Abstract
We explored the use of virtual reality distraction techniques for use as adjunctive therapy to treat chronic pain. Virtual environments were specifically created to provide pleasant and engaging experiences where patients navigated on their own through rich and varied simulated worlds. Real-time physiological monitoring was used as a guide to determine the effectiveness and sustainability of this intervention. Human factors studies showed that virtual navigation is a safe and effective method for use with chronic pain patients. Chronic pain patients demonstrated significant relief in subjective ratings of pain that corresponded to objective measurements in peripheral, noninvasive physiological measures.
Introduction
Pain medications are the third most written prescription today, and few prescription pain drugs achieve acceptable pain relief in more than 50% of treated patients. Many people deal with physical pain in their daily lives, and the pain can range from mild to excruciating. The most common causes of pain include chronic illness, accidents, surgery, advanced cancer, lower back problems, arthritis, shingles, headaches, and fibromyalgia. Additionally, many of these patients have problems obtaining adequate medication to control their pain.1 One way to help is by using virtual reality (VR) to draw attention away from the patients' mental processing, thereby decreasing the amount of pain consciously experienced by the patient.
VR has also been found to be effective in reducing reported pain and distress in patients undergoing burn wound care, chemotherapy, dental procedures, venipuncture, and prolonged hospital visits.2–16 It appears that VR may change how the brain physically registers pain, not just the perception of pain stimuli.2 An interesting study showed that 86% of patients undergoing wound care from a burn injury reported severe to excruciating pain even with therapeutic levels of opioids.3 The challenges of treating severe pain confront clinicians daily. The search for adjunctive techniques has led to a number of studies where pharmacological agents are combined with behavioral modification approaches. More recently, distraction techniques have been used as an adjunct during unpleasant medical procedures. Examples of these techniques include deep breathing, viewing videotapes, listening to music, and playing video games.4–6 The success of these psychologically based techniques has led to the innovative use of VR as a distraction technique (see Table 1).
Table 1.
Current Research of Virtual Reality (VR) Treatment of Chronic Pain
| Title | Method | Result |
|---|---|---|
| Do Neck Kinematics Correlate with Pain Intensity, Neck Disability or with Fear of Motion?16 | Twenty-five patients (19 females, 6 males; mean age 39±12.7 years) with chronic neck pain participated in this cross-sectional study. A customized VR system was employed to evaluate cervical range of motion (ROM) and kinematics, using an interactive game controlled by cervical motion via electromagnetic tracking. Self-reported outcome measures included pain intensity (visual analog scale), disability (Neck Disability Index), and fear of motion (TAMPA scale of kinesiophobia). Kinematic measures included cervical ROM, mean and peak velocity, and number of velocity peaks (NVP) reflecting smoothness of motion. | Results showed significant correlations of approximately 0.4–0.6 between ROM and fear of motion, pain intensity, and disability. All 12 kinematic measures were correlated with fear of motion, but only a few were correlated with pain intensity, and with disability. The results emphasize fear of motion as a subjective measure primarily correlated with neck kinematics, including range, velocity, and smoothness of cervical motion. The level of neck disability was found to be partly related to ROM or to other kinematic impairments. However, ROM by itself remains a valid measure related to pain intensity and to fear of motion in patients with chronic neck pain. All correlations demonstrated were moderate, indicating that these measures involve other factors in need of further research. |
| A Virtual Reality System Combined with Biofeedback for Treating Pediatric Chronic Headache—A Pilot Study17 | Ten children attending an outpatient pediatric neurology clinic were treated by the proposed system. Participants practiced relaxation with biofeedback and learned to associate successful relaxation with positive pain-free virtual images of themselves. | Nine patients completed the 10-session intervention. Ratings of pain, daily functioning, and quality of life improved significantly at 1 and at 3 months post-treatment. Most patients reported applying their newly acquired relaxation and imagery skills to relieve headache outside the lab. |
