Abstract
After surgical therapy of diffuse pigmented villonodular synovitis (DPVNS), recurrence is seen in almost half of the patients. The effectiveness of radiosynovectomy (RSV) in preventing recurrence and complaints of DPVNS is well known. Elbow involvement in DPVNS is a very rare condition; therefore, RSV in elbow hasn’t been experienced widely. The aim of this case report is to show the effectiveness of RSV with rhenium-186 (Re-186) sulfide colloid. We applied Re-186 sulfide colloid to the elbow joint of DPVNS patients six weeks after arthroscopic synovectomy. As a result, the patient did not have any complaints, and our findings are compatible with residue or recurrence on magnetic resonance imaging (MRI) in sixth and twentieth month controls after administration. We concluded that Re-186 is an effective adjuvant therapy for the prevention of recurrence and complaints.
Keywords: Rhenium-186 (Re-186), Radiosynovectomy, Elbow, Diffuse Pigmented Villonodular Synovitis (DPVNS)
Introduction
Diffuse pigmented villonodular synovitis (DPVNS) is seen frequently in the third or fourth decades of life. It is a benign proliferative disease of the synovial membrane that causes joint and limb dysfunction [1]. The disease is usually monoarticular and affects the knee joint mostly [2]. The traditional treatment of DPVNS is surgery. Radiosynovectomy (RSV) is the application of radioactive material into the joint. This method is used as an adjuvant therapy after the surgery to eliminate residual tissue and to prevent recurrence. The involvement of the elbow in DPVNS is rare and nearly 20 cases have been reported [3]. For DPVNS, radiosynovectomy to the elbow joint with colloidal choromic phosphorus-32 (P-32) has been reported only in one case [4]. On the other hand, there are no reports on the use of rhenium-186 (Re-186) sulfide colloid (CIS Bio International, France) in the treatment of DPVNS of the elbow.
Case Report
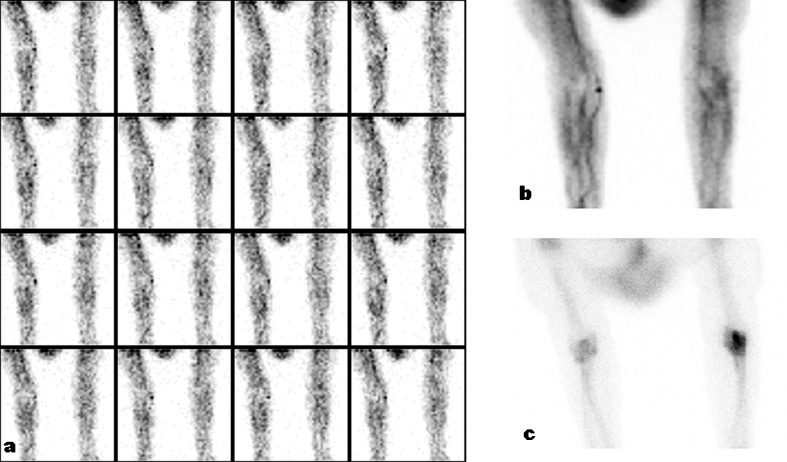
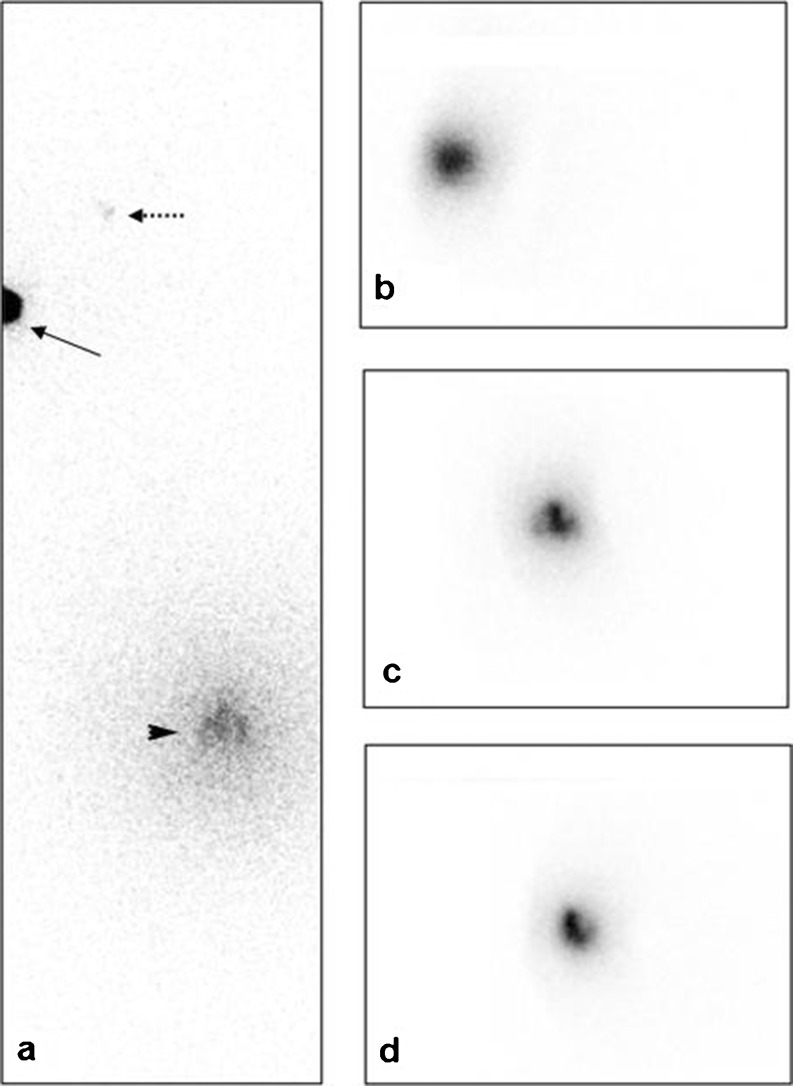
The patient, a 41-year-old female, had arthroscopy for DPVNS of the left knee. She had no recurrence initially, but was admitted with pain and swelling in her right elbow and left knee one year after the treatment. A magnetic resonance imaging (MRI) with contrast media was made for possible diagnosis of DPVNS in her right elbow joint. She underwent arthroscopic synovectomy for the lesions in her right elbow and left knee. Six weeks after the surgery, RSV was applied to her right elbow. In addition to the elbow joint, we applied yttrium-90 (Y-90) colloid (CIS Bio International, France) to her left knee joint. Before RSV, we took a three phase bone scintigraphy (Fig. 1). Minimal increased perfusion in perfusion phase (a) and minimal hyperemia in blood pool phase (b) were detected in the right elbow. On the late-phase image (c), increased activity accumulation was seen. She was given 3 mCi (111 MBq) Re-186 sulfide colloid under fluoroscopy guidance to her right elbow. We took an image of the right elbow to evaluate the distribution of Re-186 sulfide colloid (Fig. 2) on the fourth hour after the RSV application. The imaging of Re-186 sulfide colloid was performed using General Electric (GE) Millennium MG (USA) adjusted to 137 keV ± 10 % gamma rays with low energy general purpose collimator. The retention of the radiocolloid in the elbow joint was normal. There was low intensity axillary lymph node accumulation of radioactivity due to extraarticular leakage. Following the radiocolloid injection, the right elbow was stabilized with the cast for 72 hours. In the six months control after the RSV application, she didn’t have any complaints about her elbow. In twenty months control, MRI was taken. There was no residual lesion or recurrence on MRI images. Mayo elbow score was used to evaluate the functional status of the patient's right elbow joint. The score was 65/100 before RSV, which increased to 100/100 after 20 months.
Fig. 1.
Initial three phase bone scintigraphy (before RSV). (a) Perfusion phase, (b) Blood pool phase, (c) Late static phase
Fig. 2.
4 hours after Re-186 colloid injection into the right elbow, images show good intraarticular distribution. (a) Whole body view (right elbow-arrow, right axillary leakage-dashed arrow, left knee-arrow head), (b) Anterior view, (c) Lateral view, (d) Oblique view
Discussion
Jaffe, Lichtenstein and Sutro described the first DPVNS case in 1941. DPVNS is a rare, proliferative disease of the synovial membrane. The knee is the most frequently involved joint, but elbow, wrist, hip, ankle and finger joints can be also involved [5]. The symptoms are pain, swelling, stiffness of the joint. The disease usually affects only one joint [6]. The surgery is the choice of the therapy, but the relapse rate of DPVNS is high. Despite surgical treatment, the recurrence rate was high 46 % [7]. The factors causing relapse are unknown. The common outcome of DPVNS is the destruction of the joint. After the surgery, adjuvant radiotherapy or RSV is applied to improve the local control of the disease and the effectiveness of the treatment [8].
RSV is effective, low cost and easy to perform. It is a safe procedure that has few side effects and are generally avoidable [9]. Shabat et al. applied RSV to ten patients, and they didn’t observe any side effects [10]. Kat et al. applied 13 RSV to the knee joints of 11 pigmented villonodular synovitis (PVNS) patients, and they mentioned that the combination of surgical synovectomy with RSV is highly efficacious in treating the symptoms of PVNS [11].
