Abstract
Purpose: To assess the impact of listening to preferred music on relieving male patients' pain and anxiety during flexible cystoscopy.
Patients and Methods: A total of 124 male patients were admitted to our hospital for flexile cystoscopy by a single urologist between January 2013 and September 2013 and randomized to two equal groups. Group 2 included 62 patients who could select and listen to their preferred music during flexible cystoscopy. Group 1 included 62 patients who were unable to listen to the music. All patients were administered the same amount of lidocaine (10 mL) for 3 minutes for local anesthesia before flexible cystoscopy. A visual analog scale (VAS) ranging from 0 to 10 was used to assess patients' pain feeling after the cystoscopy procedure. Anxiety levels were calculated according to the State Instrument of State-Trait Anxiety Inventory (STAI-S), and the pulse rate were recorded 5 minutes before and immediately after the procedure. The duration of the procedure of each group were also analyzed.
Results: Statistically significant differences were detected between group 1 and group 2 in the mean pain score on VAS (2.53±1.34 vs 1.63±1.09, P=0.002, Mann-Whitney U test), mean postprocedural State Anxiety Inventory pain score (39.4±6.5 vs 34.5±5.8), and postprocedural pulse rate (79.8±5.5 vs 76.0±7.3) (P<0.001 for both, t test). Patients who listened to their preferred music experienced less discomfort and lower anxiety at cystoscopy. Patient age, duration of the procedure, preprocedural STAI-S, and preprocedural pulse rate of each group were comparable.
Conclusion: Listening to preferred music during flexible cystoscopy is an easy way to improves male patients' comfort and reduce their anxiety. It could be recommended for male patients.
Introduction
Flexible cystoscopy is widely used as a routine procedure in many urology institutes. Flexible cystoscopy could significantly decrease patients' pain and discomfort and make sedation for cystoscopy unnecessary when compared with rigid cystoscopy1,2; however, it can still be painful and morbidity still could be observed when this procedure was performed, especially in male patients.3 Because the amount of patients undergoing this procedure is increasing year by year,4 improving patients' comfort during flexible cystoscopy has been an issue of great importance. In recent years, music has been advocated as a therapeutic method to manage patients' pain and anxiety.5 The study by Lin and associates6 had confirmed that patients' spiritual, emotional, and psychological feelings could be satisfied by music intervention, and music engagement became more and more popular in perioperative care as an adjuvant therapy.7
To our knowledge, there has been no research on reducing paitents' discomfort and anxiety during flexible cystoscopy by music intervention. Because male patients suffer more discomfort than females3 and most female patients undergo cystoscopy by rigid cystoscope at our institute, we performed a randomized controlled study for male patients to estimate the effect of music engagement on responses to pain and anxiety during flexible cystoscopy.
Patients and Methods
Participants, exclusions, and ethics statement
One hundred and twenty-four male patients admitted to our institute for flexile cystoscopy by the same urologist between January 2013 and September 2013 were enrolled. Ethics review was approved and written approval was obtained from the Institutional Review Board of our hospital (Shanghai Changhai Hospital); full written and informed consent was provided by every patient. Indications for flexible cystoscopy were hematuria and surveillance for bladder tumors. Exclusion criteria were other procedures such as urethral dilation, biopsies, stent placement, and stent removal. Patients undergoing manipulation of the lower urinary tract, patients with a history of chronic pelvic pain syndrome, or with a history of diabetes or arrhythmia were also excluded from the study.
Randomization and procedure
All 124 patients were informed of this study, then randomized into two equal groups. A research nurse had a random number list to ensure an equal number in two groups. Patients were randomized as follows: Group 2 included 62 patients who could select and listen to their preferred music during flexible cystoscopy. Four major kinds of music—classical music, Chinese folk music, popular music, and foreign music—were ready for patient selection. A wide variety of CD and audio equipment was available in the operating room. Group 1 included 62 patients who were unable to listen to the music. The same volume of 10 mL 2% lidocaine jelly was administrated intraurethrally for 3 minutes before flexible cystoscopy for every patient as local anesthesia. The instrument for flexible cystoscopy included a 16F flexible cystoscope (Olympus CYF-5A), a color video monitor (Olympus OEV-191H), and a digital camera (Olympus OTV-S7).
