Abstract
Skull base osteomyelitis is a potentially fatal disease. We demonstrate here the utility of SPECT/CT in diagnosing this entity, which was not obvious on a planar bone scan. A 99mTc MDP bone scan with SPECT/CT was carried out on a patient with clinically suspected skull base osteomyelitis. Findings were correlated with contrast-enhanced CT (CECT) and MRI. Planar images were equivocal, but SPECT/CT showed intense uptake in the body of sphenoid and petrous temporal bone as well as the atlas corresponding to irregular bone destruction on CT and MRI. These findings indicate that SPECT/CT may have an additional role beyond planar imaging in the detection of skull base osteomyelitis.
Keywords: Skull base osteomyelitis, Bone scan, SPECT/CT
Introduction
Skull base osteomyelitis is a common complication of infections of the ear, especially in diabetic, immunocompromised, elderly patients [1]. Most commonly it involves the temporal bone, but sphenoid and occipital bone sometimes also may be involved [2]. Pseudomonas aeruginosa is the most commonly involved microorganism. Earache is usually the presenting symptom, but headache can be the predominant feature in some atypical cases [3]. We present here the findings of a 99mTc MDP planar bone scan and SPECT/CT in a case of skull base osteomyelitis.
Case Report
A 62-year-old female diabetic patient presented to the neurology clinic with symptoms of severe headache and dizziness for 1 week. The patient had a history of left earache that had progressively increased for 2 weeks before the onset of the headache. She also had had a low grade fever for the last week. She was diabetic and had been on 25 units of insulin/day for the last 12 years. On examination the patient was febrile (38 °C) with a pulse of 90/min. The patient was ambulatory and stable. She was evaluated with hematological reports, MRI, CT and bone scans. Hematological reports showed leukocytosis with 80% neutrophils. CT of the central skull base showed irregular lytic bony destruction involving the apex of the petrous temporal bone and body of the sphenoid on the left side (Fig. 1). MRI (T2-weighted) revealed a hyperintensity involving the apex of the left petrous bone and left half of the body of the sphenoid. Also noted was a hyperintense lesion on the left side of the arch of the atlas. On T1-weighted post-contrast (Gd-DTPA) MRI images, enhancement of the above-mentioned regions were seen (Figs. 2, 3). A bone scan was was carried out in three phases, namely the blood flow, blood pool and delayed static phase. The delayed imaging was done 4 h after intravenous injection of 20 mCi (740 MBq) of 99mTc MDP using a Siemens E-cam dual-head gamma camera with acquisition in the continuous mode at a speed of 15 cm/min. SPECT/CT was done on a Siemens Symbia T-6 scanner. Slice thickness was kept at 5 mm. For SPECT acquisition, a frame time of 20 s was used with a 3° angular step. The planar bone scan showed faint uptake overlapping with the sphenoid bone on the anterior regional image and with the occiput on the posterior regional image (Fig. 4). However, on SPECT/CT intense uptake was noted in the left half of the body of the sphenoid bone, petrous temporal bone and left side of the arch of the atlas (Figs. 5, 6). The bone scan thus corroborated the findings of CT and MRI, and aided in the clinical diagnosis. The patient was then treated with intravenous broad-spectrum antibiotics.
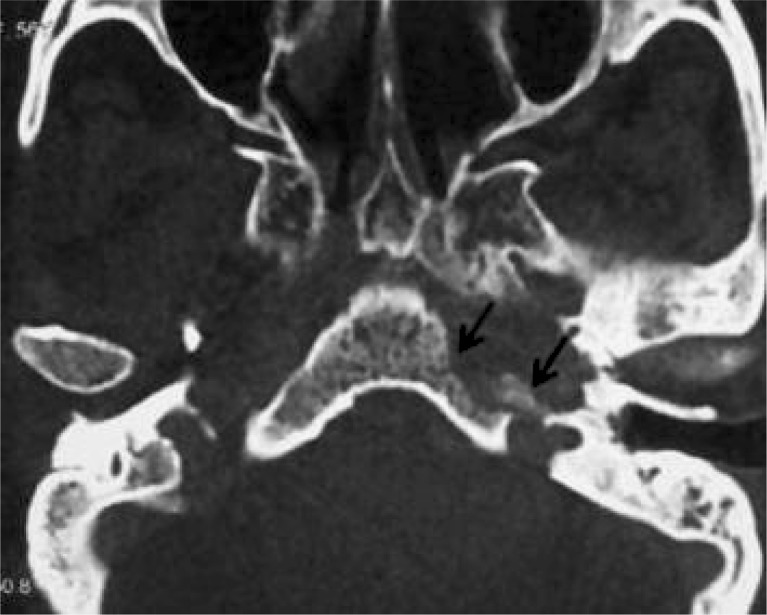
Fig. 1.
