Abstract
Purpose
The purpose of this study is to compare post-therapy third day and seventh day I-131 whole body scans (3DWBS and 7DWBS) in detecting lung or bone metastasis from well-differentiated thyroid cancer.
Materials and Methods
We enrolled 52 patients with lung or bone metastasis out of 1,152 patients who were treated with high-dose I-131 therapy from January 2008 to June 2009. All patients underwent 3DWBS and 7DWBS. I-131 avidity was classified into three grades: no uptake, suspicious for uptake, and definite uptake. We compared the presence and grades of metastatic lesions on each scan. We categorized all cases into three groups based on I-131 uptake on each scan and compared several clinical parameters including FDG uptake and thyroglobulin (Tg) level among the groups.
Results
Sixty metastatic cases from 52 patients (45 lung and 15 bone metastases) were included. In 35 cases, I-131-avid metastatic lesions were detected by both 3DWBS and 7DWBS (group A). In 15 cases, metastatic lesions were missed on 3DWBS but detected on 7DWBS (group B). In 10 cases, I-131 uptake was not detected on either 3DWBS or 7DWBS (group C). Ten of 45 cases (22.2%) of lung metastasis that were negative on 3DWBS were detected on 7DWBS (p = 0.002). Five of 15 cases (33.3%) of bone metastasis that were negative on 3DWBS were detected on 7DWBS (p = 0.0625). The serum Tg level (TSH stimulated) was significantly different among groups A, B, and C (p = 0.0030). However, after exclusion of cases without a history of I-131 therapy, there was no significant difference in serum Tg level among the groups (p = 0.2330). The number of cases with a prior history of metastasis was higher in group A than in group B (p = 0.0069). However, there was no significant difference in prior history of metastasis between groups A and C (p = 0.8107).
Conclusion
7DWBS showed more lung or bone metastatic lesions than 3DWBS. After high-dose I-131 therapy, 7DWBS should be considered regardless of the results of the 3DWBS for the diagnosis of lung or bone metastasis from well-differentiated thyroid cancer.
Keywords: Thyroid cancer, Distant metastasis, I-131, Post-therapy scan, Scan time
Introduction
Distant metastases occur in 7–23% of patients with thyroid cancer and are the main cause of thyroid cancer-related deaths [1–5]. The most common sites of distant metastasis from thyroid cancer are the lung and bones [6]. High-dose I-131 therapy is usually recommended for patients with well-differentiated thyroid cancer (DTC) to decrease the risk of recurrence, metastases, and disease-specific mortality [1].
An I-131 whole body scan (RxWBS) can detect the presence of metastases in patients treated with high-dose I-131 therapy [7, 8]. A recent study reported that a RxWBS after the first I-131 treatment resulted in a change in the disease stage in 8.3% and in the therapeutic approach in another 15% of patients [8]. Moreover, I-131 avidity of a metastatic lesion is an important factor in the determination of treatment approach and prognosis [8]. Following the high-dose I-131 therapy, a RxWBS is therefore recommended to assess residual I-131-avid tissue, including metastasis, in patients with DTC. Current guidelines for I-131 therapy differ in their recommendations for the optimal time of the post-therapeutic RxWBS ranging from 48–72 h [9, 10] to 2–10 days [1]. There is also a lot of discrepancy in the published literature regarding the optimal timing of post-therapy RxWBS [11–16]. In fact, several studies have showed that metastatic lesions can be missed on RxWBS when it is performed as early as 3–4 days after I-131 therapy [14, 17].
The aim of this study is to investigate I-131 uptake in lung or bone metastases on the 3rd and 7th days after high-dose I-131 therapy in patients with well-differentiated thyroid cancer, using I-131 whole body scans.
Materials and Methods
Patients and Inclusion Criteria
A total of 1,152 patients who were treated with high-dose I-131 therapy (≥3.7 GBq) from January 2008 to June 2009 underwent RxWBS on the 3rd and 7th days after therapy (3DWBS and 7DWBS, respectively). After a retrospective review of all 2,304 whole body scans (3DWBS and 7DWBS), we enrolled 52 patients with lung or bone metastasis in this study. The indications for high-dose I-131 therapy were ablation of residual thyroid gland and treatment of metastasis after total thyroidectomy with or without lymph node dissection. The presence of lung metastasis was confirmed by pathology, F-18 FDG PET/CT (PET/CT), or chest CT with correlation of serum thyroglobulin (Tg, TSH-stimulated). The presence of bone metastasis was confirmed by pathology, F-18 FDG PET/CT, or MRI with correlation of serum Tg (TSH-stimulated).
The exclusion criteria were (1) patients showing false-positive radioiodine uptake mimicking metastases in bronchiectatic lesions, esophagus, or thymus, as demonstrated by SPECT/CT, F-18 FDG PET/CT, or CT with correlation of the serum Tg (TSH-stimulated) level and (2) patients with metastases in locations other than lung and bone.
A total of 60 cases of lung or bone metastasis in 52 patients (45 lung and 15 bone metastases) were confirmed by pathology, PET/CT, CT, or MR with correlation of serum Tg and enrolled in this study [mean ± SD age 54.0 ± 14.2 years, M:F = 16:36, type of primary thyroid cancer: papillary (n = 45), follicular (n = 6), and Hurthle cell carcinoma (n = 1)].