| Virtual Visual Effect of Hospital Waiting Room on Pain Modulation in Healthy Subjects and Patients with Chronic Migraine18 | Sixteen CM and 16 controls underwent 62 channels LEPs from the right hand, during a fully immersive VR experience, where two types of waiting rooms were simulated. The RH simulated a classical hospital waiting room while the IH represented a room with sea viewing. | CM patients showed a reduction of laser pain rating and vertex LEPs during the IH vision. The sLORETA analysis confirmed that in CM patients the two VR simulations induced a different modulation of bilateral parietal cortical areas (precuneus and superior parietal lobe), and superior frontal and cingulate girus, in respect to controls. |
| Virtual Reality in the Treatment of Fibromyalgia: A Pilot Study19 | The sample comprised six women diagnosed with fibromyalgia (FM) according to the American College of Rheumatology guidelines (1990). The treatment program consisted of 10 sessions of group CBT with the support of an adaptive virtual environment (VE) containing a specific content for developing relaxation and mindfulness skills. Patients were assessed at pretreatment, post-treatment, and at a 6 months follow-up for the following outcome variables: functional status related to pain, depression, a negative and positive affect, and coping skills. | The results showed the long-term benefits of significantly reduced pain and depression and an increased positive affect and use of healthy coping strategies. |
| Using Mirror Visual Feedback and Virtual Reality to Treat Fibromyalgia20 | We have previously used noninvasive mirror visual feedback to treat subjects with chronic pain from phantom limbs and suggested its use for complex regional pain syndrome: once considered intractable pain. We wondered whether such methods would work to alleviate the chronic pain of FM. We tested mirror visual feedback on one FM patient. | On 15 trials, the patient's lower limb pain rating (on a scale from 1 to 10) decreased significantly. These preliminary results suggest that noninvasive dissociative anesthetics such as VR goggles, ketamine, and mirror visual feedback could be used to alleviate chronic pain from FM. |
| Nonimmersive Virtual Reality Mirror Visual Feedback Therapy and Its Application for the Treatment of Complex Regional Pain Syndrome: An Open-Label Pilot Study21 | A small open-label case series. Five patients with complex regional pain syndrome received VR mirror visual feedback therapy once a week for five to eight sessions on an outpatient basis. Patients were monitored for continued medication use and pain intensity. | Four of the five patients showed >50% reduction in pain intensity. Two of these patients ended their visits to our pain clinic after five sessions. |
| Neck Pain Assessment in a Virtual Environment22 | Cervical range of motion (CROM) measures were collected from 25 symptomatic and 42 asymptomatic individuals using VR and conventional assessments. Analysis of variance was used to determine differences between groups and assessment methods. Logistic regression analysis, using a single predictor, compared the diagnostic ability of both methods. | Results obtained by both methods demonstrated significant CROM limitations in the symptomatic group. The VR measures showed greater CROM and sensitivity while conventional measures showed greater specificity. A single session exposure to VR resulted in a significant increase in CROM. |
| Virtual Reality Hypnosis for Pain Associated with Recovery from Physical Trauma23 | The authors report a randomized, controlled study of 21 hospitalized trauma patients to assess the analgesic efficacy of virtual reality hypnosis (VRH)-hypnotic induction and analgesic suggestion delivered by customized VR hardware/software. Subjective pain ratings were obtained immediately and 8 hours after VRH (used as an adjunct to standard analgesic care) and compared to both adjunctive VR without hypnosis and standard care alone. | VRH patients reported less pain intensity and less pain unpleasantness compared to control groups. |
| Effects of Virtual Reality Immersion and Audiovisual Distraction Techniques for Patients with Pruritus24 | Twenty-four patients suffering from chronic pruritus—16 due to atopic dermatitis and eight due to psoriasis vulgaris—were randomly assigned to play an interactive computer game using a special visor or a computer screen. Pruritus intensity was self-rated before, during, and 10 minutes after exposure using a visual analog scale ranging from 0 to 10. The interviewer rated observed scratching on a three-point scale during each distraction program. | Student's t tests were significant for reduction of pruritus intensity before and during VRI and AVD (p=0.0002 and p=0.01 respectively), and were significant only between ratings before and after VRI (p=0.017). Scratching was mostly absent or mild during both programs. |
