Abstract
Pain symptoms have been addressed with a variety of therapeutic measures in the past, but as we look to the future, we begin encountering new options for patient care and individual health and well-being. Recent studies indicate that computer-generated graphic environments—virtual reality (VR)—can offer effective cognitive distractions for individuals suffering from pain arising from a variety of physical and psychological illnesses. Studies also indicate the effectiveness of VR for both chronic and acute pain conditions. Future possibilities for VR to address pain-related concerns include such diverse groups as military personnel, space exploration teams, the general labor force, and our ever increasing elderly population. VR also shows promise to help in such areas as drug abuse, at-home treatments, and athletic injuries.
Background
According to the International Association of Pain, pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage. It is a ubiquitous symptom underlying most illnesses, and it diverges into two unique forms: acute and chronic. Acute pain serves a biological purpose, as it usually occurs at the onset of painful incidents such as procedural operations, recovery and rehabilitation, childbirth, dental work, burns, fractures, and so on. If acute pain is not treated properly, it can become chronic.1 Chronic pain is characterized by pain that outlasts normal time of healing, or pain that is associated with a disease or injury. If chronic pain is not treated properly, it can worsen over time and lead to a reduction in quality of life.2 Pain of any sort is generally associated with psychophysiological factors because emotional and behavioral responses have the ability to influence the development of illness and the outcome of treatment, and vice versa.3 Psychological models are incorporated into pain therapy, since they provide a better understanding of the cognitive, emotional, and behavioral manifestations of pain.4 In extreme cases, pharmacological and interventional therapies can be leveraged to manage much more persistent and detrimental pain symptoms.
Pain requires cognitive attention.5 Since humans have a limited attentional capability,6 a computer-generated simulation of three-dimensional environments that can be interacted with in a seemingly realistic manner—virtual reality (VR)—is capable of transporting an individual into an alternate reality without physically leaving their current environment.7 VR has been found to reduce performance on divided attention tasks,8 and patients have less attentional capacity to focus on incoming signals from pain receptors as they shift their focus to interaction with the virtual environment (VE).
VEs can also be used to train patients on preventative and rehabilitative procedures.9 When used in combination with electrophysiological state-sensing devices such as electroencephalograph (EEG), electrocardiograph (ECG), electromyogram (EMG), and other technology, rich patient biofeedback data can be observed. Commercially available handheld devices and peripheral gaming accessories such as Razer Hydra, Leap Motion 3D controller, Myo armband, and the Virtuix Omni treadmill (to name a few) can be used to incorporate dynamic control mechanisms into VR simulations. The release of the Oculus Rift Developer's Kit (costing approximately US$275) head-mounted display (HMD) in 2013 shed light on a new era of inexpensive VR visualization systems. Because of the game-like scenarios that can be programmed, several studies have reported that patients actually have “fun” during treatment with VR.10,11
Costing up to US$635 billion each year in medical treatment costs and lost productivity in the United States,12 US$417 billion in Europe,13 (chronic) pain management is not as “fun” an issue for policy makers. The World Health Organization (WHO) estimates that 22% of the global population has some degree of chronic pain.14 Though an increased understanding of biological mechanisms underlying pain symptoms, diagnostic procedures, and therapeutic applications have been explored, current treatments for pain often do not result in the complete alleviation of symptoms.15
General Overview of Pain Management Therapies
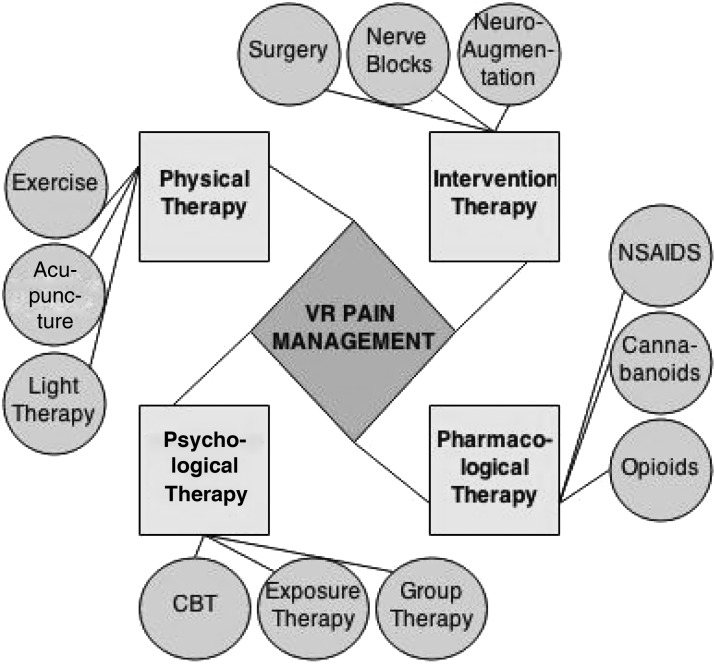
Pain management can be divided into four categories (see Fig. 1).
