Abstract
Rift Valley fever (RVF) is a mosquito-borne zoonotic disease characterized by a high rate of abortion in ruminants, and febrile illness, hemorrhagic fever, retinitis and encephalitis in humans. RVF is caused by the RVF virus (RVFV), belonging to the genus Phlebovirus of the family Bunyaviridae. RVFV encodes a major virulence factor, NSs, which is dispensable for viral replication, yet required for evasion of host innate immune responses. RVFV NSs inhibits host gene upregulation at the transcriptional level, while promoting viral translation in the cytoplasm. In this article, we summarize the virology and pathology of RVF, and countermeasure development for RVF, with emphasis on NSs function and applications.
Keywords: MP-12, NSs, Phlebovirus, Rift Valley fever virus, vaccine
Rift Valley fever
Rift Valley fever (RVF) is mosquito-borne zoonotic disease affecting both ruminants and humans. RVF was first reported in a farm near Lake Naivasha in Kenya in 1930 [1], and has been endemic to sub-Saharan Africa for more than 80 years. RVF is caused by the RVF virus (RVFV), belonging to the genus Phlebovirus of the family Bunyaviridae [2]. In 1977, a large RVF outbreak occurred in Egypt – 20,000–200,000 humans were infected, and approximately 600 patients died of RVF [3]. Furthermore, RVFV crossed the border of Africa, and caused a large outbreak in Saudi Arabia and Yemen in 2000 [4,5]. RVFV is primarily maintained in floodwater Aedes mosquitoes, by which RVFV is transmitted transovarially, while many other mosquitoes (e.g., Culex spp.) serve as amplifying vectors of RVFV [6,7]. Ruminants, such as sheep, cattle or goats, can be infected via mosquito bite, and pregnant animals show a high rate of abortion and fetal malformation, while newborn animals can die of acute hepatitis [8–11]. Most adult ruminants show subclinical or temporal febrile illness, and viremic animals may further feed mosquitoes, which can result in the amplification of RVFV. Human infection with RVF may occur by mosquito bite or contact with the body fluid of infected animals. Most human RVF patients develop self-limiting febrile illness lasting up to 1–2 weeks. In the convalescent phase of disease, some patients develop retinitis or uveitis, which may lead to blindness, while some develop neurological disorders [12]. Thrombosis in the convalescent phase is also reported in a few cases [13,14]. Importantly, some patients develop a lethal hemorrhagic fever-like illness at the early stage of disease, and the death may occur 3–6 days after the onset of symptoms [12]. Potential introduction of RVFV into nonendemic countries outside Africa may cause large RVF outbreaks, and persistence of RVFV in the area for long periods, which may negatively affect the economy of the country [15,16]. Due to the potentially serious consequences of this pathogen, RVFV is classified as Category A Priority Pathogen by the NIH in the USA. Furthermore, to regulate the possession of pathogens related to the use for bioterrorism in the USA, RVFV is included as a select agent by the CDC and the US Department of Agriculture [17].
Development of countermeasures against RVFV is important to minimize the impact of RVF. For example, early detection of RVFV or diagnosis of RVF can minimize the time for the government to take an action to prevent further spread of RVFV. Although postmortem examination, including immunohistochemistry, is still useful to identify RVFV [18], rapid detection of viral RNA from viremic samples can be done by conventional or real-time RT-PCR, loop-mediated isothermal amplification (LAMP) [19] or recombinase polymerase amplification assay (RPA) [20,21]. Alternatively, antigen-capture (or sandwich) ELISA is useful to detect RVFV antigens in the situation where viral RNA cannot be stably preserved in the field [22,23]. Since the viremic period is very short, the use of wholeblood samples rather than sera could increase the sensitivity of RVFV RNA detection [24]. Identification of animals or humans with IgM specific to RVFV by IgM-capture ELISA is also important, since the recent infection status (i.e., within 1 month) indicates the history of RVFV spread in the area [25–27]. After the detection of RVFV or IgM specific to RVFV, rapid containment of RVFV is required. In addition to the cull of infected animals, vaccination may be the most effective way to prevent animals from further amplifying RVFV in the area. In endemic countries, a live-attenuated Smithburn vaccine has been used since 1950s, which is derived from the mouse brain-adapted Entebbe strain [28–30]. The use of Smithburn vaccine in pregnant animals is prohibited because of the risk of abortion [31], and the vaccine is approved for veterinary purposes only in endemic countries. In the USA, a live-attenuated MP-12 vaccine, which was developed from the Egyptian ZH548 strain by serial plaque purification in the presence of chemical mutagen 5-fluorouracil, has been manufactured at the Salk Institute [32,33]. The MP-12 vaccine has been approved as a conditional (emergency) vaccine for veterinary use for a 2-year term. The MP-12 vaccine has also been tested in humans in a Phase II clinical trial, and no significant adverse effects have been reported [34]. Although MP-12 is highly efficacious and sufficiently safe, a lack of marker to differentiate infected from vaccinated animals (DIVA) might compromise the monitoring of animals upon the introduction of RVFV. In addition, a live-attenuated vaccine may not be the best choice for humans in terms of safety. In the USA, a highly safe formalin-inactivated vaccine for RVF is available (TSI-GSD-200). However, the dose is limited, and TSI-GSD-200 is less immunogenic compared with MP-12 [35–37]. An ideal vaccine for RVF might be the one that encompasses high efficacy, which rapidly induces protective immunity in both ruminants and humans; perfect safety, in particular, for humans; a DIVA marker for veterinary purposes; low-cost manufacturing; and no transmission in mosquito vectors. Although RVFV is still largely contained in Africa, the development of a better vaccine for RVF is an important task for the USA and other countries.
RVFV & its lifecycle in infected cells
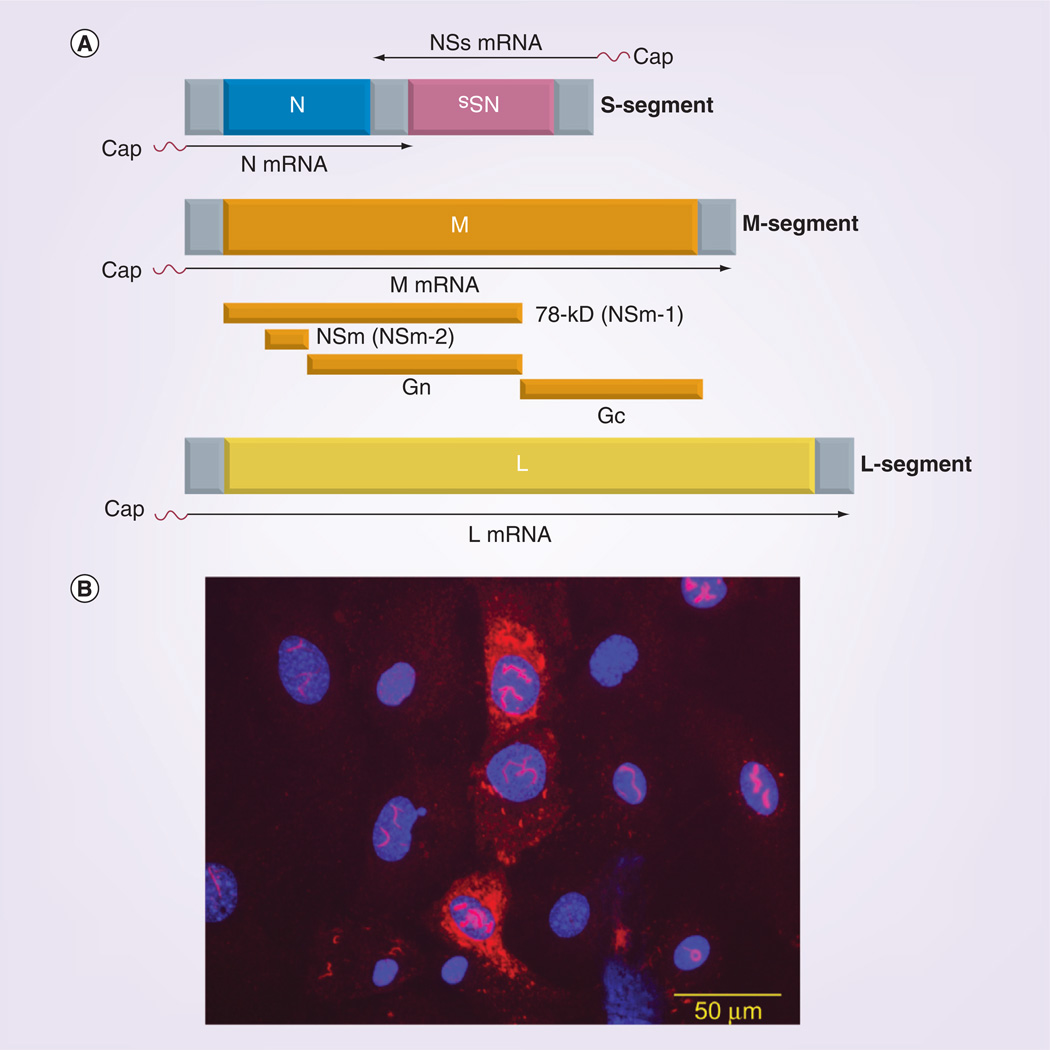
RVFV has a tripartite negative-stranded RNA genome, named small (S), medium (M) and large (L) segment (Figure 1A). As with other phleboviruses, the S-segment (1690 nt) encodes the nucleocapsid (N) gene in the negative-sense (viral-sense) genome, and the nonstructural (NSs) gene in the positive-sense (antiviral-sense) genome in an ambisense manner. The N protein encapsidates viral genomic RNA, and is required for viral RNA synthesis and packaging of viral RNA into virions [38–40]. The NSs protein is a major virulence factor for RVFV [41–43], although it is dispensable for viral replication [44,45]. The M-segment (3885 nt) encodes a single open reading frame (ORF), while the M mRNA can make at least four different proteins (i.e., 78-kD, NSm, Gn and Gc) by leaky scanning of five different initiation codons as well as cotranslational cleavage of polypeptides [46–49]. The Gn and Gc are viral envelope proteins and form heterodimers on the surface of virion to form capsomers [50–54]. It is considered that the Gn plays a role in receptor binding, and the Gc serves as a class II fusion protein. The NSm protein (also described as NSm2) is dispensable for RVFV replication [55,56], localizes to the outer membrane of mitochondria [57], and delays the progress of apoptosis in infected cells [58]. The 78-kD protein (also described as NSm1) is less characterized, yet incorporation into the virion has been suggested [59]. The L-segment (6404 nt) encodes a single ORF for the RNA-dependent RNA polymerase (L protein) [60]. The L protein plays a role in genome