Abstract
The arsenic (As) content of groundwater pumped from all tubewells within 61 contiguous villages of Araihazar, Bangladesh, was determined a first time in 2000–01 with laboratory measurements and a second time in 2012–13 using the ITS Arsenic Econo-Quick kit. The two surveys indicate that the total number of tubewells within the area almost doubled from 5,560 to 10,879 over 12 years. The evolution of the distribution of well ages between the two surveys is consistent with a simple model that combines an annual increase of 42 wells/year in the rate of installations within the 61 villages starting in 1980 and a 7%/year rate of abandonment of wells as a function of well age. Colored placards were posted on each pumphead in 2012–2013 on the basis of the kit results relative to the WHO guideline for As and the Bangladesh standard for As in drinking water: blue for As ≤10 µg/L, green >10–50 µg/L, and red: >50 µg/L. According to quality-control samples collected from 502 tubewells for comparing the kit results with laboratory measurements, not a single well labeled blue in 2012–13 should have been labeled red and vice-versa. Field-kit testing in 2012–13 did not change the status of wells relative to the Bangladesh standard of 876 (87%) out of 1,007 wells with a placard based on laboratory measurements in 2000–01 still attached to the pumphead. The high proportion of tubewells believed by households to be unsafe (66% out of 2,041) that were still used for drinking and cooking in 2012–13 underlines the need for more widespread testing to identify low-As wells as an alternative source of drinking water.
Keywords: Groundwater, arsenic, well testing, Bangladesh
Introduction
Scientists and policy makers have known for 10–25 years that a sizeable fraction of the tens of millions of tubewells installed by villagers in soft alluvial sediments of Bangladesh, Cambodia, India, Myanmar, Nepal, Pakistan, and Vietnam tap shallow groundwater that is contaminated with arsenic (As) of natural origin (Ravenscroft et al., 2009). Early concerns about exposure to As levels in drinking water exceeding the WHO guideline of 10 µg/L by ten- to hundred-fold focused on skin lesions and internal cancers (Smith et al., 2000). More recent work has revealed a marked increase in all-cause deaths attributable primarily to cardio-vascular disease (Chen et al., 2011). Arsenic in tubewell water has also been associated with increased infant mortality and impaired intellectual and motor function in children (Rahman et al., 2010; Parvez et al., 2011; Wasserman et al., 2011). In addition, the debilitating effects of As have been associated in Bangladesh, the most affected country, with a significant drop in household income and are expected to impose an enormous economic burden in the future because of lost productivity (Pitt et al., 2012; Flanagan et al., 2012).
Despite mounting evidence of the serious consequences of As exposure, the proportion of the rural population still drinking from unsafe wells in Bangladesh remains high and in some regions may not even have declined (Ahmed et al., 2006; DPHE/JICA, 2010). Millions of villagers have learned from public information campaigns and the media that As concentrations can be high in tubewell water and that drinking this water is detrimental to health. But more often than not, the same villagers do not know the status of their own or their neighbor’s well (WASH, 2008; George et al. 2012a). Blanket testing carried out in Bangladesh and neighboring affected states of India has shown that the distribution of As in groundwater is highly variable spatially, even with a single village (BGS/DPHE, 2001; Chakraborti et al., 2003; McArthur et al., 2004; Jakariya et al., 2007; Nickson et al., 2007). Repeated sampling of a limited number of wells has shown, however, that the distribution of As in the subsurface is generally stable through time (van Geen et al., 2005; 2007; Dhar et al., 2008; McArthur et al., 2010). Spatial variability in the distribution of As in groundwater therefore complicates prediction but also represents an opportunity for households to share the subset of safe wells. Within the area of Bangladesh that is the focus of this study, for instance, approximately half the tubewells were unsafe a decade ago but almost 90% of the households lived within 100 m of a safe well (van Geen et al., 2002). The implication is that the greatest barrier to exposure reduction may often not be that there are no low-As wells in a village but that they have not been identified due to lack of testing.
A blanket testing campaign of almost 5 million wells across As-affected areas of Bangladesh carried out in 2000–2005, along with the installation of community wells where low-As aquifers are available at depth, probably resulted in a marked reduction in exposure (Ahmed et al., 2006). The impact of such testing campaigns is evaluated in this paper by comparing the results of two rounds of well testing conducted 12 years apart within the same area 25 km2 of Bangladesh. The data from the two surveys are used to estimate the pace of installation of new wells and the status of the newly installed wells. The wells sampled twice that could be unambiguously identified by a placard posted on the pump during the first survey are used to determine whether their status with respect to As changed during the intervening period. On the basis of laboratory analysis for a subset of wells, the extent to which an existing commercial field-kit for As testing can be relied on to distinguish wells that meet the WHO guideline for As of 10 µg/L from wells that exceed the Bangladesh standard of 50 µg/L is also evaluated. Finally, responses to a short household survey are used to determine to what extent switching between the two surveys might have been limited by lack of testing and distance to a safe well.
Methods
The study area is located 20 km northeast of Dhaka and encompasses 61 villages distributed within a 25 km2 portion of Araihazar upazilla (van Geen et al., 2003). Sampling of all wells within these villages started in early 2000 and extended into early 2001 for the recruitment of an initial cohort of 11,000 men and women for the Health Effects of Arsenic Longitudinal Study (HEALS). While sampling, well-depth and well-age information was obtained from the households, in addition to recording geographic coordinates using hand-held Global Positioning System (GPS) receivers. The original samples were all analyzed by Graphite Furnace Atomic Absorption Spectroscopy (GFAAS). Samples below the detection limit for that method were subsequently re-analyzed by High-Resolution Inductively-Coupled Plasma Mass Spectrometry (HR ICP-MS) (van Geen et al., 2005). Whereas households were informed of the test results earlier, placards with the first round of test results were actually mounted on the wells only in 2005 (Opar et al., 2007).
