Abstract
Virtual reality (VR) has been used by clinicians to manage pain in clinical populations. This study examines the use of VR as a form of distraction for dental patients using both subjective and objective measures to determine how a VR system affects patients' reported anxiety level, pain level, and physiological factors. As predicted, results of self-evaluation questionnaires showed that patients experienced less anxiety and pain after undergoing VR treatment. Physiological data reported similar trends in decreased anxiety. Overall, the favorable subjective and objective responses suggest that VR distraction systems can reduce discomfort and pain for patients with mild to moderate fear and anxiety.
Introduction
One of the most challenging aspects of dental care that medical practitioners face today is the treatment of patient pain.1 Despite advances in dental technologies and treatment, many people still avoid or delay dental care because of the fear and anxiety of pain.2 Analgesics have been the mainstream solution for alleviating pain in the past. However, medications are often not effective. More recently, advanced technologies have integrated both the knowledge of the mechanisms of pain medications and techniques in behavioral medicine. These advances have moved toward using distraction and hypnosis techniques to treat pain.3
Pain perception has a strong psychological component. In order to experience pain, conscious attention is required.2 Distraction has been found to take a patient's attention away from pain. Attention given to pain often determines not only the level of pain being reported, but also the distress levels. By encouraging a patient to focus his/her attention on other thoughts, less attention is available for the pain.4,5 Virtual reality (VR) utilizes advanced technologies to create virtual environments (VE) that allow patients to be immersed in an interactive, simulated world.6 These advanced systems interact at many levels with the VE, stimulating sights, sounds, and motion to encourage immersion in the virtual world to enhance distraction from pain.7
Other studies have also shown that involving the patient in a VE reduced their reported levels of pain during medical procedures such as chemotherapy, physical therapy, burn wound changes, and surgery (see Table 1).8–11 In one study where children either played video games or navigated through a VE while receiving wound care for their burns, exposure to VR lessened their reported pain ratings as compared with playing video games.12 In another controlled study, adult burn patients undergoing physical therapy reported less pain while involved in VR than those that only participated in standard physical therapy.13 Evidence shows that VR is effective in reducing pain in children with cancer, as chemotherapy-related symptom distress was reduced significantly immediately after using VR during treatment.14 Specifically for dental work, another clinical study observed that dental patients undergoing plaque removal below their gum line experienced considerable reduction in pain when using VR compared to participants that watched a movie and to participants that did not have any type of distraction.15
Table 1.
Previous Research of Virtual Reality (VR) Distraction for Dental Procedures
| Title | Method | Results |
|---|---|---|
| Improving Dental Experiences Using Virtual Reality Distractions: A Simulations Study16 | Participants (n=69) were randomly assigned to one of three VR conditions: active, passive, or control. Each participant was labeled as high or low dentally anxious prior to dental treatment with the VR application. | VR distraction affected on concurrent experiences, such as perceived control, as well as memories after the dental experience had ended. Participants with higher anxiety experienced greater reduction in memory vividness. |
| The Impact of Virtual Reality Distraction on Pain and Anxiety during Dental Treatment in 4–6 Year Old Children: A Randomized Controlled Clinical Trial17 | 120 healthy children aged 4–6 years with no previous anxiety disorder were randomly divided into two even groups. The study consisted of three consecutive treatment sessions. The first visit consisted of fluoride therapy. In the next sessions, the groups received restorative treatment with and without VR eyeglasses in a randomized single blind controlled crossover fashion. Then at the end of each session, the subjects' pain severity was assessed using Wong Baker FACES Pain Rating Scale, and state anxiety was measured by Faces version of the Modified Child Dental Anxiety Scale [MCDAS (f )]. | There was a significant decrease in pain perception (p<0.001) and state anxiety scores (p<0.001) with the use of VR eyeglasses during dental treatment. |
