Abstract
Surgical anxiety creates psychological and physiological stress, causes complications in surgical procedures, and prolongs recovery. Relaxation of patients in postoperative intensive care units can moderate patient vital signs and reduce discomfort. This experiment explores the use of virtual reality (VR) cybertherapy to reduce postoperative distress in patients that have recently undergone cardiac surgery. Sixty-seven patients were monitored at IMSS La Raza National Medical Center within 24 hours of cardiac surgery. Patients navigated through a 30 minute VR simulation designed for pain management. Results were analyzed through comparison of pre- and postoperative vital signs and Likert scale survey data. A connection was found in several physiological factors with subjective responses from the Likert scale survey. Heavy positive correlation existed between breathing rate and Likert ratings, and a moderate correlation was found between mean arterial pressure and Likert ratings and heart rate and Likert ratings, all of which indicated lower pain and stress within patients. Further study of these factors resulted in the categorization of patients based upon their vital signs and subjective response, providing a context for the effectiveness of the therapy to specific groups of patients.
Introduction
When faced with upcoming surgeries, patients often claim a psychological fear of surgical failure, anesthesia, or the “unknown.”1 A widely accepted cause of surgical anxiety is the recently increasing demands for efficiency in hospital operations, leading to less time spent by healthcare professionals to assure patients of their well-being. Patients also suggest personal reasons for experiencing surgery-related anxiety, including sociodemographic or psychological variables, or past surgical experiences.2 Patients under surgical distress can experience adverse effects on their mental and physiological states, and slowed postoperative recovery.3 Even patients who report rare accounts of anxiety are susceptible to physiological changes, including increased respiratory rate, heart rate, blood pressure, vasoconstriction, and gastric stasis.4 Intense forms of surgical distress can activate the sympathetic nervous system and downregulate immune functions.5
By addressing this issue, hospitals would improve surgery outcomes, patient recovery, and patient psychological and physical well-being. Efforts are currently centered on preoperative anxiety. Medical interventions, such as midazolam, and therapeutic attempts, such as music in waiting rooms, have shown mixed results.6
Virtual reality (VR) methods have been previously explored for postoperative cases, most of which have focused on two cases: burn victims and children (see Table 1). Burn victims have shown to be a popular application of VR therapy due to the painful nature of postburn physical therapy. Past studies have explored pain management of burn injuries by measuring pain scores, as well as maximal joint range of motion immediately and after therapy. Results indicate that post-therapy pain ratings dropped, patients spent less time thinking about the pain, and a vast majority enjoyed the simulation. Similarly, distraction techniques have shown promise in use with pediatric operations. While some studies show subjective pain measurements decreased under VR conditions, others show that no measureable differences were found in either pain or distress, but the simulations were qualified as distracting.
Table 1.
Previous Research of Virtual Reality (VR) Distraction for Surgical Procedures
| Title/authors | Method | Results |
|---|---|---|
| The Use of the Virtual Reality as Intervention Tool in the Postoperative of Cardiac Surgery10 Cacau Lde A, Oliveira GU, Maynard LG, Araújo Filho AA, Silva WM Jr, Cerqueria Neto ML, Antoniolli AR, Santana-Filho VJ |
Patients were randomized into two groups: VR (VRG, n=30) and control (CG, n=30). The response to treatment was assessed through the functional independence measure (FIM), by the 6-minute walk test (6MWT) and the Nottingham Health Profile (NHP). Evaluations were performed preoperatively and postoperatively. | On the first day after surgery, patients in both groups showed decreased functional performance. However, the VRG showed lower reduction (45.712.3) when compared to CG (35.0612.09, p<0.05) on the first postoperative day, and no significant difference in performance on discharge day (p>0.05). In evaluating the NHP field, we observed a significant decrease in pain score at third assessment (p<0.05). These patients also had a higher energy level in the first evaluation (p<0.05). There were no differences with statistical significance for emotional reactions, physical ability, and social interaction. The length of stay was significantly shorter in patients of VRG (9.410.5 days vs. 12.2 1 0.9 days, p<0.05), which also had a higher 6MWD (319.9119.3 meters vs. 263.5115.4 meters, p<0.02). |