FIG. 1.
Virtual reality (VR) pain management is an interdisciplinary to therapy designed to attack pain symptoms with an omnidirectional approach.
1. Physiotherapy (physical therapy). The practice of using acupuncture, thermal agents, light therapy, electrotherapy, therapeutic exercise, and some behavior therapy all fall under the category of physiotherapy, which is the treatment of pain by promotion of mobility, functional ability, and routine physical intervention.
2. Psychotherapy (psychological therapy). Problems addressed by psychotherapy are centered on the mental well-being of patients. Techniques involve exploration of thoughts, feelings, and behavior for the purpose of achieving higher levels of functionality and quality of life. Cognitive Behavior Therapy (CBT) teaches patients to analyze and restructure their thought processes while becoming more aware and in control of physiological factors that correlate with mental state—factors such as heart rate, respiration, and so on.
3. Pharmacotherapy (pharmacological therapy). The oral administration of medicinal drugs to relieve pain symptoms is known as pharmacotherapy. WHO guidelines elicit a “pain ladder” for the consumption of pharmacological analgesics for patients experiencing severe pain that cannot be addressed solely with nonmedicinal therapy.16 The ladder starts with nonopioid drugs such as cannabinoids, paracetamol, dipyrone, nonsteroidal anti-inflammatory drugs (NSAIDs), or COX-2 inhibitors. If pain is not considerably addressed using nonopioids, further progression could require consumption of a mild opioid such as codeine phosphate, dextroproxyphene, or tramadol in conjunction with nonopioids. If pain persists, or the patient is experiencing onset of sudden severe pain symptoms, strong opioids such as morphine, diamorphine, fentanyl, buprenorphine, oxymorphine, oxycodone, or hydromorphone can be issued in conjunction with nonopioids. In patients experiencing neuropathic pain, tricylic antidepressants, class I antiarrhythmics, and anticonvulants are commonly issued to relieve pain symptoms.
4. Intervention therapy. The use of interventional applications to diagnose or locate the patient's source of pain or provide relief is known as intervention therapy. Treatments include injection therapy, surgical intervention, nerve blocks, neuroaugmentation, implantable devices or drug delivery systems, and direct brain stimulation (to name a few). Interventional procedures are most commonly used in combination with standard analgesic methods to reduce opioid side effects and to achieve a better analgesic efficiency.
Room for Improvement
In a general Western healthcare model, patients who experience symptoms of pain must consult a primary care specialist with the hope of obtaining a diagnosis and curative treatment. When such a treatment is unavailable, these patients “expect” a prescription for analgesic medication to relieve their symptoms. Some of these medications might relieve acute pain in the short term, but their utility for treating long-term chronic pain can be controversial. Studies suggest only 32% of patients placed on long-term opioids17 and 50% placed on antidepressants18 experience a pain reduction. In addition to an ambiguous success rate, a sample of orally consumed pharmacological drugs can produce a substance dependency in patients.19 A 2010 U.S. Department of Health and Human Services Nation Survey on Drug Use and Health (NSDUH) reported that approximately 1.7 million people had a pain reliever dependency.20 Side effects such as mental illness or even noneffectiveness increase pain management opportunity costs and likelihood of unwanted results. Extreme caution must be taken when issuing stronger medicinal drugs, since they oft come with side effects that can impede patient progress if appropriate considerations are not acknowledged.
In 2011, the Health Ministry of New South Wales, Australia, reported the following issues associated with the current model of care for pain management: an overdependence on pharmacotherapy, lack of services approaching pain problems using biopsychosocial approaches, lack of timely access to existing services, an increasing demand for pain management particularly in populations suffering chronic pains as a result of surviving conditions that are associated with or lead to persistent pain, and a lack of targeted services for clients experiencing pain who have differing needs.21 Having taken these issues into consideration, we observe how VR therapy can be utilized as a low-cost intervention for a variety of pain-related symptoms.
VR Intervention as a Pain Management Technique
VR is a technology that has emerged as an affordable solution for pain management therapy, proven effective in helping patients cope with pain arising from numerous ailments, being acute or chronic. Table 1 displays a number of recent (2012–2014) publications that show the efficacy of VR in the treatment of a variety of pain symptoms.
Table 1.
