Abstract
Background
Environmental influences on the rate of Alzheimer’s disease (AD) progression have received little attention. Our objective was to test hypotheses concerning associations between caregiver personality traits and the rate of AD progression.
Methods
Care receivers (CR) were 161 persons with AD from a population-based dementia progression study; 55 of their caregivers were spouses and 106 were adult children. Cognitive status of the CR was measured with the Mini-Mental State Examination every six months, over an average of 5.6 (range: 1–14) years. Linear mixed models tested rate of cognitive decline as a function of caregiver personality traits from the NEO Five-Factor Inventory.
Results
Significantly faster cognitive decline was observed with higher caregiver Neuroticism overall; however, in stratified models, effects were significant for adult child but not spouse caregivers. Neuroticism facets of depression, anxiety, and vulnerability to stress were significantly associated with faster decline. Higher caregiver Extraversion was associated with slower decline in the CR when caregivers were adult children but not spouses.
Conclusions
For adult child caregivers, caregiver personality traits are associated with rate of cognitive decline in CRs with AD regardless of co-residency. Results suggest that dementia caregiver interventions promoting positive care management strategies and ways to react to caregiving challenges may eventually become an important complement to pharmacologic and other approaches aimed at slower rate of decline in dementia.
Keywords: caregiver, personality, dementia, cognitive, decline
Introduction
Alzheimer’s disease (AD) remains a major public health problem, with a prevalence of 11–16 million cases projected by 2050 in the United States alone (Alzheimer’s Association, 2012). With no current cure, research has focused on better understanding, and potentially modifying, the rates of clinical progression. After onset of AD, the typical rate of cognitive decline in AD is about three points/year on the Mini-Mental State Examination (MMSE), a global cognitive assessment (Behl et al., 2005). Faster decline has been associated with higher education and younger onset age (Teri et al., 1995), with vascular risk factors and early neuropsychiatric and related baseline behavioral disturbances such as agitation or psychosis (Scarmeas et al., 2005).
In more recent years, the rate of clinical progression of AD has been linked with the “caregiving environment,” comprising caregiver’s (CG) characteristics as well as care management practices. Closer emotional relationships within the care dyad (Norton et al., 2009) and engagement of the care receiver (CR) in more cognitively stimulating activities (Treiber et al., 2011) are associated with slower cognitive decline in AD. CGs’ problem-focused coping style (Tschanz et al., 2013) is associated with slower decline in dementia, suggesting that the progression of AD may be modifiable. The current study evaluates whether CG’s personality characteristics (e.g. as measured by the “Big Five” model advanced by Costa and McCrae, 1992) are associated with differential rates of AD progression.
Dementia caregiving and caregiver’s personality: effects on the caregiver
Dementia caregiving is related to both negative and positive outcomes for CGs (Koerner et al., 2009), and personality is strongly associated with stress coping in CGs (Hooker et al., 1994). CG’s personality traits have been studied for their associations with CG health, in particular, higher levels of Neuroticism are associated with higher depression risk (Jang et al., 2004), higher objective and subjective CG burden (Melo et al., 2011), a lower response rate to CG interventions (Jang et al., 2004), and higher caregiver mortality risk, with a 63% greater risk of death over four years compared with non-CGs (Schulz and Beach, 1999). CG Extraversion and Agreeableness are associated with decreased CG burden, and CG Extraversion is also associated with attenuated CG depression (Melo et al., 2011). Koerner et al. (2009) similarly reported that CG Extraversion and Agreeableness were associated with CG benefits/gains. They observed that CGs high in these characteristics were more likely to value and feel more comfortable in their CG role.
Dementia caregiving and caregiver personality: effects on the care receiver
Less research has been conducted associating CG personality with CR outcomes. The transitive model for studying the effects of CG personality on the CR (Ruiz et al., 2006) posits that the characteristics of each individual member of a dyad influence the characteristics and experience of the other dyad member, where the CG may reciprocate similar emotions of CR and vice versa. For example, several studies of AD CGs found that CR depression was strongly associated with distress and depression in their CG (Teri et al., 1997). de Vugt et al. (2004) found a bi-directional pattern, where CG irritability or criticism was significantly associated with a higher level of hyperactive behavior in the CR.
Kitwood (1993, pp. 64–65) has suggested that dementia caregiving is a “cooperative and reciprocal engagement” that necessitates that CGs be emotionally available to their CR and display empathy, flexible thinking, imagination, and creativity. This approach supports the hypothesis that CG characteristics (such as personality traits) that promote acceptance of the validity of CR experiences, and stimulate conscientious identification of CR needs, are crucial to development of a positive care environment.