| Managing Pain in Military Populations with Virtual Reality11 Wiederhold BK, Wiederhold MD |
By constantly being exposed to combat and living in war zones, servicemen and women face increased risk of complicated injuries, including amputations, penetrating wounds, spinal cord injuries, and traumatic brain injuries (TBIs). In addition, many service members may undergo multiple surgical procedures as a result of serious injury. The incidence of pain syndromes is significantly higher when present with posttraumatic stress disorder (PTSD) and other psychiatric disorders such as depression. The combination of these “poly-trauma” events makes the management of both acute and chronic pain in military populations challenging. | A multifactorial approach is necessary, and the introduction of new approaches and technology can increase the numbers of tools available to combat this significant health issue in troops. |
| Comparing Distraction/Relaxation Modalities with Chronic Pain Patients12 Stetz MC, Brown KS, Folen RA, Nelson KL, Wiederhold BK |
At the present time, most providers treat chronic pain patients with a combination of analgesics and nondrug approaches. That said, many of these professionals are also starting to incorporate the use of technology (e.g., VR and biofeedback) into their practice. The purpose of this study was to compare standard chronic pain treatment (i.e., assisted relaxation with a clinician) with technology-assisted relaxation without a clinician. | Results suggest that there was a greater reduction in self-rated pain when participating in the relaxation imagery session enhanced with technology. |
| Virtual Reality Pain Control During Burn Wound Debridement of Combat-Rrelated Burn Injuries Using Robot-Like Arm Mounted VR Goggles13 Maani CV, Hoffman HG, Morrow M, Maiers A, Gaylord K, McGhee LL, DeSocio PA |
Patients were U.S. soldiers burned in combat attacks involving explosive devices in Iraq or Afghanistan. During the same wound care session using a within-subject experimental design, 12 patients received half of their severe burn wound cleaning procedure (∼6 minutes) with standard of care pharmacologies and half while in VR (treatment order randomized). Three 0 to 10 Graphic Rating Scale pain scores for each of the treatment conditions served as the primary variables. | Patients reported significantly less pain when distracted with VR. “Worst pain” (pain intensity) dropped from 6.25 out of 10 to 4.50 out of 10. “Pain unpleasantness” ratings dropped from “moderate” (6.25 out of 10) to “mild” (2.83 out of 10). “Time spent thinking about pain” dropped from 76% during no VR to 22% during VR. Patients rated “no VR” as “no fun at all” (<1 out of 10) and rated VR as “pretty fun” (7.5 out of 10). Follow-up analyses showed VR was especially effective for the six patients who scored 7 out of 10 or higher (severe to excruciating) on the “worst pain” (pain intensity) ratings. |
| Virtual Reality and Interactive Simulation for Pain Distraction8 Wiederhold MD, Wiederhold BK |
Current advances are being made to control pain by integrating both the science of pain medications and the science of the human mind. Various psychological techniques, including distraction by VR environments and the playing of video games, are being employed to treat pain. In VR environments, an image is provided for the patient in a realistic, immersive manner devoid of distractions. This technology allows users to interact at many levels with the VE, using many of their senses, and encourages them to become immersed in the virtual world they are experiencing. | When immersion is high, much of the user's attention is focused on the virtual environment (VE), leaving little attention left to focus on other things, such as pain. In this way, VR provides an effective medium for reproducing and/or enhancing the distractive qualities of guided imagery for the majority of the population who cannot visualize successfully. |