Axial CT image of the central skull base showing irregular lytic bony destruction involving the apex of the petrous temporal bone and body of the sphenoid bone on the left side
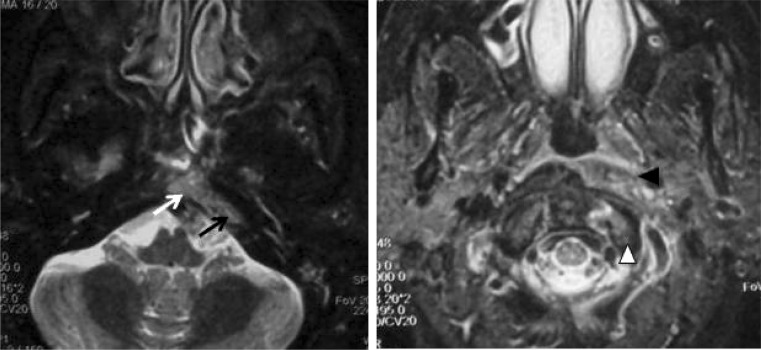
Fig. 2.
Axial sections of the T2-weighted fat-suppressed inversion recovery sequence (a, b) of the central skull base showing hyperintensity involving the apex of the petrous bone (black arrow) and left half of the body of the sphenoid bone (white arrow) (a). Hyperintensity is also noted involving the left side of the arch of the atlas (white arrowhead) (b). Note: adjacent soft tissue signal intensity alteration is seen (black arrowhead)
Fig. 3.
Axial T1-weighted post-contrast (Gd-DTPA) MRI images showing enhancement of the apex of the petrous temporal bone (black arrow) and left half of the body of the sphenoid bone (white arrow) (a). Also enhancement is noted involving the left side of the arch of the atlas (black arrowhead) and adjacent soft tissue (white arrowhead) (b)
Fig. 4.
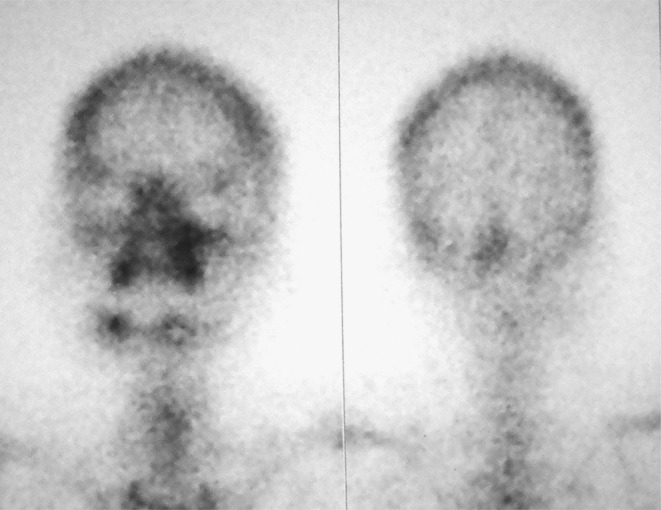
99mTc-MDP bone scan image showed faint uptake overlapping with sphenoid bone on the anterior regional image and with the occiput on the posterior regional image
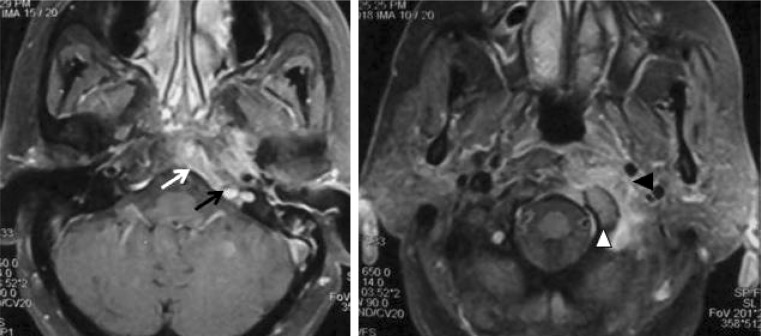
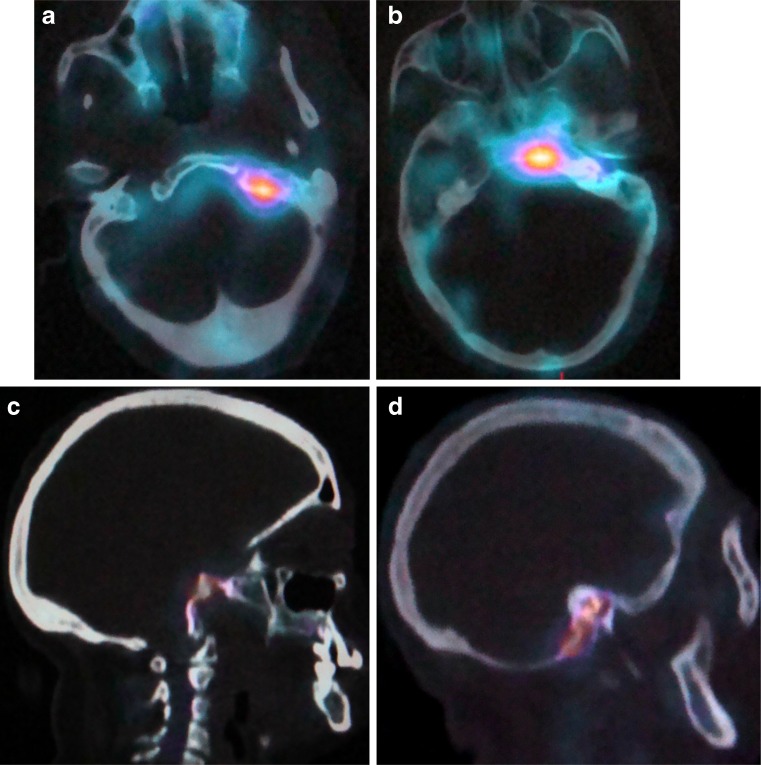
Fig. 5.