In early 2012, ten women previously employed in the HEALS study area to carry out a public-health intervention were trained by two male supervisors to use a test kit for As shown to be reliable and fast (George et al. 2012b) and to enter the results along with additional tubewell and household information on a Garmin 76Cx hand-held GPS unit. This information was typically obtained by asking the wife of the owner of a well, after explaining the purpose of the visit and summarizing the health risks posed by drinking water containing high levels of As. The testing campaign covered a total of 48,790 wells across the entire Arahaizar upazilla between February 2012 and September 2013. Within the original area surveyed in 2000–01, all but 52 of the wells were tested by a subset of six of the women because the other four were assigned to other areas within the upazilla. Testing of wells and collecting household information in Araihazar was approved by the Columbia Institutional Review Board and the Bangladesh Medical Research Council.
The ITS Arsenic Econo-Quick kit (http://www.sensafe.com/481298.php) is based on the 19th century Gutzeit method and was used according to the manufacturer’s instructions, with the exception that Reagent 2, an oxidant added to remove interference by hydrogen sulfide, was not used. In our experience, signal suppression by sulfide is not an issue for Bangladesh groundwater. Each 50 mL sample was collected directly into the kit’s reaction vessel after pumping for approximately one minute, regardless of well depth. The vessel was thoroughly cleaned with a brush between each analysis to ensure that no zinc powder from the previous analysis remained. Village workers visually compared the color of the mercuric bromide strip to that of a reference scale corresponding to 0, 10, 25, 50, 100, 200, 300, 500 and 1000 µg/L As, as detailed in George et al. (2012b). The test strip was taped in a bound notebook and the closest match in color, without interpolation, was recorded along with the village name, well depth in feet, well age in years, status of the well with respect to As if know to the owner, and whether the household was using the well for drinking or cooking. The GPS position was captured when the test result and additional well and household data were entered as a formatted string of characters, typically right at the well or nearby if this was prevented by a roof or thick tree cover.
If the test indicated that the well contained >50 µg/L As, a red placard (Fig. 1) indicating that the well was unsafe to drink from was attached to the well and the household was encouraged to seek a neighboring well that contained less As. If the test indicated that the well contained 25 or 50 µg/L As, a green placard was attached and the household was told that although their well met the national standard for As, drinking and cooking from a well that met the WHO guideline would be better for their health. If the test indicated that the well contained up to 0 or 10 µg/L As, a blue placard was attached and the household was encouraged to allow neighbors with high-As wells to use their well. Households were told that it is safe to wash with water even from a well that is high in As.
Figure 1.
Stainless steel placards attached in 2012–2013 to pumpheads of Araihazar on the basis of field-kit results. The text on the (a) blue and (b) green placards translates as “arsenic safe water” and on the (c) red placard as “arsenic unsafe water”.
Testers were assigned to a village by their supervisor and asked to complete the blanket survey of that village before moving on to the next one in order to facilitate tracking of their progress. Each tester typically worked from 8 AM to 3 PM and reported results for an average of 12 wells per day, 6 days per week excluding holidays. Once a week, the handheld GPS units were connected to one of the supervisor’s laptops through a USB cable and the data were transferred. The text string paired with each coordinate was parsed in a Microsoft Excel spreadsheet. After correcting the occasional data entry error by referring to the notebook, the spreadsheet was converted into a text file and imported in Google Earth Pro. The weekly progress of the testers was determined by comparing the location of the wells with the extent of the villages, which is easily determined from satellite image by the contrast between tree cover and open fields.
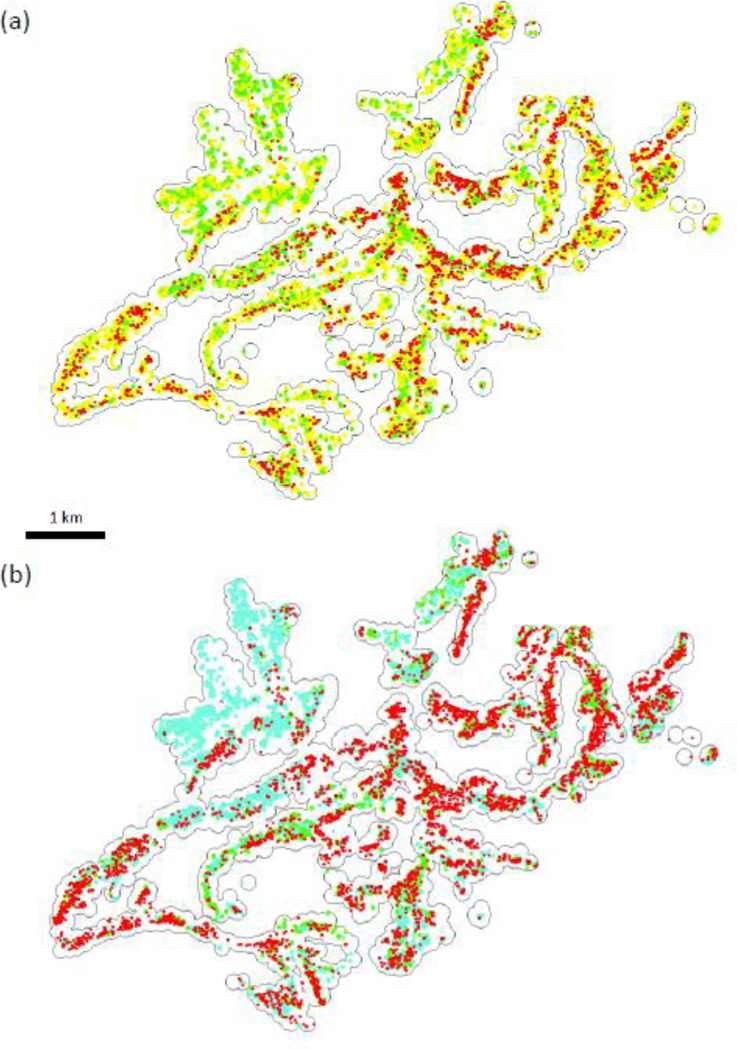
To ensure that data collected from the same set of villages are compared in this analysis, a 100-m buffer was created in ArcMap 10.1 around each of the wells from the original set of 5,999 wells tested in 2000–01 and only wells within this buffer tested in 2012–13 were selected (Fig. 2a). Similarly, wells from the original survey whose coordinates did not correspond to locations within 100 m of the newly surveyed wells, because of data entry errors or because of incomplete coverage by the new survey, were excluded. ArcMap 10.1 was also used to calculate the distance from each unsafe well to the nearest safe well, as perceived by the household or measured with the field kit.