| The Effect of Virtual Reality on Pain and Range of Motion in Adults with Burn Injuries14 Carrougher GJ, Hoffman HG, Nakamura D, Lezotte D, Soltani M, Leahy L, Engrav LH, Patterson DR |
Thirty-nine inpatients, aged 21 to 57 years (mean 35 years), with a mean TBSA burn of 18% (range=3–60%) were studied using a within-subject, crossover design. All patients received their regular pretherapy pharmacologic analgesia regimen. During physical therapy sessions on two consecutive days (VR one day and no VR the other day; order randomized), each patient participated in active-assisted ROM exercises with an occupational or physical therapist. At the conclusion of each session, patients provided 0 to 100 Graphic Rating Scale measurements of pain after each 10 minute treatment condition. On the day with VR, patients wore a head-position-tracked, medical care environment excluding VR helmet with stereophonic sound and interacted in a VE conducive to burn care. ROM measurements for each joint exercised were recorded before and after each therapy session. | Because of nonsignificant carryover and order effects, the data were analyzed using simple paired t tests. VR reduced all Graphic Rating Scale pain scores (worst pain, time spent thinking about the pain, and pain unpleasantness by 27%, 37%, and 31% respectively), relative to the no VR condition. Average ROM improvement was slightly greater with the VR condition. However, this difference failed to reach clinical or statistical significance (p=0.243). Ninety-seven percent of patients reported zero to mild nausea after the VR session. |
| Virtual Reality on Mobile Phones to Reduce Anxiety in Outpatient Surgery15 Mosso JL, Gorini A, De La Cerda G, Obrador T, Almazan A, Mosso D, Nieto JJ, Riva G |
With the present randomized controlled study, we intended to verify the effectiveness of VR in reducing anxiety in patients undergoing ambulatory operations under local or regional anesthesia. In particular, we measured the degree to which anxiety associated with surgical intervention was reduced by distracting patients with immersive VR provided through a cell phone connected to an HMD compared to a no-distraction control condition. | A significant reduction of anxiety was obtained after 45 minutes of operation in the VR group, but not in the control group. After 90 minutes, the reduction was larger in the experimental group than in the control group. |
| The Use of Virtual Reality for Needle-Related Procedural Pain and Distress in Children and Adolescents in a Paediatric Oncology Unit16 Nilsson S, Finnström B, Kokinsky E, Enskär K |
Twenty-one children and adolescents were included in an intervention group with nonimmersive VR and another 21 children and adolescents in a control group where they underwent either venous punctures or subcutaneous venous port devices. Self-reported pain and distress, heart rate, and observational pain scores were collected before, during, and after the procedures. Semi-structured qualitative interviews were conducted in conjunction with the completed intervention. | Self-reported and observed pain and distress scores were low, and few significant differences of quantitative data between the groups were found. Two themes emerged in the analysis of the interviews; the VR game should correspond to the child and the medical procedure and children enjoyed the VR game and found that it did distract them during the procedure. |
| Using Cybertherapy to Reduce Postoperative Anxiety in Cardiac Recovery Intensive Care Units17 Vazquez JLM, Santander A, Gao K, Wiederhold MD, Wiederhold BK |
Twenty-two patients were monitored at IMSS La Raza National Medical Center within 24 hours of cardiac surgery. Patients navigated through a 30 minute VR simulation designed for pain management. Results were analyzed through comparison of pre- and postoperative vital signs and Likert scale survey data. | Likert test data showed that 21 of 22 subjects reported less discomfort after navigating through the VE. Physiological data generally supported the Likert data, with 64% of patients lowering respiratory rate, moderated blood carbon dioxide levels, and decreased diastolic blood pressures in another 64% of patients. |
| Virtual Reality as a Pediatric Pain Modulation Technique: A Case Study18 Steele E, Grimmer K, Thomas B, Mulley B, Fulton I, Hoffman H |