I-131 Therapy Protocol
All patients were instructed to follow a low-iodine diet for the 2 weeks prior to I-131 therapy. Levothyroxine (LT4) withdrawal or recombinant human TSH (rhTSH) administration was used for TSH stimulation. Patients on the LT4 withdrawal protocol discontinued LT4 replacement for at least 4 weeks prior to I-131 therapy and were switched to triiodothyronine (T3) replacement for 2 weeks. Two weeks prior to I-131 therapy, T3 replacement was also discontinued.
Two weeks before I-131 treatment, F-18 FDG PET/CT (Discovery ST PET/CT system, General Electric Medical Systems, Milwaukee, WI) was performed after injection of F-18 FDG (375 MBq). Routine laboratory tests including serum Tg, anti-Tg antibody, thyroid-stimulating hormone (TSH), T3, and FT4 were done on the day of treatment. A serum TSH level of ≥30 IU/ml was required for I-131 therapy. On the 3rd day after administration of I-131, the patients underwent 3DWBS and resumed thyroid hormone replacement therapy and a normal diet. On the 7th day after I-131 therapy, patients underwent 7DWBS.
I-131 Whole Body Scan and SPECT/CT
I-131 whole body scan was done using a large field of view dual-head gamma camera (Millennium VG, GE, USA) with a medium-energy, parallel-hole collimator, and the photo peak was 364 keV with a 20% window. Continuous acquisition mode was used with a scanning ratio of 9 cm/s with a 1,024 × 256 matrix. Anterior and posterior views of the whole body were obtained simultaneously. Spot views of suspected sites of metastasis were done using a 256 × 256 matrix for a total of 500,000 counts.
SPECT/CT (Infinia/Hawkeye 4, GE, USA) was done in patients with I-131 uptake suspect for metastasis to rule out false-positive lesions. SPECT images were obtained at 20 s/frame with a 20% window centered at 364 keV. A 128 × 128 matrix was used with a zoom factor of 1.0. This was followed by CT acquisition using helical mode with 5-mm slice thickness, 140 kV, pitch 1.9, interval of 4.42 mm, and 2.5 mA.
Image Analysis
Each RxWBS was evaluated by visual analysis and interpreted individually. We classified I-131 uptake of metastatic lesions into three grades: no uptake, suspicious uptake, and definite uptake. Instances of definite and suspicious uptake were categorized as metastatic lesions. The final grade and interpretation were determined by consensus of two nuclear medicine physicians.
Data Analysis and Statistics
We evaluated the presence and grade of metastatic lesions on each scan. All cases were categorized into three distinct groups. Group A consisted of cases with metastasis on both 3DWBS and 7DWBS. Group B consisted of cases with metastasis on 7DWBS but not on 3DWBS. Group C consisted of cases in which metastases were absent on 3DWBS and 7DWBS, but present on FDG PET/CT.
The TSH-stimulated serum Tg level was categorized into six grades: grade I, Tg < 5 ng/mL; grade II, 5–10 ng/mL; grade III, 10–50 ng/mL; grade IV, 50–100 ng/mL; grade V, 100–500 ng/mL; and grade VI, >500 ng/mL.
A weighted kappa value was calculated to assess agreement between 3DWBS and 7DWBS and agreement between the two nuclear medicine physicians. McNemar’s test was used to compare the number of cases with lung or bone metastases on 3DWBS and 7DWBS. One-way analysis of variance was used to examine differences in ages, I-131 doses, Tg grades, and anti-Tg antibody levels among the three groups. A chi-squared test was used to examine differences in sex, metastasis site, FDG avidity, past history of I-131 therapy, use of rhTSH, and evidence of metastasis before I-131 therapy among the three groups. A p value <0.05 was considered to be statistically significant. The kappa value was interpreted as reported [18]. MedCalc statistical software was used for the analysis (MedCalc Software version 11.3.1.0, Mariakerke, Belgium. Medcalc).
Results
Patients
The characteristics of the 52 enrolled patients are described in Table 1. Among these, 37 patients had only lung metastasis, 7 patients had only bone metastasis, and 8 patients had both lung and bone metastasis. A total of 60 cases were evaluated in this study (45 cases with lung metastasis and 15 cases with bone metastasis). Lung or bone metastatic lesions had already been diagnosed in 40 patients before the current I-131 therapy.
Table 1.
Characteristics of patients (n = 52) with lung or bone metastases from well-differentiated thyroid cancer
| Patient characteristics | Number | |
|---|---|---|
| Pathology | Papillary cancer | 45 |
| Follicular cancer | 6 | |
| Hurthle cell cancer | 1 | |
| Sex | Male | 16 |
| Female | 36 | |
| Age (years) | Mean | 54.0 |
| Standard deviation | 14.2 | |
| Metastasis | No evidence of metastasis | 9 |
| Known lung metastasis | 27 | |
| Known bone metastasis | 11 | |
| Known bone and lung metastases | 2 | |
| Regional lymph node metastasis | 3 | |
| Previous I-131 therapy | None | 17 |
| Once | 11 | |
| 2 times | 13 | |
| 3 times | 7 | |
| 4 times | 3 | |
| 5 times | 1 | |
| TSH stimulation | LT4 withdrawal | 46 |
| rhTSH | 6 | |
| I-131 dose (MBq) | 5,550 | 17 |
| 6,660 | 6 | |
| 7,400 | 27 | |
| 9,250 | 2 | |
TSH Thyroid-stimulating hormone, LT4 levothyroxine, rhTSH recombinant human TSH
Inter-Observer Agreement
The two nuclear medicine physicians had very good agreement in interpreting imaging studies. The calculated weighted kappa values were 0.862 for 3DWBS and 0.942 for 7DWBS. Intra-observer agreement showed good agreement for 3DWBS (weighted kappa value 0.641) and very good agreement for 7DWBS (weighted kappa value 0.942).