Figure 2.
Map of well status across the Araihazar study area based on (a) perception of 10,879 households with green symbols corresponding to “safe”, red to “unsafe”, and yellow to “unknown” and (b) field-kit measurements for 10,879 wells with light blue wells indicating a reading of 0 or 10 µg/L, green 25 and 50 µg/L, and red 100 µg/L and above. The thin black line corresponds to 100-m buffers merged around each of the original set of 5,560 wells sampled in 2000–01.
During the first 5 months of the testing campaign, samples were collected for laboratory analysis from a random subset of 502 wells. Several days before analysis, groundwater was acidified to 1% Optima HCl in the laboratory. This has been shown to entirely re-dissolve any iron and As precipitates that could have formed (van Geen et al., 2007). The uncertainty of the first round of As analyses by graphite-furnace atomic absorption of the 2000–01 samples was previously estimated at ±7 µg/L for concentrations below 70 µg/L and ±10% at higher concentrations (van Geen et al., 2003). After adapting the procedure ofCheng et al. (2004) to an Element2 high-resolution inductively coupled plasma mass spectrometer at Lamont-Doherty Earth Observatory, the estimated precision was improved to ±3% across the entire range of As concentrations. This estimate is based on the analysis of the three consistency standards over a set of 20 days of analysis. For the Trace Element in Water Reference Standard NIST1640A with a certified As concentration of 8.075±0.070 µg/L, the measurements averaged 8.1±0.2 µg/L (±3%, 1-sigma; n=68); for NIST1643 with a certified concentration of 60.45±0.72 µg/L, the measurements averaged 58.6+1.3 µg/L (±2%, n=68); and reproducibility for an internal consistency standard included with each run was 433±13 µg/L (±3%, n=69). On the basis of the variability of the analytical blank, the detection limit of the new procedure is estimated to be <0.1 µg/L.
Results
Well ages
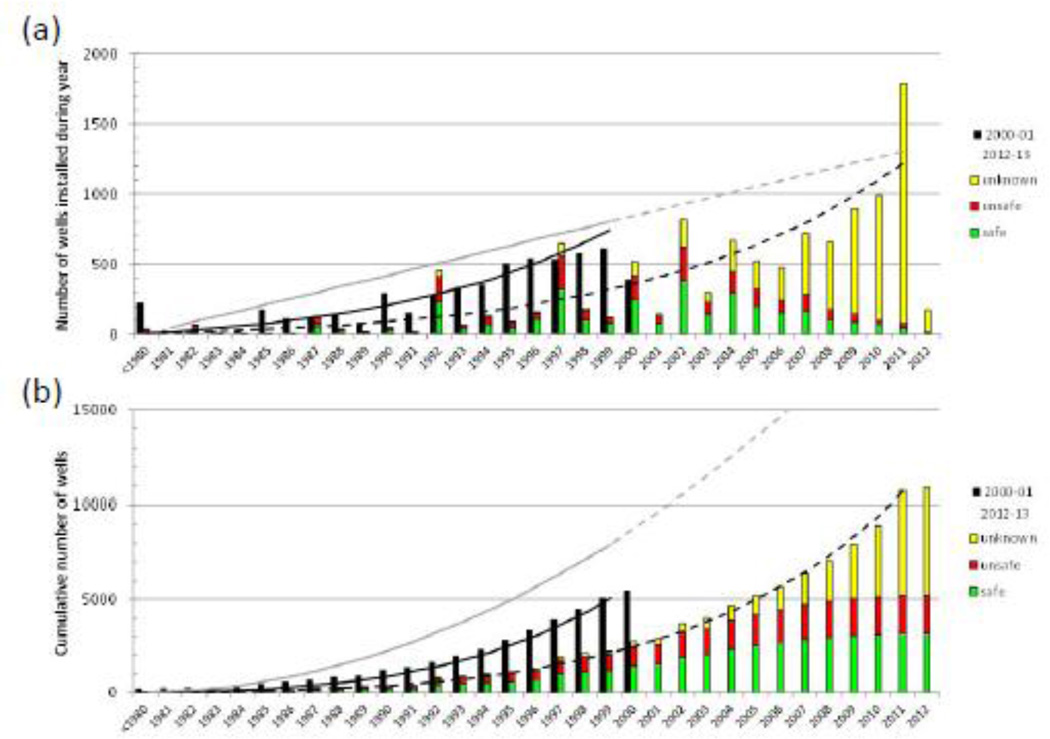
The 61 villages of Araihazar where the two blanket surveys overlap contained a total of 5,560 wells in 2000–01 and 10,879 wells in 2012–13. Only 223 of these wells were installed before 1980 according to the 2000–01 survey and 37 according to the 2012–13 survey (Fig. 3a). With some year-to-year variability possibly due in part to recall bias, the distribution of installation years indicate a steady increase in the installation rate to 600 wells/year in 2000–01 and about double that rate in 2012–13. The cumulative number of wells calculated on the basis of the two surveys dampens year-to-year variability and shows that the total number of wells within the study area throughout the decade preceding the first survey is about twice that inferred from the 2000–01 data compared to the 2012–13 data (Fig. 3b). A striking number of wells surveyed in 2000–01 were evidently abandoned during the subsequent decade.
Figure 3.