Recent Studies that Show the Efficiency of Virtual Reality (VR) in the Treatment of a Variety of Pain Symptoms
| Study | Pain/discomfort studied | Treatment | N | Findings |
|---|---|---|---|---|
| Ortiz-Catalan et al. (2014) | Phantom limb pain—chronic | Phantom movements were predicted using myoelectric pattern recognition and then used as input for VR and AR environments, including a racing game | 1 chronic PLP patient who had shown resistance to a variety of treatments for 48 years | A reduction of time at higher pain intensity levels, as well as the appearance of periods of lower or absent pain within 18 weeks |
| Loreto-Quijada et al. (2013) | General pain/discomfort | Figures that represented pain were displayed to subjects, who were asked to evaluate in terms of arousal and valence; pain figure was then paired with shock, and nonpain figure was paired with no shock | 64 undergraduate students asked to evaluate arousal and valence in response to a figure representing pain | Interaction with VR led to significant increases in pain threshold and tolerance, as well as significantly greater underestimation of time |
| Bidarra et al. (2013) | Dental treatment pain—acute | VR gaming distraction | — | Preliminary evaluation of dentist and game design domains that influence prototype development for an at-the-dentist VR distraction system |
| Botella et al. (2013) | Fibromyalgia (FM)—chronic, neuropathic | 10 sessions of 2 hours group cognitive behavioral treatment for FM supported by VR | 6 women diagnosed with FM, with a mean age of 55 years old (range=47–65; SD=7.6) and a mean duration of diagnosis of 11 years | Results indicate high levels of satisfaction of VR use by 6 patients and reduction in impairment caused by FM symptoms |
| Kipping et al. (2012) | Pediatric burn wounds—acute | VR exposure, prospective randomized controlled trial using nonpharmacological methods, | 41 adolescents aged between 11 and 17 years | Statistically significant reduction in pain scores during dressing removal, and significantly less doses of Entonix given to those receiving VR exposure |
| Villiger et al. (2013) | Neuropathic pain in patients with incomplete spinal cord injury (iSCI)—chronic | VR training, uncontrolled | 14 iSCI patients were treated over 4 weeks in 16 to20 sessions of 45 minutes | Positive changes reported by patients, improvements in lower limb function, reduced intensity and unpleasantness score on Neuropathic Pain Scale (NPS), and stability of finding even after 12 to 16 weeks of training termination |
| Cacau Lde et al. (2013) | Cardiac rehabilitation postoperatively—acute | VR cardiac rehabilitation vs. traditional cardiac rehabilitation | 30 patients exposed to VR, 30 patients not exposed to VR assessed through functional independence measure (FIM), 6-minute walk test (6MWT), and Nottingham Health Profile (NHP) | VR group shows lower reduction in functional performance on first day after surgery as compared to control group, no significant difference in performance on discharge day, a significant decrease in pain score at the third assessment, higher energy level in first evaluation, no statistical significance for emotional reactions, physical ability, or social interaction, shorter length of stay, and higher 6MWD |
| Giggins et al. (2013) | Pediatric headache—chronic | VR biofeedback pain management | 10 adolescents attending an outpatient pediatric neurology clinic were treated by a system which combined VR and biofeedback | Ratings of pain, daily functioning, and quality of life improved significantly at 1 and 3 months post-treatment |
| Wiederhold et al. (2012) | Pain in military populations | Review | — | Funded by NATO, United States Army, Defense Ministry of Austria, and Defense Ministry of Croatia |
| Stetz et al. (2012) | Pain in military populations | CBT to manage pain | 42 chronic pain patients from the Tripler Army Medical Center, older than 17 years of age, intact sensory deficits, and cognitively enabled to follow directions | Statistically significant drop in pain rating in technology-assisted sessions than during standard modality |
VR exposes patients to computer-generated sights and sounds, creating visual and auditory stimulus that would otherwise be presented through the physical environment. This method of intervention provides either distraction or training to patients suffering pain symptoms. Distraction therapy has been applied in clinical practice for decades; the foundation of logic backing the technique is based on the assumption that there exist psychological elements in the perception of pain. It is thought that the more attention someone pays to harmful stimulus, the more intense the realization of the pain. Thus, VEs are used to distract patients from ongoing treatments in a seamless fashion, so as to cause minimal amount of actual pain. Just like many other intervention therapies, VR intervention is being used in combination with other analgesic strategies such as training to attack pain symptoms with an omnidirectional approach (Fig. 1).
VR and physiotherapy
Wii Fit from Nintendo® (and other videogames) has shown that peripheral devices can be used to interact with games with new meaning. Game players balance themselves on the Wii Fit™ board, and sensor data are used as a control mechanism in the game environment. One study showed significant improvements in dynamic balance, functional mobility, and a reduced risk for falling in elderly patients when playing Wii Fit™.22 Another study, focused on the link between elderly diabetic patients and injuries due to falling, concluded that VR has the potential to train patients in balance, strength, and gait so as to reduce the risk of falling.23 For additional analysis on performance, neuromuscular movements can be monitored using electromyography (EMG). Several studies have shown that when this biofeedback is delivered through a display, sound, or haptic signal, it can serve as a correctional mechanism for the patient and as a monitoring mechanism for the therapist.24 VR displays can integrate biofeedback notifications into simulations just as games might use status bars, numerical displays, and written or spoken notifications. Quite like videogames, in fact, VEs are interacted with through a variety of human–computer interaction (HCI) factors, which gives therapists the option of incorporating environment control mechanisms that rely on handheld and peripheral gaming accessories requiring mobility. An example of such a mechanism was used earlier, when we mentioned the Wii Fit board. Another example is the Virtuix Omni (omnidirectional) treadmill, which allows users to “walk in all directions, while standing in one spot,” and enables researchers/therapists to expose patients to VEs that must be navigated through by walking. Numerous studies have shown the effect of treadmill training on rehabilitative populations.25 It is only recently that interdisciplinary researchers/therapists have affordable, commercially available tools to utilize to create more engaging and motivating physical therapy environments.