Caregivers high in Neuroticism reported CR impairments more negatively and responded to care with greater frustration (Bookwala and Schulz, 1998), perceived fewer supporters (Shurgot and Knight, 2005), and had less instrumental support from family and friends (Reis et al., 1994). Hooker et al. (1994) found that CGs high in Neuroticism and low in optimism used maladaptive coping strategies. Pot et al. (2001) reported that higher levels of Extraversion in non-spouse CGs increased the likelihood of institutionalization and speculated that this was because extraverted CGs may find it easier to discuss the difficulties inherent to dementia-related care with professionals.
The current study
While there is some evidence that CG personality traits may be associated with outcomes in the CR, the extent to which CG personality traits are related to the progression of AD in the CR remains unknown. Of the few such studies available, most were clinic-based (e.g. de Vugt et al., 2004) and in the remainder, observation time was only one to three years (e.g. Pot et al., 2001). The current study sought to examine this question in a population-based sample of care dyads observed for nearly six years, on average. Because the transitive model suggests that some personality traits might be protective for the other member of a dyad, we hypothesized that CRs in whom the CG was lower in Neuroticism, and higher in Extraversion and Agreeableness, would experience slower rates of cognitive decline.
Methods
Subjects
The Cache County Dementia Progression Study (DPS; Tschanz et al., 2011) derives its sample from the population-based longitudinal Cache County Memory Study (CCMS; Breitner et al., 1999), which is designed to evaluate genetic and environmental risk factors for dementia. Begun in 1995, the CCMS enrolled 90% of the 5,677 county residents aged 65 years or older in its first wave, with three subsequent triennial incidence waves also completed. Participants with incident dementia were followed prospectively in DPS, approximately semiannually, with visits 6–18 months apart. Of the 334 DPS participants, there were 240 who had AD and no other diagnosis. We removed 19 who were cared for by someone other than spouse or adult child (in-law). Of the remaining 221 participants, 161 had Neuroticism-Extroversion-Openness (NEO) data (73% completion rate).
Alzheimer’s disease diagnosis procedures
All DPS participants were identified from the multistage procedures of the CCMS, reported in Breitner et al. (1999). Briefly, screening began with an in-person interview that included the Modified MMSE. Participants who screened positive for possible dementia completed an in-depth clinical assessment, as did a 19% sub-sample of “designated controls.” Specially trained nurses and psychometric technicians administered the clinical assessment, which included a brief physical evaluation, a detailed history of medical and cognitive symptoms, a structured neurological examination, and a one-hour battery of neuropsychological tests.
A geriatric psychiatrist and neuropsychologist reviewed these data; participants with a working DSM-III-R diagnosis of dementia were selected for psychiatrist examinations and laboratory studies, including neuroimaging, and an 18-month follow-up clinical assessment. A consensus panel of experts in neurology, geriatric psychiatry, neuropsychology, and cognitive neuroscience reviewed all available data and assigned final consensus diagnoses. Onset age was defined as the age when the participant unambiguously met DSM-III-R criteria for dementia. AD was diagnosed according to the National Institute of Neurological Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association (NINCDS–ADRDA) criteria. Study procedures were approved by institutional review boards of Utah State, Duke, and the Johns Hopkins universities, with informed consent obtained at each visit prior to data collection.
Cognitive trajectory measurement
Cognitive status was measured at each DPS visit using the Consortium to Establish a Registry for Alzheimer’s Disease adaptation of MMSE (Morris et al., 1993). An adjusted MMSE score was calculated by discarding items missed due to sensory/motor impairment, calculating the correct percentage, rescaled to a 30-point scale. MMSE scores from all visits at which the NEO respondent was reported as being the key CR were included. When the CR changed (e.g. spouse dies, adult child is new CR), all subsequent MMSE scores corresponding to the period with the new CR were dropped from analysis.
Caregiver personality measurement
The NEO Personality Inventory – Revised (NEO-PIR) was collected from 158 CGs through mail-in questionnaire. Another 83 CGs completed the NEO Five Factor Inventory (NEO-FFI) by telephone, resulting in 241 completed personality inventories. On average, time from dementia onset to collection of the NEO was 5.6 years. We assume relative stability of caregiver personality traits over the full observation period of cognitive status in the CR.
The NEO-PIR is a 240-item personality instrument consisting of 48 items in each of the five domains, corresponding to Neuroticism, Extraversion, Openness, Agreeableness, and Conscientiousness. Within the 48 items in each domain of the NEO-PIR, there are six facets or sub-domains (eight items each), computed for secondary analyses. The NEO-FFI is a 60-item personality instrument consisting of a subset of 12 items (out of the total of 48 in the NEO-PIR) in each of the same five domains. Internal consistency of the five NEO-FFI domains as reported in the manual is as follows: Neuroticism = 0.79, Extraversion = 0.79, Openness = 0.80, Agreeableness = 0.75, and Conscientiousness = 0.83 (Costa and McCrae, 1992). To standardize the measure across both long and short versions, five personality domain scores were computed using the NEO-FFI algorithm. Using gender-specific population mean and standard deviation values provided in the NEO manual, raw scores were converted to t-scores (M = 50, SD = 10). The NEO-FFI domain scores were set to missing if 10 or more of the 60 items were missing.