(a) Distribution of well installation dates provided by 5,560 households in 2000–01 (black bars) and 10,879 households in 2012–13 (green, red, and yellow bars). (b) Cumulative number of wells calculated from the distribution of well installation dates in (a). Black lines shown model predictions assuming a 42 well/year increase in installation rate starting in 1980 and 7%/year loss rate for 2000–01 (continuous line) and 2012–13 (dashed line).
Well status
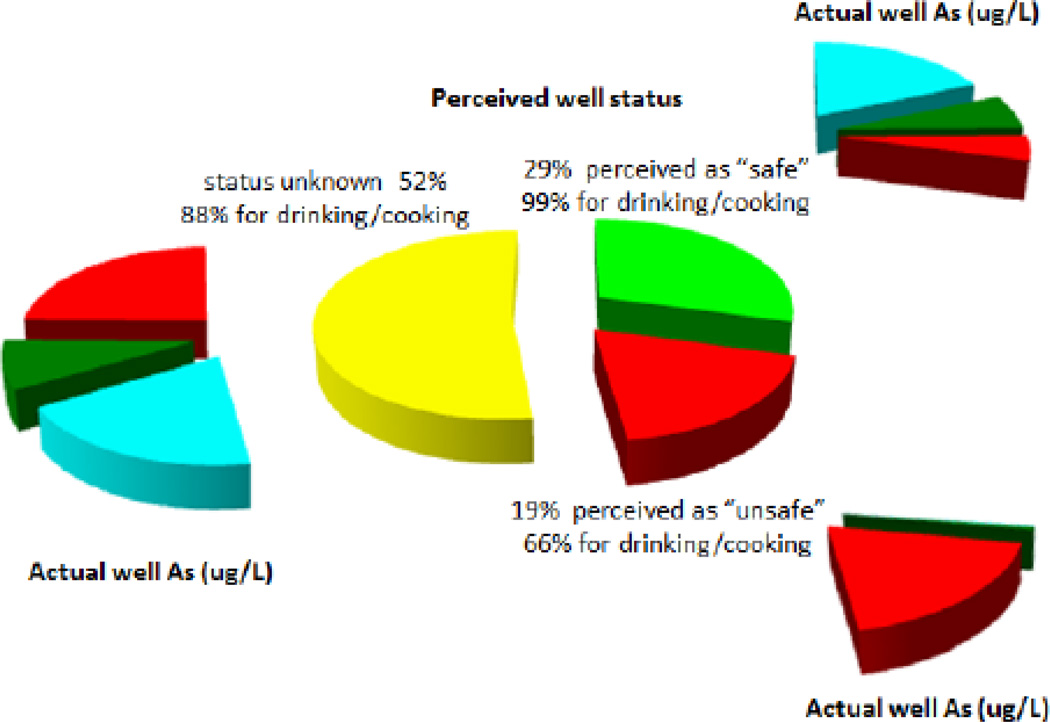
In 2000–01, very few households knew the status of their well until laboratory results were communicated by HEALS staff. In 2003, testers using a field-kit swept through the area again under the government’s Bangladesh Arsenic Mitigation and Water Supply Program (BAMWSP). Despite these two successive blanket testing campaigns, households claimed to know the status of only half the tubewells in tested in 2012–13 (Fig. 4). Household responses recorded in 2012–13 indicate that perceived well status is only one of the factors determining behavior. Among the 29% of tested wells perceived to be safe, the vast majority (99%) was used for drinking and cooking (Fig. 4). For the 52% of wells of unsafe status, the proportion used for drinking and cooking was also high at 88%. Sadly, for the remaining 19% of tested wells the proportion used for drinking and cooking remains very high at 66%. Even in an area where the population has probably been reminded of the health risks of As exposure more often than just about anywhere in Bangladesh, a high fraction of wells believed to be unsafe are still used for drinking and cooking.
Figure 4.
Pie diagrams showing the proportion of 10,879 wells believed by households to be safe (green), unsafe (red), and whose status is unknown (yellow). The central pie lists the proportion of wells within each of these groups that households use for drinking and cooking. Also shown w is the actual status of wells within each of these groups based on field-kit testing relative to the WHO guideline of 10 µg/L and the Bangladesh standard of 50 µg/L.
Quality control
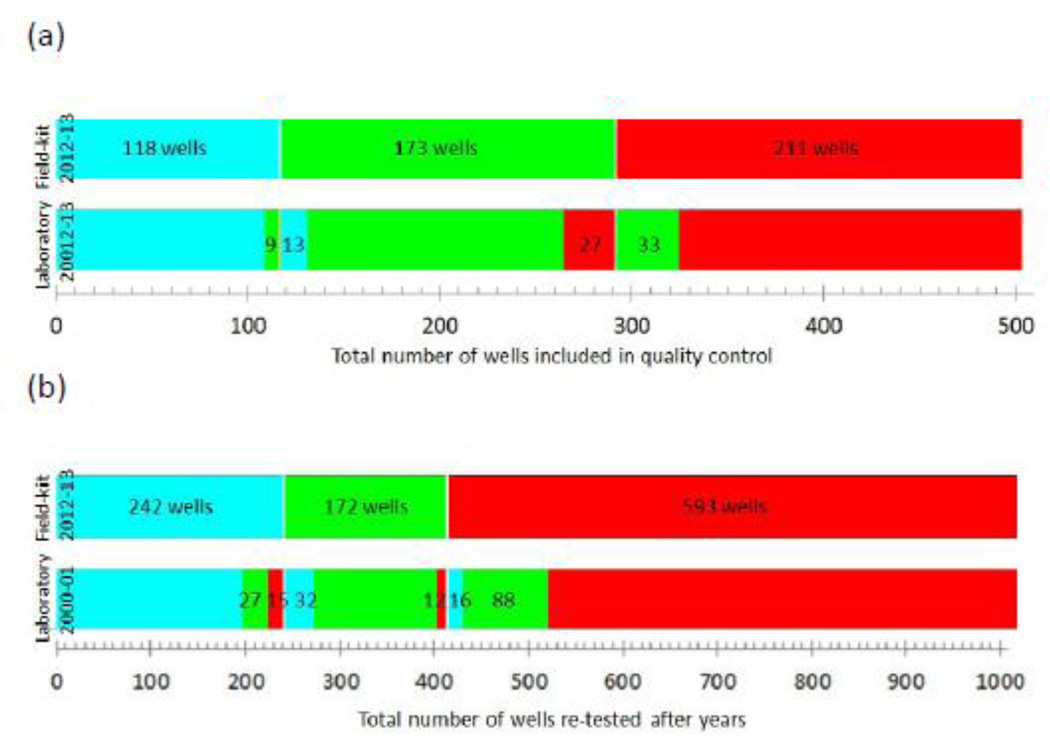
Blue placards were attached to 118 pumpheads out of the total of 502 wells sampled for quality control in 2012–13. The laboratory measurements confirm that all but 9 of the 118 wells met the WHO guideline of 10 µg/L for As in drinking water (Fig. 5a). Green placards were attached to 173 wells and, for this subset, laboratory measurements indicate that all but 27 wells did not meet the Bangladesh standard of 50 µg/L. Red placards were attached to the remaining 211 wells, even though a subset of 33 should have been labeled green instead. Overall, there were a total of 82 (16%) inconsistencies out of the 502 pairs of field-kit and laboratory measurements relative to the WHO guideline and the national standard. However, not a single well that should have been labeled red was labeled blue and, vice-versa, not one well that should have been labeled blue was labeled red.