RNA replication and viral mRNA transcription. L proteins snatch host mRNA to use it as a primer for transcription (cap snatching), and thus viral mRNAs contain heterogeneous sequences at the 5´-ends. The N-terminus of the L protein encodes a NL1 domain conserved between bunyaviruses and arenaviruses, which may serve as an endonuclease to cleave off host mRNA for the cap-snatching process [61,62]. Viral attachment occurs between Gn/Gc and DC-SIGN [63,64]. Alternatively, the virus can bind to heparansulfate for entry [65]. Upon attachment to a viral receptor, RVFV enters cells by dynamin-dependent caveolae-mediated endocytosis [66]. Like other phleboviruses, RVFV may also cause membrane fusion to cells in the late endosome via exposure of the Gc fusion loop [50,64]. Since the viral L protein is attached to the viral ribonucleocapsid (RNP; viral genomic RNA encapsidated with N proteins) [67] in virions, the incoming genomic RNA immediately becomes a template for mRNA synthesis [68]. Theoretically, N mRNA, M mRNA and L mRNA can be transcribed from the negative-stranded S-, M- and L-segments, respectively (primary transcription), and NSs mRNA can be transcribed from the positive-stranded S-segment only after viral genome RNA replication. However, NSs mRNA was also found to be transcribed at the primary transcription stage [68]. It was found that both negative-sense and positive-sense S-, M- and L-segments are packaged into virions, which allows a head-start synthesis of NSs mRNA in infected cells [68]. Subsequently, viral RNA genome replication occurs, and further accumulation of viral mRNA also occurs (secondary transcription). Then, the viral assembly process starts at the Golgi region. The Gn encodes a Golgi retention signal at the transmembrane domain and the cytoplasmic domain, while the Gc encodes an ER retention signal [69]. The coexpression of Gn and Gc allows the accumulation of Gn/Gc at the Golgi region [69]. Since there are no matrix proteins, the cytoplasmic domains of Gn/Gc are considered to be the viral components that interact with the RNP, although there has been little research regarding this so far. Gn and Gc encode one (N438) and four N-glycosylation sites (N794, N829, N1035 and N1077), respectively [47], which may play a role in the maturation of viral virions, as well as attachment to the DC-SIGN receptor in next infection cycle.
Figure 1. Rift Valley fever virus genome structure and the NSs protein.
(A) Rift Valley fever virus (RVFV) genome structure. RVFV has tripartite negative-stranded RNA genome named the S-, Mand L-segments. The S-segment encodes N and NSs mRNA in an ambisense manner. The M-and L-segments encode M and L mRNA, respectively. M mRNA will be translated into at least four different proteins – 78-kD, NSm, Gn and Gc by leaky scanning of several in-frame initiation codons, as well as cotranslational cleavage of translated polypeptides. The 5´-end terminus of each mRNA is derived from host mRNA. (B) The NSs protein. Mouse embryonic fibroblast cells lacking PKR were transfected with in vitro-synthesized RNA encoding MP-12 NSs. RVFV NSs accumulates in the nucleus and cytoplasm, while nuclear NSs forms a filament structure.
Please see color figure online at www.futuremedicine.com/doi/pdf/10.2217/fvl.13.11.
Evasion of host innate immune responses by RVFV
RVFV causes unique pathology in different animal species [8–10,12,70]. The susceptibility of host species is as follows: mouse/hamster/lamb > rat/sheep > human/monkey/cow/goat, while no symptomatic disease can occur in rabbits, pigs, horses, guinea pigs or birds [70]. The mouse is one of the most susceptible animal species to RVFV and dies in 7–10 days postinfection by either fulminant hepatitis or viral spread in the CNS [71]. Upon entry of RVFV into a mouse, dendritic cells, macrophages and granulocytes may be the primary target cells [72,73]. In BALB/c mice infected with the RVFV ZH501 strain (1000 PFU subcutaneously), the virus can spread systematically by 3–4 days postinfection (dpi; e.g., liver, spleen, kidney, heart and adrenal gland), while viral antigens can be efficiently cleared in those tissues by 6–7 dpi [71]. At the same time, RVFV spreads throughout the CNS around 6–7 dpi, which leads to the death of mice [71,74]. To control the virulence of RVF, it is important to know how the clearance of RVFV can occur. It was reported that passive transfer of neutralizing antibodies (1:10) was sufficient to protect hamsters from virulent RVFV challenge [75]. This result indicates that neutralizing antibodies are sufficient to protect the host from the progression of disease. Viral evasion in the host occurs by the NSs protein, since RVFV lacking NSs induces abundant type-I interferon (IFN) in mice and cannot establish viremia [41]. On the other hand, mice lacking IFNAR succumb to the infection with RVFV lacking NSs [41], indicating that host innate immunity plays an important role in preventing RVFV replication, while viral replication can induce the death of mice even without NSs if the host does not have a competent innate immune system. Using C57BL/6 mouse models, the requirement for mice to be protected from disease due to RVFV lacking NSs (RVFVΔNSs) was studied [76]. Although B-cell-deficient mice were largely resistant to infection with RVFVΔNSs, such mice were all dead after challenge with wild-type RVFV [76]. On the other hand, mice with depleted CD4+ T cells, but not with depleted CD8+ T cells, succumbed to lethal encephalitis caused by the infection [76]. Therefore, CD4+ T cells (and maybe neutralizing antibodies) but not CD8+ T cells should play an important role in viral clearance and prevention of the progression of disease in this model. This result is also consistent with the finding that mice with neutralizing antibodies can be always protected from wild-type RVFV challenge [73,77,78]. Other studies indicate that cellular immune responses toward N protein can also alter the pathology of the diseases [79]. Currently, it remains unknown how viral clearance occurs by immune cells in the liver or other organs.
Multiple functions of RVFV NSs
As described above, RVFV NSs plays a role in evasion from host innate immunity. NSs protein (265 amino acids) forms a unique filamentous structure in the nucleus, although it also accumulates in the cytoplasm (Figure 1B) [80]. The 17 C-terminal amino acids are required for the formation of the NSs filament [80]. There is no typical nuclear localization signal in NSs, while there are four proline-rich motifs (PXXP motif 1–4) [81] and two phosphorylation sites by casein kinase II at Ser 252 and Ser 256 [82]. Mutations of the PXXP motif 1 and 2, but not 3 and 4, could largely abolish the accumulation and filament formation of NSs in the nucleus, while mutations of Ser 252 or 256 did not affect filament formation [81]. NSs is responsible for the suppression of IFN-β gene expression, and the intact PXXP motif 1 and 2 appears to be important for NSs function [81]. Inhibition of the IFN-β gene occurs at the transcription level: that is, the inhibition of IFN-β mRNA synthesis occurs in the presence of the activation of three important transcription factors for IFN-β promoter activation – IRF-3, NF-κB and AP-1 in infected cells [81]. Subsequently, it was found that RVFV NSs could bind to and sequester the subunit protein p44 of TFIIH, which is an essential transcription factor for host RNA polymerase I and II, and inhibits general host transcription [83]. RVFV NSs also binds to SAP30, and it has been proposed that the recruitment of CBP/p300 is interrupted when the NSs filament is bound to the IFN-β gene promoter via SAP30 [84]. It is still unclear how the two distinct mechanisms affect IFN-β promoter suppression, since there are no available mutants lacking either function.
