Abstract
Aim
To investigate the sodium composition of maintenance intravenous fluids used by paediatric residents throughout the United States in common clinical scenarios of arginine vasopressin excess.
Methods
We distributed an online survey to paediatric residency programs asking what type of maintenance intravenous fluids (0.2%, 0.45%, 0.9% NaCl or Lactated Ringers) they would administer in four common clinical scenarios of arginine vasopressin excess (gastroenteritis, pneumonia, meningitis and post-operative) in both a 6-month-old (mo) and a 13-year-old (yo) child.
Results
We had 472 responses, representing 5% of the total paediatric residency population in the US. Hypotonic maintenance intravenous fluids were selected in 78% of children (88.2% of 6 mo and 68.5% of 13 yo). Isotonic maintenance intravenous fluids were selected approximately twice as often for patients with meningitis as for those without (21.4% vs 8.7% 6 mo and 42.8% vs 27.7% 13 yo; p <.0.001).
Conclusions
The majority of US paediatric residents would prescribe hypotonic maintenance intravenous fluids in disease states associated with arginine vasopressin excess. However, a significant number of residents are using isotonic maintenance intravenous fluids. Isotonic fluids are more likely to be prescribed in older children and children with meningitis.
Keywords: Fluid therapy, sodium, saline, hyponatraemia, children
Introduction
Over the past decade, there has been increasing concern within the paediatric community that the commonplace practice of using hypotonic fluids for maintenance intravenous fluid (mIVF) therapy may contribute to or induce dangerous hyponatraemia in patients (1, 2). Numerous retrospective, observational, and randomized controlled studies have confirmed that hypotonic fluids contribute to hospital-acquired hyponatraemia (3-6). These studies, as well as the numerous reports of iatrogenic hyponatraemic encephalopathy, have drawn the attention of patient safety organizations. The British National Patient Safety Agency (7) and the Institutes of Safe Medication Practices of both Canada and the United States have issued patient safety alerts concerning the use of hypotonic fluids (8). These studies have generated a debate in the paediatric community as to the most appropriate sodium composition of intravenous fluids, hypotonic or isotonic (9, 10).
We conducted a study to assess current mIVF prescribing practices in light of this new literature. To evaluate this, we distributed an online survey among US paediatric residents asking them what sodium composition of mIVF they would administer in a variety of common clinical scenarios. We chose scenarios that are known to be associated with arginine vasopressin (AVP) excess and hospital-acquired hyponatraemia. We chose to survey paediatric residents for this study because their practices reflect what is being taught and practiced in major paediatric centers across the US.
Methods
The survey was constructed using an online survey tool. The survey and study design was assessed by the institutional review board at the University of Pittsburgh and was granted exempted status. It was distributed on November 18th 2009 to Residency Program directors of the paediatrics and paediatrics/combined specialty programs listed within the Fellowship and Residency Electronic Interactive Database Access System (FREIDA), the American Medical Association database of all accredited graduate medical education programs. Upon receipt, it was at the discretion of the program director to distribute the survey to residents. We requested that the program directors reply with the number of residents to whom the survey was distributed to aid in determining the survey response rate. Respondents were informed that responses were anonymous and that the survey was for the purpose of research.
Respondents were asked to provide basic demographic data including year of postgraduate training, location of residency program, and size of residency program (See Appendix S1). The program location was categorized into four regions as defined by the US Census Bureau: Northeast, South, Midwest and West (11). The size of the residency program was defined by number of residents per year and segmented into groups of fewer than 15 (small), between 15 and 25 (mid), and more than 25 (large).
The survey presented four common clinical scenarios in which paediatric patients receive mIVF therapy: gastroenteritis, pneumonia, meningitis, and post-operative following a nissen-fundoplication procedure (See Appendix S1). The respondents were asked to assume that the patients were of average weight, had no known electrolyte disturbances, had received 1-2 normal saline fluid boluses in the emergency department if indicated, had adequate urine output, and shows no overt signs of clinical dehydration. They were also asked to ignore considerations of dextrose or other supplemental electrolytes. In all scenarios the patient was either explicitly made NPO or it was noted that the patient was not tolerating any oral intake. Respondents were asked to select the type of maintenance fluid they would normally use in each scenario for both a 6-month-old(mo) infant and a 13-year-old(yo) adolescent. Respondents were allowed to select from four fluid options: 0.2% NaCl, 0.45% NaCl, 0.9% NaCL and Lactated Ringer’s (LR) solution. They were also asked to state the criteria they commonly use to select the sodium content of the intravenous fluids they prescribe. As a final question, they were asked whether or not they are familiar with the clinical controversy regarding the use of hypotonic maintenance fluids. The study was structured so that respondents could not change any previous survey answers once a question had been completed
The results of the survey were analyzed using χ2 testing to look for variations in prescribing patterns among the clinical scenarios. The scenarios involving the 6-mo infant and 13-yo adolescent were analyzed separately due to profound differences in the fluids selected for each group. The data were then cross-tabulated by the demographic responses. Univariate odds ratios and 95% confidence intervals were then calculated and compared against a designated standard in each group. Due to the paucity of responses selecting LR solution, the solutions were grouped into either hypotonic (0.2% NaCl, 0.45% NaCl) or isotonic (0.9% NaCl or LR) for the purpose of analysis.