This case study explored the use of VR analgesia with a 16-year-old patient with cerebral palsy participating in a twice daily physiotherapy program following Single Event Multi-Level Surgery. Over 6 days, the patient spent half of his physiotherapy sessions using VR and the other half without (order randomized). Traditional pharmacological pain management was administered throughout the trial. | Using a subjective pain scale (5 faces denoting levels of pain), the patient's overall pain ratings while in the VR (experimental) condition were 41.2% less than those in the no-VR (control) condition. |
| Cybertherapy—New Applications for Discomfort Reductions. Surgical Care Unit of Heart, Neonatology Care Unit, Transplant Kidney Care Unit, Delivery Room-Cesarean Surgery and Ambulatory Surgery, 27 Case Reports19 Mosso JL, Rizzo S, Wiederhold B, Lara V, Flores J, Espiritusanto E, Minor A, Santander A, Avila O, Balice O, Benavides B |
27 patients have been participated in this preliminary report from 3 public hospitals from Mexico city in 2006. The VR scenarios were developed in the Virtual Reality Medical Center of San Diego CA, and the HMD is from the Southern University of los Angeles, CA. | The majority of patients demonstrated comfort with virtual scenarios during surgical procedures or hospitalization. |
In this study, we aim to address postoperative anxiety through the application of VR distraction therapy. Advancements in technology have allowed the use of VR in intensive care units (ICUs) to complement standard pain management techniques. A report by Kho et al. concluded that VR techniques are promising in their study of the efficacy of video games as an additional tool in physical therapy ICU patients.7 Another study at the Virtual Reality Medical Center correlates immersion in a virtual world with patients' attention to the virtual environment (VE) as opposed to pain.8 Immersiveness also has been shown to have beneficial effects on various physiological factors that link to anxiety, such as heart rate, respiratory rate, skin temperature, and skin resistance.9
Methodology
Patients (n=67; 25 female, 42 male) in the cardiac surgery department of IMSS La Raza National Medical Center were asked to participate in the study. Each patient was monitored in hyperacute units within 24 hours of their cardiac surgery, which included mitral valve replacement, aortic valve replacement, tricuspid valve replacement, coronary stent insertion, coronary revascularization, tricuspid plasty, ventricular communication repair, and bridge tricuspid resection.
The clinical team consisted of four physicians, nurses, and technicians. Procedural instructions were given to the patients after their admission to the ICU. Consent to participate and basic demographic information were collected. A clinical professional recorded relevant vital signs and administered the presimulation questionnaire to measure patient discomfort. Once all preliminary data were collected, the physician installed the head-mounted display on the patient's head to display a VR simulation. Meanwhile, a projector emitted the same simulation on the unit wall so the clinical team could follow along. The simulation consisted of a set of five cybertherapy environments (developed by the Virtual Reality Medical Center in San Diego, CA): Cliff, Dream Castle, Enchanted Forest, Icy Cool World, and Drive, Walk, Bike. The patient was allowed to explore the VE for 30 minutes. Throughout the simulations, all patients were conscious, had normal vision, free movement of limbs, and did not have airway cannulation or hemodynamic disorders. Postsimulation data were collected through a questionnaire and vital signs.
Results
Data analysis is composed of comparisons between pre and post cybertherapy vital signs and subjective scale results using a Likert scale design. Complications included a 68 year old female patient who experienced cardiac arrhythmia during treatment, and three patients who presented signs of nausea and vertigo that interrupted the cybertherapy session.
Overall, the results of the therapy were positive (see Fig. 1). Of the 67 patients, 59 patients (88%) reported a decreased level of pain experienced post-therapy. The mean change in the Likert scale was 3.75, which corresponds to a decrease from “severe” to “moderate” or “moderate” to “light.” Physiologically, 25 patients (37.3%) experienced reduced heart rates, 35 (52.2%) experienced reduced mean arterial pressure, and 14 (64%) of 22 patients tested for respiratory rate experienced a reduction.
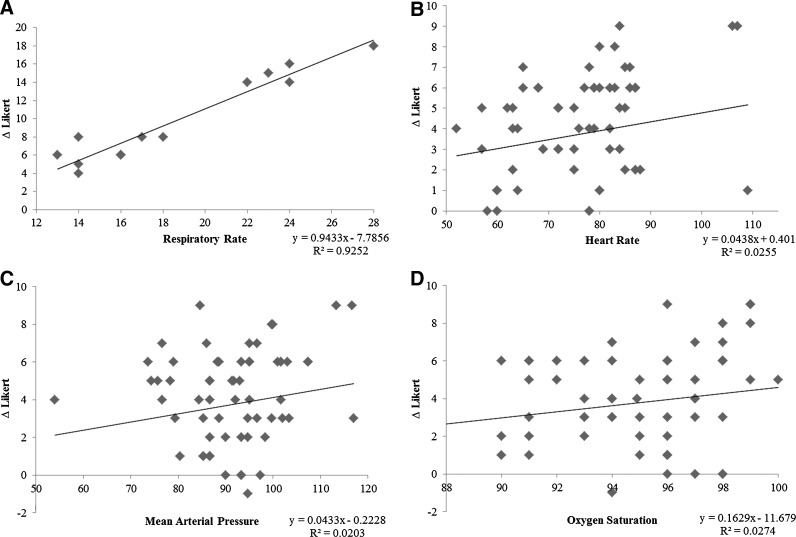
FIG. 1.