RVFV NSs also promotes the post-translational degradation of dsRNA-dependent PKR [43,85]. The degradation of PKR does not require the replication of RVFV, and PKR could be stabilized in the presence of the proteasome inhibitor MG132 [43,85]. A point mutation at R173 into alanine could abolish this PKR degradation function due to a lack of specific interactions with PKR [86]. Interestingly, this mutant NSs could form filament structures with a mosaic-like pattern in the nucleus, which is distinct from the intact NSs filament, and allows early accumulation of eIF2α phosphorylation in infected cells, which dramatically decreases the accumulation of viral proteins [86]. Those findings indicate that RVFV regulates host transcription suppression and PKR degradation independently. Although the mechanism of early accumulation of phosphorylated eIF2α remains unclear, a similar phenomenon was also observed in cells infected with RVFV lacking NSs in the presence of transcription inhibitor, actinomycin D [85]. Thus, it is proposed that NSs-mediated PKR degradation plays an important role in active viral translation in the presence of host transcription suppression induced by NSs itself.
TFIIH consists of ten subunit proteins: XPD (a gene defective in xeroderma pigmentosum patient complementation group D), p8, p34, p44, p52, p62, XPB (a gene defective in xeroderma pigmentosum patient complementation group B), MAT1, cyclin H and cdk7. RVFV also promotes the post-translational degradation of TFIIH p62 subunit protein [87]. Similarly to PKR degradation by NSs, the NSs can bind to p62, and p62 was stabilized in the presence of MG132. On the other hand, the degradation of p62 occurs even in the presence of leptomycin B (nuclear export inhibitor), indicating that degradation occurs inside the nucleus [87]. Thus, there are at least two distinct substrates for RVFV NSs-mediated degradation: PKR and TFIIH p62. Currently, there is no evidence of increased polyubiquitination of these proteins in the presence of NSs. It is also unclear whether the sequestration of p44 and the degradation of p62 are redundant functions to inhibit host transcription, or whether they are just a snapshot of more dynamic NSs functions that inhibit host transcription machinery.
RVFV NSs also affects cell cycle progression. Cells usually undergo interphase – G1 phase (growth), S phase (DNA replication), G2 phase (growth) and M phase (preparation for mitosis) – before mitosis. Chromosomal segregation is driven by the centromere, which binds to the mitotic spindles [88]. RVFV NSs filaments physically exclude chromatin DNA and interact with the γ-satellite sequence (pericentromere; a region flanking the centromere), but not with the α-satellite sequence (centromere) [89]. Cells infected with RVFV exhibit nuclear abnormality and a reduced rate of mitosis, which are most likely the results of chromosome cohesion and segregation defect [89]. RVFV NSs also activates the classical DNA damage signaling pathway via ATM (phosphorylation of p53 [Ser 1]), Chk.2 [Thr 68] and H2A.X [Ser 139]) and induces cell cycle arrest at the S phase (MP-12 strain) or the G0/G1 phase (ZH548 strain) [90]. Another study also showed that RVFV NSs can induce the phosphorylation of p53 at Ser 9, 15, 20, 37, 46 and 392 in cells infected with RVFV, and a lack of p53 reduction could result in reduced viral replication and a subsequent decrease in cell death [91].
Subsequently, genome-wide identification of cellular DNA bound to RVFV NSs was performed by chromatin immunoprecipitation (IP) combined with a promoter array chip. Among the 33 NSs-interacting genes, the expression of ten genes (Mapk8ip3, Fbxo3, Stat2, Il3, Il10rb, Tyk2, Casp9, Phf21, Ncoa3 and Notch4) at 8 hpi was significantly downregulated in RVFV-infected cells [92]. Those genes are involved with protein phosphorylation, ubiquitination, immune responses, apoptosis, transcription or development. In addition, the upregulation (FX, FII, FVIII, Tfpi) or downregulation (FIII) of coagulation factors occurs in cells infected with RVFV, indicating the potential involvement of NSs with coagulation disorders during hemorrhagic fever [92]. These results also indicate that RVFV NSs selectively inhibits host genes.
RVFV accumulates a lower level of NSs proteins in C6/36 cells derived from Aedes albopictus or LL-5 cells derived from Lutzomyia longipalpis (sandfly) than that in mammalian cells [93]. A recent study showed that U4.4 cells (Aedes aegypti) barely allow the expression of NSs filament formation, and Aag2 cells (Aedes aegypti) allow NSs filament formation only at the early stage of infection (~24 hpi), whereas C6/36 cells (A. albopictus) can express NSs filaments for a longer period [94]. In mosquito cells infected with RVFV, the RNAi silencing pathway can potentially inhibit the replication of RVFV. Namely, RNA secondary structures or viral replicative intermediates become the template to form a small virus-derived RNA duplex (viRNA) by Dicer-2, which allows sequence-specific degradation of target mRNA via RISC [94]. The viRNAs specific to S (mostly antiviral-sense), M (both viral and antiviral-sense) and L (both viral and antiviral-sense) appears as 21–28 nt in size, while the signature for Piwi-interacting RNA (piRNA; 5´-terminal uridine and an adenosine at position 10) is clearly visible for large viRNA such as 27–28 nt in size [94]. Although C6/36 cells are known to be Dicer-2 deficient, the presence of viRNA with a piRNA signature indicates that there is also an antiviral mechanism in C6/36 cells [94]. The attenuated expression of the NSs gene in mosquitoes may contribute to the persistent infection of RVFV.
Significance of RVFV NSs in live-attenuated vaccine development
The first RVFV strain lacking NSs (Clone 13) was isolated from the RVFV 74HB59 strain (in the Central African Republic), and the NSs encodes an in-frame 69% truncation, which results in the abolishment of all known NSs functions [44]. The Clone 13 strain has been extensively used as a control virus to evaluate the functions of NSs. Clone 13 is completely attenuated in mice, and its safety and efficacy has been demonstrated in sheep and cattle [41,95,96]. Due to a lack of functional NSs, infected animals can mount innate immune responses, including IFN-α/β, and no viremia can be detected in immunocompetent animals. On the other hand, Clone 13 can cause lethal disease in IFNAR−/− mice or PKR knockout mice [41,43], indicating that the limiting factor is the competent host innate immune system. The reassortment of Clone 13 with the ZH548 S-segment; that is, reassortant consisting of ZH548 S and Clone 13 M and L, resulted in a virulent RVFV strain [41]. On the other hand, the reassortant consisting of Clone 13 S and ZH548 13 M and L was completely attenuated [41]. A reassortant virus encoding the Clone 13 S-segment and MP-12 M- and L-segments is also under development as the R566 strain [97], which might decrease the risk of the potential creation of virulent reassortant RVFV.
The recent development of reverse genetics for RVFV allowed the creation of recombinant RVFV lacking NSs [42,45,56,98]. The recombinant ZH501 strain lacking both NSs and NSm (rZH501ΔNSsΔNSm) has been tested in pregnant ewes and has been demonstrated to be efficacious and safe for veterinary vaccine use [99,100]. Vaccination with rZH501ΔNSsΔNSm does not cause detectable viremia, does not induce abortion or fetal malformation in pregnant ewes, and protects ewes from wild-type RVFV challenge [100]. The NSm truncation partly attenuates the ZH501 M-segment [101], and, thus, the risk of reversion to virulence upon reassortment with wild-type RVFV may be reduced compared with the single deletion of the NSs gene. Another study also indicated that RVFV lacking NSm, but not that lacking NSs, is less efficient in mosquito transmission [102]. Thus, this may be an advantage for use in the field. Due to demonstrated safety, rZH501ΔNSsΔNSm is excluded from the select agent rule, and can be handled at biosafety level (BSL) 2 in the USA upon approval by each institutional biosafety committee. The absence of anti-NSs antibodies in vaccinated animals is useful for DIVA [100,103], although not all animals naturally infected with RVFV raise against NSs sufficiently [104]. On the other hand, the sensitive detection of anti-NSm antibody in ruminant sera infected with RVFV appears to be more difficult than that of anti-NSs [100,105].
A live-attenuated MP-12 vaccine is highly attenuated in both animals and humans, and it is considered as a conditional vaccine for veterinary use in the USA, as well as a potential vaccine candidate for human use [34]. MP-12 is also excluded from the select agent rule, and handling can be done at BSL2 level in the USA. MP-12 is derived from the wild-type RVFV ZH548 strain, and encodes 23 mutations in the genome (four in the S-segment, nine in the M-segment and ten in the L-segment) [33]. The attenuation largely occurs by the M- and/or L-segment, but not in the S-segment [42], while the attenuation mutation(s) are still not identified among them. Importantly, the NSs of MP-12 is still fully functional, and the recombinant ZH548 strain encoding MP-12 NSs has a virulent phenotype [42]. Since the NSs is a major virulence factor for RVFV [41], the deletion of the NSs gene from the vaccine can greatly improve the safety profile of the vaccine. On the other hand, the reduction in efficacy due to a lack of NSs may also need to be considered. Therefore, a recombinant MP-12 lacking a functional NSs (rMP12-C13type) was generated by a reverse genetics system [45], and efficacy was compared with parental MP-12 in a mouse model. MP-12 vaccination induced viremia in 30% of vaccinated mice without detectable induction of IFN-α, and 72% of vaccinated mice were protected from wild-type RVFV challenge at 44 days postvaccination [73]. On the other hand, the rMP12-C13type failed to develop detectable viremia, induced detectable IFN-α (~100 pg/ml) in sera at day 1, and 80% of vaccinated mice were protected from the wild-type RVFV challenge [73]. The mean neutralizing antibody titers of mice vaccinated with MP-12 or rMP12-C13type (1 × 105 PFU subcutaneously, one dose) are 1:641 or 1:549 on day 30, 1:2,987 or 1:1,056 on day 90, and 1:1,067 or 1:216 on day 180, respectively. Thus, some reduction of neutralizing antibody titer might occur due to a lack of the NSs gene in the MP-12 vaccine. On the other hand, rMP12-C13type is attenuated in the S-, M- and L-segment, and encodes a DIVA marker for agricultural use [106]. To further develop rMP12-C13type as a vaccine, a dose–response analysis should be carried out in ruminants.