Pain measures
A visual analog scale (VAS) ranging from 0 to 108 was used to evaluate pain. After flexible cystoscopy, patients wrote down their pain feeling on a VAS form. According to the Collins definition, “no pain” was a score of 0, “mild pain” was a score of 1 to 3, “moderate pain” was a score of 4 to 7, and “severe pain” was a score of 8 to 10.8 The duration of the procedure of each group was also recorded and analyzed.
Anxiety measures
Anxiety levels were calculated 5 minutes before and immediately after the procedure according to the State Instrument of State-Trait Anxiety Inventory (STAI-S).9 STAI-S is a scale commonly used to measure the trait and state anxiety that contains 20 self-report items. It can measure tension, worry, and apprehension that the respondent experiences at this moment or in current circumstances (state anxiety). The respondent reports on the frequency that he/she experiences symptoms on a 4-point scale (1: not at all; 2: somewhat; 3: moderately so; 4: very much so), and higher score means a greater anxiety level.9 The duration of the procedure and pulse rate were recorded and analyzed. A research nurse was in charge of recording the patients' pulse rate 5 minutes before and immediately after the procedure by taking the pulse.
Data analyses
SPSS 13.0 was used for data analysis. The Mann-Whitney U test was used to compared the VAS score between the two groups, with P<0.05 considered statistically significant. The independent-samples t test was used to determine differences in preprocedural and postprocedural STAI-S, preprocedural and postprocedural pulse rate, ages, and duration of procedure between the two groups. The chi-square test was used to determine differences of count data between groups.
Results
Of the 124 flexible cystoscopies, 46 (24 in group 1 and 22 in group 2) were performed for diagnostic purposes, with the remainder surveillance procedures; 43 (23 in group 1 and 20 in group 2) were performed for the first time, with the remainder repeated cystoscopy. Age distribution (t test), duration of the procedure (t test), preprocedural pulse rate (t test), ratio of cystoscopy for diagnostic purpose (chi-square), and ratio of patients who had repeated cystoscopy (chi-square) in the two groups were all comparable (both P>0.05) (Table 1).
Table 1.
Patient Variables, Duration of Procedure, and Comparison of Anxiety and Pain Scores Between Two Groups
| Group 1 (n=62) | Group 2 (n=62) | P value | |
|---|---|---|---|
| Age (y) | |||
| Mean±SD | 62.0±12.7 | 64.8±11.2 | 0.205 |
| Range | 25–81 | 33–84 | |
| Duration of procedure (min) | |||
| Mean±SD | 7.1±1.3 | 7.4±1.2 | 0.214 |
| Pulse (beats/min) Mean±SD | |||
| Preprocedure | 72.4±7.1 | 72.6±7.7 | 0.876 |
| Postprocedure | 79.8±5.5 | 76.0±7.3 | 0.002 |
| STAI–S score Mean±SD | |||
| Preprocedure | 41.4±7.6 | 41.6±7.9 | 0.889 |
| Postprocedure | 39.4±6.5 | 34.5±5.8 | <0.001 |
| First ever cystoscopy | 40.8±6.2 (n=23) | 34.8±6.6 (n=20) | 0.003 |
| Previous cystoscopy | 38.5±6.6 (n=39) | 34.4±5.5 (n=42) | 0.003 |
| Diagnostic cystoscopy | 41.0±6.8 (n=24) | 36.5±6.6 (n=22) | 0.031 |
| Surveillance cystoscopy | 38.3±6.1 (n=38) | 33.4±5.0 (n=40) | <0.001 |
| Mean pain score | |||
| Mean±SD | 2.53±1.34 | 1.63±1.09 | <0.001 |
| First ever cystoscopy | 2.91±1.62 (n=23) | 1.65±1.27 (n=20) | 0.009 |
| Previous cystoscopy | 2.31±1.10 (n=39) | 1.62±1.01 (n=42) | 0.006 |
| Diagnostic cystoscopy | 2.83±1.58 (n=24) | 2.05±1.17 (n=22) | 0.063 |
| Surveillance cystoscopy | 2.34±1.15 (n=38) | 1.40±0.98 (n=40) | <0.001 |
| Classification of pain | |||
| No pain | 3 | 10 | |
| Mild pain | 48 | 50 | |
| Moderate pain | 11 | 2 | |
| Severe pain | 0 | 0 | |
SD=standard deviation; STAI-S=State Instrument of State-Trait Anxiety Inventory.
