Abstract
Purpose of review
Robotic surgery in Otolaryngology-Head and Neck Surgery has become a valuable tool in certain anatomic approaches, however its application in surgery of the paranasal sinuses and anterior skull base is still in an investigatory phase and requires further evaluation.
Recent findings
Existing robotic surgical systems face particular limitations in their application at the skull base because of instrument size and lack of variability. Unfortunately, only one system is available commercially that is applicable in the head and neck region and FDA approved for use in patients. This system, while advantageous in many otolaryngologic procedures, is difficult to use for endoscopic sinus and skull base surgery. However, other systems that target this anatomic subsite specifically are in development and show promise. Advances in the design of robotic arms, materials, and shape will potentially give surgeons significant advantage over traditional endoscopic techniques.
Summary
This paper will review the current applications of robotic systems in paranasal sinus and skull base surgery, describe the requirements of a robotic system for use in this type of surgery, and describe a system under development at our institution.
Keywords: robotic surgery, skull base surgery, endoscopic sinus surgery
Introduction
Endoscopic approaches to the nose, paranasal sinuses, and anterior skull base continue to expand with new technologies and improved surgical techniques. Some surgeons in the U.S. and abroad are experimenting with the application of robotic tools in surgery (1–3). The draw of using the robot in surgery has been fueled by legitimate advantages in control and visualization discovered by our colleagues in general, urologic, and gynecologic surgery (4–6). However, operating in the head and neck provides a different set of anatomic constraints that challenge the existing robotic technology's capabilities. This article will review the current state of robotic surgery in the paranasal sinuses and anterior skull base, define the key variables that limit endonasal approaches to the paranasal sinuses and skull base (PSSB), and discuss the future of robotic surgery in PSSB surgery.
Current Technologies
The only FDA approved robotic system currently used in Otolaryngology is the da Vinci Surgical System by Intuitive Surgical Inc. This device is well described in the literature. The impetus for design of the da Vinci system was improved control of instruments at the surgical field via wristed motion (7), particularly in laparoscopic surgeries. (4–6).
Within Otolaryngology, the da Vinci system has been utilized primarily in head and neck cancer surgery and thyroid surgery. Advances have been made in control of base of tongue and supraglottic cancers (8). Transaxillary robotic thyroidectomy has been used to effectively treat thyroid disease through a minimally invasive approach (9,10).
The application of the da Vinci system in the PSSB realm has been less successful. While natural orifice surgery is the primary goal of transnasal endoscopic surgery of the PSSB, the tools must fit through the orifice being used. Attempts have been made to augment the approach to PSSB using transantral approaches (1), transoral/transnasal approaches (11), and combined transnasal, transcervical approaches (12). These attempts have had some success and bring the benefit of the wristed robotic instruments to PSSB. Unfortunately, the morbidity associated with these approaches is not negligible. In all described approaches, there is natural tissue disturbance outside of the nasal cavity. However, the advantages of the wristed controls at the skull base are non-negligible. Improved ability to manipulate the tissue with grasping forceps provides significant advantage over standard endonasal techniques with rigid grabbing instruments - especially when dural resection/repair is necessary.
Concepts of Endonasal Endoscopic Surgical Approaches to the PSSB
Much has been written on the various approaches to the PSSB (13–15, 16, 17). These approaches were developed through a thorough understanding of the anatomy. However, these approaches are also constrained by the anatomic limitations with regard to current instrumentation. The guiding principles of endoscopic sinus and skull base surgery are:
Line of sight - instrumentation must be visualized in the endoscopic field to reach the target tissue while minimizing damage to surrounding structures
Orbital and Skull Base Preservation/Repair - Limit the unintended violations and repair the necessary violations with robust materials
Neurovascular control - identify and preserve neurovascular structures
The benefits of existing robotic instrumentation are more precision with wristed movements at the millimeter level (7) and improved visualization with stable endoscopy with three-dimensional visualization. But the size of both telescopes and instruments relative to surgical site anatomic limitations and rigidity of instruments except at the tip hinder the da Vinci system’s utility in PSSB surgery. To address the guiding principles, new technology must be developed. Despite the limitations of the da Vinci robot in the PSSB, the application of robotic surgery to this space is not without merit. However, a more appropriate technology has yet to be developed. Applying a technology that was developed for closed cavity abdominal surgery to a rigid, bony structure with multiple corners is suboptimal at best.