Another strategy to make the MP-12 vaccine capable of DIVA is to replace the NSs gene with functional NSs derived from other phlebovirus species. Using this approach, MP-12 may still escape host innate immune responses, while being more attenuated than original MP-12. Phlebovirus genera consist of approximately 70 named viruses, which are largely divided into three major phylogenetic groups: the mosquito/sandfly-borne phlebovirus group, the Uukuniemi group, and the severe fever with thrombocytopenia syndrome virus (SFTSV)/Heartland/Bhanja group [107,108]. The mosquito/sandf ly-borne phlebovirus consists of Naples serocomplex (e.g., Toscana virus [TOSV]), Sicilian serocomplex (e.g., Sandfly fever Sicilian virus [SFSV]), Punta Toro serocomplex (e.g., Punta Toro virus Adames strain [PTV]), RVF serocomplex, Icoaraci serocomplex (e.g., Icoaraci virus) and Frijoles serocomplex (e.g., Frijoles virus) [109]. Recombinant MP-12 encoding the NSs of TOSV (rMP12-TOSNSs), SFSV (rMP12-SFSNSs) or PTV (rMP12-PTNSs), which are phylogenetically close to RVFV NSs, were generated by reverse genetics, and efficacy in mice was tested. Surprisingly, the rMP12-TOSNSs induced viral encephalitis in up to 30% of vaccinated mice [77]. Since parental MP-12 infrequently induces viral encephalitis in mice, the high rate of neuroinvasion might be caused by a unique TOSV NSs function. All mice vaccinated with rMP12-TOSNSs could be protected from wild-type RVFV challenge. On the other hand, the efficacy of rMP12-PTNSs or rMP12-SFSNSs was 78 or 89%, respectively [78]. Thus, these chimeric MP-12s showed similar or better efficacy in the mouse model than MP-12. To further understand the phenomenon, the NSs functions of TOSV, SFSV and PTV were analyzed. TOSV NSs does not induce host general transcription suppression [110], but inhibits the IFN-β gene [77,111], and promotes the degradation of PKR [110]. PTV NSs induces host general transcription suppression and inhibits the IFN-β gene, but no degradation of PKR is induced [78,112]. SFSV NSs induces neither host general transcription suppression nor PKR degradation, but inhibits the IFN-β gene [43,78]. It is of note that TOSV NSs retains similar functions with RVFV NSs, except for host general transcription suppression. If infected cells play a role in the neuroinvasion of the virus, rMP12-TOSNSs-infected cells might trigger neuroinvasion at the blood–brain barrier by active host gene expression. On the other hand, SFSV or PTV NSs appear to be more suitable for vaccine development than TOSV NSs. The attenuation levels of SFSV or PTV NSs compared with RVFV NSs should be further evaluated in a virulent RVFV background to understand the risk of reversion to virulence of those chimeric viruses. Furthermore, the efficacy of these vaccine candidates in ruminants should be determined in the future. Although we only described live-attenuated vaccines, the status of other type of vaccines may be found elsewhere [34,113–116].
RVFV NSs & therapeutics for RVF
Upon exposure to wild-type RVFV, either effective antiviral or postexposure vaccination might be required to improve the prognosis of RVF. Ribavirin (1-β-d-ribofuranosyl-1,2,4-triazole-3-carboxamide) was found to be effective to RVF alone or combination with poly-l-lysine and carboxymethylcellulose (poly[ICLC]) [117,118] with or without the liposome-encapsulated form in mice or rhesus monkeys [119]. In the USA, ribavirin is approved for the treatment of hepatitis C (oral ribavirin) [120] and respiratory syncytial virus (ribavirin with aerosol form) [121], whereas the adverse effects such as hemolytic anemia or teratogenicity hamper the development of ribavirin for intravenous use to treat many viral diseases [122]. Currently, there are no approved therapeutics for RVFV infection. RVFV MP-12 and rMP12-C13type were evaluated for potential post-exposure vaccine candidates in a mouse model. When mice were exposed to wild-type RVFV, subcutaneous administration of 1 × 105 PFU of rMP12-C13type, but not MP-12, significantly attenuated the replication of wild-type RVFV in the liver and spleen, and improved the survival of the mice, although administration should be carried out within 20–30 min postexposure [123]. If a lack of NSs is important for protection, the postexposure vaccination regimen may be further improved by the stimulating host’s innate immune response.
On the other hand, coexpression of a nonfunctional NSs in RVFV-infected cells might inhibit the functions of an intact NSs. To test this, 293 cells were infected with MP-12 (functional NSs gene is encoded) and separately transfected with 11 different in vitro-synthesized RNA encoding a partially truncated NSs (lacking all known NSs functions). Although the truncated NSs could be coexpressed abundantly, the intact MP-12 NSs could still inhibit the host IFN-β gene and promote the degradation of PKR [124]. Although NSs can self-assemble via the C-terminus and form filament structures (Figure 1B), coexpression of truncated NSs does not allow the dominantnegative suppression of NSs, potentially due to the change of NSs structure required for correct protein localization. Thus, other approaches will be required to target NSs functions to attenuate RVFV replication.
It was found that RVFV NSs could be phosphorylated by a unique form of IKK-β, called IKK-β2, which forms in cells infected with RVFV [125]. IKK-β2 can form a complex (IKK complex) with IKK-α and IKK-γ, and phosphorylate IkBα, which leads to the degradation of IkBα and nuclear translocation of p65. The phosphorylated NSs can bind to mSin3A better than nonphosphorylated NSs [125]. Curcumin, which is known as the major active component of turmeric, can inhibit both conventional IKK-β and IKK-β2 complexes [125]. Cells treated with curcumin fail to arrest the cell cycle at the S phase upon MP-12 infection and reduce RVFV replication, indicating attenuation of NSs function by curcumin [125]. Furthermore, IFNAR−/− mice that were pretreated with curcumin (sc.) showed 60% survival upon MP-12 infection and up to a 90% decrease in the virus titer in the liver [125]. Thus, the attenuation of NSs effector functions may be an important concept to develop therapeutics for RVF.
Conclusion
RVFV NSs has multiple functions to allow the virus to replicate efficiently by shutting down host antiviral responses. Live-attenuated vaccine candidates with the deletion of NSs are highly attenuated in the S-segment, and a lack of the NSs gene may be useful for DIVA, while the RVFV MP-12 strain encoding other phlebovirus species exerts NSs functions partly similar to those of RVFV NSs, and can be applicable to DIVA. Furthermore, MP-12 lacking NSs is efficacious in a postexposure vaccination regimen, and further optimization can be expected. Finally, inhibition of the NSs function is an effective approach to improve the prognosis of RVFV-infected animals.
Future perspective
Since 1930s, sporadic RVF outbreaks have been a concern for public health and agriculture in Africa. During the past 80 years, scientific techniques in multidisciplinary fields have been greatly advanced, and the best approaches, to date, to detect and prevent this disease have also changed. On the other hand, RVFV continues to spread throughout Africa, and has even invaded the Arabian Peninsula. A recent study indicates that the live-attenuated Smithburn vaccine potentially reassorted with wild-type RVFV during a RVF outbreak [30]. Thus, a future live-attenuated RVF vaccine should have reduced environmental risks; complete attenuation of all the S-, M- and L-segments, or modifications of the virus to be incapable of mosquito-mediated transmission. The S-segment can be largely attenuated by the deletion or replacement of the NSs gene with little concern of reversion to virulence. This is an advantage for phleboviruses, which encode the NSs gene separately from N gene by an ambisense coding strategy. On the other hand, attenuation of the M- and L-segments is not very easy. MP-12 is attenuated by the M- and L-segments, although attenuation of the M- or L-segment is not complete by itself [Ikegami T, Freiberg AN, Unpublished Data]. Further studies to establish nonreversible attenuation for bunyaviruses will support the improvement of RVF vaccine safety. On the other hand, the development of treatment regimens for RVF patients should also be established. The approaches to inhibit the functions of RVFV NSs will be further developed in the near future.
Executive summary
Rift Valley fever
Rift Valley fever (RVF) is a mosquito-borne zoonotic disease affecting Africa and the Arabian Peninsula.
High rates of abortion in ruminants and human diseases are public health concerns.
Effective vaccines or therapeutics for animal and human for RVF are required.
RVF virus & its lifecycle in infected cells
RVF virus (RVFV; family Bunyaviridae, genus Phlebovirus) has a negative-stranded RNA genome with an S-, M- and L-segment.
RVFV attaches to DC-SIGN for entry via caveola-mediated endocytosis, transcribes viral mRNA by cap-snatching, replicates viral genomic RNA, and assembles viral genomic RNA encapsidated with nucleocapside (N) into Gn/Gc at Golgi.