| Exploratory Findings with Virtual Reality for Phantom Limb Pain: From Stump Motion to Agency and Analgesia25 | A sample of subjects with “arm” (n=7) and “leg” (n=7) amputations underwent trials of a VR system, controlled by motion captured from their stump, which was translated into movements of a virtual limb within the VR environment. Measures of pain in the phantom limb were elicited from patients before and during this exercise as they attempted to gain agency for the movement they saw, and feel embodied within the limb. After this, each subject was interviewed about their experiences. | Five subjects in each group felt the virtual limb to be moved by them and felt sensations of movement within it. With this, they also reported reductions in their phantom limb pain greater than expected from distraction alone. No carry over effect was seen. |
A study conducted by Sarig et al. explored the use of VR in managing chronic neck disability and pain. Twenty-five symptomatic and 42 asymptomatic individuals reported pain using conventional pain ratings as their cervical range of motion was measured. The goal of the study was to determine if range of motion correlates with pain management. Results indicated significant limitations in range of motion measurements, as they showed sensitivity but lacked specificity.22 In 2013, Sarig et al. conducted a similar study to explore the issue further. Out of 25 patients, a comparison of self-reported outcomes and cervical range of motion showed correlations of 0.4–0.6 between the two measurements. This objective quotient indicates that subjective pain ratings can be supplemented with range of motion measurements and fear of motion reports to measure pain for physical rehabilitation studies. Moreover, VR was seen to not only reduce pain but objectively increase function.16
A pilot study of VR to treat fibromyalgia in 2013 studied the long-term effects of VR therapy. The six women in the study who had undergone 10 sessions of therapy supported by adaptive virtual environments (VEs) were assessed at pretreatment, post-treatment, and at 6 months follow-up. Results show that both depression rates were significantly reduced and coping strategies reflected positive growth.19 Another fibromyalgia study considered the use of noninvasive mirror visual feedback using VR to treat chronic pain of one fibromyalgia patient using ketamine as a pain reliever. On a 15 trial experiment, patient pain was shown to have decreased significantly, indicating the supplementary nature of VR with other medications.20
In 2010, Patterson et al. combined VR with hypnosis. The randomized, controlled study of 21 trauma patients compared subjective pain ratings of patients that were induced under VRH (virtual reality hypnosis) and standard VR. Positive results of VRH therapy indicate a synergistic and additive effect of the analgesic efficacy of hypnosis and VR distraction techniques.23
Other chronic conditions have been studied using VR as an adjunctive treatment. The first dermatological study of pruritus was conducted in 2009. Exposure to a computer-simulated game seemed to reduce the subjective pruritus intensity significantly among the 24 patients. Although pain and itching are activated under different internal brain mechanisms, a comparison of the commonalities of pain receptors, activations, and neural pathways can lead to insights on how to use these tools for the treatment of a variety of conditions such as chronic itching and chronic pain.24
Methods
Participating in this study to investigate the efficacy of an interactive VE were 40 patients aged 22–68 years with average daily pain for at least 3 months and a daily average pain intensity score of ≥4 (0=no pain, 10=worst possible pain).
Results
Before we tested the pain distraction system on patients, we wanted to validate usability and safety in controls. To determine the human factors related to the use of our pain distraction system, we conducted an initial study with 15 controls. The subjects were enrolled as per the approved IRB protocol and signed the consent form. All participants went through a 15 minute VR exposure session while wearing a HMD. The VEs consisted of pleasant and relaxing scenes, including natural areas such as forests, beaches, and mountains. Relaxing music and soothing effects such as the branches swaying and tall grass moving were added. Tree branches for example moved six to eight times per minute to guide breathing regulation.
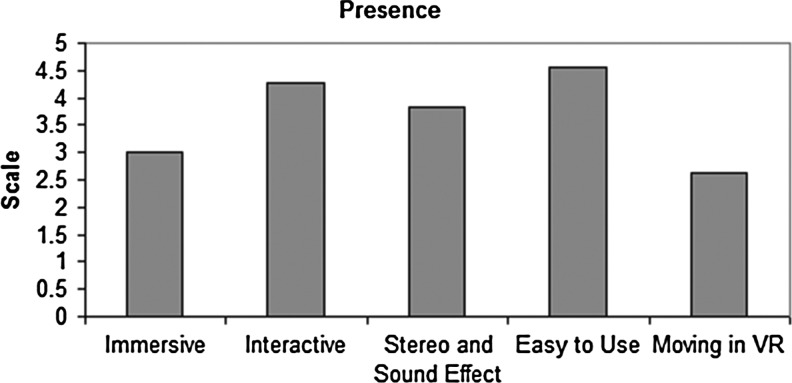
Self-report questionnaires were completed by participants and scored on a scale of 1 to 7, where 1=“no effect” and 7=“highly effective.” Overall the pain distraction VE was found easy to use, had good stereo sound effects, and was immersive and interactive (see Figs. 1–3).
