Abstract
For daily burn wound care and therapeutic physical therapy skin stretching procedures, powerful pain medications alone are often inadequate. This feasibility study provides the first evidence that entering an immersive virtual environment using very inexpensive (∼$400) wide field of view Oculus Rift Virtual Reality (VR) goggles can elicit a strong illusion of presence and reduce pain during VR. The patient was an 11-year-old male with severe electrical and flash burns on his head, shoulders, arms, and feet (36 percent total body surface area (TBSA), 27 percent TBSA were third-degree burns). He spent one 20-minute occupational therapy session with no VR, one with VR on day 2, and a final session with no VR on day 3. His rating of pain intensity during therapy dropped from severely painful during no VR to moderately painful during VR. Pain unpleasantness dropped from moderately unpleasant during no VR to mildly unpleasant during VR. He reported going “completely inside the computer generated world”, and had more fun during VR. Results are consistent with a growing literature showing reductions in pain during VR. Although case studies are scientifically inconclusive by nature, these preliminary results suggest that the Oculus Rift VR goggles merit more attention as a potential treatment for acute procedural pain of burn patients. Availability of inexpensive but highly immersive VR goggles would significantly improve cost effectiveness and increase dissemination of VR pain distraction, making VR available to many more patients, potentially even at home, for pain control as well as a wide range of other VR therapy applications. This is the first clinical data on PubMed to show the use of Oculus Rift for any medical application.
Introduction
The problem: uncontrolled pain
The current standard of care=pain medications alone. For over 100 years, opioid narcotic pain medication has been the cornerstone of pain control for severe burn patients during wound cleaning. Procedural pain is still managed largely as it has been managed for the past 100 years, pharmacologically, through opioid narcotic analgesics, often in combination with anxiolytics. Analgesics reduce pain by interfering at a neuronal level with the transmission of signals from pain receptors to the brain (e.g., neurotransmission).1 Although this pharmacologic blocking of physical transmission of pain signals from pain receptors to the brain is the foundation of traditional burn pain control, pharmacologic analgesics alone typically fail to control pain during wound debridement.1
When relying on pharmacologies as the primary (and often the only) treatment for pain, most patients with large severe burn wounds report experiencing severe or higher pain during daily wound debridement (worst pain intensity of seven or higher on a 0 to 10 scale).2 This is even true of soldiers.3,4 Pain of five or higher is considered uncontrolled pain. Patients with unusually large severe pediatric burn wounds are especially challenging. Typically, the larger the severe burn, the longer the wound cleaning/debridement takes each day, and greater the number of days the patient receives wound care.
Because of the inadequacy of pharmacological interventions alone to control burn pain during wound debridement and during occupational and physical therapy skin stretching exercises, adjunctive nonpharmacological interventions could provide a valuable additional component of a multiprogram burn pain treatment regimen. Psychological interventions can facilitate the effects of standard pharmacologic analgesics.
Immersive virtual reality pain distraction
The goal of immersive virtual reality (VR) is to give patients the illusion of visiting the virtual world, as if it is a place they are visiting, an illusion known as “presence.” The rationale of why VR could be valuable for pain control is explained as follows. With burn patients, pain receptors send neural signals/information to the patient's brain that the brain processes, resulting in the patient's conscious experience of pain. This information processing requires attention.5,6 There is a limit to how much information the brain can process at any given time.7 Virtual Reality (e.g, SnowWorld) floods the brain with attention grabbing information from multiple senses. SnowWorld is unusually attention grabbing, leaving less attention available for processing pain signals. Patients feel less pain, and spend less time thinking about their pain.8–12
SnowWorld was the first virtual reality world specifically designed for treating pain (www.vrpain.com). SnowWorld is custom designed to treat burn patients who are on powerful pain medications, and in pain. During painful wound care procedures, patients interact with snowmen, igloos, penguins, woolly mammoths and flying fish by using a wireless mouse (or sometimes head tracking) to aim and throw snowballs. Snowballs thrown by the patients impact objects in the virtual world with special effects and sound effects. Music by Paul Simon plays in the background, helping to block out anxiety producing sounds from the hospital. Immersive virtual reality visually isolates patients from the “real world.” The helmet typically used to deliver VR blocks the patients' view of the hospital room and substitutes computer-generated images via small computer screens and lenses positioned near the patient's eyes.