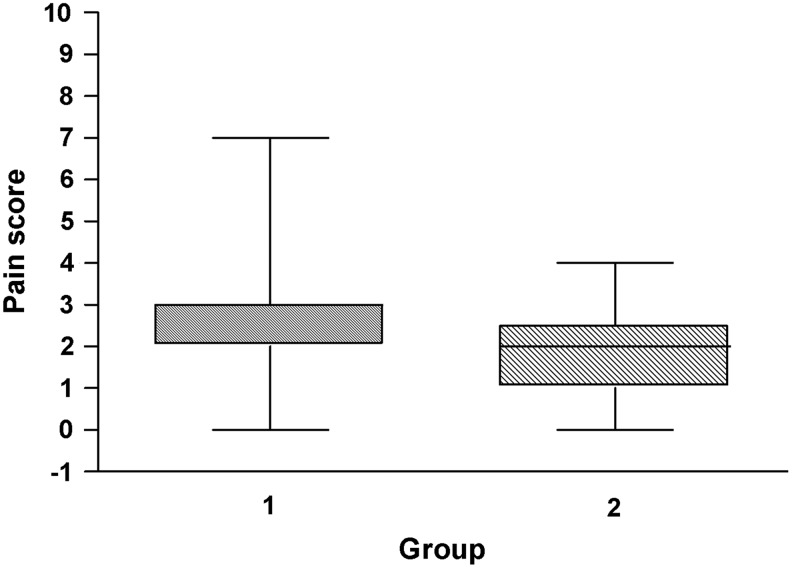
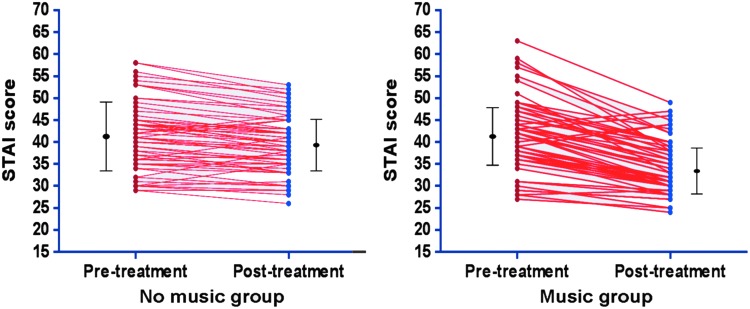
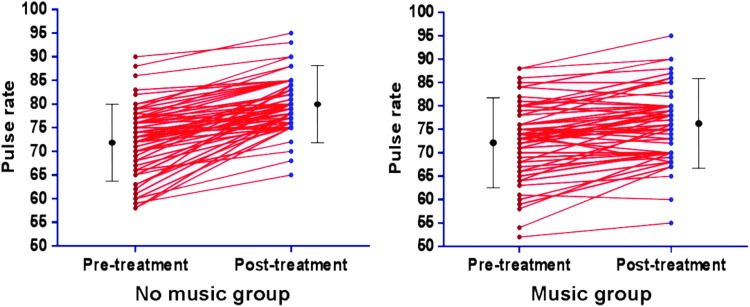
The mean pain score on VAS was 2.53±1.34 in group 1 and 1.63±1.09 in group 2. STAI-S score decreased in both groups after the procedure: The mean postprocedural STAI-S score was 39.4±6.5 in group 1 and 34.5±5.8 in group 2. Mean pain score and mean postprocedural anxiety level (STAI-S score) in group 2 were statistically significantly lower than those in group 1 (P<0.001 for both) (Figs. 1, 2). Statistically significant differences were also detected between group 1 and group 2 in the postprocedural pulse rate (79.8±5.5 vs 76.0±7.3, P=0.002) (Fig. 3).
