Abstract
A 53-year-old man with fever of unknown origin underwent F-18 fluorodeoxyglucose positron emission tomography/computed tomography (F-18 FDG PET/CT) as a workup for a fever of unknown origin. On presentation, he complained of fever, chills, and myalgia. The F-18 FDG PET/CT scan showed diffusely increased uptake of the liver with mild hepatomegaly. A liver biopsy then revealed fibrin-ring granulomas typically seen in Q fever. The patient was later serologically diagnosed as having acute Q fever as the titers for C. burnetii IgM and IgG were 64:1 and 16:1, respectively. He recovered completely following administration of doxycycline. This indicates that F-18 FDG PET/CT may be helpful for identifying hepatic involvement in Q fever as a cause of fever of unknown origin.
Keywords: Q fever, F-18 FDG PET/CT, Fever of unknown origin
Introduction
Q fever, a zoonosis caused by Coxiella burnetii, an obligate, intracellular, gram-negative organism, is seen throughout the world. Q fever infects a variety of hosts, including humans, ruminants (cattle, sheep, and goats), pets, and, rarely, reptiles, birds, and ticks. Humans are exposed to the disease as other animals shed the organism in feces, urine, milk, and products of conception [1]. Presentation of the disease is extremely variable and infection may lead to asymptomatic seroconversion, acute disease (ranging from flu-like syndrome to severe pneumonia requiring intensive care) or chronic infection (manifesting primarily as endocarditis) [2]. The diagnosis is mainly based on serologic testing, and the treatment of choice is 100 mg oral doxycycline every 12 h for 14 days. Decreased efficacy of therapy has been reported when treatment was not initiated within a week of the symptom onset [1]; however, the variability of the clinical expression often causes delayed diagnosis in the clinical setting. We report a case of acute Q fever, showing diffusely increased uptake by the liver of F-18 FDG on PET/CT scan, and which provides a clue in order to reach an early diagnosis and initiate treatment.
Case Report
A 53-year-old, previously healthy man was referred to a physician for the evaluation and treatment of fever. He complained of striking fever, chills, and pain in both buttocks that had started 5 days earlier. His past medical history was unremarkable. He did not drink or take any herbal medicine. He smoked occasionally. He had not suffered any previous trauma and had never travelled abroad. He worked in a market as a fruit dealer. Upon physical examination, his body temperature was 38.5°C, his pulse rate was 84/min, his respiratory rate was 18/min, and his blood pressure was 117/78 mmHg. Upon neurologic examination, there were no focal neurologic or diffuse meningeal irritation signs. Both scleras were anicteric. His heart beat was regular without murmur, and his breathing sound was clear. Diffuse epigastric tenderness, but no rebounding tenderness, was noted in the abdomen. There was no pitting edema. Laboratory tests revealed a normal range of white blood cell count, hemoglobin and decreased platelets (139,000/mm3). Liver function test showed an elevated alanine transaminase (ALT) of 206 IU/l, aspartic acid transaminase (AST) of 153 IU/l, alkaline phosphatase of 213 IU/l, total bilirubin of 1.4 mg/dl, and a normal range of albumin and creatinine . The prothrombin time (PT INR) and activated partial thrombin time (aPTT) were within the normal range. The C-reactive protein was elevated (15.64 mg/dl). A serology test for hepatitis A, B, C, and E was negative. Test for Epstein-Barr virus (EBV) and Cytomegalovirus were negative. Antibodies for human immunodeficiency virus type 1 (HIV-1) and VDRL were negative. A test for antimitochondrial antibodies, antinuclear antibodies, and anti-smooth-muscle antibody was negative. A chest X-ray on his first day of hospitalization was normal. Abdominal computed tomography (CT) revealed fatty liver disease and small hemagiomas (Fig. 1). There was no growth in the blood cultures. An electrocardiogram was normal. To clarify the origin of his fever, F-18 FDG PET/CT was performed 2 weeks after his symptoms had started. F-18 FDG-PET/CT images of the skull base to the mid-thigh exhibited diffusely increased uptake by the liver and the mean standardized uptake value (SUV) was 2.7 (Fig. 2). Abnormally increased uptake was also noted in the right pulmonary hilar and left interlobar LNs, and which was considered as benign reactive hyperplasia. Under the impression of possible infiltrative liver disease which is associated with fever of unknown origin, a percutaneous liver biopsy was done. Pathology examination revealed multiple, fibrin-ring granulomas characterized by a central, round, clear space surrounded by an eosinophilic fibrin ring and infiltrated by histiocytes, lymphocytes, and neutrophils (Fig. 3). And no acid-fast bacilli were identified on Ziehl-Neelsen stain. No positive cells were observed by EBV in situ hybridization or CMV immunostaining. Although no exposure to wild animals or their products was identified by reviewing his history, a serologic test for C. burnetii immunoglobulin M (IgM) and G (IgG) was performed. An empirical therapeutic trial was also done by administering 200 mg doxycycline daily for 2 weeks. The patient’s fever decreased and he was then discharged. On the subsequent reports of the serologic test, there was significant rise in the titers of IgM and IgG antibodies against C. burnetii as 64:1 and 16:1, respectively. This indicated recent, acute Q fever by recent infection of C. burnetii. Three weeks following his discharge, the patient visited the out-patient clinic, his liver function tests were normal, and he had completely recovered.