Correlation of physiological factors with change in subjective pain measurements. (A) Patients' initial respiratory rates and change in subjective responses were measured against each other. Upwards trend line indicates that patients with higher respiratory rates experienced a larger decrease in their reported pain. (B) Subjects with higher initial heart rates generally reported a larger decrease in pain post-therapy, while other subjects with lower to normal heart rates indicated little to no change in pain. (C) Initial mean arterial pressure and change in subjective ratings showed slight positive correlation. (D) Initial oxygen saturation and change in subjective pain responses showed slight correlation, possibly explained by the small range of possible oxygen saturation within healthy subjects.
Respiratory rate measurements were plotted against the change in subjective responses before and after the therapy treatment. The correlation had a linear fit, with an R2 value of 0.925. Similarly, heart rate and mean arterial pressure were plotted against the survey responses, showing positive correlation but with much higher variation (R2=0.025 and R2=0.02 respectively). Oxygen saturation showed similar trends. However, they were not as substantial as respiratory rate, heart rate, or mean arterial pressure.
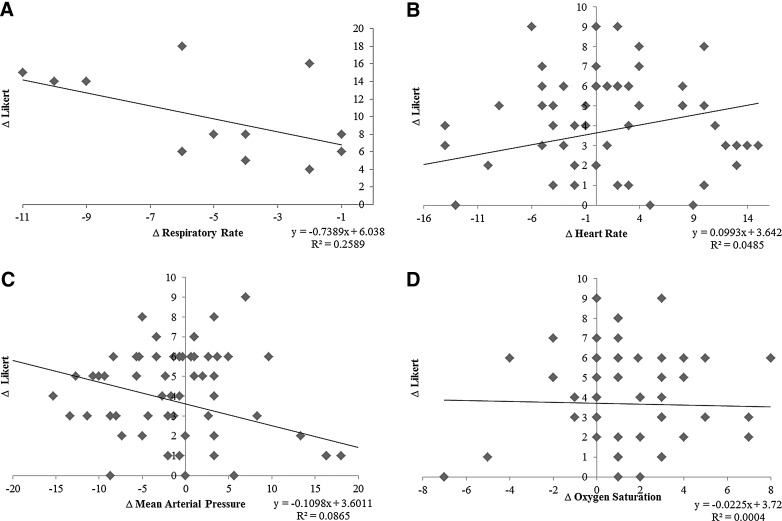
Interestingly, when the changes in the physiological factors were analyzed against the change in Likert scales, similar correlations existed (see Fig. 2). Thus, not only is there a trend in the match between objective and subjective pain measurements, but the level of pain reduction matches as well.
FIG. 2.
Correlation of change in physiological factors with change in subjective pain measurements. (A) Significant correlation existed between change in Likert scale responses and respiratory rate. (B) A positive sloping trend line for change in heart rate and change in subjective responses positively supports the calming effect of the simulation. (C) As opposed to heart rate, a decreasing trend for change in mean arterial pressure and change in Likert ratings indicates the same pain reducing effect. (D) Change in oxygen saturation and Likert responses showed little correlation, again, most likely due to the small range of oxygen saturation.