RVFV encodes two nonstructural proteins: NSs and NSm.
Evasion of host innate immune responses by RVFV
RVFV lacking NSs does not cause disease in mice.
CD4+ T cells and B cells play key roles in host immune responses against RVFV.
Multiple functions of RVFV NSs
RVFV NSs sequesters TFIIH p44, while promoting the degradation of TFIIH p62 and PKR.
RVFV interacts with chromatin DNA, induces cell cycle arrest and affects various host gene expressions, including the IFN-β gene.
RVFV NSs accumulation is restricted in mosquito cells by the RNAi mechanism.
Significance of RVFV NSs in live-attenuated vaccine development
RVFV lacking NSs (e.g., Clone 13, R566, rZH501ΔNSsΔNSm and rMP12-C13type) is highly attenuated in animals and may be useful to differentiate infected from vaccinated animals.
Replacement of MP-12 NSs with that of other phleboviruses does not decrease the efficacy of MP-12.
RVFV NSs & therapeutics for RVF
MP-12 lacking NSs, but not parental MP-12, is efficacious as a postexposure vaccine.
Coexpression of a nonfunctional NSs does not exhibit a dominant-negative phenotype.
Curcumin inhibits the phosphorylation of NSs, and may attenuate NSs functions.
Future perspective
A live-attenuated vaccine for RVF with complete nonreversible attenuation in S-, M-and L-segments will solve the safety concerns of vaccination use in the environment.
Postexposure vaccination regimens can be further optimized.
RVFV therapeutics may be developed by the inhibition of NSs functions.
Acknowledgements
The authors thank Inaia Phoenix (UTMB) for proofreading this manuscript. The authors would like to thank BRG Williams (Monash University, Australia) for the MEF PKR0/0 cells used for the figure in this manuscript.
This review is supported by NIH grant R01 AI08764301, and by the Sealy Center for Vaccine Development at UTMB.
Footnotes
Financial & competing interests disclosure
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
• of interest
•• of considerable interest
- 1.Daubney R, Hudson JR. Enzootic hepatitis or Rift Valley fever: an undescribed virus disease of sheep, cattle and man from east Africa. J. Path. Bact. 1931;34:545–579. [Google Scholar]
- 2.Schmaljohn C, Nichol ST. In: Bunyaviridae. Fields Virology. Knipe DM, Howley PM, Griffin DE, Lamb RA, Martin MA, Roizman B, Straus SE, editors. Lippincott, Williams & Wilkins, PA, USA; 2007. pp. 1741–1789. [Google Scholar]
- 3.Meegan JM. The Rift Valley fever epizootic in Egypt 1977–78. 1. Description of the epizzotic and virological studies. Trans. R Soc. Trop. Med. Hyg. 1979;73(6):618–623. doi: 10.1016/0035-9203(79)90004-x. [DOI] [PubMed] [Google Scholar]
- 4.Shoemaker T, Boulianne C, Vincent MJ, et al. Genetic analysis of viruses associated with emergence of Rift Valley fever in Saudi Arabia and Yemen, 2000–01. Emerg. Infect. Dis. 2002;8(12):1415–1420. doi: 10.3201/eid0812.020195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balkhy HH, Memish ZA. Rift Valley fever: an uninvited zoonosis in the Arabian peninsula. Int. J. Antimicrob. Agents. 2003;21(2):153–157. doi: 10.1016/s0924-8579(02)00295-9. [DOI] [PubMed] [Google Scholar]
- 6.Pepin M, Bouloy M, Bird BH, Kemp A, Paweska J. Rift Valley fever virus (Bunyaviridae: Phlebovirus): an update on pathogenesis, molecular epidemiology, vectors, diagnostics and prevention. Vet. Res. 2010;41(6):61. doi: 10.1051/vetres/2010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Linthicum KJ, Davies FG, Kairo A, Bailey CL. Rift Valley fever virus (family Bunyaviridae, genus Phlebovirus). Isolations from Diptera collected during an inter-epizootic period in Kenya. J. Hyg. (Lond.) 1985;95(1):197–209. doi: 10.1017/s0022172400062434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Swanepoel R, Coetzer JAW. Rift Valley fever. In: Coetzer JAW, Tustin RC, editors. Infectious Diseases of Livestock with Special Reference to Southern Africa (2nd Edition) South Africa: Oxford University Press; 2004. pp. 1037–1070. • Provides historical reviews of Rift Valley fever (RVF) in endemic countries.
- 9.Weiss KE. Rift Valley fever – a review. Bull. Epz. Dis. Afr. 1957;5:431–458. [Google Scholar]
- 10.Easterday BC. Rift Valley fever. Adv Vet Sci. 1965;10:65–127. [PubMed] [Google Scholar]
- 11.Bird BH, Ksiazek TG, Nichol ST, Maclachlan NJ. Rift Valley fever virus. J. Am. Vet. Med. Assoc. 2009;234(7):883–893. doi: 10.2460/javma.234.7.883. [DOI] [PubMed] [Google Scholar]
- 12.Ikegami T, Makino S. The pathogenesis of Rift Valley fever. Viruses. 2011;3(5):493–519. doi: 10.3390/v3050493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwentker FF, Rivers TM. Rift Valley fever in man: report of a fatal laboratory infection complicated by thrombophlebitis. J. Exp. Med. 1934;59(3):305–313. doi: 10.1084/jem.59.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mundel B, Gear J. Rift Valley fever; I. The occurrence of human cases in Johannesburg. S. Afr. Med. J. 1951;25(44):797–800. [PubMed] [Google Scholar]
- 15.Sindato C, Karimuribo E, Mboera EG. The epidemiology and socio-economic impact of Rift Valley fever epidemics in Tanzania: a review. Onderstepoort J. Vet. Res. 2012;79(2):e1. doi: 10.4314/thrb.v13i5.1. [DOI] [PubMed] [Google Scholar]
- 16.Hartley DM, Rinderknecht JL, Nipp TL, Clarke NP, Snowder GD. Potential effects of Rift Valley fever in the United States. Emerg. Infect. Dis. 2011;17(8):e1. doi: 10.3201/eid1708.101088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Department of Agriculture. Part II. 7 CFR Part 331 and 9 CFR Part 121. Agricultural Bioterrorism Protection Act of 2002. Possession, use transfer of biological agents and toxins; final rule. Fed. Register. 2005;70:13241–13292. [Google Scholar]
- 18.Shieh WJ, Paddock CD, Lederman E. Pathologic studies on suspect animal and human cases of Rift Valley fever from an outbreak in eastern Africa 2006–2007. Am. J Trop. Med. Hyg. 2010;83(2 Suppl):38–42. doi: 10.4269/ajtmh.2010.09-0463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ikegami T. Molecular biology and genetic diversity of Rift Valley fever virus. Antiviral Res. 2012;95(3):293–310. doi: 10.1016/j.antiviral.2012.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Euler M, Wang Y, Heidenreich D. Development of a panel of recombinase polymerase amplification assays for detection of biothreat agents. J. Clin. Microbiol. 2013;51(4):1110–1117. doi: 10.1128/JCM.02704-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Euler M, Wang Y, Nentwich O, Piepenburg O, Hufert FT, Weidmann M. Recombinase polymerase amplification assay for rapid detection of Rift Valley fever virus. J. Clin. Virol. 2012;54(4):308–312. doi: 10.1016/j.jcv.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 22.Jansen van Vuren P, Paweska JT. Laboratory safe detection of nucleocapsid protein of Rift Valley fever virus in human and animal specimens by a sandwich ELISA. J. Virol. Methods. 2009;157(1):15–24. doi: 10.1016/j.jviromet.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 23.Fukushi S, Nakauchi M, Mizutani T, Saijo M, Kurane I, Morikawa S. Antigen-capture ELISA for the detection of Rift Valley fever virus nucleoprotein using new monoclonal antibodies. J. Virol. Methods. 2012;180:68–74. doi: 10.1016/j.jviromet.2011.12.013. [DOI] [PubMed] [Google Scholar]
- 24.Grolla A, Mehedi M, Lindsay R, Bosio C, Duse A, Feldmann H. Enhanced detection of Rift Valley fever virus using molecular assays on whole blood samples. J. Clin. Virol. 2012;54(4):313–317. doi: 10.1016/j.jcv.2012.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sall AA, Macondo EA, Sene OK. Use of reverse transcriptase PCR in early diagnosis of Rift Valley fever. Clin. Diagn. Lab. Immunol. 2002;9(3):713–715. doi: 10.1128/CDLI.9.3.713-715.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paweska JT, Burt FJ, Anthony F. IgG-sandwich and IgM-capture enzyme-linked immunosorbent assay for the detection of antibody to Rift Valley fever virus in domestic ruminants. J. Virol. Methods. 2003;113(2):103–112. doi: 10.1016/s0166-0934(03)00228-3. [DOI] [PubMed] [Google Scholar]
- 27.Paweska JT, Burt FJ, Swanepoel R. Validation of IgG-sandwich and IgM-capture ELISA for the detection of antibody to Rift Valley fever virus in humans. J. Virol. Methods. 2005;124(1–2):173–181. doi: 10.1016/j.jviromet.2004.11.020. [DOI] [PubMed] [Google Scholar]
- 28.Smithburn KC. Rift Valley fever; the neurotropic adaptation of the virus and the experimental use of this modified virus as a vaccine. Br. J. Exp. Pathol. 1949;30(1):1–16. [PMC free article] [PubMed] [Google Scholar]
- 29.WHO. The use of veterinary vaccines for prevention and control of Rift Valley fever: memorandum from a WHO/FAO meeting. Bull. World Health Organ. 1983;61(2):261–268. [PMC free article] [PubMed] [Google Scholar]
- 30. Grobbelaar AA, Weyer J, Leman PA, Kemp A, Paweska JT, Swanepoel R. Molecular epidemiology of Rift Valley fever virus. Emerg. Infect. Dis. 2011;17(12):2270–2276. doi: 10.3201/eid1712.111035. ••Indicates the occurrence of reassortment between Smithburn vaccine and wild-type RVF virus (RVFV).