Moderator variable and covariates
Because having a non-spouse CG has been associated with faster rate of cognitive and functional decline in CR with AD (Norton et al., 2009), and there is greater likelihood of institutionalization when CG exhibits high levels of Extraversion (Pot et al., 2001), we examined whether kin relationship of CG (spouse vs. adult child) moderated the association between personality traits and rate of cognitive decline. Education was recorded in years. Behavioral problems associated with dementia were measured with the neuropsychiatric interview (NPI), which possesses strong content and concurrent validity, and excellent inter-rater and test–retest reliability. In each of the ten behavioral domains, the product of severity (ranging from 1–3 for mild, moderate, and severe) and frequency (ranging from 1–4 for occasional, often, frequently, very frequently) was computed, with a score of zero when a behavioral domain was absent. These products were summed to create a total NPI score ranging from 0–120, trichotomized as follows: none, “mild” (score > 0 but no domain had frequency × severity > = 4), and “moderate to severe” (score > 0, one or more domains with frequency × severity ≥ 4).
Statistical analysis
Linear mixed models (LMM) of the trajectory of MMSE scores were computed from AD onset forward, using SPSS v20. LMM estimates the effects of fixed factors (e.g. personality traits) on cognitive status, while accounting for the within-subject correlation across time points. LMM accommodates attrition in longitudinal data, utilizing all available data from participants with incomplete participation at follow-up. A predictor variable was retained if its Wald statistic yielded p < 0.05 or the likelihood ratio χ2 test of nested models, including vs. and excluding the term yielded p < 0.05 (only the latter are reported herein for clarity). The MMSE trajectory was tested for a quadratic effect and found to be statistically significant; therefore, all models included a quadratic time effect.
Separate models were estimated for each of the five personality domains. Model fitting procedures began with a “base” model, including the personality trait and its interaction with time and time-squared. Next, kin relationship was tested for moderating effect via adding to the base model kin relationship and its interaction with both time and time-squared, and the interaction of these terms with the personality variable. LMM was adjusted for two additional covariates – CR educational level and behavioral disturbances (the latter having correlated significantly with at least two personality domains).
In secondary analyses we examined the six facets for the given domain to explore which component(s) of the trait were contributing significantly to the overall domain effect for NEO personality domains significantly associated with cognitive trajectory. This necessitated use of the subsample of subjects who completed the NEO-PIR long form. We first repeated the model derived on the larger sample (including long- and short-form NEO) using the long-form subsample to confirm that effects were robust (we always found this to be the case) and then computed separate models for each facet.
Results
Our analysis included 161 CR/CG dyads with NEO data. The 60 subjects without NEO data did not differ from NEO responders on any demographic variable examined (Table 1 footnote). Dyads were followed for periods of time ranging between 1 and 14 years (M = 5.65, SD = 2.89) and between 1 and 13 visits (M = 4.72, SD = 2.57). CRs were 60% females, with a mean age of 82.9 years (SD = 6.19) and education of 13.3 years (SD = 3.02). Behavioral disturbances were absent in 85 (55%), “mild” in 38 (25%), and “moderate to severe” in 31 (20%) CRs. CGs providing NEO data were 78% females with a mean age of 67.9 years (SD = 13.62) and an education of 14.3 years (SD = 2.39); 34% of CGs were spouses to the CR, and 66% were adult child(ren) (or child(ren)-in-law; comparison of NEO responders and non-responders appears as a footnote in Table 1).
Table 1.