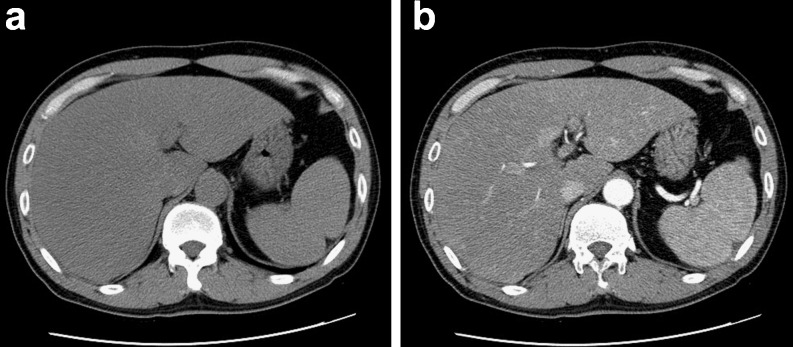
Fig. 1.
There were no hepatic masses or parenchymal abnormalities on non-enhanced (a)/enhanced (b) CT scans except small hemangiomas (not seen on these images)
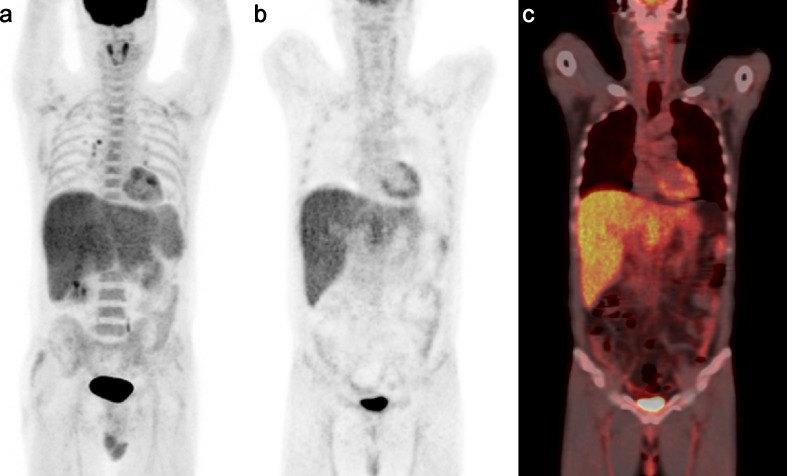
Fig. 2.
MIP (a) image of F-18 FDG PET/CT, coronal PET (b), and fusion PET/CT (c) images shows a diffusely increased F-18 FDG uptake in the liver (max SUV 4.0, mean SUV 2.7) with mild hepatomegaly
Fig. 3.
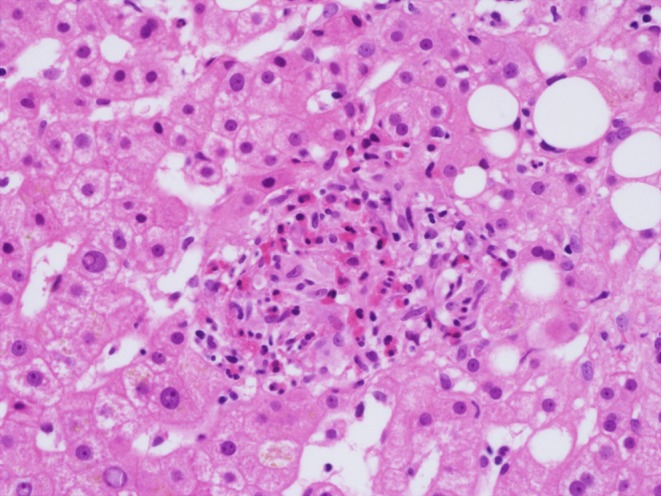
The percutaneous liver biopsy sample demonstrates distinctive, fibrin-ring granulomas showing central lipid cores, an eosinophilic ring of fibrin, and a mixed infiltrate of histiocytes, lymphocytes, and neutrophils (H & E, ×400)
Discussion
This case study demonstrates that F-18 FDG PET/CT scan can be helpful in identifying and localizing the cause. In this patient, it demonstrated diffusely increased F-18 FDG uptake of the liver as seen on F-18 FDG PET/CT scan, which was important for making an early diagnosis of his Q-fever by suggesting the need for further invasive diagnostic procedures such as a biopsy.