FIG. 1.
The scales of sense of being in the virtual reality (VR) simulated environment—Ease of use, Immersive, and Interactive effects on a scale from 1 to 7, where 7 represents the normal experience of being in a place. 1=“not at all,” 7=“very much.” VR environment was easy to use, interactive, immersive, and real.
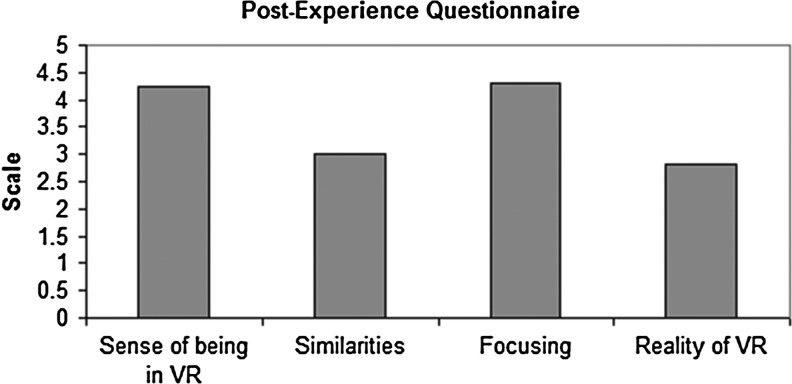
FIG. 2.
The scales of sense of being in the VR—how real was VR versus the simulated environment, similarities between the simulated environment and the actual places patients visited, how focused on the tasks patients were during the simulated environment, on a scale from 1 to 7, where 7 represents the normal experience of being in a place. 1=“not at all,” 7=“very much.” VR was immersive and real.
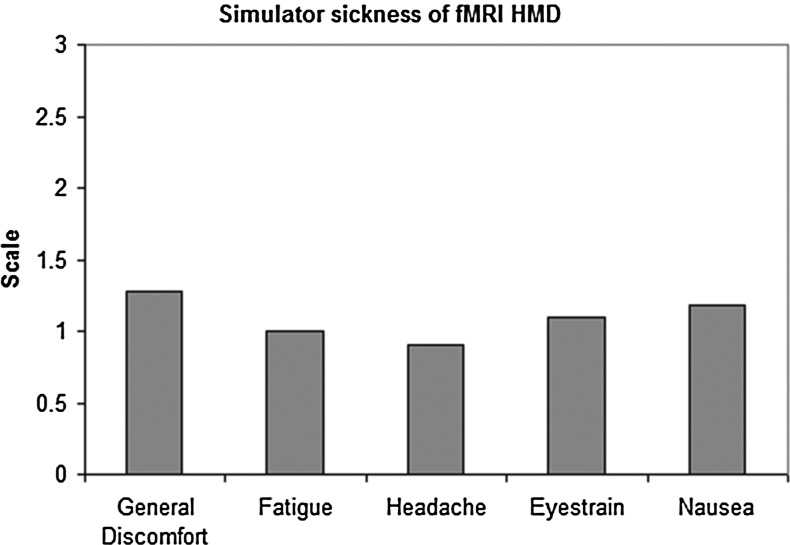
FIG. 3.
Sickness exploration questionnaire scores in terms of general discomfort, fatigue, headache, eyestrain, and nausea, their mean scales are all <1.5, where the scales range from 0 to 3. 0=“Absent,” 3=“Severe.” No serious side effects were observed. It was determined that VR was indeed safe to use with this population.