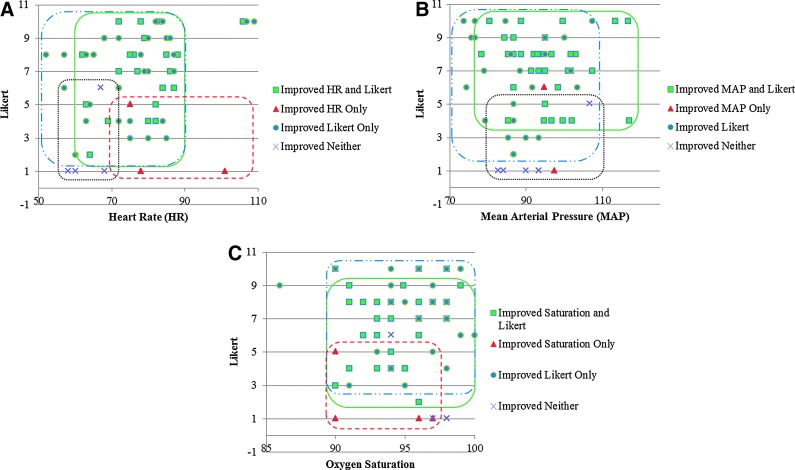
To provide further context to the patients who were positively affected by the therapy, patients were categorized using Boolean values based upon their change in responses (see Fig. 3). For each physiological factor, for example heart rate, patients were identified with “improvements in heart rate and reported survey response,” “improvement in heart rate, but not survey response,” “improvement in survey response, but not in heart rate,” and “improvement in neither heart rate nor survey response.” By categorizing patients into these groups, a visual representation of the type of patients that should undergo this therapy can be seen. Respiratory rate was not taken into consideration for this analysis due to the small sample size.
FIG. 3.
Categorization of patients using Boolean values. (A) Four distinct groups are seen using heart rate and subjective responses. Notably, those who improved in neither category had initially low heart rates and pain responses, whereas those who improved in both started with higher values. (B) Three groups are visualized, with patients that improved in MAP and Likert categories having a wide range of MAP but high pain ratings. (C) As expected, oxygen saturation values were evenly distributed across the healthy range.
Discussion
After cardiac surgery, it is common for patients to show symptoms of worry, apprehension, and depression. The melancholic state can last many weeks and disrupt recovery, both psychologically and physiologically. Patient relaxation can reduce postsurgical pain, improve overall well-being, and prevent hematomas and other complications. This experiment has shown that navigating through a VE can reduce psychological stress. Improvements could be made to the therapy content or procedure to benefit those who did not report positive changes in vital signs or discomfort, although we recognize that cybertherapy may not be suitable for some patients.
It is evident from past studies to date that presence is an important factor in delivering pain distraction. Hoffman et al. describes how immersion and presence enhances distractive properties of the VE.20 Wiederhold et al. presented comparisons of subjects that experienced varying levels of VR immersion, noting significant differences in not only subjective responses but also physiology.9 Considering the influence of immersion on the efficacy of pain distraction, a future improvement to this study could correlate the change in reported Likert pain ratings to a presence rating.
This is an uncontrolled study, possibly leading to overestimation of effectiveness. While not as extensive as a controlled trial, it is conclusive that there are changes in physiology before and after the virtual simulation, especially in the patient-reported discomfort scale. As this study was performed under real-world clinical conditions, the validity and clinical utility of the observed data are significant.
VR has shown to be a noninvasive and innocuous procedure to improve postsurgical distress in ICUs. Using this technology allows patients to interact at many levels with the VE, using multiple senses, and encourages them to become immersed in the virtual world they are experiencing. In this way, VR provides an effective medium for reproducing and/or enhancing the distractive qualities of a pain treatment. VR in ICUs represent a tremendous social impact in patients that are in critical condition by acting as additional support mechanism to avoid and reduce postsurgical distress.