Research using wide field of view VR goggles and interactive VR worlds
Research using wide field of view VR goggles and inter-active virtual reality worlds has shown significant drops in subjective burn pain in both case series as well as randomized controlled trials. VR analgesia has been demonstrated in burn patients during wound debridement (see Figure 1a) and as shown in Figure 1b, during physical/occupational therapy skin stretching exercises.11,13 In one recent study of soldiers with combat-related burn injuries during wound cleaning, VR distraction with SnowWorld boosted patients ratings of “fun during wound care” from “no fun at all” (with no VR), to “pretty fun” during VR.4
FIG. 1.
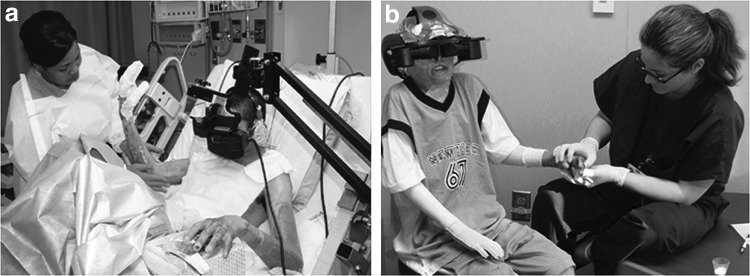
(a) VR during wound cleaning of a soldier. (b) VR of pediatric burn patient during passive range of motion exercises. VR, virtual reality. Photo credits and copyright Hunter Hoffman, UW, www.vrpain.com.
A number of laboratory studies have also explored the potential of VR distraction as a non-pharmacologic analgesic. Laboratory studies have explored the relationship between the immersiveness of the VR system and the magnitude of pain reduction during VR distraction.11,14–17 These studies have helped researchers design more effective VR systems. For example, in laboratory studies with healthy volunteer participants, allowing patients to interact with the virtual world via throwing snowballs by clicking their computer mouse,16 and use of wide field of view (large) goggles, have both been shown to significantly boost VR pain reduction compared to less immersive VR.15
In addition to reducing the amount of pain reported by participants during brief painful stimuli, studies using functional Magnetic Resonance Imaging (fMRI) have shown large reductions in pain-related brain activity during VR.19 Healthy volunteers received brief thermal stimuli at painful but tolerable temperatures during brain scans (pain on/off approximately every 30 seconds for approximately six minutes). Half of the stimuli were during no VR, and participants played SnowWorld in the brain scanner during the other three pain stimuli (treatment order randomized). During VR, participants reported large reductions in how much pain they experienced, and their brains showed large reductions in pain-related brain activity in all five brain regions of interest, the thalamus, insula, anterior cingulate cortex, and the primary and secondary somatosensory cortices. A related laboratory pain study showed that the amount of pain reduction from VR was comparable to the amount of pain reduction from a moderate dose of hydromorphone typical of what a burn patient would receive during wound care, and the greatest analgesia was achieved by combining the two treatment modalities (pharmacologic and non-pharmacologic).20
Critical Barriers to using immersive VR adjunctively, (i.e., in addition to traditional pain medications), for pediatric patients with large severe burn injuries
Despite the growing evidence that VR is effective during painful medical procedures, VR is not yet widely used clinically during everyday clinical practice. The expense of wide field of view VR systems has limited dissemination. Over the past 20 years, the price of VR computers has dropped from $90,000 to less than $1,500, as graphics processor and CPU speeds have been accelerated and miniaturized for video game consumers. In contrast, during the past 20 years, wide field of view VR goggles have improved in quality, but have remained expensive. However, a similar breakthrough in VR goggle technology is in development, and scheduled for commercial sale in 2014 or 2015: the Oculus Rift, www.oculusvr.com (not available to consumers at the time this was written). The Oculus Rift goggles are wide field of view, roughly similarly in FOV to VR goggles currently being used for VR pain distraction at several regional burn centers, (e.g., the Rockwell Collins SR80 VR goggles, priced at $35,000).4 The new Oculus Rift goggles are being developed for mass production to be used to play video games and movies. Instead of being built one at a time like the current wide field of view VR goggles, Oculus Rift are mass produced. Fifty thousand Oculus Rift goggles have reportedly already been manufactured and sold to software developers, and when Oculus Rift goes commercial, the goggles are priced to sell to a very large market of PC video game players, a 20 billion dollar a year industry. The estimated selling price of the Oculus Rift goggles is ∼$400. (1/1000th the cost of the Rockwell Collins SR80 used in several key VR analgesia studies). As evidence of the magnitude of this development, Oculus Rift was purchased by Facebook for 2 billion dollars in March 2014.