Controls reported good levels of presence and immersion when using the environments. The system was easy to use and understand. Evaluation of post-experience questionnaires showed that the sense of being in the VEs was high. This sense of being in VR correlated well with levels of immersion and interactivity on the presence questionnaires. Because we were concerned with potential adverse effects in patients using the VR system, we administered the Simulator Sickness Questionnaire. This questionnaire showed very low levels of fatigue, headache, eyestrain, and nausea when using the VR system. These low numbers indicate the VR system is both safe and effective.
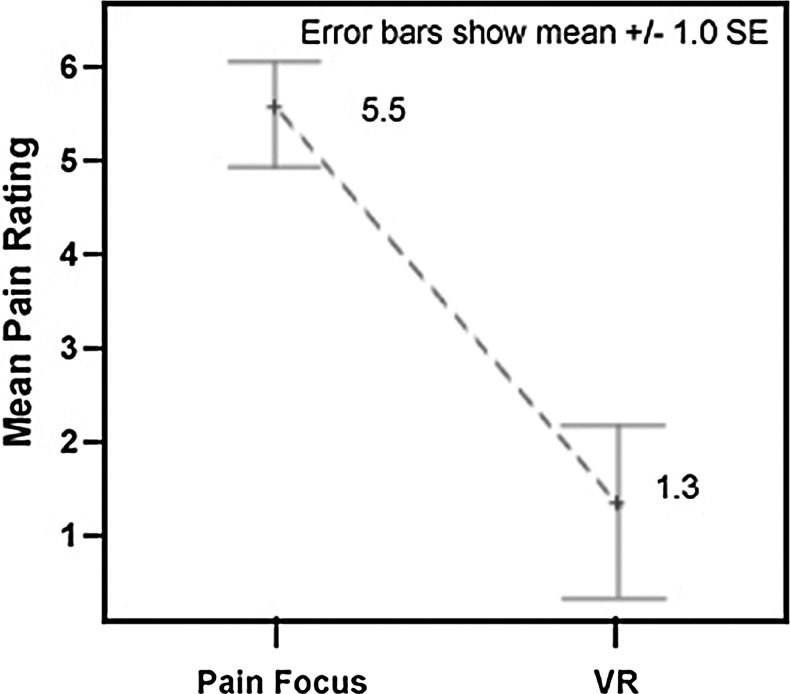
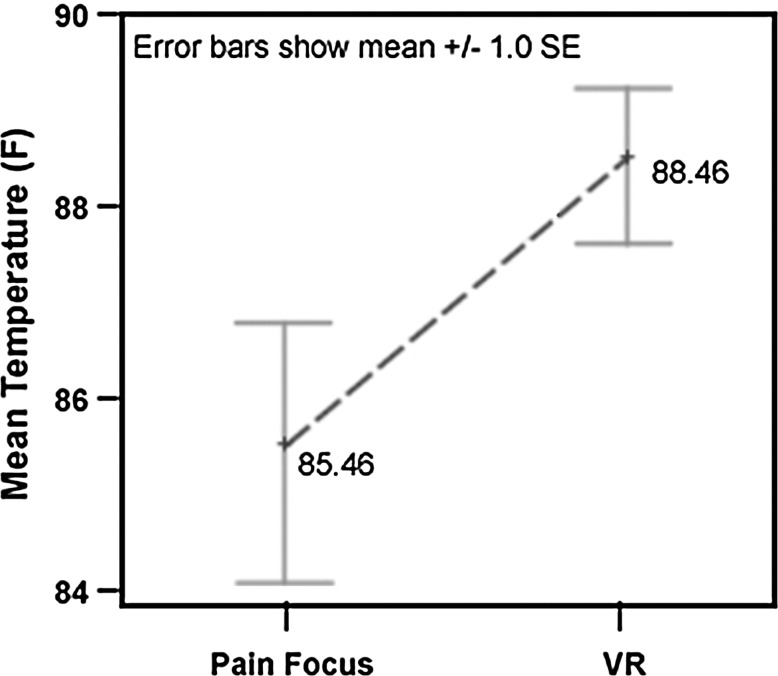
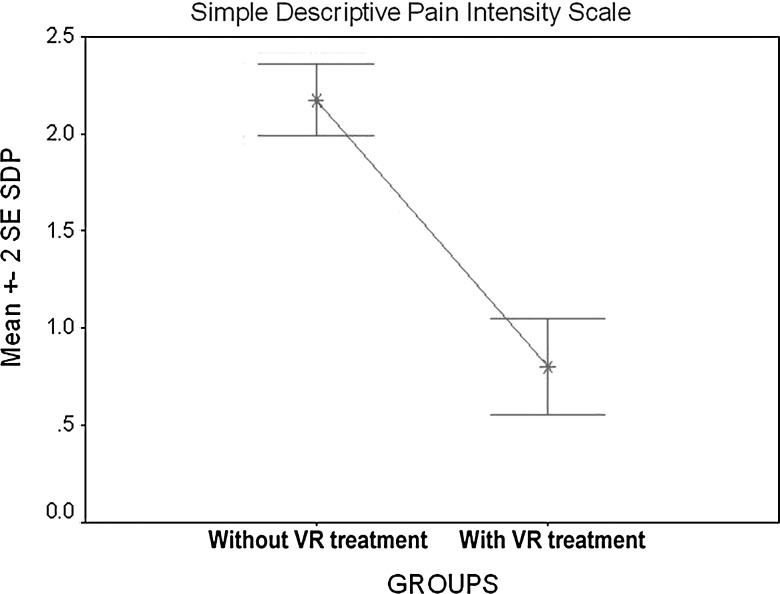
In our first pilot study, six chronic pain patients, ranging in age from 22 to 68 years, tested the VE with a head-mounted display and physiological sensors. All six participants reported a drop in pain while in the VE, and the magnitude of pain reduction from the VR compared to the pain focus condition was large (75.8%) and significant. A nonparametric Wilcoxon signed rank test indicated that the mean pain rating during the VR condition was significantly lower than the session with no distraction (n=6; p=0.028). Each of the six participants exhibited higher mean skin temperature when engaged in the VE than when in the pain focus condition. A paired t test also indicated that the overall mean temperature was significantly higher when participants were using VR (df=5; p=0.004). A higher average temperature in VR suggests a reduced level of discomfort and anxiety, substantiates the self-reported pain ratings, and suggests that VR is an effective method of reducing pain and anxiety (see Figs. 4 and 5).
FIG. 4.
Comparison of subjective pain ratings.
FIG. 5.
Comparison of objective pain ratings.
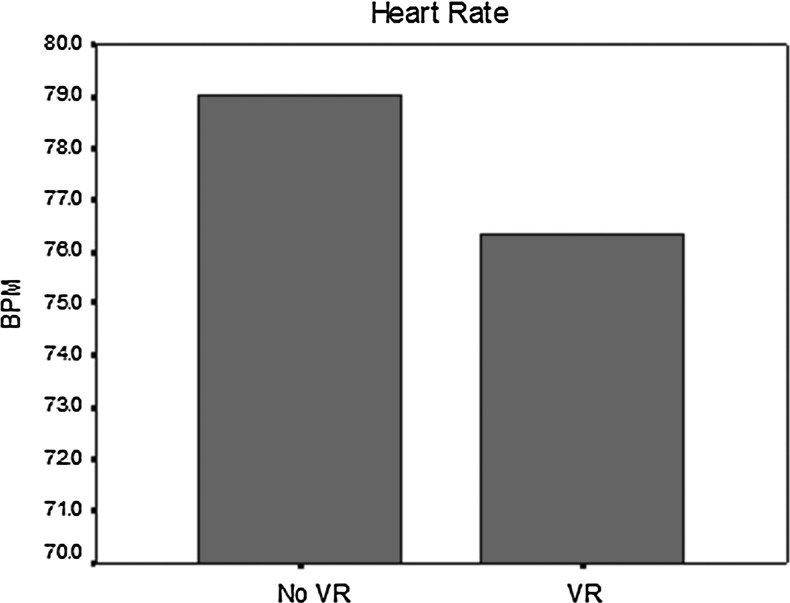
As in the previous study, we compared a pain focus condition to a VE exploration condition in 34 additional chronic pain patients. Data on heart rate and skin temperature were collected, as well as pain intensity ratings obtained from self-report questionnaires. All patients reported a decrease in pain while in the VE, with significance ranging from p<0.05 to p<0.001, depending upon which of the three pain rating scales were used (see Fig. 6). The significant decrease in heart rate (p<0.05) while the patients were in the VE indicates a reduced level of pain and anxiety, and suggests that VR is an effective method of reducing this distress (see Fig. 7).