Mean (SD) of each of the five personality traits of AD caregivers from NEO-FFI, overall and by caregiver gender, and caregiver relationship to person with ADa
| PERSONALITY DOMAIN b | OVERALL
|
CAREGIVER GENDER
|
CAREGIVER RELATIONSHIP
|
||||
|---|---|---|---|---|---|---|---|
| MEAN(SD); ONE -SAMPLE t-TESTc | MALE (n = 35) | FEMALE (n = 126) | IN -DEP. SAMPLES t-TESTd | SPOUSE (n = 55) | ADULT CHILD (n = 106) | IN -DEP. SAMPLES t-TESTd | |
| Neuroticism | 50.3 (8.8), t = 1.66, df = 2,092, p = 0.097 | 48.9 (8.7) | 51.3 (8.7) | t = −6.17, df = 2,091, p < 0.001 | 48.5 (8.5) | 51.3 (8.8) | t = 7.03, df = 2,091, p < 0.001 |
| Extraversion | 48.4 (9.2), t = −8.18, df = 2,092, p < 0.001 | 49.1 (9.3) | 47.9 (9.1) | t = 3.09, df = 2,091, p = 0.002 | 48.1 (9.0) | 48.5 (9.3) | t = 0.80, df = 2091, p = 0.429 |
| Openness | 46.3 (8.4), t = −19.87, df = 2,092, p < 0.001 | 45.2 (7.9) | 47.1 (8.7) | t = −5.03, df = xx, p < 0.001 | 45.6 (7.7) | 46.7 (8.7) | t = 2.84, df = 2,091, p = 0.005 |
| Agreeableness | 51.8 (10.2), t = 8.14, df = 2,092, p < 0.001 | 52.8 (8.9) | 51.2 (10.9) | t = 3.50, df = 2,091, p < 0.001 | 52.9 (11.0) | 51.2 (9.8) | t = −3.65, df = 2,091, p < 0.001 |
| Conscientiousness | 46.0 (10.3), t = −17.85, df = 2,092 p < 0.001 | 44.6 (11.1) | 47.0 (9.5) | t = −5.28, df = 2091, p < 0.001 | 44.6 (11.5) | 46.7 (9.4) | t = 4.63, df = 2,091, p < 0.001 |
Notes:
Compared to NEO non-responders (NR), NEO responders were not significantly different in age (M = 76.4/SD = 6.0 vs. M = 75.3/SD = 5.9 (NR), t = 1.16, df = 219, p = 0.248), were no better educated (M = 13.3/SD = 3.0 vs. M = 13.1/SD = 3.0 (NR), t = 0.345, df = 219, p = 0.730), were no more likely to be female (60.2% vs. 63.3% (NR), χ2 = 0.175, df = 1, p = 0.676), and did not differ on presence of e4 allele (47.2% vs. 50.0% (NR), χ2 = 0.137, df = 1, p = 0.711).
Each personality domain score was converted to a t-score with a mean of 50 and a standard deviation of 10; thus, mean scores above 50 indicate a personality trait that is more pronounced, while mean scores below 50 indicate personality traits that are less pronounced, in the CGs in the present study, compared to population norms.
One-sample t-test to test null hypothesis that each personality domain mean is equal to 50.
Independent samples t-test comparing either male versus female CRs or spouse versus adult child CRs with sample sizes as noted in the table.
Cronbach α internal consistency reliability coefficients for the five NEO-FFI domain scores were 0.788, 0.731, 0.668, 0.801, and 0.847 for Neuroticism, Extraversion, Openness, Agreeableness, and Conscientiousness, respectively. Compared to a t-score mean of 50, CGs in this cohort reported average level of Neuroticism, but were slightly higher on Agreeableness and slightly lower on Extraversion, and were somewhat lower on Openness and Conscientiousness (Table 1). Pair-wise correlation between domains ranged from −0.39 to −0.49 (Neuroticism vs. Extraversion, Agreeableness, and Conscientiousness), from +0.23 to +0.42 (Extraversion vs. Openness, Agreeableness, and Conscientiousness), was +0.24 for Agreeableness vs. Conscientiousness (all p < 0.001; other correlation coefficients had p > 0.05).
Females reported significantly higher levels of Neuroticism, Openness, and Conscientiousness than males, while males reported significantly higher levels of Extraversion and Agreeableness than females (Table 1). Spouses reported significantly higher levels of Agreeableness, while adult child CGs reported significantly higher levels of Neuroticism, Openness, and Conscientiousness (Table 1).
Rate of care receivers cognitive decline as a function of caregiver personality
Significantly faster cognitive decline was observed with higher CG Neuroticism (Table 2). Higher CG Neuroticism facet scores were associated with faster cognitive decline for anxiety and depression, with a trend for vulnerability to stress. Angry hostility, self-consciousness, and impulsiveness facets were not related to rate of decline.
Table 2.