Results
We received a total of 536 responses to our survey. Of these, 64 responses included only demographic information without addressing the clinical scenarios and were therefore excluded from the study. An estimated 2457 surveys were distributed by program director report, giving an effective response rate of 19.2%. Our respondents represent approximately 5% of the total paediatric resident population (12)), which gave an estimated survey accuracy of 95% confidence with a 4% margin of error (13).
The demographic data of the respondents is detailed in Table 1. The respondents were well distributed by the demographic criteria selected. Respondents from the Northeast were slightly overrepresented, constituting 36.7% of survery respondents compared to 26% of residents nationally. For all other regions, the response rates were proportional to the population of residents from that region, within a variability of 4%. Respondents from small programs were underrepresented, constituting 29% of survey respondents compared to 52% of residents nationally. The fluids selected by the respondents for each scenario are shown in Figures 1 and 2 for the 6-month-old infant and 13-year-old adolescent, respectively. Hypotonic fluids were selected for 78% of children and isotonic fluids for 22%. The selection of mIVF was affected by both age and disease process. Residents were more likely to select hypotonic mIVF for younger children (88.2% 6 mo and 68.5% 13 yo) and isotonic mIVF for older children (11.8% 6 mo and 31.5% 13 yo, respectively). The most commonly prescribed mIVF was 0.45% NaCl (administered to 52.6% of 6 mo and 68.0% of 13 yo). 0.2% NaCl was commonly used in the 6 mo (35.6%) and rarely used in the 13 yo (0.55%).
Table 1.
Response rate, demographic information and general question results from survey respondents
| Category | Variable | N | % |
|---|---|---|---|
| Response Rate | Surveys Distributed | 2457 | |
| Responses | 472 | 19.2 | |
| Year of Training | PGY-1 | 133 | 28.2 |
| PGY-2 | 156 | 33.1 | |
| PGY-3 | 153 | 32.4 | |
| PGY-4 | 30 | 6.4 | |
| Location of Residency | Northeast | 173 | 36.7 |
| South | 113 | 23.9 | |
| Midwest | 130 | 27.5 | |
| West | 56 | 11.9 | |
| Size of Residency Class | Less than 15 | 138 | 29.2 |
| 15-25 | 164 | 34.7 | |
| Greater than 25 | 170 | 36.0 | |
| Aware of Clinical Controversy | Yes | 356 | 75.4 |
| No | 116 | 24.6 | |
| Primary Criteria Used for Selecting MIVF Tonicity | Patient’s Age | 234 | 49.6 |
| Patient’s Weight | 118 | 25.0 | |
| Calculated Na Requirement | 57 | 12.1 | |
| Other | 63 | 13.3 |
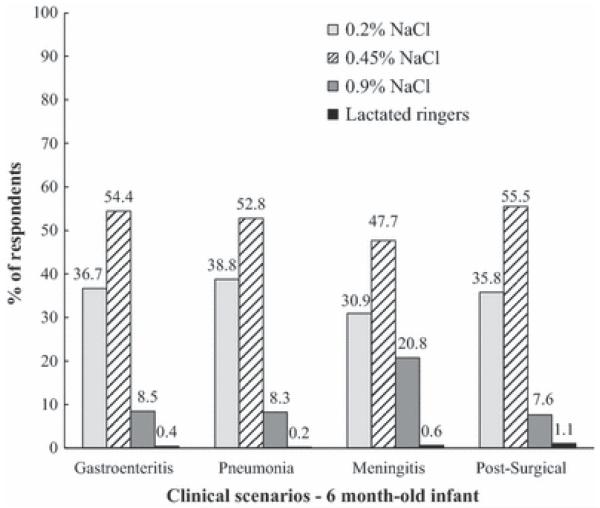
Fig. 1.