New Technology Requirements
Given the guiding principles mentioned above, what are the functional requirements for an ideal robotic system for PSSB surgery?
Instruments are small
Instruments are flexible
Instruments are strong
Multiple instruments with endoscopy can be present in the same field
Instrument exchange is facile
Instruments are compatible with an image guidance system
Entire system is transnasal in approach
System is not cumbersome at the surgical field
Instruments provide haptic feedback.
The first challenge in development concerns requirements 1–3. Traditional transnasal instruments, while small and strong, are not flexible. Movement of the instruments across the PSSB occurs around the pivot point at the nostril. The Da Vinci instruments were developed to move the pivot point closer to the operative site - a significant advantage over traditional instruments. However, the cost of that flexibility is an increase in diameter. Designed as a wire/pulley system, pulleys can only be miniaturized so far before they force wires to turn too small of a corner, damaging the wire. Wristed movements in PSSB surgery likely require an alternative design to maintain the small size of the instruments.
The second challenge involves the number of instruments present in the surgical field. In traditional sinus surgery, the surgeon holds the telescope and operates with one instrument. This technique becomes less useful as the acuity of the surgery and the proximity to the skull base increases. "Two-handed" and "four-handed" surgery was developed with endoscope holders and co-surgeon participation to allow for bimanual instrumentation use - significantly improving dissection techniques. The ideal robot system would allow for easy visualization with the ability to control two or more instruments at the field. If those instruments are small enough, they would also not get in each other's way. "Sword fighting" between instruments becomes problematic as the size of the surgical field decreases.
The third design challenge concerns the facility of instrument exchange and entry through the nose. While the nose can be thought of as a dual "port" similar to current approaches to abdominal surgery, entry must be visualized so that the external nose is protected from cosmetic damage. Similarly, because visualization of instruments occurs only distal to the camera head, instrument placement at the surgical field must not result in damage to normal intranasal structures behind the visual field. Neurovascular control at the skull base requires fast and efficient instrument exchange. Just as in traditional transnasal endoscopic surgery, unintended injury to major vascular structures requires rapid response with clamps, cautery, or packing - that may require instrument exchange within the robot OR removal of the robot entirely. This is difficult to achieve with the da Vinci system given its current design. Undocking the robot to allow the surgeon unfettered access to the nose is challenging unless the surgical team is trained in this activity.
The robot must incorporate/cooperate with a image guidance system. Currently image-guidance is governed by either electromagnetic or optical technology. These two technologies impose different requirements on instrumentation. Optical systems require line of sight with the instruments, electromagnetic systems require care to reduce interference from other metallic structures around the surgical field - including other instrumentation. These challenges are significant, however, they are not insurmountable.
Perhaps one of the most challenging aspects of surgical robotics is haptic feedback. In traditional PSSB surgery, it is invaluable for the surgeon to feel the resistance of tissue and bone in deciding the next surgical move. With robotic surgery, this ability to feel is lost in the electromechanical mapping of the robot arm motions to the controls. In the engineering literature, researchers have identified two issues. The first issue is how to sense the occurring forces, i.e. finding appropriate small sensors and how to integrate them. The second issue is how to present the sensed information to the user, i.e. design of an interface that provides haptic feedback intuitively in a manner the user can perceive the information in a natural way. In her review, Okamura (18) demonstrates that those tasks are not yet perfected. However, it is a critical component of robotic development because the lack of haptic feedback at the skull base could limit the usefulness of a robotic platform in this sub-specialty.
Next we describe the development of new technology in robotic surgery.