VR represents an opportunity to both enrich and intensify the experience patients have when receiving physiotherapy. The dramatically interactive nature of VR requires patients to become more involved in the therapy process and can significantly improve both compliance and therapeutic results. During physiotherapy, the main impediment to progress is often pain. VR can help overcome this pain so patients may more rapidly proceed through the therapeutic hierarchy.
VR and psychotherapy
A 17-country study examined the incidence of mental disorders among people with comorbid single or multiple pain conditions. Results indicated that mental disorders followed a linear pattern, with the lowest rates found among individuals with no pain, intermediate rates among those with one pain symptom, and highest rates among those experiencing multiple pain symptoms.26 Psychological factors are highly correlated with pain; depression, anxiety, and posttraumatic stress disorder (PTSD) are frequent byproducts of traumatic physical injury and chronic pain.27 VR used within a CBT model can train patients on shifting attention away from pain or stress-inducing thoughts.28 Self-management (SM) is an action taken by the patient to manage or minimize the impact of pain.29 Along with guided in-clinic therapy, patients have the opportunity to heal with at-home mobile interfaces like those that have been used in numerous studies to monitor and assist patients in SM over long periods of time.30 VR can provide a mobile experience that is programmable and useful for targeting patients with special needs.31
VR exposure therapy targets anxiety disorders in patients with pain symptoms by exposing them to stimuli that trigger unwanted psychophysiological behaviors and training them to condition their psychophysiological responses accordingly. Low-cost EEG systems can be used to monitor real-time brain activity during mobile and immobile tasks in VR.32 This adds another dimension of analysis for monitoring patients with psychological problems because emotional correlates can be drawn from reading spatio-temporal source dynamics and event potentials during different tasks.33
VR and pharmacotherapy
Patients can use VR as an adjunct to pharmaceutical drugs for an increased analgesic efficiency. A study, focused on burn pain reduction in adolescent populations undergoing wound dressing, found that patients experienced a significant reduction in pain scores and dosage of Entonix with VR as opposed to otherwise.34 The combined usage of VR and pharmaceutical drugs has also been utilized in treating by-products of trauma, such as PTSD, with no recorded evidence of negative side effects in the well-being of the patient.35 The ingestion of pharmaceutical drugs can activate primary physiological systems. VR treatment acknowledges these changes and offers methods for promoting activation of systems otherwise unacknowledged by drug treatment.
VR and other interventional therapies
Attention to acute pain during interventional treatments can be repressed with the use of VR devices.36,37 A pilot study conducted on VR distraction at the dentist found that when designing these interfaces, special attention had to be paid for different patient and therapist domains. For example, devices interfering with the work of the dentist could cause a disturbance during the procedure, and devices that were not engaging enough could fail to distract patients.38
Future Implications
Approximately US$14.6 billion over the next 10 years has been allocated by the 2014 U.S. Executive Budget to “implement innovative policies to train new health care providers and ensure that the future health care workforce is prepared to deliver high-quality and efficient health care services.”39
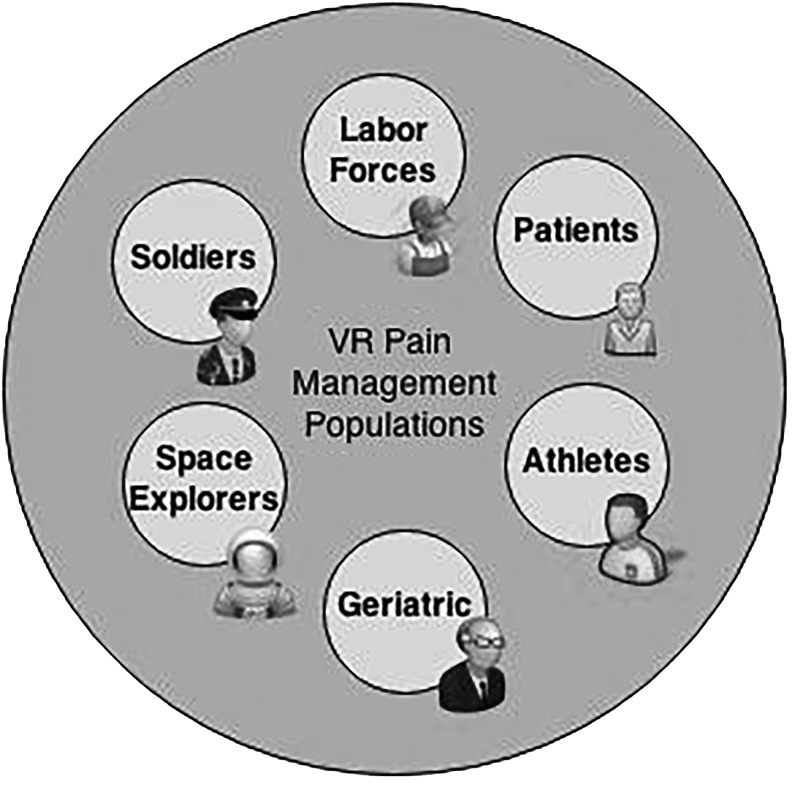
Below, we explore areas and populations that may benefit from the incorporation of VR into existing training and treatment protocols (Fig. 2).