Diffusely increased hepatic F-18 FDG uptake seen on F-18 FDG PET scan has been reported in malignant lymphoma, tuberculosis, hepatic angiocarcoma, and infiltrative hepatocellular carcinoma [3–6]. To exclude such critical diseases, a percutaneous liver biopsy should be performed.
The result of the biopsy showed fibrin-ring granulomas. The granulomas of Q fever are histologically characterized by a clear central space with a fibrinoid type of ring, which is consistent with the biopsy specimen of this patient. Although this type of granuloma is thought to be characteristic of Q fever hepatitis [7], it is not pathognomic. It has also been described in patients with leishmaniasis, infectious mononucleosis, giant-cell arthritis, and allopurinol hypersensitivity [8–11]. Furthermore, it has also recently been reported in acute hepatitis A and in chronic hepatitis C [12, 13]. Although those diseases have been ruled out by laboratory results and careful review of the patient’s history, a serologic test is needed. This patient’s diagnosis was subsequently confirmed by the detection of C. burnetii IgM and IgG antibodies in the serum.
It is true that the pathogenic mechanisms and interaction of C. burnetii with the host’s immune systems are still poorly understood; however, the hematogenous spread of C. burnetii results in infection of the liver, spleen, bone marrow, and reproductive tract, thus causing the formation of granulomatous lesions [14]. This can explain why the F-18 FDG PET/CT scan showed the increased hepatic F-18 FDG uptake that we observed. High rates of glucose utilization by the infected hepatocytes involved in the pathogenesis of Q fever might also explain our findings.
There have been several previous reports regarding the findings of Q fever on F-18 FDG PET and which demonstrated a vascular graft infection [15], bone marrow infiltration [16], and lymphadenopathy [17] because of Q fever. Almost all of these patients presented with fever of unknown origin (FUO), as seen in this case. However, to our knowledge, this is the first case which shows diffuse hepatic uptake on F-18 FDG PET/CT as a manifestation of acute Q fever.
Although, varying degrees of hepatitis have been reported in 9.0–67% of the endemic area as a manifestation of Q fever [18], non-specific findings of hepatitis, such as a mild elevation of liver enzymes and hepatomegaly, have often delayed the diagnosis and initiation of treatment. Such a delay can then decrease the efficacy of therapy and lead to serious complications such as endocarditis, encephalitis, and osteomyelitis [1]. However, in this case, identifying the involvement of the liver on F-18 FDG PET/CT made an early diagnosis possible.
In general, the use of F-18 FDG PET imaging as a tool for evaluating patients with FUO is reserved for cases in which the initial evaluation remains negative. We report, however, a case of acute Q fever with diffuse hepatic uptake of F-18 FDG on PET/CT as an example of the early use of F-18 FDG PET/CT to make an early diagnosis. As this case demonstrates, early identification and precise localization of the cause for FUO are important for guiding subsequent invasive diagnostic procedures and for prompt initiation of appropriate treatment, which has a significant impact on successful patient care [19].