| Virtual Reality Distraction for Pain Control During Periodontal Scaling and Root Planing Procedures18 | The authors recruited 38 patients. They used a within-patient/split-mouth design. Patients received scaling and root planing procedures (SRP) under three treatment conditions in three quadrants. The three conditions were control, watching a movie, and VR. After each SRP procedure, patients responded to questions about their discomfort and/or pain by using a visual analog scale (VAS) (range=0 to 10 in which lower numbers indicate less pain or discomfort). The authors also recorded patients' blood pressure (BP) and pulse rate (PR). Patients were asked which of the three treatment modalities they preferred. | The mean (±standard deviation) VAS scores for five questions pertaining to control, movie, and VR were 3.95±2.1, 2.57±1.8, and 1.76±1.4 respectively. Paired t tests revealed that VAS scores were significantly lower during VR compared with the movie (p<0.001) and control (p<0.001) conditions. Similarly, BP and PR were lowest during VR, followed by the movie and control conditions. Patients reported that they preferred the VR condition. |
| The Effect of Virtual Reality During Dental Treatment on Child Anxiety and Behavior19 | The behavior, anxiety, and heart rate of 26 children aged 5–7 years were evaluated for the first 5 minutes of two restorative treatment visits. Thirteen children viewed VR at their first restorative visit and not the second, and 13 children viewed VR at the second restorative visit and not the first. Before and immediately following the restorative visits, each child was instructed to draw a human figure. The restorative appointments were video recorded and heart rate monitored. The Koppitz method of evaluating drawings was used to measure anxiety. The Frankl behavior rating scale was used to evaluate behavior. | Differences (ANOVA) in behavior (p≤0.50) and anxiety (p≤0.65) were not significant. The overall pulse rate was significantly lower (ANOVA; p≤0.001) when the child was wearing glasses and viewing VR. |
| The Effectiveness of Virtual Reality for Dental Pain Control: A Case Study15 | Two patients (aged 51 and 56 years old) with adult periodontitis—a chronic, progressive inflammatory disease that affects gums, ligaments, and bones around the teeth—were studied in the treatment room of a periodontist. Each patient received periodontal scaling and root planing (scraping off/removing plaque deposits below the gum line, hereafter referred to as scaling) under three treatment conditions: (1) VR distraction, (2) movie distraction, and (3) a no-distraction control condition. Condition order was randomized and counterbalanced. For each of the three treatment conditions, five visual analog pain scores for each treatment condition served as the dependent variables. On 0–10 labeled scales, both patients provided sensory and affective pain ratings, and subjective estimates of time spent thinking about his pain during the procedure. | For patient 1, mean pain ratings were in the severe range while watching a movie (7.2) or no distraction (7.2), but in the mild pain range (1.2) during the VR condition. Patient 2 reported mild to moderate pain with no distraction (M=4.4), mild pain while watching the movie (M=3.3), and essentially no pain while in VR (M=0.6) during his periodontal scaling. |
Research involving the concept of distraction has shown that techniques used in the past such as concentrating on deep breathing or watching a movie are less effective than using VR. This study examines the efficacy of using VR to control dental pain using both patient reported surveys and physiological measurements to evaluate fear and pain before and after dental treatment. Dental fear has been measured with questionnaires such as the Dental Anxiety Scale and Dental Fear Survey, as well as the Dental Fear Interview. While there are numerous self-report instruments that measure various aspects of the sensory, affective, and evaluative components of pain, only a few tools have been developed that directly assess fear and anxiety associated with pain. This study will integrate both subjective and objective variables to determine a more effective way of measuring and reducing both pain and distress.
Methods
Setting and patients
We recruited five adult patients for the study on a voluntary basis as they came for their dental treatments at the Scripps Center for Dental Care in La Jolla, CA (Dr. John F. Weston, D.D.S.) (see Fig. 1).
FIG. 1.

Patient in treatment room.