- 31.Botros B, Omar A, Elian K. Adverse response of nonindigenous cattle of European breeds to live attenuated Smithburn Rift Valley fever vaccine. J. Med. Virol. 2006;78(6):787–791. doi: 10.1002/jmv.20624. [DOI] [PubMed] [Google Scholar]
- 32.Caplen H, Peters CJ, Bishop DH. Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J. Gen. Virol. 1985;66(Pt 10):2271–2277. doi: 10.1099/0022-1317-66-10-2271. [DOI] [PubMed] [Google Scholar]
- 33.Lokugamage N, Freiberg AN, Morrill JC, Ikegami T. Genetic subpopulations of Rift Valley fever ZH548, MP-12 and recombinant MP-12 strains. J. Virol. 2012;86:13566–13575. doi: 10.1128/JVI.02081-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Italy: FAO Animal Production and Health Proceedings, No 12. Food and Agriculture Organization of the United Nations (FAO); 2011. Rift Valley fever vaccine development, progress and constraints. Proceedings of the GF-TADs meeting, Rome, Italy, January 2011. [Google Scholar]
- 35.Eddy GA, Peters CJ, Meadors G, Cole FE., Jr Rift Valley fever vaccine for humans. Contr. Epidem. Biostatist. 1981;3:124–141. [Google Scholar]
- 36.Pittman PR, Liu CT, Cannon TL. Immunogenicity of an inactivated Rift Valley fever vaccine in humans: a 12-year experience. Vaccine. 2000;18(1–2):181–189. doi: 10.1016/s0264-410x(99)00218-2. [DOI] [PubMed] [Google Scholar]
- 37.Rusnak JM, Gibbs P, Boudreau E, Clizbe DP, Pittman P. Immunogenicity and safety of an inactivated Rift Valley fever vaccine in a 19-year study. Vaccine. 2011;29(17):3222–3229. doi: 10.1016/j.vaccine.2011.02.037. [DOI] [PubMed] [Google Scholar]
- 38.Piper ME, Sorenson DR, Gerrard SR. Efficient cellular release of Rift Valley fever virus requires genomic RNA. PLoS ONE. 2011;6(3):e18070. doi: 10.1371/journal.pone.0018070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lopez N, Muller R, Prehaud C, Bouloy M. The L protein of Rift Valley fever virus can rescue viral ribonucleoproteins and transcribe synthetic genome-like RNA molecules. J. Virol. 1995;69(7):3972–3979. doi: 10.1128/jvi.69.7.3972-3979.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ikegami T, Peters CJ, Makino S. Rift Valley fever virus nonstructural protein NSs promotes viral RNA replication and transcription in a minigenome system. J. Virol. 2005;79(9):5606–5615. doi: 10.1128/JVI.79.9.5606-5615.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bouloy M, Janzen C, Vialat P, et al. Genetic evidence for an interferon-antagonistic function of Rift Valley fever virus nonstructural protein NSs. J. Virol. 2001;75(3):1371–1377. doi: 10.1128/JVI.75.3.1371-1377.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Billecocq A, Gauliard N, Le May N, Elliott RM, Flick R, Bouloy M. RNA polymerase I-mediated expression of viral RNA for the rescue of infectious virulent and avirulent Rift Valley fever viruses. Virology. 2008;378(2):377–384. doi: 10.1016/j.virol.2008.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Habjan M, Pichlmair A, Elliott RM. NSs protein of Rift Valley fever virus induces the specific degradation of the double-stranded RNA-dependent protein kinase. J. Virol. 2009;83(9):4365–4375. doi: 10.1128/JVI.02148-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Muller R, Saluzzo JF, Lopez N. Characterization of clone 13, a naturally attenuated avirulent isolate of Rift Valley fever virus, which is altered in the small segment. Am. J. Trop. Med. Hyg. 1995;53(4):405–411. doi: 10.4269/ajtmh.1995.53.405. [DOI] [PubMed] [Google Scholar]
- 45.Ikegami T, Won S, Peters CJ, Makino S. Rescue of infectious Rift Valley fever virus entirely from cDNA, analysis of virus lacking the NSs gene, and expression of a foreign gene. J. Virol. 2006;80(6):2933–2940. doi: 10.1128/JVI.80.6.2933-2940.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gerrard SR, Nichol ST. Synthesis, proteolytic processing and complex formation of N-terminally nested precursor proteins of the Rift Valley fever virus glycoproteins. Virology. 2007;357(2):124–133. doi: 10.1016/j.virol.2006.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kakach LT, Suzich JA, Collett MS. Rift Valley fever virus M segment: phlebovirus expression strategy and protein glycosylation. Virology. 1989;170(2):505–510. doi: 10.1016/0042-6822(89)90442-x. [DOI] [PubMed] [Google Scholar]
- 48.Kakach LT, Wasmoen TL, Collett MS. Rift Valley fever virus M segment: use of recombinant vaccinia viruses to study Phlebovirus gene expression. J. Virol. 1988;62(3):826–833. doi: 10.1128/jvi.62.3.826-833.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Keegan K, Collett MS. Use of bacterial expression cloning to define the amino acid sequences of antigenic determinants on the G2 glycoprotein of Rift Valley fever virus. J. Virol. 1986;58(2):263–270. doi: 10.1128/jvi.58.2.263-270.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dessau M, Modis Y. Crystal structure of glycoprotein C from Rift Valley fever virus. Proc. Natl Acad. Sci. USA. 2013;110(5):1696–1701. doi: 10.1073/pnas.1217780110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Freiberg AN, Sherman MB, Morais MC, Holbrook MR, Watowich SJ. Three-dimensional organization of Rift Valley fever virus revealed by cryoelectron tomography. J. Virol. 2008;82(21):10341–10348. doi: 10.1128/JVI.01191-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rusu M, Bonneau R, Holbrook MR. An assembly model of Rift Valley fever virus. Front. Microbiol. 2012;3:254. doi: 10.3389/fmicb.2012.00254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sherman MB, Freiberg AN, Holbrook MR, Watowich SJ. Single-particle cryo-electron microscopy of Rift Valley fever virus. Virology. 2009;387(1):11–15. doi: 10.1016/j.virol.2009.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Huiskonen JT, Overby AK, Weber F, Grunewald K. Electron cryo-microscopy and single-particle averaging of Rift Valley fever virus: evidence for GN-GC glycoprotein heterodimers. J. Virol. 2009;83(8):3762–3769. doi: 10.1128/JVI.02483-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Won S, Ikegami T, Peters CJ, Makino S. NSm and 78-kilodalton proteins of Rift Valley fever virus are nonessential for viral replication in cell culture. J. Virol. 2006;80(16):8274–8278. doi: 10.1128/JVI.00476-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gerrard SR, Bird BH, Albarino CG, Nichol ST. The NSm proteins of Rift Valley fever virus are dispensable for maturation, replication and infection. Virology. 2007;359(2):459–465. doi: 10.1016/j.virol.2006.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Terasaki K, Won S, Makino S. The C-terminal region of Rift Valley fever virus NSm protein targets the protein to the mitochondrial outer membrane and exerts anti-apoptotic function. J. Virol. 2013;87:676–682. doi: 10.1128/JVI.02192-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Won S, Ikegami T, Peters CJ, Makino S. NSm protein of Rift Valley fever virus suppresses virus-induced apoptosis. J. Virol. 2007;81(24):13335–13345. doi: 10.1128/JVI.01238-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Struthers JK, Swanepoel R, Shepherd SP. Protein synthesis in Rift Valley fever virus-infected cells. Virology. 1984;134(1):118–124. doi: 10.1016/0042-6822(84)90277-0. [DOI] [PubMed] [Google Scholar]
- 60.Muller R, Poch O, Delarue M, Bishop DH, Bouloy M. Rift Valley fever virus L segment: correction of the sequence and possible functional role of newly identified regions conserved in RNA-dependent polymerases. J. Gen. Virol. 1994;75:1345–1352. doi: 10.1099/0022-1317-75-6-1345. [DOI] [PubMed] [Google Scholar]