References
- 1.Parker NR, Barralet JH, Bell AM. Q fever. Lancet. 2006;367:679–688. doi: 10.1016/S0140-6736(06)68266-4. [DOI] [PubMed] [Google Scholar]
- 2.Raoult D, Tissot-Dupont H, Foucault C, Gouvernet J, Fournier PE, Bernit E, et al. Q fever 1985-1998. Clinical and epidemiologic features of 1,383 infections. Medicine (Baltimore) 2000;79:109–123. doi: 10.1097/00005792-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Basu S, Nair N. Unusually elevated liver radioactivity on F-18 FDG PET in Hodgkin’s disease: hepatic ‘superscan’. Clin Nucl Med. 2004;29:626–628. doi: 10.1097/00003072-200410000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Jeong YJ, Sohn MH, Lim ST, Kim DW, Jeong HJ, Chung MJ, et al. ‘Hot liver’ on 18F-FDG PET/CT imaging in a patient with hepatosplenic tuberculosis. Eur J Nucl Med Mol Imaging. 2010;37:1618–1619. doi: 10.1007/s00259-010-1477-2. [DOI] [PubMed] [Google Scholar]
- 5.Oe A, Habu D, Kawabe J, Torii K, Kawamura E, Kotani J, et al. A case of diffuse hepatic angiosarcoma diagnosed by FDG-PET. Ann Nucl Med. 2005;19:519–521. doi: 10.1007/BF02985582. [DOI] [PubMed] [Google Scholar]
- 6.Trojan J, Schroeder O, Raedle J, Baum RP, Herrmann G, Jacobi V, et al. Fluorine-18 FDG positron emission tomography for imaging of hepatocellular carcinoma. Am J Gastroenterol. 1999;94:3314–3319. doi: 10.1111/j.1572-0241.1999.01544.x. [DOI] [PubMed] [Google Scholar]
- 7.Cone LA, Curry N, Shaver P, Brooks D, DeForge J, Potts BE. Q fever in the Southern California desert: epidemiology, clinical presentation and treatment. Am J Trop Med Hyg. 2006;75:29–32. doi: 10.4269/ajtmh.2006.75.1.0750029. [DOI] [PubMed] [Google Scholar]
- 8.Moreno A, Marazuela M, Yebra M, Hernandez MJ, Hellin T, Montalban C, et al. Hepatic fibrin-ring granulomas in visceral leishmaniasis. Gastroenterology. 1988;95:1123–1126. doi: 10.1016/0016-5085(88)90192-8. [DOI] [PubMed] [Google Scholar]
- 9.Nenert M, Mavier P, Dubuc N, Deforges L, Zafrani ES. Epstein-Barr virus infection and hepatic fibrin-ring granulomas. Hum Pathol. 1988;19:608–610. doi: 10.1016/S0046-8177(88)80215-6. [DOI] [PubMed] [Google Scholar]
- 10.de Bayser L, Roblot P, Ramassamy A, Silvain C, Levillain P, Becq-Giraudon B. Hepatic fibrin-ring granulomas in giant cell arteritis. Gastroenterology. 1993;105:272–273. doi: 10.1016/0016-5085(93)90036-c. [DOI] [PubMed] [Google Scholar]
- 11.Vanderstigel M, Zafrani ES, Lejonc JL, Schaeffer A, Portos JL. Allopurinol hypersensitivity syndrome as a cause of hepatic fibrin-ring granulomas. Gastroenterology. 1986;90:188–190. doi: 10.1016/0016-5085(86)90092-2. [DOI] [PubMed] [Google Scholar]
- 12.Yamamoto T, Ishii M, Nagura H, Miyazaki Y, Miura M, Igarashi T, et al. Transient hepatic fibrin-ring granulomas in a patient with acute hepatitis A. Liver. 1995;15:276–279. doi: 10.1111/j.1600-0676.1995.tb00685.x. [DOI] [PubMed] [Google Scholar]
- 13.Glazer E, Ejaz A, Coley CJ, 2nd, Bednarek K, Theise ND. Fibrin ring granuloma in chronic hepatitis C: virus-related vasculitis and/or immune complex disease? Semin Liver Dis. 2007;27:227–230. doi: 10.1055/s-2007-979473. [DOI] [PubMed] [Google Scholar]
- 14.Woldehiwet Z. Q fever (coxiellosis): epidemiology and pathogenesis. Res Vet Sci. 2004;77:93–100. doi: 10.1016/j.rvsc.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 15.van Assen S, Houwerzijl EJ, van den Dungen JJ, Koopmans KP. Vascular graft infection due to chronic Q fever diagnosed with fusion positron emission tomography/computed tomography. J Vasc Surg. 2007;46:372. doi: 10.1016/j.jvs.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Alwis L, Balan K, Wright P, Lever A, Carmichael A. Bone marrow involvement in Q fever–detection by fluorine-18-labelled fluorodeoxyglucose PET. Lancet Infect Dis. 2009;9:718. doi: 10.1016/S1473-3099(09)70113-6. [DOI] [PubMed] [Google Scholar]
- 17.Takanami K, Kaneta T, Tamada T, Yamada T, Higano S, Yamada S, et al. Q fever with lymphadenopathy on F-18 FDG PET. Clin Nucl Med. 2008;33:436–437. doi: 10.1097/RLU.0b013e318170d52e. [DOI] [PubMed] [Google Scholar]
- 18.Tissot Dupont H, Raoult D, Brouqui P, Janbon F, Peyramond D, Weiller PJ, et al. Epidemiologic features and clinical presentation of acute Q fever in hospitalized patients: 323 French cases. Am J Med. 1992;93:427–434. doi: 10.1016/0002-9343(92)90173-9. [DOI] [PubMed] [Google Scholar]
- 19.Keidar Z, Gurman-Balbir A, Gaitini D, Israel O. Fever of unknown origin: the role of 18F-FDG PET/CT. J Nucl Med. 2008;49:1980–1985. doi: 10.2967/jnumed.108.054692. [DOI] [PubMed] [Google Scholar]