Fluid selected by respondents in each clinical scenario for the 6 month-old infant. The respondents predominantly selected hypotonic fluids in all cases. They were significantly more likely to select isotonic fluids in patients with meningitis as compared to all other cases. (p <0.001)
Fig. 2.
Fluid selected by respondents in each clinical scenario for the 13 year-old child. The respondents predominantly selected hypotonic fluids in all cases. They were significantly more likely to select isotonic fluids in patients with meningitis as compared to all other cases. (p <0.001)
Isotonic mIVF were selected approximately twice as often for patients with meningitis as for those without, (21.4% vs. 8.7% in 6mo and 42.8% vs. 27.7% in 13 yo; p <0.001). Fluid selection was relatively similar for disease states other than meningitis.
The respondents’ aggregate responses following cross-tabulation by demographic factors revealed few overarching patterns. The respondents’ awareness of the clinical controversy (Table 1) was the factor most closely correlated with selection of isotonic fluids. Those respondents who were aware of the clinical controversy were approximately twice as likely to utilize isotonic fluids as those who were not (24.5% vs. 12.9%; OR 1.996; 95%CI 1.557-2.558; p <0.001).
For a preponderance of respondents, the patient’s age was the primary determining factor when selecting mIVF (49.6% of respondents, Table 1). Only 12.1% calculated an estimated Na requirement, the method outlined by Holliday and Segar (14). Of the 13.3% who designated other criteria, representative answers included: the patient’s underlying illness, the patient’s calculated free water needs, the institutional culture and a default selection of one fluid for all scenarios.
Discussion
The majority of paediatric residents surveyed would prescribe hypotonic mIVF in common disease states that are known to be associated with AVP excess and hyponatraemia. However, despite the traditional educational emphasis on the use of hypotonic fluids, a substantial proportion of respondents selected fluid with a higher sodium concentration. The most common mIVF selected was 0.45% NaCl for both children and adolescents, which represents a significant increase in sodium concentration over the 0.2% NaCl originally proposed by Holliday and Segar(14) in 1957 and historically taught to paediatric residents(15, 16). Nearly half (42.8%) of the respondents elected to use isotonic fluids in the scenario involving the 13-yo child with meningitis and 21.4% of respondents chose to use these fluids for the 6-mo infant. Residents who were aware of the clinical controversy were almost twice as likely to select isotonic fluids as their colleagues who were not. Although we do not have compiled data regarding the use of maintenance intravenous fluids from decades past, this likely represents a substantial change from the traditional use of 0.2% NaCl in mIVF which has prevailed since the original formula published by Holliday and Segar.
The clinical scenarios selected for this survey all represent conditions associated with AVP excess where the risk of developing hyponatraemia has been well documented. Patients with gastroenteritis have both hemodynamic and non-hemodynamic stimuli for AVP production. Nausea and emesis are known stimulators of AVP release. Central nervous system and pulmonary disorders are a frequent cause of The Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH). Post-operative patients have numerous stimuli for AVP production including pain, stress, nausea, vomiting, third spacing and narcotic use. If AVP excess occurs in the setting of hypotonic fluid administration, dangerous hyponatraemia can develop (2). There have been over 20 studies, both prospective and retrospective, in approximately 2000 children which demonstrate that hypotonic fluids produce hyponatraemia and that isotonic fluids prevent it (6).
These studies underline the importance of practitioners involved in medical education turning a critical eye to the use of intravenous fluids in the clinical setting. Like many aspects of paediatric care that become ingrained during training, it is possible for the use and selection of IV fluids to become habit rather than an exercise in therapeutic evaluation. Just as many paediatric residents can state the dosing of acetaminophen or amoxicillin without a second thought, residents become used to ordering 0.2% NaCl fluids for infants and 0.45% NaCl fluids for older children. This habitual practice is reflected in the finding of our survey that only approximately 12% of respondents actually calculate a patient’s daily Na requirement, the method detailed in the Holliday-Segar formula, even though a majority of respondents continue to prescribe the hypotonic fluids that the formula suggests.
Conclusion
This study demonstrates that while the majority of paediatric residents would choose to use hypotonic mIVF in daily practice, there is growing support for the use of isotonic mIVF within this group and greater utilization of 0.45% NaCl rather than 0.2% NaCl. We feel that a preponderance of the research performed on this topic supports the use of isotonic fluids in the majority of clinical cases. More important than the choice of a given fluid, however, is a mindful awareness of the clinical situation in which fluids are used and an attentive re-evaluation of the necessary fluid choice as the clinical scenario changes. By emphasizing a critical evaluation of the data regarding the use of mIVF to paediatric residents in training, we can help to provide optimal care for patients both now and in the future.
