Gardner’s syndrome (GS), a variant of familial adenomatous polyposis, is an autosomal dominant disease. Originally, Gardner described a syndrome consisting of hereditary intestinal polyposis with osteomas and multiple cutaneous and subcutaneous lesions [1] (Figs. 1 and 2). The syndrome was later modified by the addition of other features, such as dental abnormalities, abdominal fibromatosis, and a number of malignant tumors. The principal cutaneous lesions that have been described in GS are epidermoid cysts. Other cutaneous lesions include fibromas, lipomas, leiomyomas, neurofibromas, and pigmented skin lesions [2]. Fibromatoses are histologically benign, but locally aggressive fibrous tumors consisting of mature fibroblasts within an extensive collagen matrix. Most cases are sporadic, but there is a clear association with familial adenomatous polyposis and GS, suggesting a link with a mutation of the APC gene on chromosome 5q22 [3]. Fibromatosis occurs in 3.5%–29% of patients with GS, and is more likely to be multiple and to involve the mesentery and abdominal wall rather than being an isolated form [4, 5]. Clinically, fibromatosis presents as a painless firm soft tissue mass. Most cases of fibromatosis are believed to be precipitated by surgical trauma; however, a few cases of spontaneous occurrence have been reported [6]. In our patient, no history of abdominal surgery or trauma was present. In addition, an abdominal CT obtained 2 years ago revealed no abnormality.
Fig. 1.

A 20-year-old man was admitted to oral surgery with a dental problem. A panoramic radiograph showed multiple osteomas in the right angle and anterior portion of the mandible with dental abnormalities (impacted or unerupted teeth, and supernumerary teeth). Surgery was performed, and a biopsy confirmed osteomas
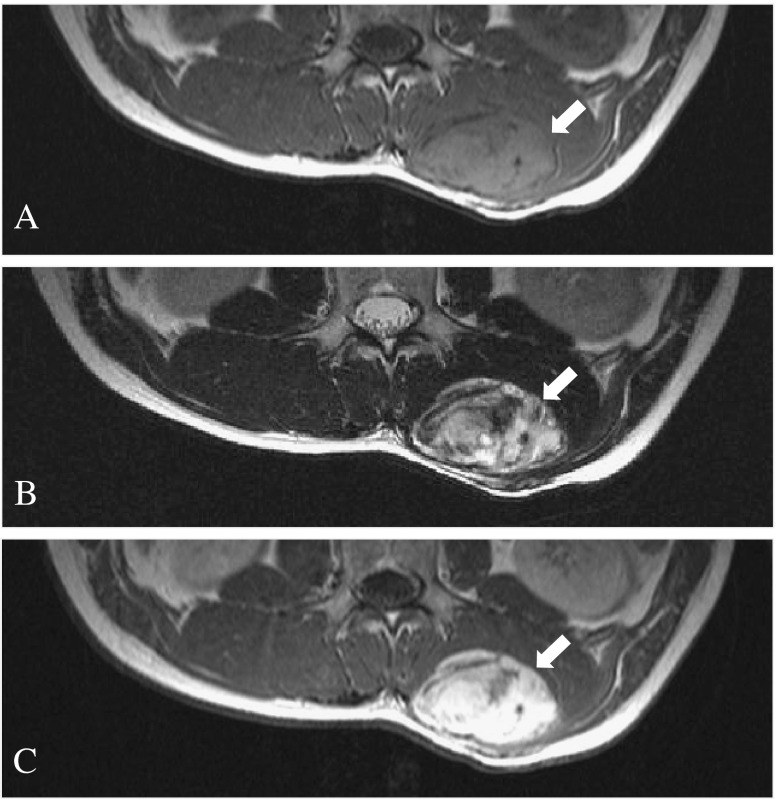
Fig. 2.
The patient had a history of excision of a mass on the back 4 years previously. (a–c) Transverse MR images showed low-signal intensity on T1-weighted image (WI), heterogenous high-signial intensity on T2WI, and marked enhancement on contrast-enhanced T1WI. Biopsy confirmed a neurofibroma
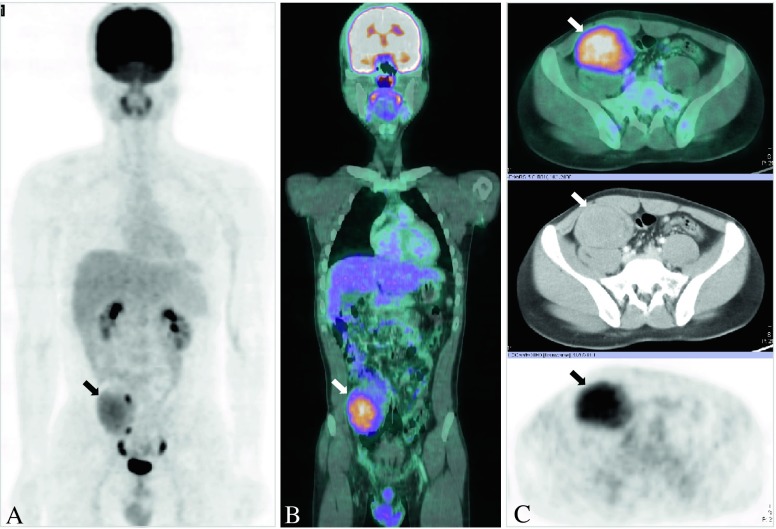
Although the radiological features of fibromatosis on CT or MR have been described in the literature, F-18 FDG-PET or PET/CT findings are rarely reported [7–10]. The F-18 FDG uptake in patients with fibromatosis ranged from low to moderate grade and was generally heterogenous with a few tiny foci of relatively intense uptake or relatively homogenous. The areas of higher FDG metabolism are likely to represent more cellular and mitotically active areas [7]. Mesenteric fibromatosis has similar findings to extra-abdominal lesions [7, 9] (Fig. 3).