Materials and Methods
The current case study was conducted as a proof of concept, to explore the feasibility of using the Oculus Rift goggles to distract burn patients during occupational therapy and other painful medical procedures. The patient was an 11-year-old male with severe electrical and flash burns on his head, shoulders, arms, and feet (36 percent TBSA, 27 percent TBSA third-degree burns), from an electrical accident where high voltage electricity passed through his body. Because the patient had severe burn wounds on his head, we mounted our monocular Oculus Rift goggles to a robot-like arm goggle holder.4 On day 1 (baseline), the patient spent some of his 20 minutes of physical therapy with no VR (standard pain medications alone). On day 2, the patient received the same pain medications, and his occupational therapist conducted the same 20-minute passive range of motion skin stretching exercises while the patient looked into the VR goggles (see Fig. 2) and interacted with the world using a computer mouse (standard pain medications+VR, see Fig. 3a). On day 3, the patient received 20 minutes of physical therapy with no VR, same as day 1.
FIG. 2.

Pediatric burn patient was the first to try out the Oculus Rift VR goggles for VR pain distraction during physical therapy. Photo credits and copyright Hunter Hoffman, UW, www.vrpain.com.
FIG. 3.
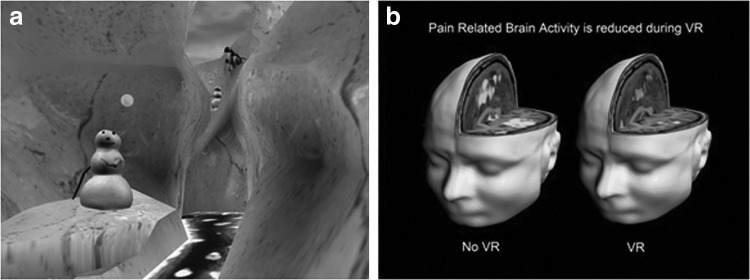
(a) SnowWorld, a VR world designed for distracting patients from acute procedural pain. During wound cleaning and physical therapy, severe burn trauma patients typically report 35–50 percent reductions in worst pain intensity on subjective pain rating scales.11,13 (b) Functional magnetic resonance imaging (fMRI) brain scan studies show large reductions in pain-related brain activity in subjects using SnowWorld.19,20 SnowWorld still image by Ari Hollander and Howard Rose, copyright Hunter Hoffman, UW, www.vrpain.com. fMRI brain image by Todd Richards and Aric Bills, copyright Hunter Hoffman, UW, www.vrpain.com.
Results
The GRS ratings18 of the patient are shown in Figure 4. Pain intensity and pain unpleasantness dropped during VR. The patient reported having more fun during physical therapy with VR than without it. Also, despite the fact that we used a custom robot-like arm mounted oculus rift goggles holder with no head tracking, and a preconsumer software developers prototype version of the helmet with considerably lower quality resolution than the forthcoming consumer version, the patient rated his presence in VR as a 10 (on a graphic rating scale from 0 to 10), reporting that he went “completely inside the computer generated world as if it was a place he visited.”