Acknowledgments
We thank the National Institutes of Health, National Institute on Drug Abuse for funding of the virtual world development. We also thank the participants who were willing to spend time with our clinical team to answer questions and surveys.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Pritchard MJ. Identifying and assessing anxiety in pre-operative patients. Nursing Standard 2009; 51:35–40 [DOI] [PubMed] [Google Scholar]
- 2.Dirik G, Karanci AN. Predictors of pre- and postoperational anxiety in emergency surgery patients. Journal of Psychosomatic Research 2003; 4:363–369 [DOI] [PubMed] [Google Scholar]
- 3.Kiecolt-Glaser JK, Page GG, Marucha PT, et al. Psychological influences on surgical recovery. American Psychologist 1998; 11:1209–1218 [DOI] [PubMed] [Google Scholar]
- 4.Bailey L. Strategies for decreasing patient anxiety in the perioperative setting. Association of Perioperative Registered Nurses Journal 2010; 4:445–457 [DOI] [PubMed] [Google Scholar]
- 5.Moon JS, Cho KS. The effects of handholding on anxiety in cataract surgery patients under local anesthesia. Journal of Advanced Nursing 2001; 3:407–415 [DOI] [PubMed] [Google Scholar]
- 6.Ni CH, Tsai WH, Lee LM, et al. Minimising preoperative anxiety with music for day surgery patients—a randomised clinical trial. Journal of Clinical Nursing 2012; 21:620–625 [DOI] [PubMed] [Google Scholar]
- 7.Kho ME, Damluji A, Zanni JM, et al. Feasibility and observed safety of interactive video games for physical rehabilitation in the intensive care unit: a case series. Journal of Critical Care 2011; 2:219.e1–e219.e6 [DOI] [PubMed] [Google Scholar]
- 8.Wiederhold MD, Wiederhold BK. Virtual reality and interactive simulation for pain distraction. Pain Medicine 2007; S3:S182–188 [Google Scholar]
- 9.Wiederhold BK, Davis R, Wiederhold MD. The effects of immersiveness on physiology. Virtual Environments in Clinical Psychology & Neuroscience 1998; 58:52–60 [PubMed] [Google Scholar]
- 10.Cacau Lde A, Oliveira GU, Maynard LG, et al. The use of virtual reality as intervention tool in the postoperative of cardiac surgery. Revista brasileira de cirurgia cardiovascular 2013; 28:281–289 [DOI] [PubMed] [Google Scholar]
- 11.Wiederhold BK, Wiederhold MD. Managing pain in military populations with virtual reality. NATO Science for Peace & Security Series—E: Human & Societal Dynamics 2012; 91:75–93 [Google Scholar]
- 12.Stetz MC, Brown KS, Folen RA, et al. Comparing distraction/relaxation modalities with chronic pain patients. NATO Science for Peace & Security Series—E: Human & Societal Dynamics 2012; 91:171–177 [Google Scholar]
- 13.Maani CV, Hoffman HG, Morrow M, et al. Virtual reality pain control during burn wound debridement of combat-related burn injuries using robot-like arm mounted VR goggles. The Journal of Trauma 2011; 71:S125–130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carrougher GJ, Hoffman HG, Nakamura D, et al. The effect of virtual reality on pain and range of motion in adults with burn injuries. Journal of Burn Care & Research 2009; 30:785–791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mosso JL, Gorini A, De La Cerda G, et al. Virtual reality on mobile phones to reduce anxiety in outpatient surgery. Studies in Health Technology & Informatics 2009; 142:195–200 [PubMed] [Google Scholar]
- 16.Nilsson S, Finnström B, Kokinsky E, et al. The use of virtual reality for needle-related procedural pain and distress in children and adolescents in a paediatric oncology unit. European Journal of Oncology Nursing 2009; 13:102–109 [DOI] [PubMed] [Google Scholar]
- 17.Vazquez JLM, Santander A, Gao K, et al. Using cybertherapy to reduce postoperative anxiety in cardiac recovery intensive care units. Journal of Anesthesia & Clinical Research 2013; 4:363 [Google Scholar]
- 18.Steele E, Grimmer K, Thomas B, et al. Virtual reality as a pediatric pain modulation technique: a case study. CyberPsychology &Behavior 2003; 6:633–638 [DOI] [PubMed] [Google Scholar]
- 19.Mosso JL, Rizzo S, Wiederhold B, et al. Cybertherapy—new applications for discomfort reductions. Surgical care unit of heart, neonatology care unit, transplant kidney care unit, delivery room-cesarean surgery and ambulatory surgery, 27 case reports. Studies in Health Information & Informatics 2007; 125:334–336 [PubMed] [Google Scholar]
- 20.Hoffman HG, Richards T, Coda B, et al. The illusion of presence in immersive virtual reality during an fMRI brain scan. CyberPsychology & Behavior 2003; 6:127–131 [DOI] [PubMed] [Google Scholar]