Figure 5.
Bar graphs comparing well status for: (a) quality-control samples based on field-kit testing and, within each of the 3 status categories, laboratory measurements in 2012–13. The proportion of wells for which laboratory measurements contradict the field-kit testing is indicated by a switch in color on either side of the transitions. (b) laboratory analysis of samples collected in 2000–01 and laboratory analysis of samples collected from wells with placards still attached to the pumphead in 2012–13. The proportion of discrepancies between the two measurements are again indicated by a switch in color on either side of the transitions.
Concentrations of As measured in the laboratory ranged 11–28 µg/L for the 9 wells that should have been labeled green instead of blue and 1–9.8 µg/L for an additional 13 wells that should have been labeled blue instead of green (Fig. 5a). Concentrations of As measured in the laboratory ranged 50.5–113 µg/L for the 27 wells that should have been labeled red instead of green and 17–49.9 µg/L for and additional 33 wells that should have been labeled green instead of red. Given the accuracy of the HR ICP-MS measurements, most but not all the inconsistencies are attributable to limitations of the chemistry of the kit and/or handling and visual perception of the testers. A third of the discrepancies between field and laboratory measurements (27 out of 502 wells analyzed both ways, i.e. 5%) led to a misclassification that underestimated exposure relative to the Bangladesh standard. Given that South and Southeast Asian countries should eventually also target the WHO guideline, it is worth pointing out that the kit underestimated the exposure relative to 10 µg/L for only 9 (2%) out of 502 wells analyzed.
Comparison between the two surveys
The field-kit testing conducted in 2012–13 did not change the status of wells relative to the Bangladesh standard of 876 (87%) out of 1,007 wells with a placard based on laboratory measurements for samples collected in 2000–01 still attached to the pumphead. Within the subset of 131 wells whose status did change, 104 were converted from safe (16 originally with <10 µg/L and 88 with 10–50 µg/L) to unsafe and 27 from unsafe to safe (15 now with <10 µg/L and 12 with 10–50 µg/L) (Fig. 5b). The latitudes or longitudes recorded in 2000–01 and 2012–13 differed by more than 0.01 degree (~1 km) for a subset of the 20 pumpheads with a placard still attached. The results for 14 of these wells (i.e. 70%) are inconsistent between laboratory analysis of samples collected in 2000–01 and field-kit testing in 2012–13. The installation year recorded for 196 of the 1,007 for which the placards with 2000–01 results were still attached ranged between 2002 and 2012. For this subset, the results for 47 wells (i.e. 24%) are inconsistent between the two surveys. The higher proportion of inconsistencies for these two subsets suggests that a considerable number of pumpheads were probably re-mounted on a new well between 2005 and 2012 while their placard remained attached. The overall agreement between the two sets of measurements is therefore probably better than indicated by the comparison based on the entire set of 1,007 wells with placards still attached. Given the uncertainties of well identification, the higher proportion of wells whose status changed from safe to unsafe compared to wells whose status changed from unsafe to safe should probably not be a source of concern.
Discussion
Well turnover
A simple model of well installation and abandonment applied to the evolution of the cumulative number of wells quantifies the two processes. After trying other formulations, the rate of well installations was assumed to increase by a fixed number each year and the rate of well abandonment was assumed to be proportional to well age. According to this model, a growing batch of new wells is added to the stock of wells each year starting in 1980 while a reduction in the number of older wells is compounded. The model comes closest to matching the cumulative well data for 2000–01 and 2012–13 with an annual increase in the installation rate of 42 wells/year starting in 1980 and a 7% loss from a cohort of wells as it ages by one year (Fig. 3b). The two parameters were obtained by minimizing the sum of square residuals between observed and predicted cumulative well counts in 1981–1999 for the 2000–01 survey and 1981–2011 for the 20012–2013 survey. The actual year of the surveys was not included in the residual calculation because a significant number of wells were probably installed after the testers swept through the village during those surveys. The simple model predicts the broad trends in the apparent number of wells installed each year inferred from the two surveys, even if the field observations show more variability (Fig. 3a).