In the uptake grading, the two nuclear medicine physicians had very good agreement as well. The calculated weighted kappa values were 0.846 for 3DWBS and 0.974 for 7DWBS.
Comparison of 3DWBS and 7DWBS in Detecting Lung or Bone Metastasis
3DWBS showed I-131 uptake in lung or bone metastasis in 35 out of the 60 cases (positive cases on 3DWBS). 7DWBS showed I-131 uptake in lung or bone metastasis in 50 out of the 60 cases. In 35 cases, metastatic lesions were detected on both 3DWBS and 7DWBS (group A). In 15 cases, metastatic lesions were detected only on 7DWBS (group B). In 10 cases, metastatic lesions were not shown on either 3DWBS or 7DWBS (group C). Numbers and grades are described in Tables 2 and 3. Overall, 25% more cases were detected by 7DWBS, which was statistically significant (difference 25%, 95% CI 14.1 to 25.0, p = 0.0001).
Table 2.
Distribution of I-131-avid bone and lung metastatic lesions on I-131 whole body scans on the post-therapy 3rd day (3DWBS) and 7th day (7DWBS)
| Lung metastasis (n = 45) | Bone metastasis (n = 15) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 3DWBS | 3DWBS | ||||||||
| Uptake | None | Suspicious | Definite | Total | None | Suspicious | Definite | Total | |
| 7DWBS | None | 9 | 0 | 0 | 9 (20.0%) | 1 | 0 | 0 | 1 (6.7%) |
| Suspicious | 2 | 3 | 0 | 5 (11.1%) | 0 | 0 | 0 | 0 (0%) | |
| Definite | 8 | 8 | 15 | 31 (68.9%) | 5 | 0 | 9 | 14 (93.3%) | |
| Total | 19 (42.2%) | 11 (24.4%) | 15 (33.3%) | 45 (100%) | 6 (40.0%) | 0 (0%) | 9 (60.0%) | 15 (100%) | |
Table 3.
Comparison of clinical parameters between two groups according to lesions detected by 3DWBS and/or 7DWBS
| Group A | Group B | Group C | p value | |
|---|---|---|---|---|
| Cases (n) | 35 | 15 | 10 | |
| Lung metastasis | 26 | 10 | 9 | 0.4137 |
| Bone metastasis | 9 | 5 | 1 | |
| Age (mean ± SD, years) | 54.6 ± 11.9 | 55.2 ± 14.1 | 54.8 ± 15.0 | 0.9320 |
| Sex (n) | ||||
| Male | 13 | 3 | 3 | 0.4864 |
| Female | 22 | 12 | 7 | |
| History of I-131 therapy (n) | ||||
| Yes | 21 | 7 | 10 | 0.0207 |
| No | 14 | 8 | 0 | (0.5758a, 0.0431b) |
| Evidence of metastasis before I-131 therapy (n) | ||||
| Yes | 32 | 8 | 10 | 0.0012 |
| No | 3 | 7 | 0 | (0.0069a, 0.8107b) |
| I-131 Doses (mean ± SD, MBq ) | 6,941.2 ± 1,021.2 | 6,560.1 ± 1,132.2 | 6,993.0 ± 625.4 | 0.4730 |
| TSH stimulation (n) | ||||
| LT4 withdrawal | 34 | 13 | 6 | 0.0053 |
| Recombinant human TSH | 1 | 2 | 4 | (0.4356a, 0.0064b) |
| TSH (mean ± SD, μIU/ml) | 70.5 ± 18.4 | 72.0 ± 19.1 | 56.7 ± 32.7 | 0.4050 |