Omnibus F-tests in linear mixed models of (rate and acceleration of) cognitive decline in a sample of 161 persons with Alzheimer’s disease as a function of caregiver personality traitsa
| NEO DOMAIN | OVERALL DOMAIN | INDIVIDUAL FACETS | MODERATION BY KIN RELATIONSHIP |
|---|---|---|---|
| Neuroticism (higher Neuroticism = faster decline) | F(1,369) = 13.32, p < 0.001 F(1,388) = 21.59, p < 0.001 |
Anxiety: F(1,282) = 5.68, p = 0.018 F(1,307) = 8.60, p = 0.004 Depression: F(1,236) = 16.79, p < 0.001 F(1,321) = 27.59, p < 0.001 Vulnerability to stress: F(1,259) = 2.99, p = 0.085 F(1,271) = 4.26, p = 0.040 |
F(1,382) = 3.56, p = 0.060 F(1,416) = 7.77, p = 0.006 Adult child CG: F(1, 232) = 13.02, p < 0.001 F(1,253) = 25.41, p < 0.001 Spouse CG: F(1,163) = 0.29, p = 0.592 F(1,151) = 0.01, p = 0.905 |
| Extraversion (higher Extraversion = slower decline) | F(1,371) = 1.88, p = 0.171, F(1,274) = 5.81, p = 0.017 | Not computed because overall domain was n.s. | F(1,394) = 0.01, p = 0.012, F(1,290) = 0.003, p = 0.003 Adult child CG: F(1,220) = 5.59, p = 0.019, F(1,169) = 11.23, p = 0.001 Spouse CG: F(1,171) = 2.69, p = 0.103, F(1,125) = 2.92, p = 0.090 |
| Openness | F(1,285) = 0.39, p = 0.531, F(1,248) = 0.10, p = 0.751 | Not computed because overall domain was n.s. | F(1,297) = 0.11, p = 0.744, F(1,288) = 0.22, p = 0.638 |
| Agreeableness | F(1,285) = 1.35, p = 0.247, F(1,247) = 0.70, p = 0.405 | Not computed because overall domain was n.s. | F(1,304) = 0.58, p = 0.449, F(1,279) = 0.09, p = 0.764 |
| Conscientiousness | F(1,273) = 0.05, p = 0.831, F(1,264) = 0.12, p = 0.729 | Not computed because overall domain was n.s. | F(1,307) = 0.24, p = 0.623, F(1,309) = 0.001, p = 0.979 |
Note:
Additional covariates included CR education and neuropsychiatric disturbances.
Higher Neuroticism was associated with significantly faster cognitive decline in participants with adult child CGs, but not with spouse CGs (Table 2). Because cognitive trajectory is non-linear and effect size varies across time, we provide graphs showing estimates of cognitive scores as a function of time, for illustrative values of covariates in the model at 25th, 50th, and 75th percentiles (Figure 1). The relative shape of the three resulting curves in each plot is unchanged, but moves vertically up or down, at other covariate values. Decline is notably faster at higher levels of Neuroticism for adult child CGs, but with little association for spouse CGs. The results were robust after adjustment for co-residency (not shown in Figure 1).
Figure 1.
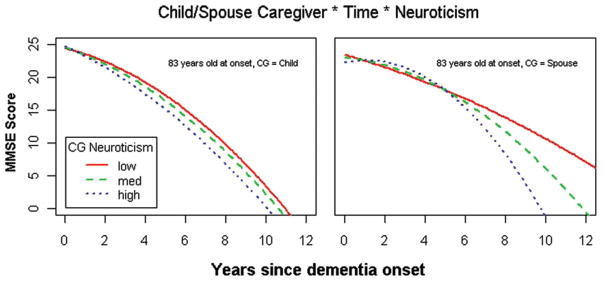
(Colour online) Higher level of self-reported caregiver Neuroticism is significantly associated with faster rate of cognitive decline among persons with AD cared for by adult child, but with non-significant association for persons with AD cared for by spouses (total n = 161; interaction p <0.001).
Caregiver Extraversion did not have a significant overall effect on rate of CR cognitive decline; however, kin relationship was a significant moderator (Table 2). Slower cognitive decline was observed when CG was an adult child, who reported higher Extraversion, but effect was non-significant with spouse CGs (robust after adjustment for co-residency; results not shown). Openness, Agreeableness, and Conscientiousness were not significantly associated with cognitive decline, and were also not moderated by kin relationship.
Discussion
In this population-based sample of incident cases of AD, higher CG Neuroticism was associated with faster cognitive decline in the CR, controlling for behavioral disturbances in the CR, an indicator of dementia severity. Results are similar to prior findings that CGs high in Neuroticism tend to use more emotional and maladaptive coping strategies (Hooker et al., 1994), consistent with our result of faster CR decline associated with Neuroticism facets of depression, anxiety, and vulnerability to stress. Individuals with higher Neuroticism tend to be more emotionally withdrawn, more focused on worries and fears, and more sensitive to perceived stress (Costa and McCrae, 1992). We suspect that these attributes might impede the CGs’ ability to effectively engage their CRs in positive and stimulating experiences, which in prior research are associated with slower dementia progression (Treiber et al., 2011). CGs scoring high on Neuroticism also tend to feel greater frustration with the caregiving role (Bookwala and Schulz, 1998). CRs have a significant level of awareness of their CGs’ state of psychological health (Ablitt et al., 2010), and thus it is possible that perceiving their CGs’ depression, anxiety and frustrations may negatively influence the CRs’ mood, and contribute toward overall cognitive decline.