Endonasal Robotic Surgery
In terms of surgical robotics research, many systems are under development (most at the research lab prototype phase) for natural orifice surgery or single port abdominal surgery, while comparatively few systems are targeting the PSSB surgery. For a survey of the state of the art in surgical robotics in general, see the following review papers (19,20). The reason that very few of these prior systems have been targeted at PSSB is likely due the smaller diameter of the nostril compared to other natural orifices (e.g. the throat, single abdominal port, etc.). Prior prototype robot systems (that is, non-commercial, non-FDA approved) developed for endonasal surgery have been intended to ensure safety during the initial bone drilling operations needed to expose the surgical site (21,22), assist in endoscope manipulation (23,24), or to control a camera with a steerable tip (conceptually similar to a small colonoscope or bronchosocope) for visual inspection of the sinus cavities (25).
PSSB Robot Prototype
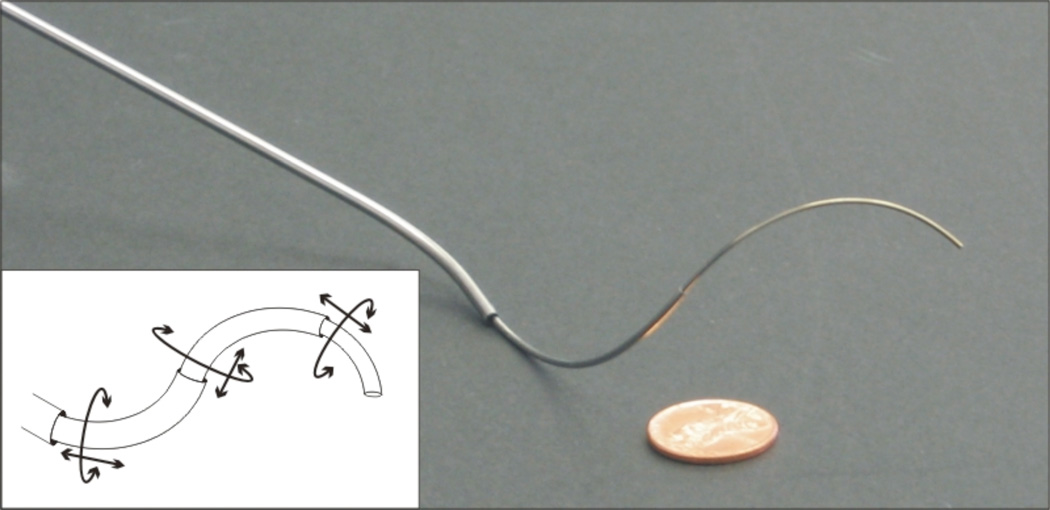
A new dedicated PSSB robot system is in development by our team of engineers and physicians at Vanderbilt University. This robotic system seeks to address limitations in current instrumentation by utilizing a new concentric tube technology (26,27). It is composed of several (usually three or more) flexible, precurved tubes that are nested within each other (see Figure 1). These tubes are made from Nitinol – the same high-strength, yet elastic metal used to make cardiac stents. Through linear insertion and axial rotation of each tube at its base, this robot achieves “tentacle-like” motion (meaning that it can elongate as well as bend controllably into complex curves). The diameter of the component tubes of this robot are typically 0.8–1.8mm, but can be as small as 0.2mm, or larger than 4mm in diameter, if desired. Hence, these robotic instruments are comparable to needles in size.
Figure 1.
A three-tube concentric tube continuum robot. The line drawing illustrates the degrees of freedom achievable through translation and rotation of each component tube. Reproduced with permission [23].
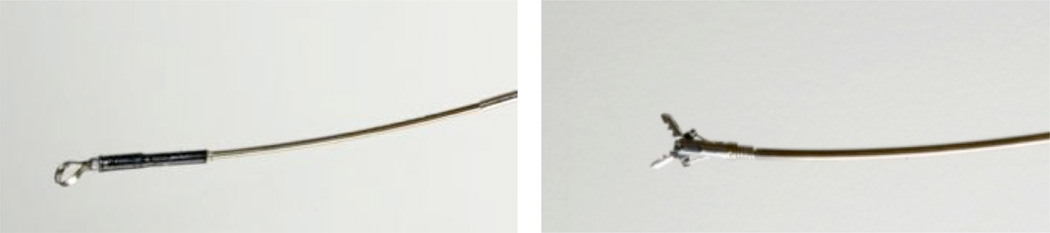
Regarding instrumentation, the innermost tube carries various tools, such as curettes, forceps, or aspiration (see Figure 2). The many existing instruments designed for PSSB surgery can be adapted to the new technology by mounting them at the tip of this tube. The small diameter of the concentric tube device combined with its dexterity means that up to approximately four instruments can be inserted and manipulated through a single nostril simultaneously with no danger of “sword fighting”.