Outcome measures
Patients first completed the Dental Anxiety Scale and Amount of Fear Scale. The Dental Anxiety Scale is a 4-item questionnaire that asks about fear of dental treatment. The Amount of Fear Scale is a 45-item, Likert-type (1–5 scale) verbal report instrument used to assess dental fear. The survey provides a total dental fear score.
A post-experience questionnaire was created by the investigators to assess patient treatment preference and effects of the VR distraction system. This questionnaire includes the presence questionnaire (from Usoh et al. “Using Presence Questionnaires in Reality,” Witmer & Singer, Vs. 3.0), and STAIP-AD Test form Y (from Consulting Psychologists Press).
The Procomp+ biofeedback device by Thought Technology was used to assess physiological measures. This device is an advanced biofeedback and psychophysiological data acquisition system. It measures electromyogram (EMG), temperature, galvanic skin response (GSH), electroencephalogram (EEG), heart rate variability, heart rate, and respiration rate (see Fig. 2).
FIG. 2.
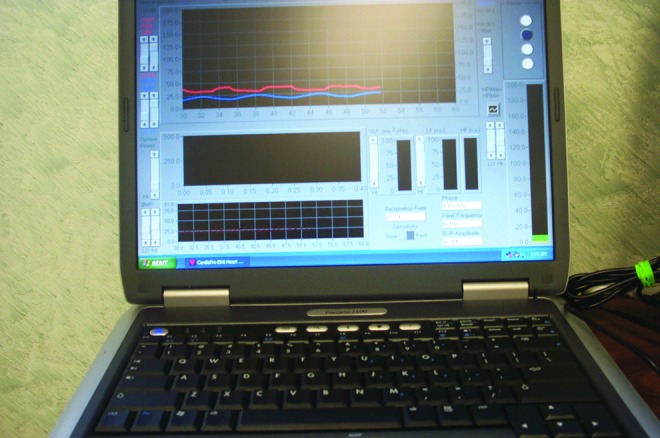
Psychophysiological monitoring and biofeedback equipment.
Procedures
Before we began treatment, the patients completed the questionnaires. We also recorded demographic information, the date of last treatment, and the details about the dental procedure. We attached seven sensors to the patients' fingers, abdomens, and arms to gather physiological information. The clinician performed the dental treatment without the use of the VR distraction system for 5 minutes (see Figs. 3 and 4) and then performed it with use of the VR distraction system for 5 minutes (see Fig. 5).
FIG. 3.

Measurement without the virtual reality (VR) distraction system.
FIG. 4.

Biofeedback sensors and wireless trackball.
FIG. 5.

Measurement with VR distraction system.
The VEs included relaxing nature worlds where the patients could navigate through beaches, forest, mountains, and other pleasant areas. The patients self-navigated to provide a further sense of control.
Results
Standardized questionnaires
Scores for the pre/post questionnaires, including their sub-scales, are shown in Table 2.
Table 2.
Patient Scores Between Pre- and Post- Questionnaire
| Pre questionnaire | ||||
|---|---|---|---|---|
| Patient | Amount of fear | Self-Eval1 | Self-Eval2 | Absorption |
| P1 | 83 | 39 | 10 | 16 |
| P2 | 113 | 22 | 27 | 16 |
| P3 | 136 | 25 | 16 | 18 |
| P4 | 144 | 30 | 19 | 12 |
| P5 | 111 | 21 | 17 | 16 |
| Mean | 117.4 | 27.4 | 17.8 | 15.6 |
| Post questionnaire | ||||
|---|---|---|---|---|
| Patient | Post_Exp | Self-Eval1 | Self-Eval2 | Presence |
| P1 | 37.5 | 40 | 9 | 166 |
| P2 | 55 | 23 | 29 | 127 |
| P3 | 40 | 31 | 11 | 179 |
| P4 | 56 | 31 | 17 | 136 |
| P5 | 45 | 17 | 25 | 138 |
| Mean | 46.7 | 28.4 | 18.2 | 149.2 |
| Difference in scores between pre and post questionnaires | ||
|---|---|---|
| Patient | Part I | Part II |
| P1 | 1 | −1 |
| P2 | 1 | 2 |
| P3 | 6 | −5 |
| P4 | 1 | −2 |
| P5 | −4 | 8 |
| Mean | 1 | 0.4 (−1.5)* |
0.4 for all patients; −1.5 for patients 1–4.