The effects of Neuroticism were moderated by CG kin relationship, with the strongest effects found among CRs cared for by adult children. It is plausible that in spouse CGs, an accustomed lifelong pattern of interactional styles and relational adjustments has been already established long before CR’s transition into dementia, while CRs with adult child CGs may have experienced a more abrupt exposure to CG personality. These CRs face a multitude of psychological challenges – declining cognitive capacity, possible spousal bereavement, loss of autonomy and independent living, and concerns about having become a burden to their family. A change in CR residence may also reduce social connectedness. In the spousal caregiving setting, the spouse has made a lifelong commitment and may feel that the caregiving role is their duty. Adult child CGs may have simultaneous responsibilities to their own families and often an employer, which may cause the CR to perceive that he or she is a burden to the adult child CG, especially if that CG exhibits anxiety, depression, and stress.
Higher CG Extraversion was associated with slower decline among CRs cared for by adult children, potentially because this makes the CG more proactive in discussing dementia care options with healthcare providers. A positive social environment can enable the CR to experience relative well-being. Higher levels of Extraversion may also be found in CGs more willing to engage CRs in activities with social stimulation. Pot et al. (2001) demonstrated that Extraversion effects were present only among non-spouse CGs, but higher Extraversion was associated with an increased likelihood of institutionalization. We also observed a trend for slower cognitive decline with higher Extraversion in CRs cared for by a spouse, consistent with prior findings that CRs had more positive emotions when their spouse CG had higher Extraversion (Rabins et al., 1990). No other NEO personality trait was associated with CR rate of decline.
Strengths and limitations
A potential measurement limitation is that we used a mixture of short- and long-form NEO measurement; however, robustness of findings between long-form subsample only and full sample lessens concerns for biases. In addition, we emphasize that ethnic and religious homogeneity of this sample may limit generalizability of findings to similar populations.
A major strength is that these data are derived from one of the few population-based studies of dementia progression in the world; this would likely increase generalizability compared to studies using clinic-based samples. The length of follow-up, averaging nearly six years, allowed us to obtain data individuals who progressed from mild to more advanced stages of dementia. Adjusting models for neuropsychiatric disturbance measures allowed model adjustment for dementia severity.
Future directions
Whether CG personality directly impacts the pathobiology of the disease or acts indirectly through CG depression, anxiety, and stress vulnerability cannot be determined here. The identification of potential mechanisms underlying these associations requires further study. Higher CG Neuroticism and distress proneness have been linked to higher CR depression (Ruiz et al., 2006), and elsewhere, CR depression is associated with a faster rate of cognitive decline (Rapp et al., 2011), suggesting one possible mechanism. CGs high in Neuroticism report higher levels of CG burden (Shurgot and Knight, 2005), and elsewhere burden is associated with faster cognitive decline in the CR (Viatonou et al., 2009), another potential pathway. The third potential mechanism may derive from CGs higher in Neuroticism tending to use less problem-focused coping (Chappell and Dujela, 2009), which has been linked to slower cognitive decline (Tschanz et al., 2013). CGs with more adaptive coping styles may be better able to formulate and implement an effective plan to address challenging aspects of dementia caregiving.
While personality traits are largely stable (Roberts and DelVecchio, 2000), individuals with high Neuroticism may exhibit modifiable behaviors amenable to interventions designed to decrease depression and anxiety. Understanding personality may help psychosocial interventions to be more targeted and effective. It may also be advisable when training professionals who provide help to family caregivers to distinguish between CG-spouses and CG-adult children concerning CG personalities. It may be possible to train CGs to adopt alternative ways to think about, react, or adapt to the challenges of caregiving, recognizing that therapeutic approaches may work differently across individuals with different personality types. In this context, interventions that target the vulnerabilities associated with high levels of Neuroticism seem promising, but warrant further study.
Conclusion
To our knowledge, this is the first population-based study of dementia progression to identify an association between caregiver personality traits and rate of cognitive decline in persons with AD. Findings contribute toward a broader understanding of how the “caregiving environment” may be optimized as a complement to other (e.g. pharmacological) modes of intervention aimed at slowing the progression of disease. While additional studies will be necessary to determine which mechanism(s) are involved, these initial results can stimulate such studies and encourage replication with other datasets.
Acknowledgments
This work was supported by the National Institutes of Aging (grant numbers R01AG21136 and R01AG11380). The authors are indebted to Dr. Ronald Munger for his unqualified support of the DPS. We also acknowledge the contributions of the following individuals whose activities have helped to ensure the success of the project: John C. S. Breitner, MD, MPH, Cara Brewer, BA, Tony Calvert, RN, BA, Michelle Carlson, PhD, Kimberly Graham, BA, Jeanne-Marie Leoutsakos, PhD, Carol Leslie, MS, Lawrence S. Mayer, PhD, Michelle M. Mielke, PhD, Chiadi U. Onyike, MD, Georgiann Sanborn, MS, Nancy Sassano, PhD, Sarah Schwartz, MS, Ingmar Skoog, MD, Martin Steinberg, MD, Katherine Treiber, PhD, Yorghos Tripodis, PhD, Kathleen A. Welsh-Bohmer, PhD, Heidi Wengreen, PhD, RD, James Wyatt, and Peter P. Zandi, PhD, MPH. Finally, we thank the participants and their families for their generous contributions to this study.