Figure 2.
Example instruments for concentric tube continuum robots: ring curette (left) and forceps (right). Reproduced with permission [23].
One valuable feature of this device is that it offers a great deal of customizability. Its stiffness can be easily changed by changing tube wall thicknesses. Where it can reach can be changed by modifying individual tube curves, which can be created by a heat treatment process on the individual tubes. Also, the tubes are inexpensive enough that these can be disposable instruments.
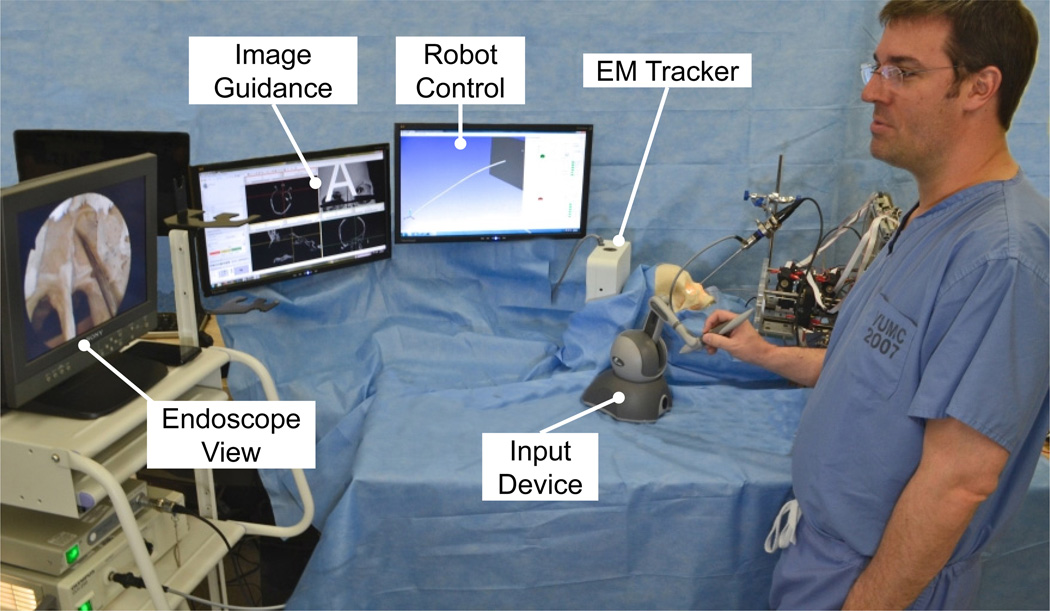
The surgeon control console for this new robot is similar that of the da Vinci surgical robot. Figure 3 shows the PSSB prototype system in a laboratory setup. As with any robot, motion scaling and tremor filtering are available features that can be adjusted to suit individual surgeon preference. Image-guidance is included in the PSSB prototype via electromagnetic tracking (Aurora, NDI) with visual screen displays created using open-source and freely available software (3D Slicer) (28). Visualization can be achieved using a rigid, straight endoscope, or by attaching a chip-tip camera to the end of one of the robots
Figure 3.
Paranasal sinuses and skull base (PSSB) robot prototype setup. The surgeon directly controls (teleoperates) the robot using the input device. Image guidance is achieved using electromagnetic (EM) tracking and a research interface to 3D Slicer. The movements of the surgeon with the input device’s stylus are directly mapped to robot’s motions. Reproduced with permission [23].
In a series of laboratory experiments with the PSSB robot prototype, we were able to achieve improved manipulation in the nasal cavity, because the device’s motion is not restricted by one single pivot point, such as the nasal entry point. The dexterous, tentacle-like motion along the shaft results in essentially zero pressure on structures near the entrance of the nose.
