Abstract
The findings of an ovarian mass with marked ascites and pleural effusion are highly suggestive of malignancy, especially in a postmenopausal female with an elevated level of CA-125. However, benign conditions such as Meigs’ syndrome should be considered in the differential diagnosis if the primary mass shows benign features. 18F-FDG is known to be useful to differentiate between malignant and benign diseases, and this utility is also promising in the case of ovarian tumor. We present here a case of Meigs’ syndrome that was evaluated by 18F-FDG PET/CT, and this helped the preoperative diagnosis be made. 18F-FDG PET/CT is a promising modality to diagnose the pathological character of an ovarian tumor preoperatively, which can lead to a proper therapeutic plan.
Keywords: Meigs’ syndrome, Fluorodeoxyglucose, Positron-emission tomography, CA-125
Introduction
Meigs’ syndrome was first described in 1937 [1]. It consists of a benign ovarian tumor, typically fibroma, ascites, and pleural effusion. High serum carbohydrate antigen 125 (CA-125) level in a postmenopausal woman with associated solid ovarian tumor, ascites, and pleural effusion is highly suggestive of ovarian malignancy. However, patients with Meigs’ syndrome can also have elevated levels of serum CA-125 [2, 3].
The recently developed [18F] fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) is a promising modality to differentiate a malignant ovarian mass from a benign mass [4]. We report here a case of Meigs' syndrome presenting with bilateral ovarian fibromas and elevated levels of CA-125. The ovarian masses showed mildly increased uptake of 18F-FDG.
Case Report
A 62-year-old postmenopausal woman who presented with a palpable abdominal mass was transferred to our hospital for further evaluation of her mass and its management. She had undergone radiologic evaluation at the other hospital, and a huge ovarian mass with ascites was found. She was initially diagnosed with a malignant ovarian mass, along with the suspicion of peritoneal seeding, at the other hospital.
The CA-125 level was reported to be 336 U/mL (normal range: 0–36 U/mL) and the carcinoembryonic antigen (CEA) level was 2.4 ng/mL (normal range: 0–5.0 ng/mL). The initial imaging examination that employed contrast-enhanced computed tomography (CT) showed a slightly low-attenuating, multilobulated huge homogeneous solid mass around the uterus and ascites. A smaller mass was also found in right abdomen. The possibility of malignancy was considered due to ascites and the possible peritoneal seeding (Fig. 1a).
Fig. 1.

a The contrast-enhanced CT image shows a multilobulated huge solid mass and another smaller mass (arrow) in the abdominopelvic area. b The non-contrast CT image shows ascites (top arrow) and a right-sided pleural effusion (bottom arrow)
With the suspicion of malignant possibilities such as Krukenberg tumor or ovarian cancer, 18F-FDG PET/CT was performed to evaluate these masses and to determine whether other malignant lesions were present. PET/CT was performed (Biograph LSO; Siemens Medical System) after 12 h fasting and 1 h after the intravenous administration of 407 MBq of 18F-FDG. The previously determined huge lobulated homogeneous mass in the pelvic to the abdominal cavity showed mild 18F-FDG uptake, and the maximum standardized uptake value was 2.2 (Fig. 2a, b, c). In addition, there were ascites and right-sided pleural effusion without significant 18F-FDG uptake (Fig. 1b, 2d). These findings were interpreted as a benign ovarian tumor rather than a malignant one on the basis of the low 18F-FDG metabolism even though the size was huge.
Fig. 2.
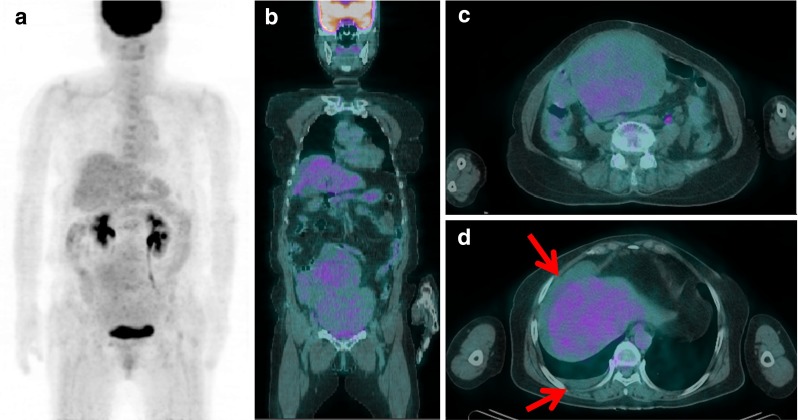
The huge abdominal mass shows mild 18F-FDG uptake on a the anterior maximum intensity projection image and b the coronal and c the axial PET/CT fusion image. d The axial PET/CT fusion image shows ascites (top arrow) and a right-sided pleural effusion (bottom arrow) without significant 18F-FDG uptake
Exploratory laparotomy with bilateral salpingo-oophorectomy was performed. The histopathological examination reported that there were fibromas on both ovaries: the sizes were 24 × 14 × 10 cm on the left ovary and 8 × 7 × 3 cm on the right ovary (Fig. 3). Another mass, which had been thought to be a peritoneal seeding, turned out to be a pedunculated part of the main mass. The cytology of the ascitic fluid was also negative for malignant cells. Based on the pathological findings of the ovarian masses and the radiological findings of ascites and right-sided pleural effusion, she was diagnosed as having Meigs’ syndrome. Her simple chest radiographic images demonstrated that her pleural effusion spontaneously resolved after resection of both ovarian fibromas.