Footnotes
Description of authors’ roles
M. Norton assisted with collecting the data, formulated the research questions, interpreted the statistical analyses, and wrote the paper. C. Clark, E. Fauth, K. Piercy, and R. Greene assisted with writing the paper. K. Piercy also assisted with collecting the data. R. Pfister conducted and C. Corcoran supervised the statistical analyses. P. Rabins assisted with formulating the research questions and writing the paper. J. Tschanz and C. Lyketsos supervised data collection, formulated the research questions, and assisted with writing the paper.
Conflict of interest
Conflicts of Interest and Source of Funding: Lyketsos grant support (NIMH, NIA, Assoc. Jewish Fe. of Baltimore, Weinberg Foundation, Forest, Glaxo-Smith-Kline, Eisai, Pfizer, Astra-Zeneca, Lilly, Ortho-McNeil, Bristol-Myers, Novartis, National Football League, Elan, Functional Neuromodulation Inc., Janssen), Lyketsos consulting (Astra-Zeneca, Glaxo-Smith Kline, Eisai, Novartis, Forest, Supernus, Adlyfe, Takeda, Wyeth, Lundbeck, Merz, Lilly, Pfizer, Genentech, Elan, NFL Players Assoc, NFL Benefits Office, Avanir, Zinfandel, BMS), Lyketsos honorarium/travel support (Pfizer, Forest, Glaxo-Smith-Kline, Health Monitor). All other authors have no disclosures to report.
References
- Ablitt A, Jones G, Muers J. Awareness of carer distress in people with dementia. International Journal of Geriatric Psychiatry. 2010;25:1246–1252. doi: 10.1002/gps.2461. [DOI] [PubMed] [Google Scholar]
- Alzheimer’s Association. [last accessed 25 June 2013];2012 Alzheimer’s disease facts and figures. 2012 Available at: http://www.alz.org/downloads/facts_figures_2012.pdf.
- Behl P, Stefurak TL, Black SE. Progress in clinical neurosciences: cognitive markers of progression in Alzheimer’s disease. Canadian Journal of Neurological Sciences. 2005;32:140–151. doi: 10.1017/s0317167100003917. [DOI] [PubMed] [Google Scholar]
- Bookwala J, Schulz R. The role of neuroticism and mastery in spouse caregivers’ assessment of and response to a contextual stressor. Journals of Gerontology: Psychological Sciences and Social Sciences. 1998;53:P155–P164. doi: 10.1093/geronb/53B.3.P155. [DOI] [PubMed] [Google Scholar]
- Breitner JCS, et al. APOE-epsilon4 count predicts age when prevalence of AD increases, then declines: the Cache County Study. Neurology. 1999;53:321–331. doi: 10.1212/WNL.53.2.321. [DOI] [PubMed] [Google Scholar]
- Chappell NL, Dujela C. Caregivers – who copes how? International Journal of Aging and Human Development. 2009;69:221–244. doi: 10.2190/AG.69.3.d. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. Professional Manual: Revised NEO Five-Factor Inventory. Lutz, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- de Vugt ME, et al. Do caregiver management strategies influence patient behavior in dementia? International Journal of Geriatric Psychiatry. 2004;19:85–92. doi: 10.1002/gps.1044. [DOI] [PubMed] [Google Scholar]
- Hooker K, Frazier LD, Monahan DJ. Personality and coping among caregivers of spouses with dementia. Gerontologist. 1994;34:386–392. doi: 10.1093/geront/34.3.386. [DOI] [PubMed] [Google Scholar]
- Jang Y, Clay OJ, Roth DL, Haley WE, Mittelman MS. Neuroticism and longitudinal change in caregiver depression: impact of a spouse-caregiver intervention program. Gerontologist. 2004;44:311–317. doi: 10.1093/geront/44.3.311. [DOI] [PubMed] [Google Scholar]
- Kitwood T. Toward a theory of dementia care: the interpersonal process. Ageing and Society. 1993;13:51–67. doi: 10.1017/s0144686x0000502x. doi:org/10.1017/S0144686X00000647. [DOI] [PubMed] [Google Scholar]
- Koerner SS, Kenyon DB, Shirai Y. Caregiving for elder relatives: which caregivers experience personal benefits/gains? Archives of Gerontology and Geriatrics. 2009;48:238–245. doi: 10.1016/j.archger.2008.01.015. [DOI] [PubMed] [Google Scholar]
- Melo G, Maroco J, de Mendonca A. Influence of personality on caregiver’s burden, depression and distress related to the BPSD. International Journal of Geriatric Psychiatry. 2011;26:1275–1282. doi: 10.1002/gps.2677. [DOI] [PubMed] [Google Scholar]
- Morris JC, et al. The consortium to establish a registry for Alzheimer’s disease (CERAD). Part IV. Rates of cognitive change in the longitudinal assessment of probable Alzheimer’s disease. Neurology. 1993;43:2457–2465. doi: 10.1212/WNL.43.12.2457. [DOI] [PubMed] [Google Scholar]