FIG. 4.
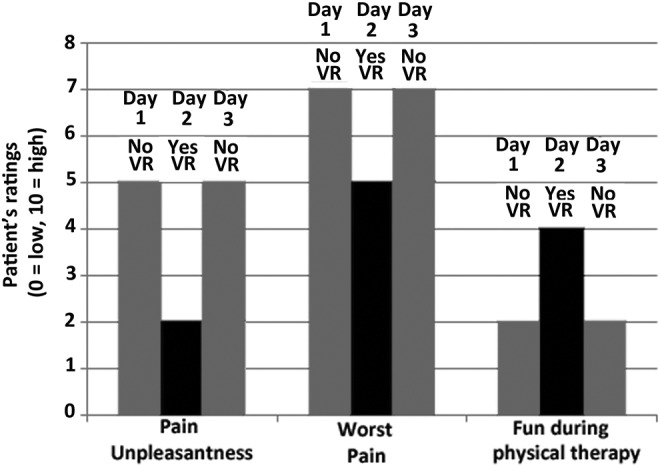
Pain during passive range of motion exercises during no VR, (gray bars) vs. pain during the same exercises while in VR (black bar).
Discussion
Results showing reductions in pain intensity and pain unpleasantness, during the 20 minutes of occupational therapy skin stretching exercises, are consistent with a growing literature showing reductions in pain during VR21,22 but remarkably, in the current study, this was accomplished using a pair of ∼$400 VR goggles. Although preliminary, and although case studies are by nature scientifically inconclusive,23 these results suggest that the Oculus Rift VR goggles merit more attention as a potential treatment for acute procedural pain of burn patients. Randomized controlled studies are warranted. Availability of inexpensive, but highly immersive VR goggles would significantly improve cost effectiveness and increase dissemination of VR pain distraction, making VR distraction available to many more patients, potentially even at home, for pain control, and for a wide range of other VR therapy applications (e.g., VR exposure therapy for phobias,24 and post-traumatic stress disorder,25 and beyond; see Figure 5).
FIG. 5.

SpiderWorld VR exposure therapy for phobias.24 Photo credit Stephen Dagadakis, copyright Hunter Hoffman, www.vrpain.com.
Acknowledgments
Funding from Shriners Hospitals for Children Grant to Walter Meyer III. NIH grants 2 R01 GM042725-17 and 1 R01AR054115-01A1.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Malchow RJ, Black IH. The evolution of pain management in the critically ill trauma patient: emerging concepts from the global war on terrorism. Critical Care Medicine 2008; 36:S346–S357 [DOI] [PubMed] [Google Scholar]
- 2.Choiniere M, Melzack R, Rondeau J, et al. The pain of burns: characteristics and correlates. Journal of Trauma 1989; 29:1531–1539 [DOI] [PubMed] [Google Scholar]
- 3.Maani C, Hoffman HG, DeSocio PA, et al. Pain control during wound care for combat-related burn injuries using custom articulated arm mounted virtual reality goggles. Journal of CyberTherapy and Rehabilitation 2008; 1:193–198 [Google Scholar]
- 4.Maani CV, Hoffman HG, Morrow M, et al. Virtual reality pain control during burn wound debridement of combat-related burn injuries using robot-like arm mounted VR goggles. Journal of Trauma 2011; 71:S125– S130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eccleston C. Role of psychology in pain management. British Journal of Anaesthesia 2001; 87:144–152 [DOI] [PubMed] [Google Scholar]
- 6.Eccleston C, Crombez G. Pain demands attention: a cognitive-affective model of the interruptive function of pain. Psychological Bulletin 1999; 125:356–366 [DOI] [PubMed] [Google Scholar]
- 7.Kahneman D. (1973). Attention and effort. Englewood Cliffs, NJ: Prentice-Hall, p. 246 [Google Scholar]
- 8.Hoffman HG, Garcia-Palacios A, Kapa VA, et al. Immersive Virtual Reality for reducing experimental ischemic pain. International Journal of Human-Computer Interaction 2003; 15:469–486 [Google Scholar]
- 9.Hoffman HG. Virtual-reality therapy. Scientific American 2004; 291:58–65 [DOI] [PubMed] [Google Scholar]