Axial and sagittal images of SPECT showing increased uptake in the left skull base. However, the exact anatomic location is not clear
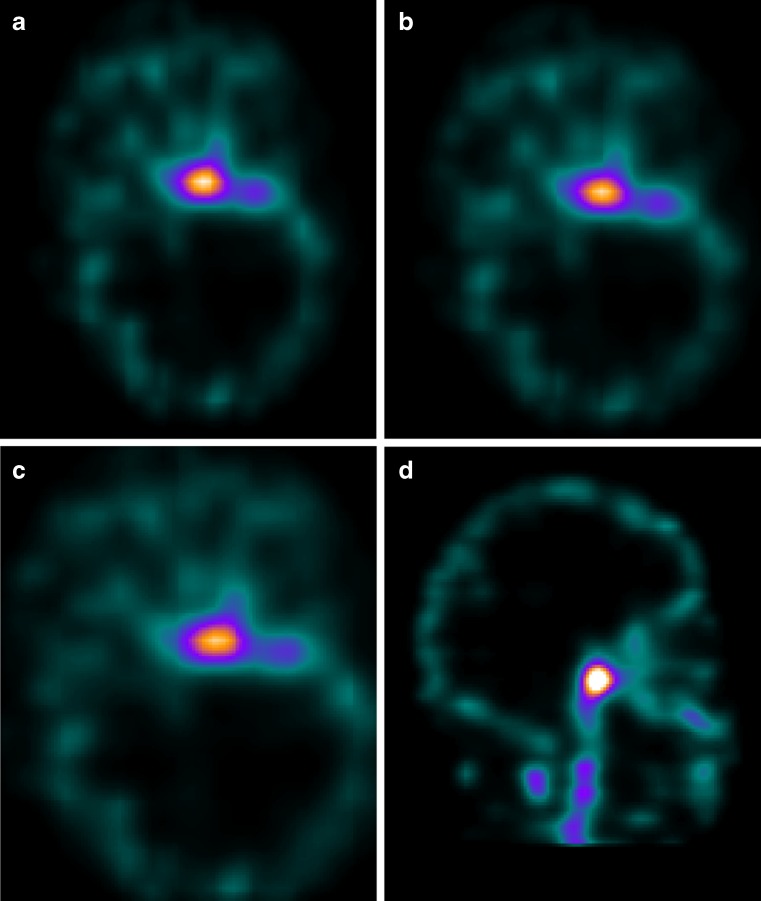
Fig. 6.