| Serum Tg (median and interquartile range, ng/mL) | 372.0 (49.5–781.3) | 22.0 (7.25–65.5) | 65.0 (28.8–547.0) | |
| Grade of serum Tgd | ||||
| Grade I | 0 | 3 | 0 | 0.0030 |
| Grade II | 2 | 2 | 0 | 0.2330c |
| Grade III | 3 | 6 | 2 | |
| Grade IV | 4 | 1 | 2 | |
| Grade V | 1 | 1 | 4 | |
| Grade IV | 5 | 2 | 2 | |
| Serum anti-Tg antibody (median and interquartile range, U/mL) | 197.1 (33.0–182.0) | 40.0 (18.8–98.2) | 58.5 (45.9–82.0) | 0.7130 |
| F-18 FDG PET/CT examination (+) | 32 | 12 | 10 | |
| FDG avid | 15 | 5 | 7 | 0.3573 |
| Non-FDG avid | 17 | 7 | 3 | |
| Macronodular/micronodular metastasis (lung) e | 12/12 | 2/7 | 2/7 | 0.1859 |
RxWBS Post-therapy I-131 whole body scan, 3DWBS post-therapy 3rd day I-131 whole body scan, 7DWBS post-therapy 7th day I-131 whole body scan, Tg thyroglobulin
Group A Metastasis present on both 3DWBS and 7DWBS, group B metastasis present on 7DWBS but not on 3DWBS, group C cases in which metastasis was confirmed but I-131 uptake was not shown on RxWBS
aBetween groups A and B
bBetween groups A and C
cBetween cases with previous I-131 ablation history
dThyroglobulin grade (TSH-stimulated, described in section “Materials and Methods”)
eAmong cases for which chest CT was available
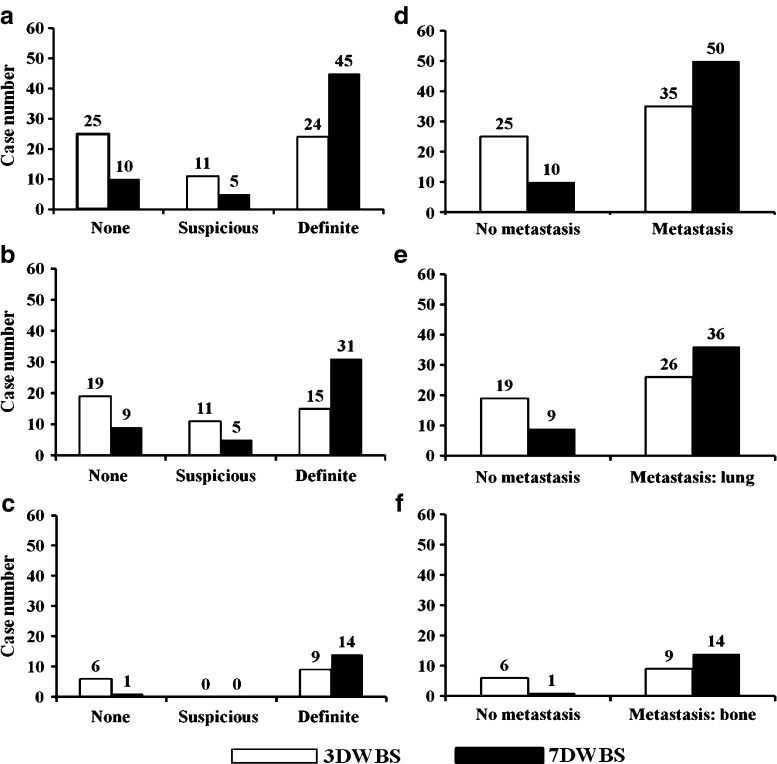
In grading of I-131 uptake, there was moderate agreement between 3DWBS and 7DWBS (kappa value: 0.464, 95% CI 0.257 to 0.671) (Fig. 1). The number of cases with definite uptake was higher on 7DWBS, while the number of cases with suspicious uptake was higher on 3DWBS.
Fig. 1a-f.
Comparison of the number of lesions between 3DWBS and 7DWBS. a–c Differences in grading (none, suspicious and definite) of I-131 uptake. d–f Differences in results (no metastasis or metastasis) of whole-body scan. Suspicious and definite uptake cases were considered metastatic disease. a and d All cases (lung and bone metastases). b and e Lung metastasis. c and f Bone metastasis. Abbreviation: 3DWBS, post-therapy 3rd Day I-131 Whole Body Scan; 7DWBS, Post-therapy 7th Day I-131 Whole Body Scan; n, number
Comparison of Lung Metastasis
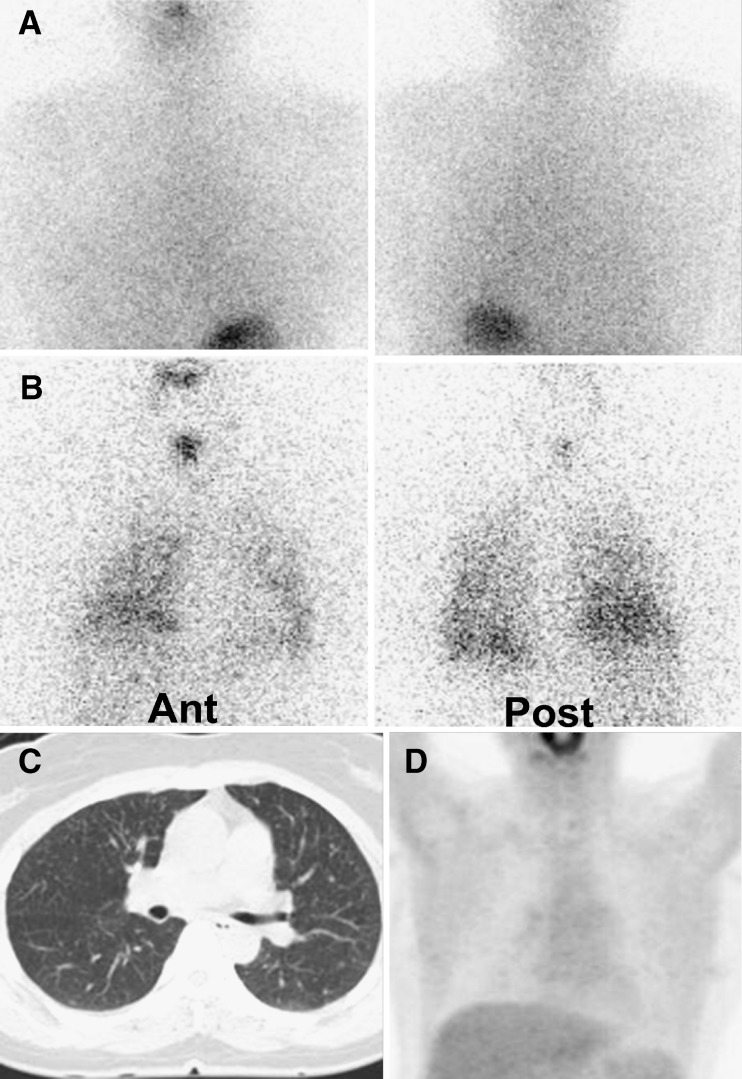
Twenty-six cases of lung metastases were detected on both 3DWBS and 7DWBS (Fig. 2). Additionally, 7DWBS detected 10 cases that were negative on 3DWBS. Overall, 22.2% more cases were detected on 7DWBS than on 3DWBS (95% CI 8.51 to 22.22, p = 0.002). Nine cases were not detected on either 3DWBS or 7DWBS. Numbers and grades are described in Table 2.