By setting the loss rate to zero, the same model can calculate the number of wells that were actually installed each year. This amounts to 8,800 rather than the 5,560 wells that were counted in 2000–01 and 21,000 instead of the 10,879 counted in 2012–13 (Fig. 3b). With the loss term set to zero, the distribution of well ages is identical for the overlapping time span of the two surveys. The model indicates that only 42% of the wells tested in 2012–13 had been tested in 2000–01. Taking into account that only 62% of the placards manufactured on the basis of the 2000–01 testing could be placed on a well in 2005 (Opar et al., 2007), this partly explains why only 1,007 metal placards out of the total of 5,560 that were attached to pumpheads during the first round of test results were found again. As in the original 2000–01 survey, close to half the wells with placards still attached in 2012–13 met the Bangladesh standard for As in drinking water. This means that unsafe wells were not preferentially abandoned during the previous decade.
Limited change in well status over time
The overall consistency of the data for wells with placards still attached indicates that concentrations of As in well water of Araihazar did not change dramatically in one direction or the other over a 12-year period. This is a significant observation and contrasts with suggestions that As concentrations might have increased over time elsewhere in the Bengal basin (Chakraborti et al., 2001; Mukherjee et al. 2011). The new data do not rule out that As concentrations can increase or decrease gradually in a subset of wells, as reported elsewhere, especially at geological transitions where the groundwater flow has been modified by groundwater pumping (McArthur et al., 2010). A small subset of wells could also have been affected over time by leakage through disconnected or broken PVC pipe (van Geen et al., 2007). Such failures might explain why small but statistically significant increases in As concentrations with well age have been documented across Bangladesh and in Araihazar (Burgess et al., 2000; van Geen et al., 2003; McArthur et al. 2004). On the basis of the new field-kit data, a linear regression of the new field-kit results as a function of well age yields a small increase of 12±2 µg/L (1-sigma) in As concentration per decade across all depths. The comparison of wells with placards still attached primarily indicates, however, that the distribution of As in groundwater is generally stable. The stability of groundwater As concentrations is consistent with the presence of a large pool of exchangeable As at the surface of aquifer particles (Fendorf et al., 2010).
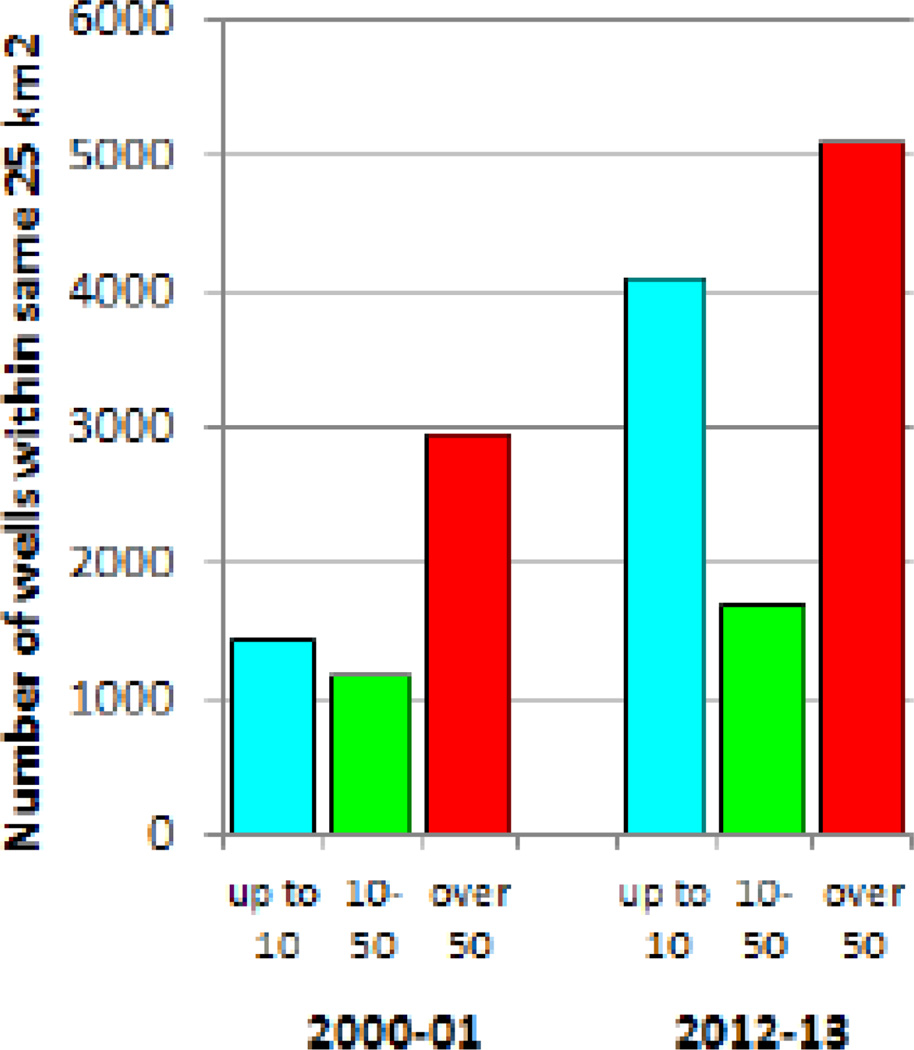
Broadly stable As concentrations means that differences in the proportion of wells of different status between the two surveys reflect primarily the combined effects of well installations and well abandonment. Unfortunately, the proportion of wells with more than 50 µg/L As within the study area declined only from 53% to 47% in 12 years (Fig. 6). Over the same period, however, the proportion of wells meeting the WHO guideline of 10 µg/L grew from 26% to 38%. The number of wells containing >10–50 µg/L As also increased over 12 years, but not by nearly as much as wells with either lower or higher As concentrations. Even if low-As aquifers are within reach of private drillers within many of the villages of Araihazar, and at least some of the drillers were aware of this, the information was evidently not taken into account by thousands of households deciding to what depth to install their new wells between 2002 and 2012 (van Geen et al., 2006; von Brömssen et al., 2007).
Figure 6.
Bar graphs comparing the proportion of wells according to their status in the same 61 villages of the study area in 2000–01 and 2012–13.