Fig. 3.

The macroscopic and microscopic pictures of the ovarian tumor specimen. The a uncut and b cross-section images show a firm and solid mass. c Under microscope, the ovarian tumor specimen shows bundles of spindle cells and large amounts of collagen
Discussion
Meigs’ syndrome is defined by the presence of (1) a benign ovarian tumor, typically an ovarian fibroma, (2) ascites, and (3) pleural effusion. Fibroma is the most common sex cord-stromal tumor, and it is composed of fascicles of spindle cells and collagen [5]. Women with ovarian fibroma are usually asymptomatic, and the masses are often discovered accidentally in middle-aged women. The proportion of ovarian fibroma of all ovarian tumors is about 4% [6, 7]. Fifteen to 40% of the ovarian fibromas are accompanied by isolated ascites and approximately 1% of the ovarian fibromas are associated with Meigs’ syndrome [2, 7, 8]. Fibromas have a low malignant potential, and they are almost always benign. The ascites and pleural effusion resolve after the ovarian tumor is removed. However, ovarian fibromas may mimic malignant neoplasm because they appear as solid masses, and they are sometimes accompanied with ascites and pleural effusion.
In addition to imaging studies, CA-125 is widely used to predict malignancy of an ovarian mass. The sensitivity of CA-125 for detecting ovarian malignancy is 80% [9]. However, the CA-125 level is also known to increase in various benign gynecologic conditions. In a study with 115 patients with histologically proven nonmalignant pelvic tumor, a significantly elevated CA-125 level was found in 14 patients and the highest values were detected in the patients with ascites [10]. There are some case reports of elevated CA-125 levels in patients with Meigs’ syndrome, and in some of them, the levels of CA-125 were over 1,000 U/mL [2, 11]. Therefore, pathologic evaluation of ovarian tumor is needed to make the correct diagnosis since the tumor markers and the other indicators of malignancy may be misleading [2].
18F-FDG is known to be useful to differentiate between malignant and benign diseases [12, 13], and this utility is also promising in the case of ovarian tumor. Fenchel et al. [14] analyzed asymptomatic adnexal masses with 18F-FDG PET, and the overall sensitivity, specificity, and accuracy of 18F-FDG PET for differentiating malignant ovarian tumors were 58, 76, and 74%, respectively. These initial results for ovarian cancer show that 18F-FDG PET had some limitations in distinguishing malignant from benign ovarian tumors. However, in a recent study taking advantage of hybrid PET/CT, Castellucci et al. [4] reported higher sensitivity, specificity, and accuracy of 18F-FDG PET for differentiating between malignant and benign ovarian lesions, and those were 87, 100, and 92%, respectively. The criterion for ovarian malignancy used in the study was a focally increased 18F-FDG uptake with a maximum standardized uptake value (SUVmax) higher than 3.0 in the ovarian lesion. In three of four false-negative PET/CT scans in that study, primary tumors measured ≤5 mm, which implies that the tumor size can be the main cause of false negativity.
In the current case of Meigs’ syndrome, 18F-FDG PET/CT helped us make the patient’s preoperative diagnosis. The fibroma of the patient showed mild 18F-FDG uptake. 18F-FDG is reported to accumulate in fibroblasts [15], and so a benign ovarian fibroma might show increased 18F-FDG uptake. However, we were able to diagnose it as a benign lesion based on the level of SUVmax (2.2), which was lower than would be expected if the huge tumor were really malignant.
In summary, we present here a case of Meigs’ syndrome with an elevated CA-125 level, and 18F-FDG PET/CT helped us make a preoperative diagnosis. The finding of an ovarian mass accompanied by a significant amount of ascites and pleural effusion is highly suggestive of malignancy, especially in a postmenopausal female with an elevated CA-125 level. But benign conditions such as Meigs’ syndrome should be considered in the differential diagnosis if the primary mass shows benign features. 18F-FDG PET/CT holds promise of assessing the pathological character of an ovarian tumor preoperatively, which can lead to a proper therapeutic plan.