FIG. 1.
Box plots of pain score (visual analog scale [VAS]) showed difference in pain level between the two groups. VAS score was 2.53±1.34 in group 1 (no music) and 1.63±1.09 in group 2 (music); patients who listened to their preferred music experienced less discomfort at cystoscopy.
FIG. 2.
Data point graphs for no-music and music groups pre- and post-treatment with mean and interquartile ranges. The graphs showed reduction of the anxiety levels (State Instrument of State-Trait Anxiety Inventory [STAI-S] score) in both groups after flexible cystoscopy, but the postprocedural STAI-S score in the music group (34.5±5.8) was less than the no-music group (39.4±6.5), P<0.001.
FIG. 3.
Data point graphs for no-music and music groups pre- and post-treatment with mean and interquartile ranges. The graphs show increase of pulse rate in both groups after flexible cystoscopy, but the postprocedural pulse rate in the music group (76.0±7.3) was less than in the no-music group (79.8±5.5), P=0.002.
Especially when stratified analysis was performed and postprocedural STAI-S and pain scores were compared between subgroups, it was found that music engagement was effective for patients receiving flexible cystoscopy for surveillance or diagnostic purposes, as well as those undergoing their first or repeated cystoscopy, in reducing their pain and anxiety (Table 1). Classification of pain according to VAS scores in the two groups was also demonstrated in Table 1.
Discussion
Flexible cystoscopy has greatly dereased patients' discomfort and made cystoscopy more tolerable, especially for male patients; however, pain is still inevitable during this procedure. So many studies had examined different methods to reduce male patients' discomfort, such as assessment of the volume of lidocaine,10 increasing hydrostatic pressure by squeezing the irrigation solution bag,11 cooled lignocaine gel,12 simultaneous visualization,13 application of nitrous oxide inhalation,14 slow delivery of local anesthetics,15 use of a special flexible cystoscope sheath,16 and transcutaneous electrical nerve stimulation.17 Controversy still exists, however. Some randomized controlled trials and meta-analysis reported that there is no significant difference between lidocaine gel and placebo in the efficacy of reducing pain for male patients during flexible cystoscopy,18,19 and Cornel and colleagues20 reported that the pain score of men undergoing flexible cystoscopy could not be obviously affected by simultaneous visualization.
In recent years, several studies had confirmed that music could help patients experience less pain and anxiety during other endoscopic procedures, such as bronchoscopy, gastroscopy, colonoscopy, colposcopy, and hysteroscopy.21–25 Similarly, in our trial, we demonstrated that music could improve psychological and physiologic parameters related to pain and anxiety, the VAS score, and that the postprocedural STAI score among patients who listened to their preferred music were significantly lower, either in the patients with surveillance cystoscopy or diagnostic cystoscopy, and either in the patients with first time cystoscopy or repeated cystoscopy. Compared with group 1, the decrease of STAI score in group 2 was significantly more, but the increase of pulse rate was significantly less after the procedure, indicating that music intervention might smooth patients' mood, reduce their discomfort, and relieve their anxiety. Just recently, Yeo and coworkers26 also stated that listening to music during rigid cystoscopy decreased anxiety, pain, and dissatisfaction in male patients. To a great degree, this statement is supported and confirmed by our results.