Chen et al. used Y-90 colloid twice in three months on a patient that has PVNS in his knee. The efficiency of the therapy is seen with the significant MRI changes and a good correlation is seen with clinical outcome [12].
In six and twenty months controls, the patient in our case study didn’t have any symptoms about her right elbow. In twenty months control, there wasn’t any residual lesion or recurrence on MRI. We didn’t see any side effects during a 22-month follow-up.
Although RSV is indicated in DPVNS, we couldn’t find any case report or clinic paper for the elbow application of Re-186 sulfide colloid RSV. Colloidal chromic P-32 therapy was used only for one case in the elbow joint with DPVNS [4]. P-32 can be used in a wide range of the joints, but due to its longer half-life (14 days) when compared with Re-186 sulfide colloid (3.7 days) and high lymphatic transport; it is not recommended anymore [13]. In our case, RSV was useful for the complaints and recurrence. We suggest that Re-186 sulfide colloid can be used safely for the elbow involvement of DPVNS, but further studies are required.
Acknowledgments
Conflicts of interest
All named authors hereby declare that they have no conflicts of interest to disclose.
References
- 1.Berger B, Ganswindt U, Bamberg M, Hehr T. External beam radiotheraphy as postoperative treatment of diffuse pigmented villonodular synovitis. Int J Radiat Oncol Biol Phys. 2007;67(4):1130–1134. doi: 10.1016/j.ijrobp.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 2.Dorwart RH, Genant HK, Johnston WH, Morris JM. Pigmented villonodular synovitis of synovial joints: clinical, pathologic, and radiologic features. AJR Am J Roentgenol. 1984;143(4):877–885. doi: 10.2214/ajr.143.4.877. [DOI] [PubMed] [Google Scholar]
- 3.Sekiya H, Ozawa H, Sugimoto N, Kariya Y, Hoshino Y. Pigmented villonodular synovitis of the elbow in a 6-year-old girl: a case report. J Orthop Surg (Hong Kong) 2007;15(1):106–108. doi: 10.1177/230949900701500124. [DOI] [PubMed] [Google Scholar]
- 4.Ward WG, Sr, Boles CA, Ball JD, Cline MT. Diffuse pigmented villonodular synovitis: preliminary results with intralesional resection and p32 synoviorthesis. Clin Orthop Relat Res. 2007;454:186–191. doi: 10.1097/01.blo.0000229345.57092.a2. [DOI] [PubMed] [Google Scholar]
- 5.Miller WE. Villonodular synovitis: pigmented and nonpigmented variations. South Med J. 1982;75(9):1084–1086. doi: 10.1097/00007611-198209000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Ogilvie-Harris DJ, McLean J, Zarnett ME. Pigmented villonodular synovitis of the knee: The results of total arthroscopic synovectomy, partial arthroscopic synovectomy, and arthroscopic local excision. J Bone Joint Surg Am. 1992;74:119–123. [PubMed] [Google Scholar]
- 7.Jones FE, Soule EH, Doventry MB. Fibrous xanthoma of synovium (giant-cell tumor of tendon sheath, pigmented nodular synovitis) J Bone Joint Surg [Am] 1969;51:76–86. [PubMed] [Google Scholar]
- 8.Nassar WA, Bassiony AA, Elghazaly HA. Treatment of diffuse pigmented villonodular synovitis of the knee with combined surgical and radiosynovectomy. HSS J. 2009;5:19–23. doi: 10.1007/s11420-008-9104-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wiss DA. Recurrent villonodular synovitis of the knee. Successful treatment with yttrium-90. In Orthop Relat Res. 1982;169:139–144. [PubMed] [Google Scholar]
- 10.Shabat S, Kollender Y, Merimsky O, Isakov J, Flusser G, Nyska M, Meller I. The use of surgery and yttrium 90 in the management of extensive and diffuse pigmented villonodular synovitis of large joints. Rheumatology. 2002;41:1113–1118. doi: 10.1093/rheumatology/41.10.1113. [DOI] [PubMed] [Google Scholar]
- 11.Kat S, Kutz R, Elbracht T, Weseloh G, Kuwert T. Radiosynovectomy in pigmented villonodular synovitis. Nuklearmedizin. 2000;39:209–213. [PubMed] [Google Scholar]
- 12.Chen DY, Lan JL, Chou SJ. Treatment of pigmented villonodular synovitis with yttrium-90: changes in immunologic features, Tc-99 m uptake measurements, and MR imaging of one case. Clin Rheumatol. 1992;11:280–285. doi: 10.1007/BF02207973. [DOI] [PubMed] [Google Scholar]
- 13.Turkmen C. Safety of Radiosynovectomy in Hemophilic Synovitis: it is Time to Re-evaluate! J Coagul Disord. 2009;1(1):29-36.