We evaluated the differences between pre/post self-evaluation scores (post−pre score=changes) with the t test (see Table 3).
Table 3.
Statistical Analysis of Pre and Post Questionnaires
| Mean | Standard deviation | n | Standard error | Reference | t Value | df | p | |
|---|---|---|---|---|---|---|---|---|
| Pre questionnaire | 1.000000 | 3.535534 | 5 | 1.581139 | 0.00 | 0.632456 | 4 | 0.280719 |
| Post questionnaire | 0.400000 | 4.929503 | 5 | 2.204541 | 0.00 | 0.181444 | 4 | 0.864843 |
| Post questionnaire (without patient 5) | −1.500000 | 2.886751 | 4 | 1.443376 | 0.00 | −1.03923 | 3 | 0.187548 |
For part I of the self-evaluation questionnaire (Ho:u=0, Ha:u<0), the p value is 0.56. This is strong evidence to support that the true mean of the change is >0, that is, treatment increased the scores for patients. Data from part II has a p value of 0.1875 (except patient 5 data; it is obvious that the value 8 is an outlier), supporting that using the VR distraction system decreased the anxiety for patients.
Physiology
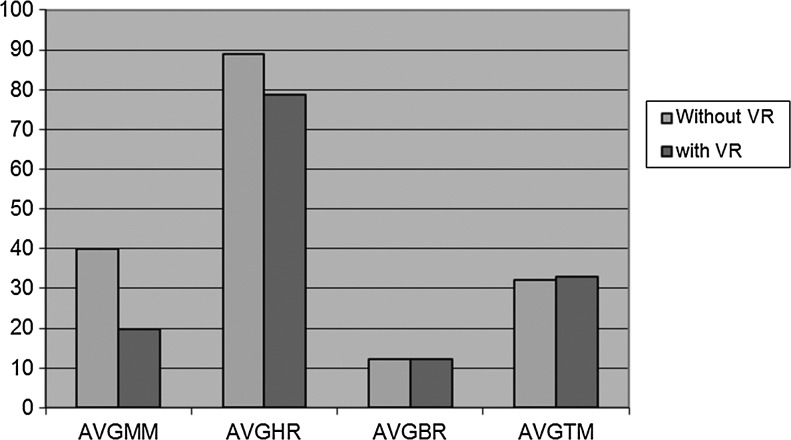
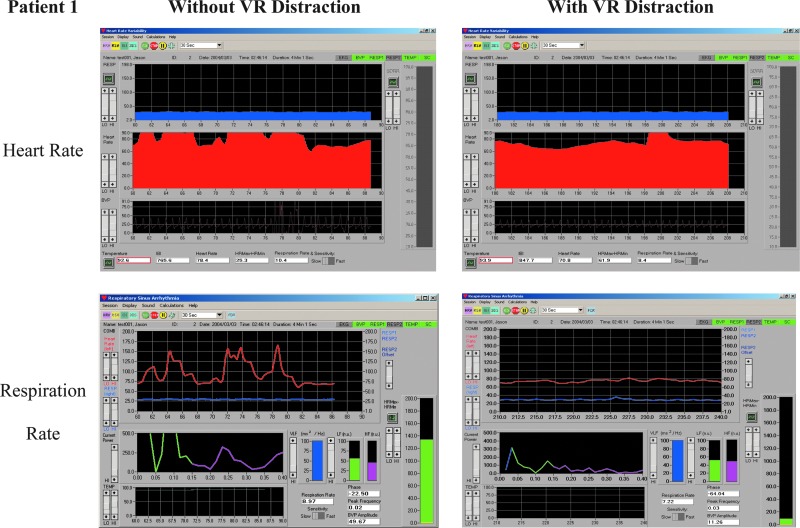
We analyzed physiological measures (such as the heart rate and respiration rate) along with order and condition (after use of the VR distraction system and after nonuse of the system). In these analyses, several significant effects were shown (see Figs. 6 and 7; Tables 4–6).