FIG. 2.
Areas and populations that could benefit with interdisciplinary incorporation of VR.
Military populations
Military personnel exposed to traumatic incidents have a high risk for developing PTSD. Incidents may result in injuries such as severed limbs, traumatic brain injury (TBI), and other acute and chronic pain conditions. Treatment typically requires administration of opioid drugs. Studies have shown that these drugs may induce a high dependency in patients, thus the need to investigate new methods for providing efficient pain relief to veterans.28 One area of investigation is phantom limb pain, and VR applications are being studied to investigate advancing treatments for this syndrome further.40 There has been a significant amount of work in applying VR therapies to wounded warriors,28,41–44 and room for improvement still remains. The U.S. Department of Veteran's Affairs was provided $56 billion (from the 2014 Executive Budget) for war veteran healthcare services, which “include innovative programs to educate and support veterans' caregivers, enhance veteran's access to care through telehealth technologies, and support equitable, high-quality care for women veterans in an appropriate and safe environment.”45
Space exploration
Difficulties associated with illness and injury have accounted for more space exploration failures than any other technical or environment reason.46 There is room for incorporating VR into space exploration as a countermeasure to deal with the threat of traumatic incidences occurring during extravehicular activity, onset of neuropathic pain during missions, and other pain-inducing incidents. Low back pain in microgravity is one of the most common problems experienced by astronauts.47 A portable wireless VR solution for back pain telemonitoring has been previously explored to meet similar application requirements.48 Opportunities such as these provide reason for the two interdisciplinary fields to marry so they can potentially produce a synergy.
Geriatric populations
Injury prevention in elderly populations continues to be an issue, as one out of three adults aged 65 or older falls each year. Falls are the leading cause of both fatal and nonfatal injuries. Arthritis is another big issue among geriatric populations, costing the United States up to US$128 billion per year in medical costs and lost productivity.48,49 Approximately 50 million adults are affected with some form of arthritis. The U.S. Center for Disease Control and Prevention was provided approximately US$14 million from the president's 2014 Executive Budget to expand and disseminate evidence-based programs for the treatment of arthritis.50 The European Commission also adopted the European Innovative Partnership on Active and Healthy Ageing initiative with the goal to add 2 years to the average healthy lifespan of Europeans by 2020.51 With resources such as these, we expect to see significant advances in the implementation of VR devices with geriatric populations experiencing pain symptoms in the future.
Pain due to cancer and other chronic injuries
VR has been used in the treatment of illnesses that often result in chronic pain. Yet there remains a need for further exploration of VR treatment methods used in conjunction with traditional analgesics to relieve pain symptoms in these populations. Because pain is not monomorphic, patients can develop intolerance to treatments. This ushers in the use of VR where medication cannot go. VR simulations can be programmed to change in response to patient pain, dialing up the “dosage” as more relief is needed, and dialing down the “dosage” as less is necessary. This ability to control the CyberDose© may prove useful as more self-care is administered by patients in their home environment.
Occupational injuries
On average, up to 12 people die every day due to occupational injury and illness. In 2012, out of 3,945 U.S. worker fatalities in the private industry, 775 (19.6%) were in construction. Leading causes for worker deaths on construction sites were falls, followed by object impalement, and electrocution.52 VR techniques can be implemented to train labor force on preventative techniques to reduce the number of fatalities and injuries in the workspace. In addition, the millions of injuries that occur each year in the workplace can be effectively treated using VR to guide both cognitive and physical rehabilitation.
Drug abuse
The National Institute for Drug Abuse has begun a research program to examine the intersection of pain treatment with the abuse of and addiction to opioid medications. Goals are centered on developing alternative pain management solutions (such as VR) with reduced addiction potential, and elucidating risk or protective factors associated with opioid abuse and addiction.
Safe at-home treatments
The National Institute for Health's 8th Pain Symposium in 2012 was primarily focused on exploring self-management techniques for pain management.53 VR applications are promising for the advancement of at-home medical services because they enable mobility, remote patient monitoring, and treatment specialization capabilities. Much work still needs to be done to quantify the benefits of using topical agents and other safe self-applied techniques such as VR for at-home pain management purposes.