FIG. 6.
Comparison of reported pain intensity.
FIG. 7.
Comparison of heart rate.
Discussion
Overall, the results of this study show VR is effective at reducing pain. Within the subjective outcomes, patients reported significantly lower pain ratings while exploring the VE than during the pain focus session. Several patients reported encouraging feedback as well, such as “this is the first pain relief I have had in 3 years,” “I was so busy playing the game, I forgot about my pain,” and “even though the procedure was finished, I wanted to keep playing.” This shows that this technology is significant not only in reducing pain but also in eliminating the interruptive nature of chronic pain.
Moreover, objective measures further supported the reduction of pain with use of the VR system. Skin temperature was significantly higher and heart rate was lower during the VR session, which indicates greater relaxation.
In virtual technologies, a necessary factor to consider is the presence felt by the user. In a study conducted by Hoffman et al., the distractive properties of a virtual program were greatly enhanced with higher immersion and presence of the VE used to reduce pain and anxiety of burn patients.26 Similarly, a comprehensive review of immersiveness on physiology reported that greater immersion has relaxing effects on physiological factors such as heart rate, respiration rate, skin temperature, and skin resistance.27 Due to the high presence and realism scores of the self-report surveys, the virtual program used in this study can be considered as effective in engaging patients, and thus distracting from pain.
Additional studies can further determine the correlation between presence and pain management, as well as the association of pain distracting qualities of VR and various types of pain.
Acknowledgments
We thank the National Institute on Drug Abuse, National Institutes of Health for partial funding of this project. We also thank the participants who were willing to spend time with our clinical team.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Brody JE. (2006) Let's get serious about relieving chronic pain. The New York Times, Jan. 6, 2006. www.nytimes.com/2006/01/10/health/10brod.html?pagewanted=all&_r=0 (accessed Mar. 23, 2014)
- 2.Hoffman HG. (2004) Virtual-reality therapy. Scientific American. www.hitl.washington.edu/projects/vrpain/index_files/SCIAMFin.pdf (accessed Mar. 22, 2014) [DOI] [PubMed]
- 3.Hoffman HG, Patterson DR, Carrougher GJ. Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy. Clinical Journal of Pain 2000; 17:229–235 [DOI] [PubMed] [Google Scholar]
- 4.Schneider SM, Workman ML. Effects of virtual reality on symptom distress in children receiving chemotherapy. CyberPsychology & Behavior 1999; 2:125–134 [DOI] [PubMed] [Google Scholar]
- 5.Schneider SM. (2003) Virtual reality for the treatment of breast cancer. CyberTherapy. San Diego, CA: Interactive Media Institute [Google Scholar]
- 6.Schneider SM, Ellis M, Coombs WT, et al. Virtual reality intervention for older women with breast cancer. CyberPsychology & Behavior 2003; 6:301–307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vazquez JLM, Santander A, Gao K, et al. Using cybertherapy to reduce postoperative anxiety in cardiac recovery intensive care units. Journal of Anesthesia & Clinical Research 2013; 4:363 [Google Scholar]
- 8.Mühlberger A, Wieser MJ, Kenntner-Mabiala R, et al. Pain modulation during drives through cold and hot virtual environments. CyberPsychology & Behavior 2007; 10:516–522 [DOI] [PubMed] [Google Scholar]
- 9.Wiederhold BK, Wiederhold MD. Managing pain in military populations with virtual reality. NATO Science for Peace & Security Series—E: Human & Societal Dynamics 2012; 91:75–93 [Google Scholar]