The mechanism of music playing an adjuvant therapeutic role in reducing pain and anxiety is sophisticated. Mitchell and colleagues27 reported that listening to preferred music might provide an emotional distraction and consequently reduce the feeling of pain and the concomitant negative emotional experience. According to functional magnetic resonance imaging analysis, Valet and associates28 stated that distraction could increase the activation of the cingulo-frontal cortex, the periaqueductal gray, and the posterior thalamus significantly; they also found that distraction could be significantly associated with reduction of pain intensity, unpleasantness, and pain-related activation in some brain areas, especially in the “medial pain system.” The study by Valet and associates28 also confirmed the opinion of Cook29 that music therapy could divert patients' attention from fear of pain and that is the reason why so many clinical research studies had reported music therapy could be widely used in both acute pain and chronic pain treatment.30,31 In addition, some studies even reported that music intervention could reduce the dose of analgesic and sedation drugs in invasive procedures.23,32
Careful consideration is needed when selecting music for the purpose of releasing both pain and anxiety. Some studies demonstrated patient selection was better27; on the contrary, some stated that researcher-selected music would be most effective, because researcher-selected music could take into account factors that had been known and accepted to be effective in relaxation and pain control.7,33–35 In our trial, we combined the patient preference and researcher selection. We selected the music according to experts' recommendations, which should fulfill the conditions such as moderate volume, gentle timbre, smooth melody, few percussive instruments, and without strong rhythm,7,35 then divided these songs and melodies into four major kinds. Therefore, patients in our study could select their preferred music style that could both match their taste and meet the standard of “theraputic music.”
This study has some possible limitations. First, This is a small and single-center study; a multi-center and large sample study could be more convincing from which to draw a meaningful conclusion. Second, the cystoscopist was not blinded during the procedure, so it is potentially possible that patients in group 2 could get more careful manipulation than those in group 1. Third, there were no specific orientations for patients to watch the flexible cystoscopy procedure, so potentially simultaneous visualization of the procedure might divert attention and reduce discomfort.13,36 Fourth, although some studies had confirmed that local anesthetic played a role just as a placebo18 and might make patient exerience more pain when the physician injected the lidocaine jelly into the urethera,37 leading to a conclusion that local anesthetic might be unnecessary, we still used lidocaine jelly for every patient in our study because of the clinical routine and patient demand for topical anesthesia. Fifth, VAS and SATI scores are partly subjective; some more objective parameters, such as the bispectral index,38 were not used. Despite these limitations, our study demonstrated that listening to preferred music during cystoscopy reduces feelings of pain and enhances satisfaction and compliance during this invasive procedure.
Conclusion
Patients who were listening to preferred music experienced less discomfort and anxiety at flexible cystoscopy. As a nonpharmacologic and noninvasive intervention, music might be one of the simple but important strategies in office urology for patient satisfaction.
Abbreviations Used
- STAI-S
State Instrument of State-Trait Anxiety Inventory
- VAS
visual analog scale
Disclosure Statement
No competing financial interests exist.