FIG. 6.
Results show a trend of factors related to fear and anxiety reduction with VR distraction.
FIG. 7.
Evaluation outcome chart (heart rate, respiration rate) example.
Table 4.
Statistical Variable Definitions and Abbreviations
| SDNN | Standard deviation on the NN intervals (NN=normalized R to R=normalized IBI) |
| VLF | Power in the VLF bandwidth (0.0033–0.04 Hz) |
| LFN | Power in the LF bandwidth (0.04–0.15 Hz), in normalized unit |
| HFN | Power in the HF bandwidth (0.15–0.4 Hz), in normalized unit |
| LF/HF | Ratio LF/HF |
| Total Power | Total power in the 0.0033–0.4 Hz bandwidth |
| AvgMM | Average HR Max–HR Min value |
| AvgHR | Average heart rate |
| AvgBR | Average respiration (breathing) rate |
| AvgTM | Average temperature |
Table 5.
EKG Statistical Data Without VR Distraction
| SDNN | VLF | LFN | HFN | LF/HF | POWER | |
|---|---|---|---|---|---|---|
| Patient 1 | 322.91 | 12,726.91 | 56.46 | 43.54 | 1.3 | 32,431.2 |
| Patient 2 | 119.85 | 905.51 | 36.18 | 63.82 | 0.57 | 3,069.24 |
| Patient 3 | 194.59 | 1,514.26 | 49.41 | 50.59 | 0.98 | 6,206.21 |
| Patient 4 | 149 | 508.68 | 33.17 | 66.83 | 0.5 | 1,885.13 |
| Patient 5 | 116.04 | 1,613.61 | 44.59 | 55.41 | 0.8 | 5,730.46 |
| Mean | 180.478 | 3,453.794 | 43.962 | 56.038 | 0.83 | 9,864.448 |
Table 6.
EKG Statistical Data With VR Distraction
| SDNN | VLF | LFN | HFN | LF/HF | POWER | |
|---|---|---|---|---|---|---|
| Patient 1 | 350.46 | 7,080.83 | 54.97 | 45.03 | 1.22 | 34,153.53 |
| Patient 2 | 54.07 | 385.69 | 73.41 | 26.59 | 2.76 | 947.02 |
| Patient 3 | 71.6 | 394.2 | 59.78 | 40.22 | 1.49 | 1,518.05 |
| Patient 4 | 116.61 | 2,095.33 | 60.1 | 39.9 | 1.51 | 2,525.88 |
| Patient 5 | 81.59 | 739.1 | 46.39 | 53.61 | 0.87 | 1,166.04 |
| Mean | 134.866 | 2,139.03 | 58.93 | 41.07 | 1.57 | 8,062.104 |
Within the EKG data, LFN increased an average of 14.968 for four of the five patients after VR distraction. The average increase of the LF frequency band most likely indicates effectiveness of the VR distraction in reducing anxiety.