Athletic injuries
Accidents that occur during athletic activity can cause injuries in the form of sprains, knee injuries, swollen muscles, fractures, dislocations, and more. According to the U.S. Consumer Product Safety Commission's National Electronic Injury Surveillance System, more than 1.9 million individuals were treated for a sports-related injury in an emergency medical facility.54 VR can be incorporated during athletic conditioning to prevent injury, and during rehabilitation as a vehicle on the road to recovery.
Conclusions
The use of VR to treat pain and manage patients with a variety of medical conditions has been well established. VR distraction is effective during medical and surgical procedures, acute pain, chronic pain, pain with rehabilitation, chronic pain of cancer, diabetic neuropathic pain, and related conditions such as pruritus. The technique is safe and effective and has been used on patients with migraine headaches. The often relaxing and stress-reducing capabilities of virtual environments demonstrate wide applicability in behavioral medicine and patients with psychophysiological disorders. These disorders, such as functional abdominal pain, muscle sprain, fibromyalgia and neuropathic pain, and postherpetic neuralgia, are very common in primary care practices. There is significant national and international attention focused on pain management in the occupational and clinical settings.
Table 2 describes some of the funding mechanisms available and those funding agencies that have made pain research one of their priorities. We encourage readers to take advantage of these and other funding resources to continue research on more effective and innovative pain reduction strategies.
Table 2.
Global Funding for Advancing Pain Management Techniques and Research
| Agency | Location | Goals | Additional Information |
|---|---|---|---|
| American Fibromyalgia Syndrome Association, Inc. | United States | Researching treatment, cause, and cure for fibromyalgia syndrome | www.afsafund.org |
| American Pain Society | United States | Providing grants to investigate pain | www.americanpainsociety.org |
| British Pain Society | United Kingdom | Providing grants to investigate pain | www.britishpainsociety.org |
| Canadian Pain Society | Canada | Providing grants to investigate pain | www.canadianpainsociety.ca |
| Defense Advanced Research Programs Agency | United States | Development of innovative military technology | www.darpa.mil |
| Department of Defense | United States | Involved in funding defense medical research | www.defense.gov |
| European Innovative Partnership | European Union | Commercially feasible innovative concepts | www.ec.europa.eu/research/innovation-union |
| Horizon 2020 | European Union | Increasing Europe's global competitiveness by driving innovative research | ec.europa.eu/programmes/horizon2020/ |
| Mayday Fund | United States/Canada | Clinical interventions, pediatric pain, pain in non-verbal populations, emergency treatments | www.maydayfund.org |
| NASA Innovative Advanced Concepts | United States and some international opportunity | Innovative, interdisciplinary space exploration concepts | www.nasa.gov/directorates/spacetech/niac |
| National Institute of Arthritis and Musculoskeletal and Skin Diseases | United States | Issues related to arthritis, musculoskeletal and skin disorders | www.niams.nih.gov |
| National Institute on Aging | United States | Issues related to aging | www.nia.nih.gov |
| National Institute of Health Pain Consortium | United States | Advancing pain treatment, medication, and research for pain-related diseases | www.painconsortium.nih.gov |
| National Science Foundation | United States | Funding various project related to pain and disease | www.nsf.gov |
| National Sleep Foundation | United States | Pain and sleep | www.sleepfoundation.org |
| Solving Kids Cancer Therapeutic Development Initiative | International | Pediatric cancer | http://solvingkidscancer.org |
| Thrasher Research Fund | International | Prevention, diagnosis and treatment of children's diseases | www.thrasherresearch.org |
| Department of Veteran's Affairs | United States | War veterans | www.va.gov |
| William T. Grant Foundation | United States | Illness affecting youth aged 5–25 years in the United States | www.wtgrantfoundation.org |
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Casey CY, Greenberg MA, Nicassio PM, et al. Transition from acute to chronic pain and disability: a model including cognitive, affective, and trauma factors. Pain 2008; 134:69–79 [DOI] [PubMed] [Google Scholar]
- 2.Lamé IE, Peters ML, Vlaeyen JWS, et al. Quality of life in chronic pain is more associated with beliefs about pain, than with pain intensity. European Journal of Pain 2005; 9:15–24 [DOI] [PubMed] [Google Scholar]