Acknowledgements
This work was financially supported by a NCC Korea intramural grant (1110211–1).
Conflict of Interest
We declare that we have no conflict of interest.
References
- 1.Meigs JV, Cass JW. Fibroma of the ovary with ascites and hydrothorax: A report of 7 cases. Am J Obstet Gynecol. 1937;33:249–267. [Google Scholar]
- 2.Abad A, Cazorla E, Ruiz F, Aznar I, Asins E, Llixiona J. Meigs' syndrome with elevated CA125: case report and review of the literature. Eur J Obstet Gynecol Reprod Biol. 1999;82:97–99. doi: 10.1016/S0301-2115(98)00174-2. [DOI] [PubMed] [Google Scholar]
- 3.Vieira SC, Pimentel LHC, Ribeiro JCCB. Andrade Neto AF, Santana JOI. Meigs' syndrome with elevated CA 125: case report. Sao Paulo Med J. 2003;121:210–212. doi: 10.1590/S1516-31802003000500007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Castellucci P, Perrone AM, Picchio M, Ghi T, Farsad M, Nanni C, et al. Diagnostic accuracy of 18F-FDG PET/CT in characterizing ovarian lesions and staging ovarian cancer: correlation with transvaginal ultrasonography, computed tomography, and histology. Nucl Med Commun. 2007;28:589–595. doi: 10.1097/MNM.0b013e3281afa256. [DOI] [PubMed] [Google Scholar]
- 5.Amin HK, Okagaki T, Richart RM. Classification of fibroma and thecoma of the ovary. An ultrastructural study. Cancer. 1971;27:438–446. doi: 10.1002/1097-0142(197102)27:2<438::AID-CNCR2820270231>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 6.Chechia A, Attia L, Temime RB, Makhlouf T, Koubaa A. Incidence, clinical analysis, and management of ovarian fibromas and fibrothecomas. Am J Obstet Gynecol. 2008;199:473.e1–473.e4. doi: 10.1016/j.ajog.2008.03.053. [DOI] [PubMed] [Google Scholar]
- 7.Lanitis S, Sivakumar S, Behranwala K, Zacharakis E, Al Mufti R, Hadjiminas DJ. A case of Meigs syndrome mimicking metastatic breast carcinoma. World J Surg Oncol. 2009;7:10. doi: 10.1186/1477-7819-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shanbhogue AK, Shanbhogue DK, Prasad SR, Surabhi VR, Fasih N, Menias CO. Clinical syndromes associated with ovarian neoplasms: a comprehensive review. Radiographics. 2010;30(4):903–919. doi: 10.1148/rg.304095745. [DOI] [PubMed] [Google Scholar]
- 9.Medeiros LR, Rosa DD, da Rosa MI, Bozzetti MC. Accuracy of CA 125 in the diagnosis of ovarian tumors: A quantitative systematic review. Eur J Obstet Gynecol Reprod Biol. 2009;142:99–105. doi: 10.1016/j.ejogrb.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 10.Buamah PK, Skillen AW. Serum CA 125 concentrations in patients with benign ovarian tumours. J Surg Oncol. 1994;56:71–74. doi: 10.1002/jso.2930560204. [DOI] [PubMed] [Google Scholar]
- 11.Benjapibal M, Sangkarat S, Laiwejpithaya S, Viriyapak B, Chaopotong P, Jaishuen A. Meigs’ syndrome with elevated serum CA125: Case report and review of the literature. Case Reports Oncol. 2009;2:61–66. doi: 10.1159/000210441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dimitrakopoulou-Strauss A, Strauss LG, Heichel T, Wu H, Burger C, Bernd L, et al. The role of quantitative 18F-FDG PET studies for the differentiation of malignant and benign bone lesions. J Nucl Med. 2002;43:510–518. [PubMed] [Google Scholar]
- 13.Beggs A, Hain S, Curran K, O'Doherty M. FDG-PET as a “metabolic biopsy” tool in non-lung lesions with indeterminate biopsy. Eur J Nucl Med. 2002;29:542–546. doi: 10.1007/s00259-001-0736-7. [DOI] [PubMed] [Google Scholar]
- 14.Fenchel S, Grab D, Nuessle K, Kotzerke J, Rieber A, Kreienberg R, et al. Asymptomatic adnexal masses: Correlation of FDG PET and histopathologic findings. Radiology. 2002;223:780–788. doi: 10.1148/radiol.2233001850. [DOI] [PubMed] [Google Scholar]
- 15.Kubota K, Kubota R, Yamada S. FDG accumulation in tumor tissue. J Nucl Med. 1993;34:419–421. [PubMed] [Google Scholar]