- 61.Morin B, Coutard B, Lelke M. The N-terminal domain of the arenavirus L protein is an RNA endonuclease essential in mRNA transcription. PLoS Pathog. 2010;6(9):e1001038. doi: 10.1371/journal.ppat.1001038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Reguera J, Weber F, Cusack S. Bunyaviridae RNA polymerases (L-protein) have an N-terminal, influenza-like endonuclease domain, essential for viral cap-dependent transcription. PLoS Pathog. 2010;6(9):e1001101. doi: 10.1371/journal.ppat.1001101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lozach PY, Kuhbacher A, Meier R, et al. DC-SIGN as a receptor for phleboviruses. Cell Host Microbe. 2011;10(1):75–88. doi: 10.1016/j.chom.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 64.Lozach PY, Mancini R, Bitto D, et al. Entry of bunyaviruses into mammalian cells. Cell Host Microbe. 2010;7(6):488–499. doi: 10.1016/j.chom.2010.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.de Boer SM, Kortekaas J, de Haan CA, Rottier PJ, Moormann RJ, Bosch BJ. Heparan sulfate facilitates Rift Valley fever virus entry into the cell. J. Virol. 2012;86(24):13767–13771. doi: 10.1128/JVI.01364-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Harmon B, Schudel BR, Maar D. Rift Valley fever virus strain MP-12 enters mammalian host cells via caveolae-mediated endocytosis. J. Virol. 2012;86:12954–12970. doi: 10.1128/JVI.02242-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Raymond DD, Piper ME, Gerrard SR, Smith JL. Structure of the Rift Valley fever virus nucleocapsid protein reveals another architecture for RNA encapsidation. Proc. Natl Acad. Sci. USA. 2010;107(26):11769–11774. doi: 10.1073/pnas.1001760107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ikegami T, Won S, Peters CJ, Makino S. Rift Valley fever virus NSs mRNA is transcribed from an incoming anti-viral-sense S RNA segment. J. Virol. 2005;79(18):12106–12111. doi: 10.1128/JVI.79.18.12106-12111.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gerrard SR, Nichol ST. Characterization of the Golgi retention motif of Rift Valley fever virus G(N) glycoprotein. J. Virol. 2002;76(23):12200–12210. doi: 10.1128/JVI.76.23.12200-12210.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Findlay GM. Rift Valley fever on enzootic hepatitis. Trans. R. Soc. Trop. Med. Hyg. 1931;25:229–262. [Google Scholar]
- 71.Smith DR, Steele KE, Shamblin J. The pathogenesis of Rift Valley fever virus in the mouse model. Virology. 2010;407(2):256–267. doi: 10.1016/j.virol.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 72.Gommet C, Billecocq A, Jouvion G. Tissue tropism and target cells of NSs-deleted Rift Valley fever virus in live immunodeficient mice. PLoS Negl. Trop. Dis. 2011;5(12):e1421. doi: 10.1371/journal.pntd.0001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lihoradova O, Kalveram B, Indran SV, et al. The dominant-negative inhibition of double-stranded RNA-dependent protein kinase PKR increases the efficacy of Rift Valley fever virus MP-12 vaccine. J. Virol. 2012;86(14):7650–7661. doi: 10.1128/JVI.00778-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Reed C, Steele KE, Honko A, Shamblin J, Hensley LE, Smith DR. Ultrastructural study of Rift Valley fever virus in the mouse model. Virology. 2012;431(1–2):58–70. doi: 10.1016/j.virol.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 75.Niklasson BS, Meadors GF, Peters CJ. Active and passive immunization against Rift Valley fever virus infection in Syrian hamsters. Acta Pathol. Microbiol. Immunol. Scand. (C) 1984;92(4):197–200. doi: 10.1111/j.1699-0463.1984.tb00074.x. [DOI] [PubMed] [Google Scholar]
- 76. Dodd KA, McElroy AK, Jones ME, Nichol ST, Spiropoulou CF. Rift Valley fever virus clearance and protection from neurologic disease are dependent on CD4+ T cell and virus-specific antibody responses. J. Virol. 2013;87(11):6161–6171. doi: 10.1128/JVI.00337-13. •Demonstrates the requirement for RVFV clearance in a mouse model.
- 77.Indran SV, Lihoradova OA, Phoenix I. Rift Valley fever virus MP-12 vaccine encoding Toscana virus NSs retains the neuroinvasiveness in mice. J. Gen. Virol. 2013 doi: 10.1099/vir.0.051250-0. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Lihoradova OA, Indran SV, Kalveram B, et al. Characterization of Rift Valley fever virus MP-12 strain encoding NSs of Punta Toro virus or sandfly fever Sicilian virus. PLoS Negl. Trop. Dis. 2013;7(4):e2181. doi: 10.1371/journal.pntd.0002181. ••Characterized the functions of PTV and SFSV NSs, the efficacy of MP-12 encoding such NSs in a mouse model.
- 79.Jansen van Vuren P, Tiemessen CT, Paweska JT. Anti-nucleocapsid protein immune responses counteract pathogenic effects of Rift Valley fever virus infection in mice. PLoS ONE. 2011;6(9):e25027. doi: 10.1371/journal.pone.0025027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yadani FZ, Kohl A, Prehaud C, Billecocq A, Bouloy M. The carboxy-terminal acidic domain of Rift Valley fever virus NSs protein is essential for the formation of filamentous structures but not for the nuclear localization of the protein. J. Virol. 1999;73(6):5018–5025. doi: 10.1128/jvi.73.6.5018-5025.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Billecocq A, Spiegel M, Vialat P, et al. NSs protein of Rift Valley fever virus blocks interferon production by inhibiting host gene transcription. J. Virol. 2004;78(18):9798–9806. doi: 10.1128/JVI.78.18.9798-9806.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kohl A, di Bartolo V, Bouloy M. The Rift Valley fever virus nonstructural protein NSs is phosphorylated at serine residues located in casein kinase II consensus motifs in the carboxy-terminus. Virology. 1999;263(2):517–525. doi: 10.1006/viro.1999.9978. [DOI] [PubMed] [Google Scholar]
- 83.Le May N, Dubaele S, Proietti De Santis L, Billecocq A, Bouloy M, Egly JM. TFIIH transcription factor, a target for the Rift Valley hemorrhagic fever virus. Cell. 2004;116(4):541–550. doi: 10.1016/s0092-8674(04)00132-1. [DOI] [PubMed] [Google Scholar]
- 84.Le May N, Mansuroglu Z, Leger P, et al. A SAP30 complex inhibits IFN-beta expression in Rift Valley fever virus infected cells. PLoS Pathog. 2008;4(1):e13. doi: 10.1371/journal.ppat.0040013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ikegami T, Narayanan K, Won S, Kamitani W, Peters CJ, Makino S. Rift Valley fever virus NSs protein promotes post-transcriptional downregulation of protein kinase PKR and inhibits eIF2alpha phosphorylation. PLoS Pathog. 2009;5(2):e1000287. doi: 10.1371/journal.ppat.1000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Kalveram B, Lihoradova O, Indran SV, Lokugamage N, Head JA, Ikegami T. Rift Valley fever virus NSs inhibits host transcription independently of the degradation of dsRNA-dependent protein kinase PKR. Virology. 2013;435:415–424. doi: 10.1016/j.virol.2012.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kalveram B, Lihoradova O, Ikegami T. NSs protein of Rift Valley fever virus promotes post-translational downregulation of the TFIIH subunit p62. J. Virol. 2011;85:6234–6243. doi: 10.1128/JVI.02255-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Verdaasdonk JS, Bloom K. Centromeres: unique chromatin structures that drive chromosome segregation. Nat. Rev. Mol. Cell. Biol. 2011;12(5):320–332. doi: 10.1038/nrm3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mansuroglu Z, Josse T, Gilleron J, et al. Non structural NSs protein of Rift Valley fever Virus interacts with pericentromeric DNA sequences of the host cell inducing chromosome cohesion and segregation defects. J. Virol. 2009;84:928–939. doi: 10.1128/JVI.01165-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Baer A, Austin D, Narayanan A, et al. Induction of DNA damage signaling upon Rift Valley fever virus infection results in cell cycle arrest and increased viral replication. J. Biol. Chem. 2012;287(10):7399–7410. doi: 10.1074/jbc.M111.296608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Austin D, Baer A, Lundberg L, et al. p53 activation following Rift Valley fever virus infection contributes to cell death and viral production. PLoS ONE. 2012;7(5):e36327. doi: 10.1371/journal.pone.0036327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Benferhat R, Josse T, Albaud B, et al. Large-scale chromatin immunoprecipitation with promoter sequence microarray analysis of the interaction of the NSs protein of Rift Valley fever virus with regulatory DNA regions of the host genome. J. Virol. 2012;86(20):11333–11344. doi: 10.1128/JVI.01549-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Vaughn VM, Streeter CC, Miller DJ, Gerrard SR. Restriction of Rift Valley fever virus virulence in mosquito cells. Viruses. 2010;2(2):655–675. doi: 10.3390/v2020655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Leger P, Lara E, Jagla B, et al. Dicer-2-and Piwi-mediated RNA interference in Rift Valley fever virus-infected mosquito cells. J. Virol. 2013;87(3):1631–1648. doi: 10.1128/JVI.02795-12. ••Demonstrates the generation of viRNA in mosquito cells infected with RVFV.