References
- 1.Pillai PL, Sooriakumaran P. Flexible cystoscopy: A revolution in urological practice. Br J Hosp Med (Lond). 2009;70:583–585 [DOI] [PubMed] [Google Scholar]
- 2.Samplaski MK, Jones JS. Two centuries of cystoscopy: The development of imaging, instrumentation and synergistic technologies. BJU Int 2009;103:154–158 [DOI] [PubMed] [Google Scholar]
- 3.Burke DM, Shackley DC, O'Reilly PH. The community-based morbidity of flexible cystoscopy. BJU Int 2002;89:347–349 [DOI] [PubMed] [Google Scholar]
- 4.Konety B, Joyce G, Wise M. Bladder and upper tract urothelial cancer. In: Litwin MS, Saigal CS, eds. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. NIH Publication No. 07-5512. Washington, DC: US Government Printing Office, 2007:246–247 [Google Scholar]
- 5.Nilsson U. The anxiety- and pain-reducing effects of music interventions: A systematic review. AORN J 2008;87:780– 807 [DOI] [PubMed] [Google Scholar]
- 6.Lin ST, Yang P, Lai CY, et al. . Mental health implications of music: Insight from neuroscientific and clinical studies. Harv Rev Psychiatry 2011;19:34–46 [DOI] [PubMed] [Google Scholar]
- 7.Gooding L, Swezey S, Zwischenberger JB. Using music interventions in perioperative care. South Med J 2012;105:486–490 [DOI] [PubMed] [Google Scholar]
- 8.Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: What is moderate pain in millimetres? Pain 1997;72:95–97 [DOI] [PubMed] [Google Scholar]
- 9.Speilberger C. Manual for the State-Trait Anxiety Inventory (Form Y). Palo Alto, CA: Consulting Psychologists Press, 1987 [Google Scholar]
- 10.McFarlane N, Denstedt J, Ganapathy S, et al. . Randomized trial of 10 mL and 20 mL of 2% intraurethral lidocaine gel and placebo in men undergoing flexible cystoscopy. J Endourol 2001;15:541–544 [DOI] [PubMed] [Google Scholar]
- 11.Gunendran T, Briggs RH, Wemyss-Holden GD, Neilson D. Does increasing hydrostatic pressure (“bag squeeze”) during flexible cystoscopy improve patient comfort: A randomized, controlled study. Urology 2008;72:255–259 [DOI] [PubMed] [Google Scholar]
- 12.Thompson TJ, Thompson N, O'Brien A, et al. . To determine whether the temperature of 2% lignocaine gel affects the initial discomfort which may be associated with its instillation into the male urethra. BJU Int 1999;84:1035–1037 [DOI] [PubMed] [Google Scholar]
- 13.Zhang ZS, Tang L, Wang XL, et al. . Seeing is believing: A randomized controlled study from China of real-time visualization of flexible cystoscopy to improve male patient comfort. J Endourol 2011;25:1343–1346 [DOI] [PubMed] [Google Scholar]
- 14.Calleary JG, Masood J, Van-Mallaerts R, Barua JM. Nitrous oxide inhalation to improve patient acceptance and reduce procedure related pain of flexible cystoscopy for men younger than 55 years. J Urol 2007;178:184–188 [DOI] [PubMed] [Google Scholar]
- 15.Khan MA, Beyzade B, Tau W, et al. . Effect of the rate of delivery of lignocaine gel on patient discomfort perception prior to performing flexible cystoscopy. Urol Int 2002;68:164–167 [DOI] [PubMed] [Google Scholar]
- 16.Zhang Z, Cao Z, Xu C, et al. . Better irrigation delivers better vision: An exploratory study of a novel continuous irrigation sheath for a flexible cystoscope. Urology 2013;81:25–29 [DOI] [PubMed] [Google Scholar]
- 17.Hruby G, Ames C, Chen C, et al. . Assessment of efficacy of transcutaneous electrical nerve stimulation for pain management during office-based flexible cystoscopy. Urology 2006;67:914–917 [DOI] [PubMed] [Google Scholar]
- 18.Aaronson DS, Walsh TJ, Smith JF, et al. . Meta-analysis: Does lidocaine gel before flexible cystoscopy provide pain relief? BJU Int 2009;104:506–510 [DOI] [PubMed] [Google Scholar]
- 19.Kobayashi T, Nishizawa K, Mitsumori K, Ogura K. Instillation of anesthetic gel is no longer necessary in the era of flexible cystoscopy: A crossover study. J Endourol 2004;18:483–486 [DOI] [PubMed] [Google Scholar]