- 10.Hoffman HG, Doctor JN, Patterson DR, et al. Virtual reality as an adjunctive pain control during burn wound care in adolescent patients. Pain 2000; 85:305–309 [DOI] [PubMed] [Google Scholar]
- 11.Hoffman HG, Chambers GT, Meyer WJ 3rd, et al. Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Annals of Behavioral Medicine 2011; 41:183–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van Twillert B, Bremer M, Faber AW. Computer-generated virtual reality to control pain and anxiety in pediatric and adult burn patients during wound dressing changes. Journal of Burn Care & Research 2007; 28:694–702 [DOI] [PubMed] [Google Scholar]
- 13.Sharar SR, Carrougher GJ, Nakamura D, et al. Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: preliminary results from 3 ongoing studies. Archives of Physical Medicine and Rehabilitation 2007; 88:S43– S49 [DOI] [PubMed] [Google Scholar]
- 14.Hoffman HG, Sharar SR, Coda B, et al. Manipulating presence influences the magnitude of virtual reality analgesia. Pain 2004; 111:162–168 [DOI] [PubMed] [Google Scholar]
- 15.Hoffman HG, Seibel EJ, Richards TL, et al. Virtual reality helmet display quality influences the magnitude of virtual reality analgesia. Journal of Pain 2006; 7:843–850 [DOI] [PubMed] [Google Scholar]
- 16.Wender R, Hoffman HG, Hunner HH, et al. Interactivity influences the magnitude of virtual reality analgesia. Journal of CyberTherapy and Rehabilitation 2009; 2:27–33 [PMC free article] [PubMed] [Google Scholar]
- 17.Dahlquist LM, McKenna KD, Jones KK, et al. Active and passive distraction using a head-mounted display helmet: effects on cold pressor pain in children. Health Psychology 2007; 26:794–780 [DOI] [PubMed] [Google Scholar]
- 18.Gracely RH, McGrath F, Dubner R. Ratio scales of sensory and affective verbal pain descriptors. Pain 1978; 5:5–18 [DOI] [PubMed] [Google Scholar]
- 19.Hoffman HG, Richards TL, Coda B, et al. Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI. Neuroreport 2004; 15:1245–1248 [DOI] [PubMed] [Google Scholar]
- 20.Hoffman HG, Richards TL, Van Oostrom T, et al. The analgesic effects of opioids and immersive virtual reality distraction: evidence from subjective and functional brain imaging assessments. Anesthesia and Analgesia 2007; 105:1776–1783 [DOI] [PubMed] [Google Scholar]
- 21.Malloy KM, Milling LS. The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clinical Psychology Review 2010; 30:1011–1018 [DOI] [PubMed] [Google Scholar]
- 22.Morris LD, Louw QA, Grimmer-Somers K. The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: a systematic review. Clinical Journal of Pain 2009; 25:815–826 [DOI] [PubMed] [Google Scholar]
- 23.Campbell DT, Stanley JC. (1963). Experimental and quasi-experimental design for research. Boston: Houghton Mifflin Company, p. 84 [Google Scholar]
- 24.Garcia-Palacios A, Hoffman H, Carlin A, et al. Virtual reality in the treatment of spider phobia: a controlled study. Behaviour Research and Therapy 2002; 40:983–993 [DOI] [PubMed] [Google Scholar]
- 25.Difede J, Cukor J, Wyka K, et al. D-cycloserine augmentation of exposure therapy for post-traumatic stress disorder: a pilot randomized clinical trial. Neuropsychopharmacology. 2014; 39:1052–1058 [DOI] [PMC free article] [PubMed] [Google Scholar]