Supplementary Material
Key Notes.
The majority of US paediatric residents would prescribe hypotonic maintenance intravenous fluids, 78%, in disease states associated with arginine vasopressin excess.
The most commonly selected maintenance intravenous fluid was 0.45% sodium chloride, 60%.
Isotonic maintenance intravenous fluids were most commonly selected in the scenario involving a child with meningitis, 32.1%.
Abbreviations
- AVP
Arginine vasopressin
- mIVF
Maintenance intravenous fluids
- FREIDA
Fellowship and Residency Electronic Interactive Database Access System
- mo
month-old
- yo
year-old
- NaCl
sodium chloride
- LR
Lactated Ringer’s
- SIADH
Syndrome of inappropriate antidiuretic hormone secretion
References
- 1.Moritz ML, Ayus JC. Prevention of hospital-acquired hyponatremia: a case for using isotonic saline. Pediatrics. 2003;111:227–30. doi: 10.1542/peds.111.2.227. [DOI] [PubMed] [Google Scholar]
- 2.Moritz ML, Ayus JC. Preventing neurological complications from dysnatremias in children. Pediatr Nephrol. 2005;20:1687–700. doi: 10.1007/s00467-005-1933-6. [DOI] [PubMed] [Google Scholar]
- 3.Arieff AI, Ayus JC, Fraser CL. Hyponatraemia and death or permanent brain damage in healthy children. BMJ. 1992;304:1218–22. doi: 10.1136/bmj.304.6836.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoorn EJ, Geary D, Robb M, Halperin ML, Bohn D. Acute hyponatremia related to intravenous fluid administration in hospitalized children: an observational study. Pediatrics. 2004;113:1279–84. doi: 10.1542/peds.113.5.1279. [DOI] [PubMed] [Google Scholar]
- 5.Neville KA, Sandeman DJ, Rubinstein A, Henry GM, McGlynn M, Walker JL. Prevention of hyponatremia during maintenance intravenous fluid administration: a prospective randomized study of fluid type versus fluid rate. J Pediatr. 2010;156:313–9. e1–2. doi: 10.1016/j.jpeds.2009.07.059. [DOI] [PubMed] [Google Scholar]
- 6.Moritz ML, Ayus JC. Prevention of hospital-acquired hyponatremia: do we have the answers? Pediatrics. 2011;128:980–3. doi: 10.1542/peds.2011-2015. [DOI] [PubMed] [Google Scholar]
- 7.National Patient Safety Agency . Patient Safety Alert 22:Reducing the risk of hyponatremia when administring intravenous infusions to children. London: UK: 2007. [Google Scholar]
- 8.Plain D5W or hypotonic saline solutions post-op could result in acute hyponatremia and death in healthy children. Vol. 14. Institute for Safe Medication Practices Medication Safety Alert!; 2009. pp. 1–4. [PubMed] [Google Scholar]
- 9.Hatherill M. Rubbing salt in the wound. Archives of disease in childhood. 2004;89:414–8. doi: 10.1136/adc.2003.045047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taylor D, Durward A. Pouring salt on troubled waters. Archives of disease in childhood. 2004;89:411–4. doi: 10.1136/adc.2003.045302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.United States. Bureau of the Census . Population and housing unit counts. Vol. 2003. U.S. Dept. of Commerce, Economics and Statistics Administration, U.S. Census Bureau : For sale by Supt. of Docs., U.S. G.P.O.; Washington, DC: 2000. census of population and housing. [Google Scholar]
- 12.National Resident Matching Program . Results and data: 2009 main residency match. National Resident Matching Program; Washington, D.C.: 2009. [Google Scholar]
- 13.National Statistic Service-Sample Size Calculator. National Statistic Service-Commonwealth of Australia; Belconnon, ACT: 2012. [Google Scholar]
- 14.Holliday MA, Segar WE. The maintenance need for water in parenteral fluid therapy. Pediatrics. 1957;19:823–32. [PubMed] [Google Scholar]
- 15.Chesney RW, Zelikovic I. Pre- and postoperative fluid management in infancy. Pediatr Rev. 1989;11:153–8. doi: 10.1542/pir.11-5-153. [DOI] [PubMed] [Google Scholar]
- 16.Roberts KB. Fluid and electrolytes: parenteral fluid therapy. Pediatr Rev. 2001;22:380–7. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.