Fig. 2a-d.
I-131 3rd and 7th day post-therapy whole body scans, chest CT, and F-18 FDG PET/CT findings in a patient with lung metastasis. A 44-year-old female underwent high-dose I-131 therapy (7,400 MBq) for lung metastasis from papillary thyroid cancer. She received a second treatment (7,400 MBq) because of a sustained high level of serum thyroglobulin. a There was no definite I-131 uptake on the post-therapy 3rd day whole body scan. b However, diffuse I-131 accumulations in both the lungs and focal I-131 uptake in the lower anterior neck were shown on the post-therapy 7th day whole body scan. c Chest CT showed multiple, tiny nodules in both lung fields. d MIP image of F-18 FDG PET revealed no FDG-avid lesions in the lungs. Her serum thyroglobulin (TSH-stimulated) level decreased to 414 from 610 ng/mL 1 year after her second treatment
Chest CT images were obtained in 24 cases in group A, 9 cases in group B, and 9 cases in group C. Macronodular metastases (>1 cm) were seen in 12 cases in group A, 2 cases in group B, and 2 cases in group C (Table 3). The other three cases did not undergo PET/CT or CT.
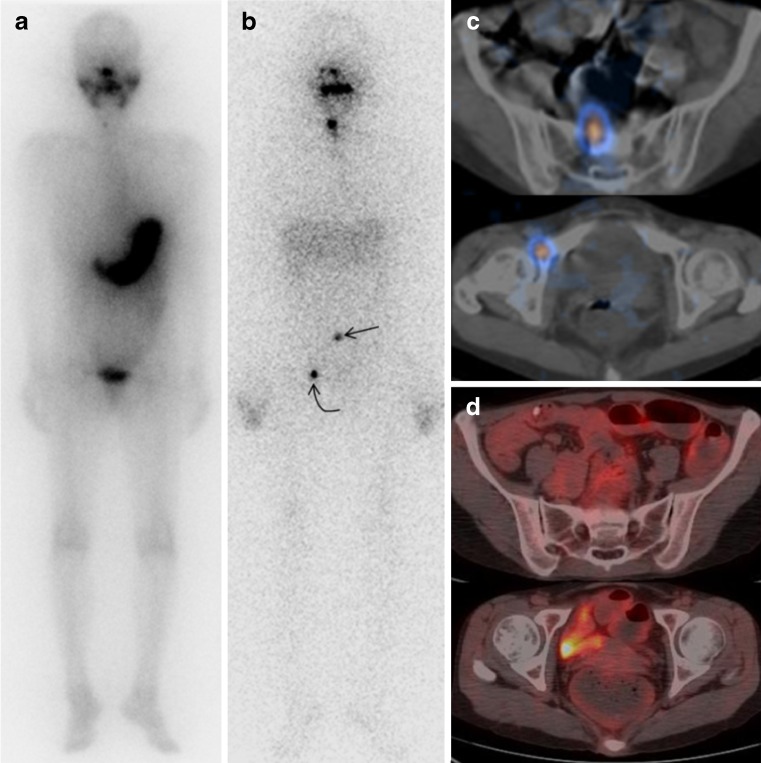
Comparison of Bone Metastasis
Nine cases of bone metastasis were detected on both 3DWBS and 7DWBS (Fig. 3). Additionally, 7DWBS detected five cases that were negative on 3DWBS. Overall, 33.3% more cases were detected on 7DWBS than on 3DWBS (95% CI −1.45 to 33.33, p = 0.0625). One case was not detected on either 3DWBS or 7DWBS. Numbers and grades are described in Table 2.
Fig. 3a-d.
I-131 3rd and 7th day post-therapy whole body scans and I-131 SPECT/CT findings in a patient with bone metastasis. A 40-year-old female underwent a total thyroidectomy for papillary thyroid cancer. a Post-therapy 3rd day whole body scan performed after therapy with 5,550 MBq of I-131 showing only focal I-131 uptake in the right thyroidectomy bed. b However, on the post-therapy 7th day whole body scan, focal areas of uptake were detected in the lower posterior back (straight arrow) and right pelvic area (bent arrow). c Post-therapy 7th day I-131 pelvic SPECT/CT also revealed I-131 accumulations in the sacrum (orange-colored lesion in upper image) and the right pelvic bone (orange-colored lesion in lower image). d On F-18 FDG PET/CT, there was no definite hypermetabolism in the sacrum (upper image) or right pelvic bone (lower image)
The sites of bone metastasis in group A included vertebra (n = 1), rib (n = 1), humerus (n = 1), pelvic bone (n = 1), sacrum (n = 1), sternum and sacrum (n = 1), pelvic bone and vertebra (n = 1), pelvic bone and sacrum (n = 1), multiple sites (vertebra, pelvic bone, and femur, n = 1). The sites of metastasis in group B were sternum (n = 1), pelvic bone (n = 1), vertebra (n = 1), humerus (n = 1), pelvic bone and vertebra (n = 1). The site of metastasis in group C was the lumbar vertebra.