Axial and sagittal images (a, b, c, d) of SPECT-CT showing increased uptake in the left half of the body of the sphenoid bone, apex of the petrous temporal bone and left side of the arch of the atlas
Discussion
Skull base osteomyelitis is an uncommon condition that is life threatening if not recognized and treated in time. Potential complications include cranial neuropathy, cavernous sinus thrombosis, septicemia, and cerebral and meningeal involvement [4]. Typical skull base osteomyelitis involves the temporal bone and is usually a complication of malignant otitis externa in a diabetic/immunocompromised patient due to Pseudomonas aeruginosa. Osteomyelitis of the skull can result as a complication of infective paranasal sinusitis, trauma, tooth extractions, chronic mastoiditis, malignant otitis externa and various surgical procedures such as surgical debridement or drainage of a mastoid abscess [5, 6]. Conventional 99mTc MDP bone scan planar images are often unable to localize the exact site of infection inspite of being a sensitive technique for the diagnosis of osteomyelitis. Also the 99mTc MDP bone scan has limited spatial resolution and cannot pinpoint the site of involvement in case of skull base osteomyelitis. However, hybrid SPECT/CT enables us to achieve a high sensitivity with exact localization and correlation with CT changes as compared to SPECT alone [7]. In a recent study Fillippi et al. found the sensitivity of SPECT and SPECT/CT to be equal and high (100%) in identifying infected foci, but the specificity of SPECT/CT was higher (89% vs. 78%) as compared to SPECT alone [8]. A study by Römer et al. showed that SPECT-guided CT clarified 92% of bone lesions that were indeterminate at SPECT and made a definite characterization as benign or malignant [9]. Horger et al. also showed that a much higher percentage of lesions can be characterized using SPECT/CT as compared to SPECT alone [10]. The role of SPECT/CT in infection imaging has been recently studied by Bar-Shalom et al. using 67Ga- or 111In-labeled WBCs. The authors concluded that SPECT/CT with 67Ga- or 111In-labeled WBCs made an incremental contribution to scintigraphy by improving the diagnosis, localization or definition of the extent of disease [11]. In this particular case planar images alone would have missed the diagnosis. SPECT alone was able to show the increased uptake, but was unclear concerning the exact anatomic location. SPECT/CT not only corrected the findings, but also showed good correlation with radiological investigations. Use of SPECT/CT may therefore be considered in all cases of clinically suspected skull base osteomyelitis.
Acknowledgments
Conflict of Interest
No conflict of interest exists with respect to this article for all the authors concerned.
References
- 1.Sreepada GS, Kwartler JA. Skull base osteomyelitis secondary to malignant otitis externa. Curr Opin Otolaryngol Head Neck Surg. 2003;11(5):316–323. doi: 10.1097/00020840-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Chang PC, Fischbein NJ, Holliday RA. Central skull base osteomyelitis in patients without otitis externa: imaging findings. Am J Neuroradiol. 2003;24(7):1310–1316. [PMC free article] [PubMed] [Google Scholar]
- 3.Carfrae MJ, Kesser BW. Malignant otitis externa. Otolaryngol Clin North Am. 2008;41(3):537–549. doi: 10.1016/j.otc.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 4.Bruni C, Padovano F, Travascio L, Schillaci O, Simonetti G. Usefulness of hybrid SPECT/CT for the 99mTc-HMPAO-labeled leukocyte scintigraphy in a case of cranial osteomyelitis. Braz J Infect Dis. 2008;12(6):558–560. doi: 10.1590/S1413-86702008000600027. [DOI] [PubMed] [Google Scholar]
- 5.Seabold JE, Simonson TM, Weber PC, Thompson BH, Harris KG, et al. Cranial osteomyelitis: diagnosis and follow-up with In-111 white blood cell and Tc-99 m methylene diphosphonate bone SPECT, CT, and MR imaging. Radiology. 1995;196(3):779–788. doi: 10.1148/radiology.196.3.7644643. [DOI] [PubMed] [Google Scholar]
- 6.Chandler JR, Grobman L, Quencer R, Serafini A. Osteomyelitis of the base of the skull. Laryngoscope. 1986;96:245–251. doi: 10.1288/00005537-198603000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Schillaci O, Simonetti G. Fusion imaging in nuclear medicine: applications of dual-modality systems in oncology. Cancer Biother Radiopharm. 2004;19:1–10. doi: 10.1089/108497804773391621. [DOI] [PubMed] [Google Scholar]
- 8.Filippi L, Schillaci O. Usefulness of hybrid SPECT/CT in 99mTc-HMPAO-labeled leukocyte scintigraphy for bone and joint infections. J Nucl Med. 2006;47(12):1908–1913. [PubMed] [Google Scholar]
- 9.Römer W, Nomayr A, Uder M, Bautz W, Kuwert T. SPECT-guided CT for evaluating foci of increased bone metabolism classified as indeterminate on SPECT in cancer patients. J Nucl Med. 2006;47:1102–1106. [PubMed] [Google Scholar]
- 10.Horger M, Eschmann SM, Pfannenberg C, et al. Added value of SPECT/CT in patients suspected of having bone infection: preliminary results. Arch Orthop Trauma Surg. 2007;127:211–221. doi: 10.1007/s00402-006-0259-6. [DOI] [PubMed] [Google Scholar]
- 11.Bar-Shalom R, Yefremov N, Guralnik L, et al. SPECT/CT using 67Ga and 111In-labeled leukocyte scintigraphy for diagnosis of infection. J Nucl Med. 2006;47:587–594. [PubMed] [Google Scholar]