In a laboratory experiment using a human skull we were able to show a curette is effective for the resection of an artificial pituitary tumor (29). We anticipate that through optimal design of the component tubes for the specific anatomy (a topic of active research in the engineering community (27,30,31)), these robots can be made even more dexterous and well suited to the specific needs of PSSB.
The overall size of the PSSB robot’s motor pack that spins and inserts the various tubes is also much smaller than existing robots like the da Vinci. The small footprint of the PSSB robot will facilitate less crowding at the surgical field, allowing both the scrub nurse/tech and assistants to more easily maneuver near the patient. For the intraoperative system, we foresee the surgeon to be seated comfortably at a console, from which he/she can control the robotic instruments.
Lastly a robotic system can improve the ergonomics of the operation for the surgeon. Senior et al. (32) recently reported on the health effects of endoscopic endonasal surgery on the surgeon. Ergonomic comfort is often difficult to achieve during endoscopic endonasal surgery which often requires contortions from the physician that cause fatigue, and in may not be conducive to long-term neck and back health. In contrast, placing the surgeon in a seated position at a comfortable console has the potential to reduce fatigue and improve ergonomics.
It is important to note that the robotic system described here is a first prototype. Much refinement of control and system development, including design modifications to enable sterilization, are required before the robot will be ready for commercial production and marketing. The discussion above is provided to illustrate what we believe is the future of robotics for PSSB surgery, and provide an example of the system that we hope will one day become the gold standard instrument set for PSSB surgery.
Conclusions
The future of robotic PSSB surgery is promising. Based on the principles mentioned above, significant work must be done but current prototypes show potential. Perhaps the boundaries of the expanded endonasal approaches will be pushed as the robotic technology improves. The instruments we have now may not be the most efficient, and with expanded freedoms of movement in all planes more useful instruments may be developed. Through robotic technology, patients with previously "challenging" anatomy that require morbid open approaches may become candidates for endoscopic procedures. The limits of current technology are real, however collaboration between clinical surgeons and engineers promises to expand the applications of this exciting technology.
Key Points.
Robotic surgical systems for paranasal sinus and skull base surgery are achievable in the near future.
Current systems in existence are suboptimal to access the sinuses and skull base
The design of an ideal robotic system requires attention to specific anatomic limitations of the surgical area.
A radiographic navigation system must be paired with the robot for ideal surgical accuracy.
Patient care can be enhanced with more precise instrument control in the confined anatomy of the sinuses and skull base.
Footnotes
CONFLICTS OF INTEREST:
John S. Schneider – No conflicts
Jessica Burgner – No conflicts
Robert Webster – No conflicts
Paul Russell – No conflicts
References
- 1.Hanna EY, Holsinger C, DeMonte F, Kupferman M. Robotic endoscopic surgery of the skull base: a novel surgical approach. Archives of otolaryngology--head & neck surgery. 2007;133(12):1209–1214. doi: 10.1001/archotol.133.12.1209. [DOI] [PubMed] [Google Scholar]