- 95.Dungu B, Louw I, Lubisi A, Hunter P, von Teichman BF, Bouloy M. Evaluation of the efficacy and safety of the Rift Valley fever Clone 13 vaccine in sheep. Vaccine. 2010;28(29):4581–4587. doi: 10.1016/j.vaccine.2010.04.085. [DOI] [PubMed] [Google Scholar]
- 96.von Teichman B, Engelbrecht A, Zulu G, Dungu B, Pardini A, Bouloy M. Safety and efficacy of Rift Valley fever Smithburn and Clone 13 vaccines in calves. Vaccine. 2011;29(34):5771–5777. doi: 10.1016/j.vaccine.2011.05.055. [DOI] [PubMed] [Google Scholar]
- 97.Thiongane Y, Lena P, Moustapha M, et al. Pathogenicity and immunogenicity of the reassortant attenuated strain R566 of Rift Valley fever virus in sheep. Presented at: The FAO/IAEA International Symposium on Applications of Gene-based Technologies for Improving Animal Production and Health in Developing Countries; Austria. 6–10 October 2003. [Google Scholar]
- 98.Habjan M, Penski N, Spiegel M, Weber F. T7 RNA polymerase-dependent and -independent systems for cDNA-based rescue of Rift Valley fever virus. J. Gen. Virol. 2008;89(Pt 9):2157–2166. doi: 10.1099/vir.0.2008/002097-0. [DOI] [PubMed] [Google Scholar]
- 99.Bird BH, Albarino CG, Hartman AL, Erickson BR, Ksiazek TG, Nichol ST. Rift Valley fever virus lacking the NSs and NSm genes is highly attenuated, confers protective immunity from virulent virus challenge, and allows for differential identification of infected and vaccinated animals. J. Virol. 2008;82(6):2681–2691. doi: 10.1128/JVI.02501-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bird BH, Maartens LH, Campbell S, et al. Rift Valley fever virus vaccine lacking the NSs and NSm genes is safe, nonteratogenic, and confers protection from viremia, pyrexia, and abortion following challenge in adult and pregnant sheep. J. Virol. 2011;85(24):12901–12909. doi: 10.1128/JVI.06046-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bird BH, Albarino CG, Nichol ST. Rift Valley fever virus lacking NSm proteins retains high virulence in vivo and may provide a model of human delayed onset neurologic disease. Virology. 2007;362(1):10–15. doi: 10.1016/j.virol.2007.01.046. [DOI] [PubMed] [Google Scholar]
- 102.Crabtree MB, Kent Crockett RJ, Bird BH, et al. Infection and transmission of Rift Valley fever viruses lacking the NSs and/or NSm genes in mosquitoes: potential role for NSm in mosquito infection. PLoS Negl. Trop. Dis. 2012;6(5):e1639. doi: 10.1371/journal.pntd.0001639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.McElroy AK, Albarino CG, Nichol ST. Development of a RVFV ELISA that can distinguish infected from vaccinated animals. Virol. J. 2009;6:125. doi: 10.1186/1743-422X-6-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Fernandez JC, Billecocq A, Durand JP, et al. The nonstructural protein NSs induces a variable antibody response in domestic ruminants naturally infected with Rift Valley fever virus. Clin. Vaccine Immunol. 2012;19(1):5–10. doi: 10.1128/CVI.05420-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Faburay B, Wilson W, McVey DS, et al. Rift Valley fever virus structural and nonstructural proteins: recombinant protein expression and immunoreactivity against antisera from sheep. Vector Borne Zoonotic Dis. 2013;13(9):619–629. doi: 10.1089/vbz.2012.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lihoradova O, Ikegami T. Modifying the NSs gene to improve live-attenuated vaccine for Rift Valley fever. Expert Rev. Vaccines. 2012;11(11):1283–1285. doi: 10.1586/erv.12.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Matsuno K, Weisend C, Travassos da Rosa AP, et al. Characterization of the Bhanja serogroup viruses (Bunyaviridae): a novel species of the genus Phlebovirus and its relationship with other emerging tick-borne phleboviruses. J. Virol. 2013;87(7):3719–3728. doi: 10.1128/JVI.02845-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yu XJ, Liang MF, Zhang SY, et al. Fever with thrombocytopenia associated with a novel bunyavirus in China. N. Engl. J. Med. 2011;364(16):1523–1532. doi: 10.1056/NEJMoa1010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Xu F, Chen H, Travassos da Rosa AP, Tesh RB, Xiao SY. Phylogenetic relationships among sandfly fever group viruses (Phlebovirus: Bunyaviridae) based on the small genome segment. J. Gen. Virol. 2007;88(Pt 8):2312–2319. doi: 10.1099/vir.0.82860-0. [DOI] [PubMed] [Google Scholar]
- 110.Kalveram B, Ikegami T. Toscana virus NSs protein promotes degradation of doublestranded RNA-dependent protein kinase. J. Virol. 2013;87:3710–3718. doi: 10.1128/JVI.02506-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gori Savellini G, Weber F, Terrosi C, Habjan M, Martorelli B, Cusi MG. Toscana virus induces interferon although its NSs protein reveals antagonistic activity. J. Gen. Virol. 2010;92(Pt 1):71–79. doi: 10.1099/vir.0.025999-0. [DOI] [PubMed] [Google Scholar]
- 112.Perrone LA, Narayanan K, Worthy M, Peters CJ. The S segment of Punta Toro virus (Bunyaviridae, Phlebovirus) is a major determinant of lethality in the Syrian hamster and codes for a type I interferon antagonist. J. Virol. 2007;81(2):884–892. doi: 10.1128/JVI.01074-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ikegami T, Makino S. Rift Valley fever vaccines. Vaccine. 2009;27(Suppl. 4):D69–D72. doi: 10.1016/j.vaccine.2009.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Indran SV, Ikegami T. Novel approaches to develop Rift Valley fever vaccines. Front. Cell. Infect. Microbiol. 2012;2:131. doi: 10.3389/fcimb.2012.00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mandell RB, Flick R. Rift Valley fever virus: an unrecognized emerging threat? Hum. Vaccin. 2010;6(7):597–601. doi: 10.4161/hv.6.7.11761. [DOI] [PubMed] [Google Scholar]
- 116.Kortekaas J, Antonis AF, Kant J, et al. Efficacy of three candidate Rift Valley fever vaccines in sheep. Vaccine. 2012;30(23):3423–3429. doi: 10.1016/j.vaccine.2012.03.027. [DOI] [PubMed] [Google Scholar]
- 117.Huggins JW. Prospects for treatment of viral hemorrhagic fevers with ribavirin, a broad-spectrum antiviral drug. Rev. Infect. Dis. 1989;11(Suppl. 4):S750–S761. doi: 10.1093/clinids/11.supplement_4.s750. [DOI] [PubMed] [Google Scholar]
- 118.Peters CJ, Reynolds JA, Slone TW, Jones DE, Stephen EL. Prophylaxis of Rift Valley fever with antiviral drugs, immune serum, an interferon inducer, and a macrophage activator. Antiviral Res. 1986;6(5):285–297. doi: 10.1016/0166-3542(86)90024-0. [DOI] [PubMed] [Google Scholar]
- 119.Kende M, Alving CR, Rill WL, Swartz GM, Jr, Canonico PG. Enhanced efficacy of liposome-encapsulated ribavirin against Rift Valley fever virus infection in mice. Antimicrob. Agents Chemother. 1985;27(6):903–907. doi: 10.1128/aac.27.6.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.McHutchison JG, Gordon SC, Schiff ER, et al. Interferon alfa-2b alone or in combination with ribavirin as initial treatment for chronic hepatitis C. Hepatitis Interventional Therapy Group. N. Engl. J. Med. 1998;339(21):1485–1492. doi: 10.1056/NEJM199811193392101. [DOI] [PubMed] [Google Scholar]
- 121.Dominguez KD, Mercier RC. Treatment of RSV pneumonia in adults–evidence of ribavirin effectiveness? Ann. Pharmacother. 1999;33(6):739–741. doi: 10.1345/aph.18243. [DOI] [PubMed] [Google Scholar]
- 122.Knowles SR, Phillips EJ, Dresser L, Matukas L. Common adverse events associated with the use of ribavirin for severe acute respiratory syndrome in Canada. Clin. Infect. Dis. 2003;37(8):1139–1142. doi: 10.1086/378304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Gowen BB, Bailey KW, Scharton D, et al. Post-exposure vaccination with MP-12 lacking NSs protects mice against lethal Rift Valley fever virus challenge. Antiviral Res. 2013;98(2):135–143. doi: 10.1016/j.antiviral.2013.03.009. •Demonstrated the efficacy of rMP12-C13type as a post-exposure vaccine in mice.
- 124.Head JA, Kalveram B, Ikegami T. Functional analysis of Rift Valley fever virus NSs encoding a partial truncation. PLoS ONE. 2012;7:e45730. doi: 10.1371/journal.pone.0045730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Narayanan A, Kehn-Hall K, Senina S, et al. Curcumin inhibits Rift Valley fever virus replication in human cells. J. Biol. Chem. 2012;287(40):33198–33214. doi: 10.1074/jbc.M112.356535. ••Demonstrates the inhibitory effect of curcumin in IKK complex and RVFV replication.