- 3.Keefe FJ, Lumley M, Anderson T, et al. Pain and emotion: new research directions. Journal of Clinical Psychology 2001; 57:587–607 [DOI] [PubMed] [Google Scholar]
- 4.Eccleston C. Role of psychology in pain management. British Journal of Anaesthesia 2001; 87:144–152 [DOI] [PubMed] [Google Scholar]
- 5.Eccleston C, Crombez G. Pain demands attention: a cognitive affective model of the interruptive function of pain. Psychological Bulletin 1999; 125:356–366 [DOI] [PubMed] [Google Scholar]
- 6.Kahneman D. (1973) Attention and effort. Englewood Cliffs, NJ: Prentice-Hall [Google Scholar]
- 7.Thalman NM, Thalmann D. (1999) Virtual reality software and technology. Encyclopedia of computer science and technology. Vol. 41 Marcel Dekker, Boca Raton, FL: Marcel Dekker, pp. 17–31 [Google Scholar]
- 8.Lengenfelder J, Schultheis MT, Al-Shibabi T, et al. Divided attention and driving: a pilot study using virtual reality technology. Journal of Head Trauma Rehabilitation 2002; 17:26–37 [DOI] [PubMed] [Google Scholar]
- 9.Kizony R, Katz N, Weiss PL. (2004) Virtual reality based intervention in rehabilitation: relationship between motor and cognitive abilities and performance within virtual environments for patients with stroke. In Proceedings of the 5th International Conference on Disability, Virtual Reality and Associated Technology Oxford, UK: The University of Reading, pp. 19–26 [Google Scholar]
- 10.Hoffman HG, Chambers GT, et al. Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. The Society for Behavioral Medicine 2011; 41:183–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maani C, Hoffman HG, DeSocio PA, et al. Pain control during wound care for combat-related burn injuries using custom articulated arm mounted virtual reality goggles. Journal of CyberTherapy & Rehabilitation 2008; 1:193–198 [Google Scholar]
- 12.Committee on Advancing Pain Research, Care, and Education; Institute of Medicine. (2011) Relieving pain in America: a blueprint for transforming prevention, care, education, and research. Washington, D.C.: The National Academies Press; [PubMed] [Google Scholar]
- 13.Wenig CM, Schmidt CO, Kohlmann T, et al. Costs of back pain in Germany. European Journal of Pain 2008; 13:280–286 [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. (2013) World health statistics. Geneva: WHO [Google Scholar]
- 15.Turk DC. Clinical effectiveness and cost-effectiveness of treatments for patients with chronic pain. Clinical Journal of Pain 2002; 18:355–365 [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. (1996) Cancer pain relief. With a guide to opioid availability. 2nd ed. Geneva: WHO [Google Scholar]
- 17.Turk DC, Loeser JD, Monarch ES. Chronic pain: purposes and costs of interdisciplinary rehabilitation programs. TENS: Trends in Evidence-Based Neuropsychiatry 2002; 4:64–69 [Google Scholar]
- 18.Onghena P, Van Houdenhove B. Antidepressant-induced analgesia in chronic nonmalignant pain: a meta-analysis of 39 placebo-controlled studies. Pain 1992; 49:205–219 [DOI] [PubMed] [Google Scholar]
- 19.Turjanski N, Lloyd GG. Psychiatric side-effects of medications: recent developments. Journal of Continuing Professional Development 2005; 11:58–70 [Google Scholar]
- 20.Department of Health and Human Services. (2011) Results from the 2011 National Survey on Drug Use and Health: summary of national findings. Washington, DC: HHS [Google Scholar]
- 21.New South Wales Ministry of Health. (2011) NSW pain management report. New South Wales: NSW [Google Scholar]
- 22.Gardner B. Effectiveness of the Nintendo® Wii Fit™ games on the balance of a community-dwelling older adult in Eastern North Carolina. Unpublished master's thesis, East Carolina University, Greenville, NC [Google Scholar]
- 23.Crews RT, Yalla SV, Fleischer AE, et al. A growing troubling triad: diabetes, aging, and falls. Journal of Aging Research 2013; 2013:1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giggins OM, Persson UM, Caulfield B. Biofeedback in rehabilitation. Journal of Neuroengineering & Rehabilitation 2013; 10:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Laufer Y, Dickstein R, Chefez Y, et al. The effect of treadmill training on the ambulation of stroke survivors in the early ages of rehabilitation: a randomized study. Journal of Rehabilitation Research & Development 2001; 38:69–78 [PubMed] [Google Scholar]
- 26.Gureje O, Von Korff M, Kola L, et al. The relation between multiple pain and mental disorders: results from World Mental Health Surveys. Pain 2008; 135:82–91 [DOI] [PubMed] [Google Scholar]
- 27.Wiseman T, Foster K, Curtis K. Mental health following traumatic physical injury: an integrative literature review. Injury 2012; 44:1–7 [DOI] [PubMed] [Google Scholar]
