jpn. J. Med. Sci. Biol. 38:151–153. 10.7883/yoken1952.38.151 [DOI] [PubMed] [Google Scholar]
- 8.Mahara F. 1997. Japanese spotted fever: report of 31 cases and review of the literature. Emerg. Infect. Dis. 3:105–111. 10.3201/eid0302.970203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mahara F. 2006. Rickettsioses in Japan and the Far East. Ann. N. Y. Acad. Sci. 1078:60–73. 10.1196/annals.1374.007 [DOI] [PubMed] [Google Scholar]
- 10.Iwasaki H, Hashimoto K, Takada N, Nakayama T, Ueda T, Nakamura T. 1994. Fulminant Rickettsia tsutsugamushi infection associated with hemophagocytic syndrome. Lancet 343:1236. 10.1016/S0140-6736(94)92456-2 [DOI] [PubMed] [Google Scholar]
- 11.Bone RC, Sibbald WJ, Sprung CL. 1992. The ACCP-SCCM consensus conference on sepsis and organ failure. Chest 101:1481–1483. 10.1378/chest.101.6.1481 [DOI] [PubMed] [Google Scholar]
- 12.Cavaillon JM, Adib-Conquy M, Cloez-Tayarani I, Fitting C. 2001. Immunodepression in sepsis and SIRS assessed by ex vivo cytokine production is not a generalized phenomenon: a review. J. Endotox. Res. 7:85–93. 10.1177/09680519010070020201 [DOI] [PubMed] [Google Scholar]
- 13.Kuroda T, Suzuki S, Konno M, Amano T, Mikame M. 1991. A case of scrub typhus with disseminated intravascular coagulation, meningitis and pulmonary fibrosis. Nihon Naika Gakkai Zasshi 80:1816–1817. 10.2169/naika.80.1816 [DOI] [PubMed] [Google Scholar]
- 14.Iwasaki H, Mahara F, Takada N, Fujita H, Ueda T. 2001. Fulminant Japanese spotted fever associated with hypercytokinemia. J. Clin. Microbiol. 39:2341–2343. 10.1128/JCM.39.6.2341-2343.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim YJ, Yeo SJ, Park SJ, Woo YJ, Kim MW, Kim SH, Chang IA, Jeon SH, Park BJ, Song GJ, Lee MG, Kim IS, Kim YW. 2013. Improvement of the diagnostic sensitivity of scrub typhus using a mixture of recombinant antigens derived from orientia tsutsugamushi serotypes. J. Korean Med. Sci. 28:672–679. 10.3346/jkms.2013.28.5.672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watthanaworawit W, Turner P, Turner C, Tanganuchitcharnchai A, Richards AL, Bourzac KM, Blacksell SD, Nosten F. 2013. Short report: a prospective evaluation of real-time PCR assays for the detection of Orientia tsutsugamushi and Rickettsia spp. for early diagnosis of rickettsial infections during the acute phase of undifferentiated febrile illness. Am. J. Trop. Med. Hyg. 89:308–310. 10.4269/ajtmh.12-0600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kern WV, Oristrell J, SeguraPorta F, Kern P. 1996. Release of soluble tumor necrosis factor receptors in Mediterranean spotted fever rickettsiosis. Clin. Diagn. Lab. Immunol. 3:233–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iwasaki H, Mizoguchi J, Takada N, Tai K, Ikegaya S, Ueda T. 2010. Correlation between the concentrations of tumor necrosis factor-alpha and the severity of disease in patients infected with Orientia tsutsugamushi. Int. J. Infect. Dis. 14:E328–E333. 10.1016/j.ijid.2009.06.002 [DOI] [PubMed] [Google Scholar]