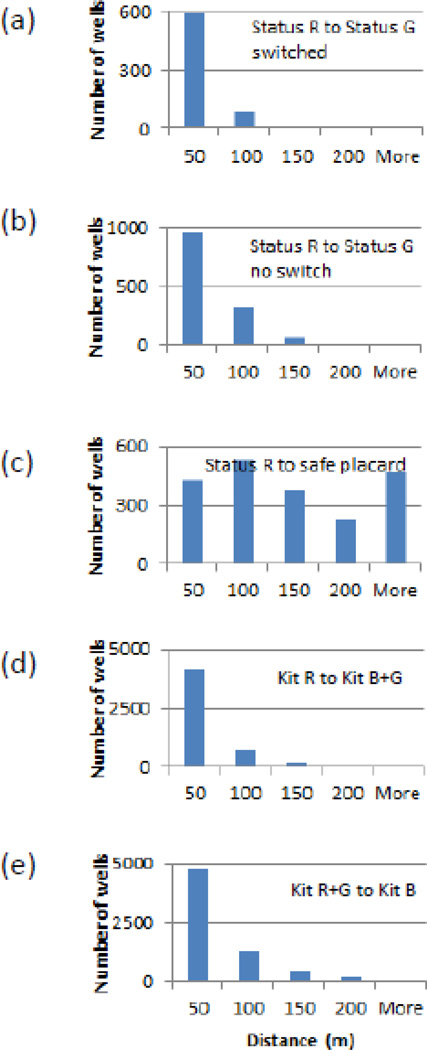
Implications for well-switching
Previous testing in Araihazar and elsewhere has reduced As exposure by well-switching, as self-reported by households (Ahmed et al., 2006; Opar et al, 2007; Madajewicz et al., 2007; Bennear et al., 2013; Inauen et al., 2013) and quantified directly by monitoring urinary As levels (Chen et al., 2007; George et al., 2012c). The 2012–13 survey shows that only 34% of the 2,041 households within the study area that knew that their well is unsafe did not drink the water or use it for cooking (Fig. 4). This is at the low end of the 30~60% range of well-switching reported previously, albeit in most cases within a few months of delivering the well status information. The new observations confirm that distance to the nearest well perceived to be safe was a determinant of switching, although clearly not the only one. Before testing, the average distance to the nearest well perceived to be safe in 2012–13 of 30±23 m (1-sigma) for switchers was somewhat lower than for non-switchers of 41±30 m. Perhaps more tellingly, 98% of switching households lived within 100 m of a well perceived to be safe whereas 84% of non-switchers did (Fig. 7a, b). The impact of insufficient testing is underlined by the fact that the distance from wells known to be unsafe to the nearest safe well with a placard was less than 100 m for only 47% of the households believing their well to be unsafe before the testing (Fig. 7c).
Figure 7.
Histograms of distances from an unsafe or red well to the nearest safe or green/blue well within the study area: (a) and (b) compare households that drink from a well that they perceive as unsafe to households that do not. (c) compares households that drink from a well that they perceive as unsafe to the nearest safe well with a placard still attached to the pumphead. (d) compares the distribution of distances for wells labeled red in 2012–13 to the nearest well labeled green or blue. (e) compares the distribution of distances for wells labeled red or green to the nearest well labeled blue
Households reporting to know the status of their well were in most cases correct according to the field-kit testing carried out in 2012–13. The As content of 85% of the 3,186 wells identified as safe indeed met the Bangladesh standard of 50 µg/L (Fig. 4). The consistency is even higher for wells identified as unsafe with 97% indeed containing over 50 µg/L As. For the 5,657 wells of unknown status, the proportion meeting the Bangladesh standard for As is only 53%. The growing number of wells that, according to their distribution of ages (Fig. 3), continue to be installed are typically not tested and therefore a major cause of unwitting exposure to As. A significant reduction in exposure is expected now that the status of the vast majority of wells in the study area is known and that 96% of all households with an unsafe well live within 100 m of a safe well (Fig. 7d). Households with a well labeled green were also encouraged during the latest round of testing to switch whenever possible to a well with a blue placard that meets to WHO guideline for As. Using this more stringent criterion, 90% of households with a well labeled red or green still live within 100 m of blue well (Fig. 7e). In Araihazar at least, the impact of reducing the national standard of 50 µg/L to the WHO guideline of 10 µg/L would therefore not be dramatic with respect to access to safe wells. Without reinforcement, however, the proportion of switching may not reach the two-thirds achieved in the past in Araihazar and elsewhere in Bangladesh.