- Norton MC, et al. Caregiver–recipient closeness and symptom progression in Alzheimer disease. The Cache County Dementia Progression Study. Journal of Gerontology: Psychological Sciences. 2009;64B:560–568. doi: 10.1093/geronb/gbp052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pot AM, Deeg DJH, Knipscheer CPM. Institutionalization of demented elderly: the role of caregiver characteristics. International Journal of Geriatric Psychiatry. 2001;16:273–280. doi: 10.1002/gps.331. [DOI] [PubMed] [Google Scholar]
- Rabins PV, Fitting MD, Eastham J, Fetting J. The emotional impact of caring for the chronically ill. Psychosomatic Medicine. 1990;31:331–336. doi: 10.1016/S0033-3182(90)72171-8. [DOI] [PubMed] [Google Scholar]
- Rapp M, et al. Cognitive decline in patients with dementia as a function of depression. American Journal of Geriatric Psychiatry. 2011;19:357–363. doi: 10.1097/JGP.0b013e3181e898d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis MF, Gold DP, Andres D, Markiewicz D, Gauthier S. Personality traits as determinants of burden and health complaints in caregiving. International Journal of Aging and Human Development. 1994;39:257–271. doi: 10.2190/6LYN-YFWQ-P87D-MKWX. [DOI] [PubMed] [Google Scholar]
- Roberts BW, DelVecchio WF. The rank-order consistency of personality traits from childhood to old age: a quantitative review of longitudinal studies. Psychological Bulletin. 2000;126:3–25. doi: 10.1037/0033-2909.126.1.3. [DOI] [PubMed] [Google Scholar]
- Ruiz JM, Matthews KA, Scheier MG, Schulz R. Does who you marry matter for your health? Influence of patients’ and spouses’ personality on their partners’ psychological well-being following coronary artery bypass surgery. Journal of Personality and Social Psychology. 2006;91:255–267. doi: 10.1037/0022-3514.91.2.255. [DOI] [PubMed] [Google Scholar]
- Scarmeas N, et al. Delusions and hallucinations are associated with worse outcome in Alzheimer disease. Archives of Neurology. 2005;62:1601–1608. doi: 10.1001/archneur.62.10.1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Beach SR. Caregiving as a risk factor for mortality: the caregiver health effects study. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- Shurgot GR, Knight BG. Influence of neuroticism, ethnicity, familism, and social support on perceived burden in dementia caregivers: pilot test of the transactional stress and social support model. Journal of Gerontology: Psychological Sciences. 2005;60:S331–S334. doi: 10.1093/geronb/60.6.P331. [DOI] [PubMed] [Google Scholar]
- Teri L, Logsdon RG, Uomoto J, McCurry S. Behavioral treatment of depression in dementia patients: a controlled clinical trial. Journals of Gerontology: Psychological Sciences and Social Sciences. 1997;52:P159–P166. doi: 10.1093/geronb/52B.4.P159. [DOI] [PubMed] [Google Scholar]
- Teri L, McCurry SM, Edland SD, Kukull WA, Larson EB. Cognitive decline in Alzheimer’s disease: a longitudinal investigation of risk factors for accelerated decline. Journals of Gerontology: Biological Sciences and Medical Sciences. 1995;50A:M49–M55. doi: 10.1093/gerona/50A.1.M49. [DOI] [PubMed] [Google Scholar]
- Treiber KA, et al. Cognitive stimulation and cognitive and functional decline in Alzheimer’s disease: the Cache County Dementia Progression Study. Journals of Gerontology: Psychological Sciences and Social Sciences. 2011;66:416–425. doi: 10.1093/geronb/gbr023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tschanz JT, et al. Progression of cognitive, functional and neuropsychiatric symptom domains in a population cohort with Alzheimer’s dementia. The Cache County Dementia Progression Study. American Journal of Geriatric Psychiatry. 2011;19:532–542. doi: 10.1097/JGP.0b013e3181faec23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tschanz JT, et al. Caregiver coping strategies predict rate of cognitive and functional decline in dementia. The Cache County Dementia Progression Study. American Journal of Geriatric Psychiatry. 2013;21:57–66. doi: 10.1016/j.jagp.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viatonou S, et al. Predictors of rapid cognitive decline among demented subjects aged 75 or more: (“Sujet Age’ Fragile–Evaluation et Suivi” Cohort – SAFES) International Journal of Geriatric Psychiatry. 2009;24:709–715. doi: 10.1002/gps.2183. [DOI] [PubMed] [Google Scholar]