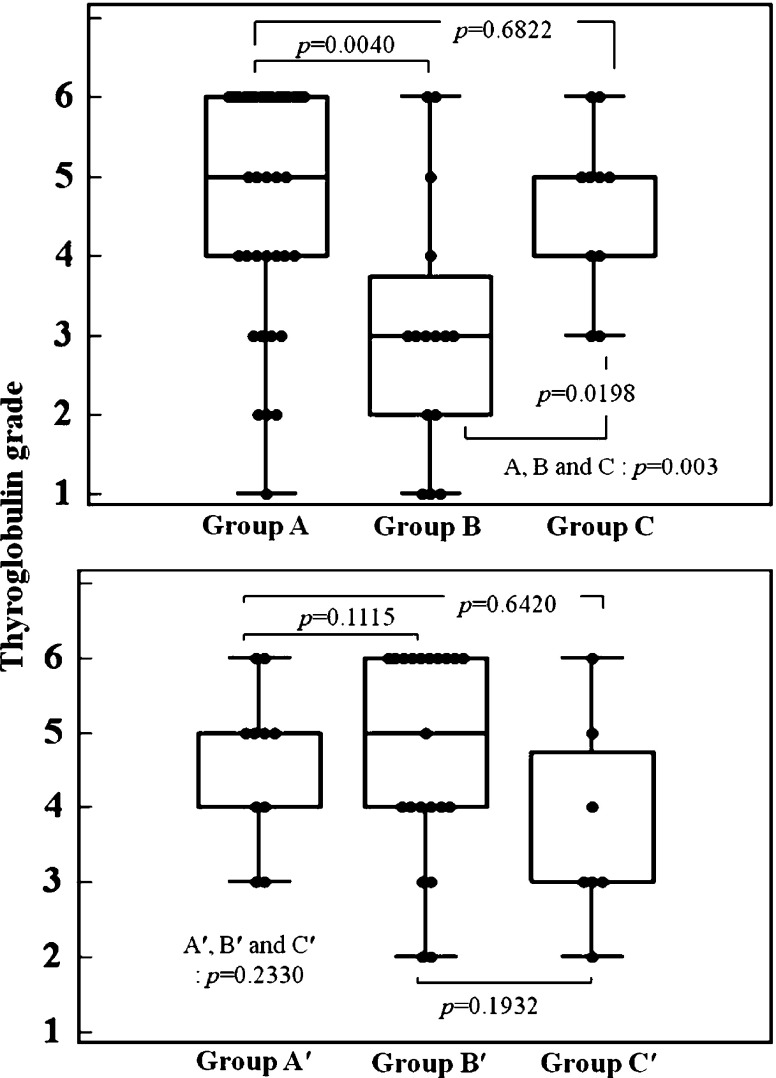
Comparison of Clinical Parameters Among Groups A, B, and C
The clinical features are described in Table 3. The serum Tg level (TSH-stimulated) was higher in group A than in group B (p = 0.0040), but comparable with group C (p = 0.6822) (Fig. 4). However, after excluding cases without a history of I-131 therapy, there was no statistically significant difference in serum Tg level among groups A, B, and C (p = 0.1115, Fig. 4). The number of cases with a prior history of metastasis before I-131 therapy was also higher in group A than in group B (p = 0.0069). However, there was no significant difference in prior history of metastasis between groups A and C (p = 0.8107) (Table 3).
Fig. 4.
Comparison of the serum thyroglobulin level among groups. Each dot represents the TSH-stimulated serum thyroglobulin grade in each case. Upper panel Group A includes cases that were detected on both the 3rd day post-therapy I-131 whole body scan (3DWBS) and the 7th day post-therapy I-131 whole body scan (7DWBS). Group B includes cases that were missed on 3DWBS but detected on 7DWBS. Group C includes cases that were not detected on either 3DWBS or 7DWBS. Groups A and C showed a higher thyroglobulin (Tg) grade than group B (p = 0.0041 and p = 0.0198, respectively). Lower panel Groups A′, B′, and C′ represent cases of groups A, B, and C after excluding cases without a history of I-131 therapy. There was no significant difference in serum Tg grade among groups A′, B′, and C′.Abbreviation: 3DWBS, post-therapy 3rd Day I-131 Whole Body Scan; 7DWBS, Posttherapy 7th Day I-131 Whole Body Scan; n, number; Tg, thyroglobulin. Classification of thyroglobulin grade is as follows: grade I, thyroglobulin below 5 ng/mL; grade II, 5 ~ 10 ng/mL; grade III, 10 ~ 50 ng/mL; grade IV, 50 ~ 100 ng/mL; grade V, 100 ~ 500 ng/mL and grade VI, > 500 ng/mL
A history of previous I-131 therapy and use of rhTSH showed no significant difference between groups A and B (p = 0.5758 and p = 0.4356, respectively). All other parameters including age, sex, I-131 doses, location of metastasis, serum anti-Tg antibody level, FDG avidity of the lesion and macro- or micronodularity of lung metastasis showed no significant differences among the groups.
Discussion
The major finding in this study was that 7DWBS could detect more I-131-avid lung or bone metastastic lesions than 3DWBS in patients with thyroid cancer. If the patients had only 3DWBS without 7DWBS, 25% (15/60) of distant metastasis would have been missed. In the absence of prediagnosed metastatic lesions before RxWBS, 7DWBS was more effective in detecting metastatic lesions than 3DWBS (p = 0.0045, Table 3). Furthermore, 7DWBS detected more cases of definite uptake and fewer cases of suspicious uptake than 3DWBS. In our study (Fig. 1), the number of cases with suspicious uptake decreased from 11 (3DWBS) to 5 (7DWBS). The number of cases with definite metastatic uptake increased from 24 (3DWBS) to 45 (7DWBS). Suspicious uptake can be equivocally interpreted by nuclear medicine physicians with less experience, resulting in disagreement between readers. In our study, interobserver agreement in uptake grading was higher in 7DWBS than 3DWBS. This suggests that 7DWBS can be of additional value when an equivocal lesion is seen on 3DWBS.