- 2.O’Malley BW, Weinstein GS. Robotic skull base surgery: preclinical investigations to human clinical application. Archives of Otolaryngology--Head & Neck Surgery. 2007;133(12):1215–1219. doi: 10.1001/archotol.133.12.1215. [DOI] [PubMed] [Google Scholar]
- 3.Lee JYK, O’Malley BW, Newman JG, Weinstein GS, Lega B, Diaz J, et al. Transoral robotic surgery of the skull base: a cadaver and feasibility study. ORL. 2010;72(4):181–187. doi: 10.1159/000276937. [DOI] [PubMed] [Google Scholar]
- 4.Sammon J, Trinh Q-D, Menon M. Robotic radical prostatectomy: a critical analysis of surgical quality. Current Opinion in Urology. 2011 May;21(3):195–199. doi: 10.1097/MOU.0b013e328344e570. [DOI] [PubMed] [Google Scholar]
- 5.Trastulli S, Farinella E, Cirocchi R, Cavaliere D, Avenia N, Sciannameo F, et al. Robotic resection compared with laparoscopic rectal resection for cancer: systematic review and meta-analysis of short-term outcome. Colorectal Disease. 2012 Mar.14(4):e134–e156. doi: 10.1111/j.1463-1318.2011.02907.x. [DOI] [PubMed] [Google Scholar]
- 6.Lowery WJ, Leath CA, III, Robinson RD. Robotic surgery applications in the management of gynecologic malignancies. In: Stojadinovic A, Zeiger M, editors. J. Surg. Oncol. 5. Vol. 105. 2012. Mar. pp. 481–487. [DOI] [PubMed] [Google Scholar]
- 7.Endowrist© system [internet] http://www.intuitivesurgical.com/products/instruments/
- 8.Weinstein GS, O’Malley BW, Snyder W, Hockstein NG. Transoral robotic surgery: supraglottic partial laryngectomy. The Annals of otology, rhinology, and laryngology. 2007;116(1):19–23. doi: 10.1177/000348940711600104. [DOI] [PubMed] [Google Scholar]
- 9.Giulianotti PC, Addeo P, Buchs NC, Ayloo SM, Bianco FM. Robotic thyroidectomy: an initial experience with the gasless transaxillary approach. Journal of laparoendoscopic & advanced surgical techniques. Part A. 2012;22(4):387–391. doi: 10.1089/lap.2010.0380. [DOI] [PubMed] [Google Scholar]
- 10.Lee J, Chung WY. Current status of robotic thyroidectomy and neck dissection using a gasless transaxillary approach. Current opinion in oncology. 2012;24(1):7–15. doi: 10.1097/CCO.0b013e32834cb813. [DOI] [PubMed] [Google Scholar]
- 11.Ohio State Skull Base Robotics [internet] http://cancer.osu.edu/mediaroom/releases/Pages/Ohio-State-Surgeons-Pioneer-Removal-Of-Skull-Based-Tumors-Through-The-Nose-And-Mouth,-Sparing-Patients-From-Open-Brain-Surg.aspx.
- 12. Dallan I, Castelnuovo P, Seccia V, Battaglia P, Montevecchi F, Tschabitscher M, et al. Combined transnasal transcervical robotic dissection of posterior skull base: feasibility in a cadaveric model. Rhinology. 2012;50(2):165–470. doi: 10.4193/Rhino11.079. Feasability study on using current robotic technology at the skull base.
- 13.Russell PT, Weaver KD. Anterior endoscopic skull-base surgery getting started: an otolaryngologist’s perspective. Current Opinion in Otolaryngology & Head and Neck Surgery. 2007;15(1):1–5. doi: 10.1097/MOO.0b013e328013f46a. [DOI] [PubMed] [Google Scholar]
- 14.Castelnuovo P, Dallan I, Battaglia P, Bignami M. Endoscopic endonasal skull base surgery: past, present and future. European Archives of Oto-Rhino-Laryngology. 2010;267(5):649–663. doi: 10.1007/s00405-009-1196-0. [DOI] [PubMed] [Google Scholar]
- 15. Wagenmann M, Schipper J. The transnasal approach to the skull base. From sinus surgery to skull base surgery. GMS Current Topics in Otorhinolaryngology, Head and Neck Surgery. 2011;10:Doc08. doi: 10.3205/cto000081. Good paper on the transnasal approach to the skull base.