- 28.Wiederhold BK, Wiederhold MD. Managing pain in military populations with virtual reality. Pain syndromes—from recruitment to returning troops. NATO Science for Peace & Security Series—E: Human & Societal Dynamics 2012; 91:75–93 [Google Scholar]
- 29.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Annals of Behavioral Medicine 2012; 26:1–7 [DOI] [PubMed] [Google Scholar]
- 30.Chukoskie L, Soomro A, Townsend J, et al. (2013) “Looking” better: designing an at-home gaze training system for children with ASD. 6th International IEEE/EMBS Conference on Neural Engineering pp. 1246–1249 [Google Scholar]
- 31.Wiederhold MD, Wiederhold BK. (2008) Pain management with cell phone technology. Proceedings of the CyberTherapy Conference: Changing the Face of Healthcare, San Diego, CA: IEEE Publishing, pp. 1246–1249 [Google Scholar]
- 32.Pfurtscheller G, Leeb R, Faller J, et al. (2011) Brain–computer interface systems used for virtual reality control. In Virtual Reality. InTech, pp. 1–20 [Google Scholar]
- 33.Makeig S, Kothe C, Bigdely-Shamlo N, et al. Evolving signal processing for brain–computer interfaces. Proceedings of the IEEE 2012; 100:1567–1584 [Google Scholar]
- 34.Kipping B, Rodger S, Miller K, et al. Virtual reality for acute pain reduction in adolescents undergoing burn wound care: a prospective randomized controlled trial. Burns 2012; 38:650–657 [DOI] [PubMed] [Google Scholar]
- 35.Wiederhold MD, Wiederhold BK. Virtual reality and pharmaceuticals: enhanced synergy to improve clinical care. CyberTherapy & Rehabilitation 2013; 1:10–12 [Google Scholar]
- 36.Wiederhold MD, Wiederhold B.K. Virtual reality and interactive simulation for pain distraction. Pain Medicine 2007; 8:S182–S188 [Google Scholar]
- 37.Wiederhold MD, Wiederhold B.K. Virtual reality and interactive simulation for pain distraction. CyberTherapy & Rehabilitation 2010; 3:14–19 [Google Scholar]
- 38.Bidarra R, Gambon D, Kooij R, et al. (2013) Gaming at the dentist's—serious game design for pain and discomfort distraction. In Games for Health. Springer Vieweg, pp. 207–215 [Google Scholar]
- 39.Department of Health and Human Services. (2014) The budget for fiscal year 2014. Washington, DC: HHS [Google Scholar]
- 40.Zeher MJ, Armiger R, Burck J, et al. Using a virtual integration environment in treating phantom limb panic. Study for Health Technology Information 2011; 163:730–736 [PubMed] [Google Scholar]
- 41.Stetz MC, Brown KS, Folen RA, et al. Comparing distraction/relaxation modalities with chronic pain. Pain syndromes—from recruitment to returning troops. NATO Science for Peace & Security Series—E: Human & Societal Dynamics 2012; 91:171–177 [Google Scholar]
- 42.Rizzo A, Buckwalter G, Forbell E, et al. Virtual reality applications to address the wounds of war. Psychiatric Annals 2013; 43:123–138 [Google Scholar]
- 43.Wiederhold MD, Wiederhold BK. A review of pain management techniques for military populations. Pain syndromes—from recruitment to returning troops. NATO Science for Peace & Security Series—E: Human & Societal Dynamics 2012; 91:217–228 [Google Scholar]
- 44.McLay RN, Wood DP, Webb-Murphy JA, et al. A randomized, controlled trial of virtual reality-graded exposure therapy for post-traumatic stress disorder in active duty service members with combat-related post-traumatic stress disorder. Cyberpsychology, Behavior, & Social Networking 2011; 14:223–229 [DOI] [PubMed] [Google Scholar]
- 45.Department of Veteran's Affairs. (2014) The budget for fiscal year 2014. Washington, DC: VA [Google Scholar]
- 46.Summers RL, Johnston SL, Marshburn TH, et al. Emergencies in space. Annals of Emergency Medicine 2005; 46:177–184 [DOI] [PubMed] [Google Scholar]
- 47.Styf JR, Hutchinson K, Carlsson S. Depression, mood state, and back pain during microgravity conditions. Psychosomatic Medicine 2001; 63:862–864 [DOI] [PubMed] [Google Scholar]
- 48.Bichindaritz I, Vaidya S, Jain A, et al. A portable wireless solution for back pain telemonitoring: a 3D-based, virtual reality approach. Computational Intelligence in Healthcare 2010; 4:425–461 [Google Scholar]
- 49.Center for Disease Control and Prevention. (2012) Arthritis: meeting the challenge of living well. Washington, DC: HHS [Google Scholar]
- 50.Center for Disease Control and Prevention. (2014) The budget for fiscal year 2014. Washington, DC: HHS [Google Scholar]
- 51.European Innovation Partnership on Active and Healthy Ageing. (2013) Excellent innovation for ageing. Brussels: EU [Google Scholar]
- 52.Department of Labor. (2014) Occupational safety and health administration common statistics. Washington, DC: DofL [Google Scholar]
- 53.National Institute of Health. (2013) The 8th Annual NIH Pain Consortium Symposium on Advances in Pain Research: Integrating Self-Management Strategies for Chronic Pain. Washington, DC: HHS [Google Scholar]
- 54.Consumer Product Safety Commission. (2012) NEISS data highlights. Bethesda, MD [Google Scholar]