Khan et al. reported similar results in 18 patients. They conducted scans at 2 days and 7 days post-therapy after 3.7–5.6 GBq of I-131 administration [19]. (Note: 2-day and 7-day post-therapeutic scans correspond to 3DWBS and 8DWBS, respectively, in the current study.) They reported a higher sensitivity for detection of iodine-avid tissue on 8DWBS than on 3DWBS. Although they performed 8DWBS (1 day later than our 7DWBS), their results support our current study by suggesting that 3DWBS has a lower sensitivity than the delayed scans.
Hung et al. analyzed RxWBS at three different time points (first scan performed 3–4 days, second scan 5–6 days, and third scan 10–11 days after I-131 therapy) [17]. (Note: post-therapy scans 3–4 and 5–6 days after I-131 administration correspond to 4–5DWBS and 6–7DWBS, respectively, in the current study.) They reported no difference between 4–5DWBS and 6–7DWBS, which does not directly correspond to our results. However, our first scan was 1–2 days earlier than their first scan (3DWBS vs. 4–5DWBS) and this may be the reason for the differences between the study results. Hung et al. also reported “early wash-out” cases in their study [17], which they defined as a loss of detection of I-131 accumulation on their third scan (11–12DWBS). They reported that 17% of lung metastases and 16% of bone metastases were missed on the 11–12DWBS. Since we did not perform RxWBS later than the 7th day after radioiodine therapy, we cannot directly compare our results with their later scans.
Serum Tg is known to correlate with tumor burden and disease extent [20]. We found a significant difference in serum Tg level (TSH-stimulated) between groups A and B (p < 0.0045, Fig. 4). However, this difference became statistically insignificant when we excluded cases without a previous history of I-131 therapy (group A′ and B′ in Fig. 4, p = 0.1115). The difference in serum Tg level between groups A and B may be due to remnant thyroid tissue in patients who did not undergo previous ablation therapy.
In contrast to the cases of lung metastasis, the cases of bone metastasis showed no statistically significant difference between 3DWBS and 7DWBS (p = 0.0625), which may be explained by the small number of cases (n = 14). However, the fact that there was no diagnosis of “suspicious uptake” on either 3DWBS or 7DWBS was a key difference in grading between bone metastasis and lung metastasis (Fig. 1c). Lesions were categorized as either no or definite uptake in all cases of bone metastasis. In contrast, there were 11 lung metastasis cases with suspicious uptake on 3DWBS (Fig. 1b). The number of cases with suspicious uptake decreased to five on 7DWBS. The reason for this difference between lung and bone metastasis is not clear. Further evaluation is needed.
The reason for the difference in I-131 accumulation between 3DWBS and 7DWBS is not clear. As reported by Coakley et al., one possible explanation could be the further acquisition of I-131 by malignant cells or an improvement of target-to-background ratios or a combination of both [21]. Chung et al. reported that the relatively well-differentiated papillary carcinomas have higher levels of sodium iodide symporter (NIS), pendrin, Tg expression, and a lower level of GLUT-1 expression than the relatively less differentiated tumors [22]. Since the number of FDG-avid lesions was not significantly different between groups A and B (41.7 vs. 46.9%, p = 0.98), cellular differentiation may play a role in retention of I-131 in the metastatic lesions. Further pathological studies are required to elucidate the relationship between the degree of tumor differentiation and patterns of I-131 retention.
There are several limitations to our study. First, we only selected patients with lung or bone metastases. Second, we applied the same protocol in patients who achieved TSH stimulation by LT4 withdrawal and by rhTSH. A shorter interval after I-131 therapy (2–5 days after treatment) is recommended for RxWBS in patients treated with rhTSH [21]. However, only three patients (two in group A, one in group B) used rhTSH in our study, thus the influence of rhTSH is limited. Third, we did not perform RxWBS later than the 7th day after radioiodine therapy. Fourth, pathologic correlation such as of biochemical markers was not done. In spite of these limitations, the current study is valuable because the results may be useful in establishing the optimal time for RxWBS. We demonstrated that 7DWBS detects more I-131-avid metastatic lesions than 3DWBS. These findings are important because without optimal timing for RxWBS, the I-131-avid lesions can be missed. Such cases might be considered as “Tg-positive and scan false-negative” cases. Larger studies with a variety of time intervals are needed to confirm the appropriate time for RxWBS.
Conclusion
7DWBS showed more I-131-avid lung or bone metastatic lesions than 3DWBS in patients with well-differentiated thyroid cancer. In our study, 3DWBS missed 25% of cases that could be detected on 7DWBS. Routine scanning on the 7th day after high-dose I-131 therapy should be considered regardless of the findings on 3DWBS.
Acknowledgments
Conflict of interest
None.