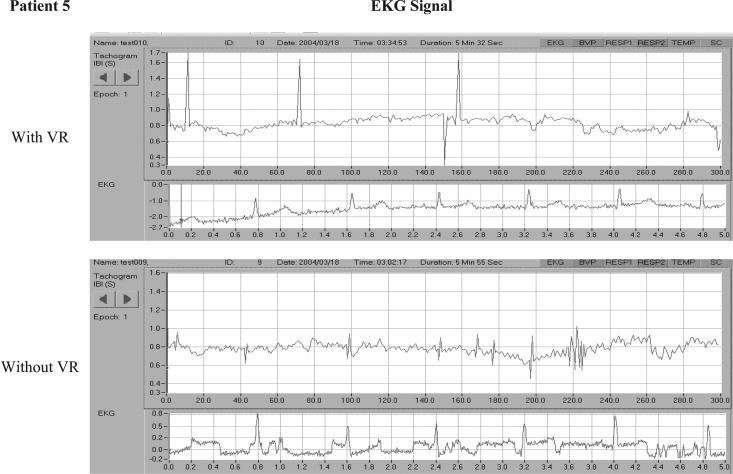
HRV is characterized by three main components: the high frequency (HF) component (0.15–0.40 Hz) measures the influence of the vagus nerve in modulating the sinoatrial node. The low frequency (LF) component (0.04–0.15 Hz) provides an index of sympathetic effects on the heart, particularly when measured in normalized units. The very low frequency (VLF) component (0.003–0.04 HZ) reflects the influence of several factors on the heart, including chemoreceptors, thermoreceptors, the renin-angiotensin system, and other nonregular factors. Almost all of the variability from a short-term spectral analysis of HRV is captured in these three components. An example of one of the patient's EKG data is shown in Figure 8 to visualize the comparative features.
FIG. 8.
EKG of patient 5 with and without VR distraction.
Discussion
An inexpensive, commercially available VE could have a significant impact in reducing perceived pain involved in a variety of medical procedures.
The physiological results of this research suggest that the use of the VR distraction system may be a beneficial option for patients with mild to moderate fear and anxiety associated with dental treatments. This system may be a useful adjunct in dental offices to help reduce anxiety, discomfort, boredom, and the time required to perform routine dental procedures. It allows them to relax by allowing them to navigate to another location while still physically remaining in the dental office.
Additional research exploring the mechanism by which VR distraction is achieved will be needed. There is much room for improving “presence and realism” in future VR applications specifically designed for treating pain. New virtual worlds, custom built to be more immersive, could produce even larger reductions in pain. Such new worlds can take advantage of the versatility of VR software. On a clinical level, several observations were noted by the clinical staff and from the survey results to improve on existing problems with the design of the study (see Table 7).
Table 7.
Observed and Reported Clinical Improvements
| 1 | Set up virtual equipment in a spacious area to allow room to operate freely |
| 2 | Ensure the patient is familiarized with the virtual environment (VE) before beginning operations |
| 3 | Head-mounted display size and compatibility are essential for a smooth operation, as it may be difficult to adjust mid-operation |
| 4 | Offer a wide range of VE to accommodate the varying tastes of patients |
| 5 | Use disposable covers between patients to maintain aseptic technique while saving time |
The cost of an immersive VR system has dropped dramatically since the mid-1990s, and additional price reductions are inevitable. At the same time, the quality and portability of VR has increased dramatically, benefiting from the enormous improvements in more conventional computer technology (e.g., cheaper memory, cheap and fast graphics accelerators, higher information processing capabilities of the hardware, and a dramatic maturation in the quality of VR world building software commercially available).
To summarize, the present study provides encouraging initial support for the use of VR as a technique for controlling fear and anxiety during dental procedures. Additional empirical research will be needed to determine whether VR can become a viable form of fear and anxiety control during dental treatments. Techniques that prove effective for treating dental pain will likely prove effective for other painful procedures.