- 19.Iwasaki H, Takada N, Nakamura T, Ueda T. 1997. Increased levels of macrophage colony-stimulating factor, gamma interferon, and tumor necrosis factor alpha in sera of patients with Orientia tsutsugamushi infection. J. Clin. Microbiol. 35:3320–3322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salvatore CM, Techasaensiri C, Tagliabue C, Katz K, Leos N, Gomez AM, McCracken GH, Hardy RD. 2009. Tigecycline therapy significantly reduces the concentrations of inflammatory pulmonary cytokines and chemokines in a murine model of mycoplasma pneumoniae pneumonia. antimicrob. Agents Chemother. 53:1546–1551. 10.1128/AAC.00979-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim HO, Kim HS, Youn JC, Shin EC, Park S. 2011. Serum cytokine profiles in healthy young and elderly population assessed using multiplexed bead-based immunoassays. J. Transl. Med. 9:113. 10.1186/1479-5876-9-113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wagner B, Freer H. 2009. Development of a bead-based multiplex assay for simultaneous quantification of cytokines in horses. Vet. Immunol. Immunopathol. 127:242–248. 10.1016/j.vetimm.2008.10.313 [DOI] [PubMed] [Google Scholar]
- 23.Reis S, Sampaio ALF, Henriques MDM, Gandini M, Azeredo EL, Kubelka CF. 2007. An in vitro model for dengue virus infection that exhibits human monocyte infection, multiple cytokine production and dexamethasone immunomodulation. Mem. Inst. Oswaldo Cruz 102:983–990. 10.1590/S0074-02762007000800014 [DOI] [PubMed] [Google Scholar]
- 24.Cohen J, Abraham E. 1999. Microbiologic findings and correlations with serum tumor necrosis factor-alpha in patients with severe sepsis and septic shock. J. Infect. Dis. 180:116–121. 10.1086/314839 [DOI] [PubMed] [Google Scholar]
- 25.Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ, ACCP/SCCM Consensus Conference Committee 1992. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101:1644–1655 [DOI] [PubMed] [Google Scholar]
- 26.Chung DR, Lee YS, Lee SS. 2008. Kinetics of inflammatory cytokines in patients with scrub typhus receiving doxycycline treatment. J. Infect. 56:44–50. 10.1016/j.jinf.2007.09.009 [DOI] [PubMed] [Google Scholar]
- 27.Kramme S, Van An L, Khoa ND, Van Trin L, Tannich E, Rybniker J, Fleischer B, Drosten C, Panning M. 2009. Orientia tsutsugamushi bacteremia and cytokine levels in Vietnamese scrub typhus patients. J. Clin. Microbiol. 47:586–589. 10.1128/JCM.00997-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kodama K, Senba T, Yamauchi H, Nomura T, Chikahira Y. 2003. Clinical study of Japanese spotted fever and its aggravating factors. J. Infect. Chemother. 9:83–87. 10.1007/s10156-002-0223-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tai K, Iwasaki H, Ikegaya S, Ueda T. 2013. Minocycline modulates cytokine and chemokine production in lipopolysaccharide-stimulated THP-1 monocytic cells by inhibiting I kappa B kinase alpha/beta phosphorylation. Transl. Res. 161:99–109. 10.1016/j.trsl.2012.10.001 [DOI] [PubMed] [Google Scholar]
- 30.Iwasaki H, Inoue H, Takada N, Mahara F, Ueda T. 2000. Cytokine modulation induced by minocycline in Tsutsugamushi disease. Kansenshogaku Zasshi 74:598–600 [DOI] [PubMed] [Google Scholar]
- 31.Popivanova NI, Murdjeva MA, Baltadzhiev IG, Haydushka IA. 2011. Dynamics in serum cytokine responses during acute and convalescent stages of Mediterranean spotted fever. Folia Med. (Plovdiv) 53:36–43. 10.2478/v10153-010-0035-9 [DOI] [PubMed] [Google Scholar]
- 32.Seki M, Ikari N, Yamamoto S, Yamagata Y, Kosai K, Yanagihara K, Kakugawa T, Kurihara S, Izumikawa K, Miyazaki Y, Higashiyama Y, Hirakata Y, Tashiro T, Kohno S. 2006. Severe Japanese spotted fever successfully treated with fluoroquinolone. Intern. Med. 45:1323–1326. 10.2169/internalmedicine.45.1831 [DOI] [PubMed] [Google Scholar]