References
- 1.Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–1214. doi: 10.1089/thy.2009.0110. [DOI] [PubMed] [Google Scholar]
- 2.Schlumberger M, Tubiana M, De Vathaire F, Hill C, Gardet P, Travagli JP, et al. Long-term results of treatment of 283 patients with lung and bone metastases from differentiated thyroid carcinoma. J Clin Endocrinol Metab. 1986;63:960–967. doi: 10.1210/jcem-63-4-960. [DOI] [PubMed] [Google Scholar]
- 3.Casara D, Rubello D, Saladini G, Gallo V, Masarotto G, Busnardo B. Distant metastases in differentiated thyroid cancer: long-term results of radioiodine treatment and statistical analysis of prognostic factors in 214 patients. Tumori. 1991;77:432–436. doi: 10.1177/030089169107700512. [DOI] [PubMed] [Google Scholar]
- 4.Samaan NA, Schultz PN, Haynie TP, Ordonez NG. Pulmonary metastasis of differentiated thyroid carcinoma: treatment results in 101 patients. J Clin Endocrinol Metab. 1985;60:376–380. doi: 10.1210/jcem-60-2-376. [DOI] [PubMed] [Google Scholar]
- 5.Mazzaferri EL, Kloos RT. Clinical review 128: current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab. 2001;86:1447–1463. doi: 10.1210/jc.86.4.1447. [DOI] [PubMed] [Google Scholar]
- 6.Mazzaferri EL. Treatment of carcinoma of follicular epithelium. In: Ingbar SH, Braverman LE, editors. The thyroid: a fundamental and clinical text. 5. Philadelphia: J. B. Lipincott; 1986. p. 1331. [Google Scholar]
- 7.Amdur RJ, Mazzaferri EL (2005) The value of a post treatment whole body scan. In Amdur RJ, Mazzaferri EL, editors. Essentials of thyroid cancer management. New York: Springer, pp 65–8
- 8.Souza Rosário PW, Barroso AL, Rezende LL, Padrão EL, Fagundes TA, Penna GC, et al. Post I-131 therapy scanning in patients with thyroid carcinoma metastases: an unnecessary cost or a relevant contribution? Clin Nucl Med. 2004;29:795–798. doi: 10.1097/00003072-200412000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Becker D, Charkes ND, Dworkin H, Hurley J, McDougall IR, Price D, et al. Procedure guideline for extended scintigraphy for differentiated thyroid cancer: 1.0. J Nucl Med. 1996;37:1269–1271. [PubMed] [Google Scholar]
- 10.Luster M, Clarke SE, Dietlein M, Lassmann M, Lind P, Oyen WJ, et al. Guidelines for radioiodine therapy of differentiated thyroid cancer. Eur J Nucl Med Mol Imaging. 2008;35:1941–1959. doi: 10.1007/s00259-008-0883-1. [DOI] [PubMed] [Google Scholar]
- 11.Nĕmec J, Röhling S, Zamrazil V, Pohunková D. Comparison of the distribution of diagnostic and thyroablative I-131 in the evaluation of differentiated thyroid cancers. J Nucl Med. 1979;20:92–97. [PubMed] [Google Scholar]
- 12.Cholewinski SP, Yoo KS, Klieger PS, O'Mara RE. Absence of thyroid stunning after diagnostic whole-body scanning with 185 MBq 131I. J Nucl Med. 2000;41:1198–1202. [PubMed] [Google Scholar]
- 13.Min JJ, Chung JK, Lee YJ, Jeong JM, Lee DS, Jang JJ, et al. Relationship between expression of the sodium/iodide symporter and 131I uptake in recurrent lesions of differentiated thyroid carcinoma. Eur J Nucl Med. 2001;28:639–645. doi: 10.1007/s002590100509. [DOI] [PubMed] [Google Scholar]
- 14.Durante C, Haddy N, Baudin E, Leboulleux S, Hartl D, Travagli JP, et al. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab. 2006;91:2892–2899. doi: 10.1210/jc.2005-2838. [DOI] [PubMed] [Google Scholar]
- 15.Mazzaferri EL. Empirically treating high serum thyroglobulin levels. J Nucl Med. 2005;46:1079–1088. [PubMed] [Google Scholar]
- 16.Hindié E, Mellière D, Lange F, Hallaj I, de Labriolle-Vaylet C, Jeanguillaume C, et al. Functioning pulmonary metastases of thyroid cancer: does radioiodine influence the prognosis? Eur J Nucl Med Mol Imaging. 2003;30:974–981. doi: 10.1007/s00259-003-1174-5. [DOI] [PubMed] [Google Scholar]
- 17.Hung BT, Huang SH, Huang YE, Wang PW. Appropriate time for post-therapeutic I-131 whole body scan. Clin Nucl Med. 2009;34:339–342. doi: 10.1097/RLU.0b013e3181a345be. [DOI] [PubMed] [Google Scholar]
- 18.Altman D. Practical statistics for medical research. 1. London: Chapman & Hall/CRC; 1991. pp. 403–407. [Google Scholar]
- 19.Khan S, Waxman A, Nagaraj N, Braunstein G (1994) Optimization of post ablative I-131 scintigraphy: comparison of 2 day vs. 7 day post therapy study in patients with differentiated thyroid cancer (DTC). J Nucl Med 35:15
- 20.Bachelot A, Cailleux AF, Klain M, Baudin E, Ricard M, Bellon N, et al. Relationship between tumor burden and serum thyroglobulin level in patients with papillary and follicular thyroid carcinoma. Thyroid. 2002;12:707–711. doi: 10.1089/105072502760258686. [DOI] [PubMed] [Google Scholar]
- 21.Coakley AJ, Page CJ, Croft D. Scanning dose and detection of thyroid metastases. J Nucl Med. 1980;21:803–804. [PubMed] [Google Scholar]
- 22.Chung JK, Youn HW, Kang JH, Lee HY, Kang KW. Sodium iodine symporter and the radioiodine treatment of thyroid carcinoma. Nucl Med Mol Imaging. 2010;44:4–14. doi: 10.1007/s13139-009-0016-1. [DOI] [PMC free article] [PubMed] [Google Scholar]