- 10.Mosso JL, Rizzo S, Wiederhold B, et al. Cybertherapy—new applications for discomfort reductions. Surgical care unit of heart, neonatology care unit, transplant kidney care unit, delivery room-cesarean surgery and ambulatory surgery, 27 case reports. Studies in Health Information & Informatics 2007; 125:334–336 [PubMed] [Google Scholar]
- 11.Hoffman HG, Doctor JN, Patterson DR, et al. (2000) Virtual reality as an adjunctive pain control during burn wound care in adolescent patients. Pain 85: 305–309 [DOI] [PubMed] [Google Scholar]
- 12.Hoffman HG, Garcia-Palacios A, Patterson DR, et al. The effectiveness of virtual reality for dental pain control: a case study. CyberPsychology & Behavior 2001; 4:527–535 [DOI] [PubMed] [Google Scholar]
- 13.Hoffman HG, Patterson DR, Carrougher GJ, et al. Effectiveness of virtual reality-based pain control with multiple treatments. The Clinical Journal of Pain 2001; 17:229–235 [DOI] [PubMed] [Google Scholar]
- 14.Hoffman HG, Coda BA, Sharar SR, et al. (2003). Virtual reality analgesia during thermal and electrical pain for longer durations, and multiple treatments. CyberTherapy. San Diego, CA: Interactive Media Institute [Google Scholar]
- 15.Tse MMY, Ng JKF, Chung JWY. (2003) Visual stimulation as pain relief for Hong Kong Chinese patients with leg ulcers. CyberTherapy. San Diego, CA: Interactive Media Institute; [DOI] [PubMed] [Google Scholar]
- 16.Sarig Bahat H, Wiess PL, Sprecher E, et al. Do neck kinematics correlate with pain intensity, neck disability or with fear of motion? Manual Therapy 2013November9; doi: 10.1016/j.math.2013.10.006 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Shiri S, Feintuch U, Weiss N, Pustilnik A, Geffen T, Kay B, Meiner Z, Berger I. A virtual reality system combined with biofeedback for treating pediatric chronic headache—a pilot study. Pain Medicine 2013; 14:621–627 [DOI] [PubMed] [Google Scholar]
- 18.De Tommaso M, Ricci K, Laneve L, et al. Virtual visual effect of hospital waiting room on pain modulation in healthy subjects and patients with chronic migraine. Pain Research & Treatment 2013;515730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Botella C, Garcia-Palacios A, Vizcaino Y, et al. Virtual reality in the treatment of fibromyalgia: a pilot study. Cyberpsychology, Behavior, & Social Networking 2013; 16:215–223 [DOI] [PubMed] [Google Scholar]
- 20.Ramachandran VS, Seckel EL. Using mirror visual feedback and virtual reality to treat fibromyalgia. Medical Hypotheses 2013; 75:495–496 [DOI] [PubMed] [Google Scholar]
- 21.Sato K, Fukumori S, Matsusaki T, et al. Nonimmersive virtual reality mirror visual feedback therapy and its application for the treatment of complex regional pain syndrome: an open-label pilot study. Pain Medicine 2010; 11:622–629 [DOI] [PubMed] [Google Scholar]
- 22.Sarig-Bahat H, Weiss PL, Laufer Y. Neck pain assessment in a virtual environment. Spine 2010; 35:E105–112 [DOI] [PubMed] [Google Scholar]
- 23.Patterson DR, Jensen MP, Wiechman SA, et al. Virtual reality hypnosis for pain associated with recovery from physical trauma. The International Journal of Clinical & Experimental Hypnosis 2010; 58:288–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Leibovici V, Magora F, Cohen S, Ingber A. Effects of virtual reality immersion and audiovisual distraction techniques for patients with pruritus. Pain Research & Management 2009; 14:283–286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cole J, Crowle S, Austwick G, et al. Exploratory findings with virtual reality for phantom limb pain; from stump motion to agency and analgesia. Disability & Rehabilitation 2009; 31:846–854 [DOI] [PubMed] [Google Scholar]
- 26.Hoffman HG, Patterson DR, Carrougher GJ. Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: a controlled study. Clinical Journal of Pain 2000; 16:244–250 [DOI] [PubMed] [Google Scholar]
- 27.Wiederhold BK, Davis R, Wiederhold MD. The effects of immersiveness on physiology. Virtual Environments in Clinical Psychology & Neuroscience 1998; 58:52–60 [PubMed] [Google Scholar]