Fig. 3.
Routine laboratory studies for dental surgery showed abnormal liver function tests. The patient was referred to the Gastroenterology Service. Computed tomography (CT) of the abdomen demonstrated a large soft tissue mass in the right lower quadrant (RLQ), suggesting a small bowel lymphoma with intussusception. A F-18 FDG PET/CT was performed to assess the tumor extent and determine the appropriate site of biopsy. (a) A maximum-intensity-projection (MIP) image showed an oval-shaped, moderate-grade FDG uptake interspersed with a few tiny foci of relatively intense uptake in the RLQ of the abdomen (arrow; SUVmax, 5.6). (b, c) Coronal (fused PET/CT) and transverse (upper image, fused PET/CT; middle image, contrast enhanced-CT; low image, PET) images through the mass revealed an 8 × 6-cm, enhanced, soft tissue mass with moderate-grade FDG accumulation in the RLQ. Upper and lower gastrointestinal endoscopy revealed multiple adenomatous polyps in the colon. Laparotomy revealed a firm mass in the mesentery. Biopsy confirmed a fibromatosis (also known as a desmoid tumor). The patient was diagnosed with Gardner’s syndrome, with multiple osteomas in the mandible, dental abnormalities, mesenteric fibromatosis, multiple colonic polyps, and neurofibroma
Acknowledgments
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Gardner EJ, Richards RC. Multiple cutaneous and subcutaneous lesions occurring simultaneously with hereditary polyposis and osteomatosis. Am J Hum Genet. 1953;5:139–47. [PMC free article] [PubMed] [Google Scholar]
- 2.Ascari-Raccagni A, Baldari U, Righini MG. Cutaneous symptoms of Gardner's syndrome. J Eur Acad Dermatol Venereol. 1999;12:80–1. doi: 10.1111/j.1468-3083.1999.tb00824.x. [DOI] [PubMed] [Google Scholar]
- 3.Clark SK, Phillips RK. Desmoids in familial adenomatous polyposis. Br J Surg. 1996;83:1494–504. doi: 10.1002/bjs.1800831105. [DOI] [PubMed] [Google Scholar]
- 4.Naylor EW, Gardner EJ, Richards RC. Desmoid tumors and mesenteric fibromatosis in Gardner's syndrome: Report of Kindred 109. Arch Surg. 1979;114:1181–5. doi: 10.1001/archsurg.1979.01370340087015. [DOI] [PubMed] [Google Scholar]
- 5.Kawashima A, Goldman SM, Fishman EK, Kuhlman JE, Onitsuka H, Fukuya T, et al. CT of intraabdominal desmoid tumors: Is the tumor different in patients with Gardner's disease? AJR Am J Roentgenol. 1994;162:339–42. doi: 10.2214/ajr.162.2.8310922. [DOI] [PubMed] [Google Scholar]
- 6.Richards RC, Rogers SW, Gardner EJ. Spontaneous mesenteric fibromatosis in Gardner's syndrome. Cancer. 1981;47:597–601. doi: 10.1002/1097-0142(19810201)47:3<597::AID-CNCR2820470329>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 7.Basu S, Nair N, Banavali S. Uptake characteristics of fluorodeoxyglucose (FDG) in deep fibromatosis and abdominal desmoids: Potential clinical role of FDG-PET in the management. Br J Radiol. 2007;80:750–6. doi: 10.1259/bjr/53719785. [DOI] [PubMed] [Google Scholar]
- 8.Maeda R, Isowa N, Onuma H, Miura H, Tokuyasu H, Kawasaki Y. Desmoid tumor of the chest wall in an elderly woman. Gen Thorac Cardiovasc Surg. 2009;57:554–7. doi: 10.1007/s11748-008-0404-y. [DOI] [PubMed] [Google Scholar]
- 9.Lo KW. Mesenteric fibromatosis as a potential source of false-positive interpretation of FDG-PET: Report of a case. Dis Colon Rectum. 2007;50:924–6. doi: 10.1007/s10350-006-0826-5. [DOI] [PubMed] [Google Scholar]
- 10.Kasper B, Dimitrakopoulou-Strauss A, Strauss LG, Hohenberger P. Positron emission tomography in patients with aggressive fibromatosis/desmoid tumours undergoing therapy with imatinib. Eur J Nucl Med Mol Imaging. 2010;37:1876–82. doi: 10.1007/s00259-010-1498-x. [DOI] [PubMed] [Google Scholar]