- 16.Nogueria JR, Stamm A, Vellutini E. Otolaryngologic Clinics of NA. 3. Vol. 43. Elsevier Ltd; 2010. Jun. Evolution of Endoscopic Skull Base Surgery, Current Concepts, and Future Perspectives; pp. 639–652. [DOI] [PubMed] [Google Scholar]
- 17.Harvey RJ, Gallagher RM, Sacks R. Otolaryngologic Clinics of NA. 3. Vol. 43. Elsevier Ltd; 2010. Jun. Extended Endoscopic Techniques for Sinonasal Resections; pp. 613–638. [DOI] [PubMed] [Google Scholar]
- 18.Okamura AM. Haptic Feedback in Robot-Assisted Minimally Invasive Surgery. Curr Opin Urol. 2009 Jan;19(1):102–107. doi: 10.1097/MOU.0b013e32831a478c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dogangil G, Davies BL, Rodriguez y Baena F. A review of medical robotics for minimally invasive soft tissue surgery. Proceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine. 2010;224:653–679. doi: 10.1243/09544119JEIM591. [DOI] [PubMed] [Google Scholar]
- 20.Okamura A, Mataric M, Christensen H. Medical and Health-Care Robotics. IEEE Robotics & Automation Magazine. 2010;17:26–37. [Google Scholar]
- 21.Wurm J, Dannenmann T, Bohr C, Iro H, Bumm K. Increased safety in robotic paranasal sinus and skull base surgery with redundant navigation and automated registration. International Journal of Medical Robotics and Computer Assisted Surgery. 2005;01(03):42. doi: 10.1002/rcs.26. [DOI] [PubMed] [Google Scholar]
- 22.Xia T, Baird C, Jallo G, Hayes K, Nakajima N, Hata N, et al. An integrated system for planning, navigation and robotic assistance for skull base surgery. International Journal of Medical Robotics and Computer Assisted Surgery. 2008;4(4):321–330. doi: 10.1002/rcs.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nimsky C, Rachinger J, Iro H, Fahlbusch R. Adaptation of a hexapod-based robotic system for extended endoscope-assisted transsphenoidal skull base surgery. Minimally Invasive Neurosurgery. 2004;47(1):41–46. doi: 10.1055/s-2003-812465. [DOI] [PubMed] [Google Scholar]
- 24. Eichhorn KWG, Bootz F. Clinical Requirements and Possible Applications of Robot Assisted Endoscopy in Skull Base and Sinus Surgery. In: Pamir MN, Seifert V, Kiris T, editors. Acta Neurochirurgica. Vol. 109. Vienna: Springer Vienna; 2011. pp. 237–240. Excellent paper that demonstrates some of the issues surrounding robotic surgery at the skull base.
- 25.Yoon H-S, Oh SM, Jeong JH, Lee SH, Tae K, Koh K-C, et al. Active bending endoscope robot system for navigation through sinus area; IEEE/RSJ International Conference on Intelligent Robots and Systems; 2011. pp. 967–972. [Google Scholar]
- 26.Rucker DC, Jones BA, Webster RJ., III A Geometrically Exact Model for Externally Loaded Concentric-Tube Continuum Robots. IEEE Transactions on Robotics. 2010;26(5):769–780. doi: 10.1109/TRO.2010.2062570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Burgner J, Swaney PJ, Rucker DC, Gilbert HB, Nill ST, Russell PT, et al. A bimanual teleoperated system for endonasal skull base surgery; IEEE/RSJ International Conference on Intelligent Robots and Systems; 2011. pp. 2517–2523. Paper that describes the robot in development at Vanderbilt University.
- 28.3d Slicer [Internet] 2012 Available from: http://www.slicer.org. [Google Scholar]
- 29.Gilbert HB, Swaney PJ, Burgner J, Weaver KD, Russell PT, III, Webster RJ., III A Feasibility Study on the use of Concentric Tube Continuum Robots for Endonasal Skull Base Tumor Removal; The Hamlyn Symposium on Medical Robotics; 2012. [Google Scholar]
- 30.Bedell C, Lock J, Gosline A, Dupont PE. Design Optimization of Concentric Tube Robots Based on Task and Anatomical Constraints; IEEE International Conference on Robotics and Automation; 2011. pp. 398–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anor T, Madsen JR, Dupont P. Algorithms for Design of Continuum Robots Using the Concentric Tubes Approach: A Neurosurgical Example; IEEE International Conference on Robotics and Automation; 2011. pp. 667–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Little RM, Deal AM, Zanation AM, McKinney K, Senior BA, Ebert CS., Jr Occupational Hazards Of Endoscopic Surgery. Int Forum Allergy Rhinol. 2012 May-Jun;2(3):212–6. doi: 10.1002/alr.20108. Paper that describes fatigue and posture problems associated with endoscopic surgery of the nose.