Acknowledgments
We thank the National Institute on Drug Abuse, National Institutes of Health for partial funding of this project. We also thank the participants who were willing to spend time with our clinical team.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Cohen LA, Harris SL, Bonito AJ, et al. . Coping with toothache pain: a qualitative study of low-income persons and minorities. Journal of Public Health Dentistry 2007; 67:28–35 [DOI] [PubMed] [Google Scholar]
- 2.Locker D. Psychosocial consequences of dental fear and anxiety. Community Dental Oral Epidemiology 2003; 31:144–151 [DOI] [PubMed] [Google Scholar]
- 3.Schmitt YS, Hoffman HG, Sharar SR. A randomized, controlled trial of immersive virtual reality analgesia during physical therapy for pediatric burn injuries. Burns 2011; 37:61–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hodes RL, Howland EW, Lightfoot N, et al. . The effects of distraction on responses to cold pressor pain. Pain 1990; 41:109–114 [DOI] [PubMed] [Google Scholar]
- 5.Miron D, Duncan GH, Bushnell MC. Effects of attention on the intensity and unpleasantness of thermal pain. Pain 1989; 39: 345–352 [DOI] [PubMed] [Google Scholar]
- 6.Sharar SR, Miller W, Patterson DR. Applications of virtual reality for pain management in burn-injured patients. Expert Review of Neurotherapeutics 2008; 8:1667–1674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wiederhold MD, Wiederhold BK. Virtual reality and interactive simulation for pain distraction. Pain Medicine 2007; 8:S182–188 [Google Scholar]
- 8.Vazquez JLM, Santander A, Gao K, et al. . Using cybertherapy to reduce postoperative anxiety in cardiac recovery intensive care units. Journal of Anesthesia & Clinical Research 2013; 4:363 [Google Scholar]
- 9.Mosso JL, Rizzo S, Wiederhold B, et al. . Cybertherapy—new applications for discomfort reductions. Surgical care unit of heart, neonatology care unit, transplant kidney care unit, delivery room-cesarean surgery and ambulatory surgery, 27 case reports. Studies in Health Information & Informatics 2007; 125:334–336 [PubMed] [Google Scholar]
- 10.Wiederhold BK, Wiederhold MD. Managing pain in military populations with virtual reality. NATO Science for Peace & Security Series—E: Human & Societal Dynamics 2012; 91:75–93 [Google Scholar]
- 11.Mühlberger A, Wieser MJ, Kenntner-Mabiala R, et al. . Pain modulation during drives through cold and hot virtual environments. CyberPsychology & Behavior 2007; 10:516–522 [DOI] [PubMed] [Google Scholar]
- 12.Hoffman HG, Doctor JN, Peterson DR, et al. . Virtual reality as an adjunctive pain control during burn wound care in adolescent patients. Pain 2000; 85:305–309 [DOI] [PubMed] [Google Scholar]
- 13.Hoffman HG, Patterson DR, Carrougher GJ. Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: a controlled study. Clinical Journal of Pain 2000; 16:244–250 [DOI] [PubMed] [Google Scholar]
- 14.Schneider SM, Workman ML. Virtual reality as a distraction intervention for older children receiving chemotherapy. Journal of Pediatric Nursing 2000; 26:593–597 [PubMed] [Google Scholar]
- 15.Hoffman HG, Garcia-Palacios A, Patterson DR, et al. . The effectiveness of virtual reality for dental pain control: a case study. CyberPsychology & Behavior 2001; 4:527–535 [DOI] [PubMed] [Google Scholar]
- 16.Tanja-Dijkstra K, Pahl S, White MP, et al. . Improving dental experiences by using virtual reality distraction: a simulation study. PLoS One 2014; 9:e91276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Asl Aminabadi N, Erfanparast L, Sohrabi A, et al. . The impact of virtual reality distraction on pain and anxiety during dental treatment in 4–6 year-old children: a randomized controlled clinical trial. Journal of Dental Research, Dental Clinics, Dental Prospects 2012; 6:117–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Furman E, Jasinevicius TR, Bissada NF, et al. . Virtual reality distraction for pain control during periodontal scaling and root planing procedures. Journal of American Dental Association 2009; 140;1508–1516 [DOI] [PubMed] [Google Scholar]
- 19.Sullivan C, Schneider PE, Musselman RJ, et al. . The effect of virtual reality during dental treatment on child anxiety and behavior. ASDC Journal of Dentistry for Children 2000; 67:193–196 [PubMed] [Google Scholar]