- 20.Cornel EB, Oosterwijk E, Kiemeney LA. The effect on pain experienced by male patients of watching their office-based flexible cystoscopy. BJU Int 2008;102:1445–1446 [DOI] [PubMed] [Google Scholar]
- 21.Dubois JM, Bartter T, Pratter MR. Music improves patient comfort level during outpatient bronchoscopy. Chest 1995;108:129–130 [DOI] [PubMed] [Google Scholar]
- 22.El-Hassan H, McKeown K, Muller AF. Clinical trial: Music reduces anxiety levels in patients attending for endoscopy. Aliment Pharmacaol Ther 2009;30:718–724 [DOI] [PubMed] [Google Scholar]
- 23.Costa A, Montalbano LM, Orlando A, et al. . Music for colonoscopy: A single-blind randomized controlled trial. Dig Liver Dis 2010;42:871–876 [DOI] [PubMed] [Google Scholar]
- 24.Galaal K, Bryant A, Deane KH, et al. . Interventions for reducing anxiety in women undergoing colposcopy. Cochrane Database Syst Rev. 2011;1A:CD006013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Angioli R, Cicco Nardone CD, Plotti F, et al. . Use of music to reduce anxiety during office hysteroscopy: Prospective randomized trial. J Minim Invasive Gynecol 2013[Epub ahead of print]; DOI: 10.1016/j.jmig.2013.07.020 [DOI] [PubMed] [Google Scholar]
- 26.Yeo JK, Cho DY, Oh MM, et al. . Listening to music during cystoscopy decreases anxiety, pain, and dissatisfaction in patients: A pilot randomized controlled trial. J Endourol 2013;27:459–462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mitchell LA, MacDonald RA, Brodie EE. A comparison of the effects of preferred music, arithmetic and humour on cold pressor pain. Eur J Pain 2006;10:343–351 [DOI] [PubMed] [Google Scholar]
- 28.Valet M, Sprenger T, Boecker H, et al. . Distraction modulates connectivity of the cingulo-frontal cortex and the midbrain during pain—an fMRI analysis. Pain 2004;109:399–408 [DOI] [PubMed] [Google Scholar]
- 29.Cook JD. The therapeutic use of music: A literature review. Nurs Forum 1981;20:252–266 [DOI] [PubMed] [Google Scholar]
- 30.Bradshaw DH, Chapman CR, Jacobson RC, Donaldson GW. Effects of music engagement on responses to painful stimulation. Clin J Pain 2012;28:418–427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guétin S, Giniès P, Siou DK, et al. . The effects of music intervention in the management of chronic pain: A single-blind, randomized, controlled trial. Clin J Pain 2012;28:329–337 [DOI] [PubMed] [Google Scholar]
- 32.Kulkarni S, Johnson PC, Kettles S, et al. . Music during interventional radiological procedures, effect on sedation, pain and anxiety: A randomised controlled trial. Br J Radiol 2012;85:1059–1063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cepda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database Syst Rev 2006;2:CD004843. [DOI] [PubMed] [Google Scholar]
- 34.Pelletier CL. The effect of music on decreasing arousal due to stress: a meta-analysis. J Music Ther 2004;41:192–214 [DOI] [PubMed] [Google Scholar]
- 35.Chi GC, Young A. Selection of music for inducing relaxation and alleviating pain: Literature review. Holist Nurs Pract 2011;25:127–135 [DOI] [PubMed] [Google Scholar]
- 36.Patel AR, Jones JS, Angie S, Babineau D. Office based flexible cystoscopy may be less painful for men allowed to view the procedure. J Urol 2007;177:1843–1845 [DOI] [PubMed] [Google Scholar]
- 37.Ho KJ, Thompson TJ, O'Brien A, et al. . Lignocaine gel: Does it cause urethral pain rather than prevent it? Eur Urol 2003;43:194–196 [DOI] [PubMed] [Google Scholar]
- 38.Dahaba AA, Lischnig U, Kronthaler R, et al. . Bispectral index guided vs clinically guided remifentanyl/propofol analgesia/sedation for interventional radiological procedures: An observer-blinded randomized study. Anesth Analg 2006;103:378–384 [DOI] [PubMed] [Google Scholar]