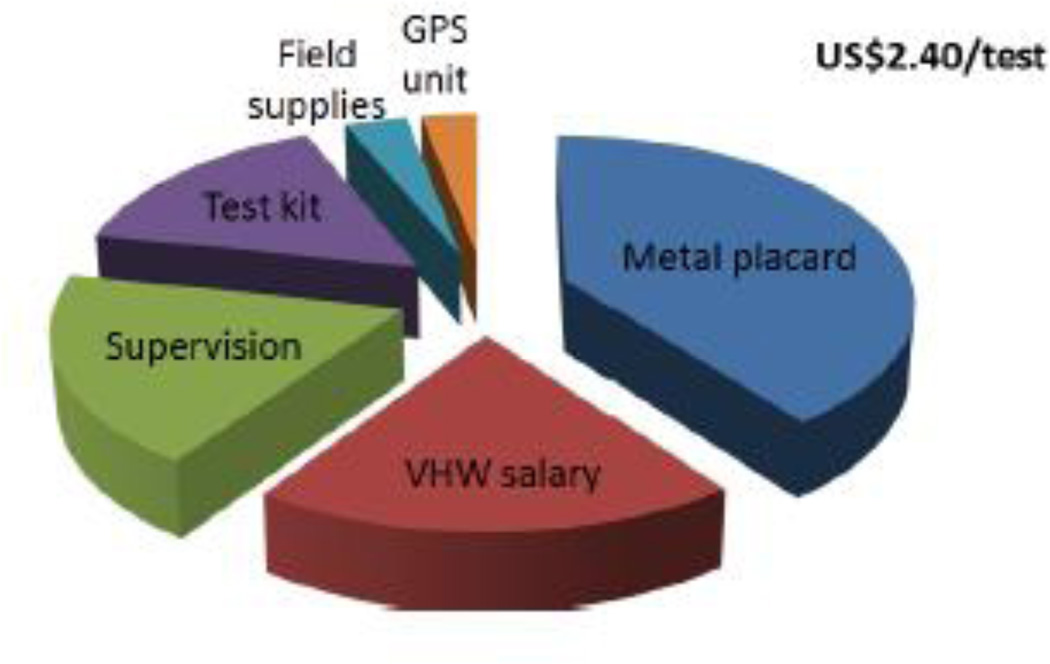
Cost of testing relative to well installations
Our data show that households within the Araihazar study area spent approximately US$1.5M over 12 years to install 15,000 wells over a period of 12 years, assuming an average cost of US$100 for a typical 100-ft deep well. The steady increase in installations before and after the 2000–01 campaign suggests that they were motivated primarily by factors other than concern about As exposure. The proportion of safe and unsafe wells relative to the Bangladesh standard of 50 µg/L indeed barely changed despite the new installations (Fig. 6). This represents an enormous missed opportunity because safe aquifers can be targeted at depths of 200–300 ft reachable by local drilling teams in many of the villages of Araihazar and elsewhere in Bangladesh (van Geen et al., 2006; von Brömssen et al., 2007). The lack of a mechanism for providing safe-depth information each time a household decides to install a new well and testing it afterwards may be one reason that prevents more widespread targeting of low-As aquifers.
Compared to the cost of a new well, the cost of field-kit testing of US$2.30/test during the 2012–13 survey was modest. This figure includes the cost of the kit itself (US$90 for 300 tests with a volume discount), the GPS units ($150 ea.), and the wages of the 10 testers and their two full-time supervisors (Fig. 8). As a quality-controlled, fee-based service, the provision of safe-depth information could therefore potentially be tied to the testing of a new well soon after it has been installed to verify that the driller was successful. This would only slightly raise the total cost of installing a well to a household while increasing the chances that a well produces low-As water. In those villages where a deeper aquifer that is consistently low in As is beyond the 300-ft maximum reach of local drilling teams (van Geen et al. 2003; 2007), deeper community wells with different technology by the government’s Department of Public Health Engineering will still be needed.
Figure 8.
Relative contribution of various components to the total cost of field-kit testing in Araihazar during 2012–13 about US$2.40 per test.
Conclusion
Exposure to As by drinking tubewell water remains high in Araihazar in 2012–13 even after two blanket testing campaigns carried out in 2000–01 and 2003 and despite enrolment for over a decade of a substantial fraction of the local population in a cohort study. Enrolled households have been reminded at least every two years of the health risks of continued exposure during a medical exam and the collection of a urine sample. The main reason for continued exposure is therefore probably not lack of awareness but the lack of an identified alternative source of drinking water. Before the recent testing campaign, the highest proportion of households in Araihazar that were drinking from a high-As well were not aware of its status. Households that knowingly drink from an unsafe well may also do so at least in part because they are not aware of a nearby well that is safe. Until the recent testing, only one out of ten wells in Araihazar still had a plate attached to its pumphead indicating that is was safe to drink from. A final indication of the need for testing is that a substantial number of households were drinking from an unsafe well under the wrong impression that it was safe.
A different approach (e.g. DPHE/UNICEF, 2011; George et al., 2013) is clearly needed to promote the testing of wells that continue to be installed not only in Araihazar but throughout Bangladesh and a halfdozen neighboring countries where groundwater can also be high in As. One possibility may be to tie testing with the decision to install a new well by disseminating at the village level the information that is available for targeting a local low-As aquifer. The technology needed to test wells reliably and provide quality control, field kits, handheld GPS units, or smart phones, is available. What is missing is a viable organizational structure with an incentive at the local level to seek untested wells and promote the installation of safe wells.
Highlights.
10,879 wells were tested in 2012–13 with a field-kit in 61 villages of Bangladesh tested in 2000–01
Well ages indicate a significant turnover due to new well installations and well abandonment
Two-thirds of tubewells believed to be unsafe are still used for drinking and cooking
Acknowledgments
The 2012–13 survey was supported primarily by a supplement to NIEHS Superfund Research Program grant P42 ES010349. We are grateful to our indefatigable team of testers which included Nazmun Nahar, Sarmin Akter, Rehana Akter, Moriom Akter, Akhi Akter, Maria Akter, Sanjida Akter, Nasrin Akter, Mahamuda Akter, Salma Akter as well field co-supervisor Md. Zakir Hossain.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahmed MF, Ahuja S, Alauddin M, Hug SJ, Lloyd JR, Pfaff A, et al. Ensuring safe drinking water in Bangladesh. Science. 2006;314:1687–1688. doi: 10.1126/science.1133146. [DOI] [PubMed] [Google Scholar]
- BGS/DPHE (British Geological Survey, Dept. of Public Health Engineering) Arsenic Contamination of Groundwater in Bangladesh, Final Report (British Geological Survey. 2001 [Google Scholar]
- Bennear L, Tarozzi A, Pfaff A, Soumya HB, Ahmed KM, van Geen A. Impact of a randomized controlled trial in arsenic risk communication on household water supply choices in Bangladesh. Journal of Environmental Economics and Management. 2013;65:225–240. doi: 10.1016/j.jeem.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess WG, Burren M, Perrin J, Ahmed KM. Constraints on sustainable development of arsenic-bearing aquifers in southern Bangladesh. part 1: A conceptual model of arsenic in the aquifer, in Sustainable Groundwater Development edited by K. M. Hiscock, M. O. Rivett, and R M. Davidson. Geol. Soc. London Spec. Publ. 2000;193:145–163. [Google Scholar]
- Chakraborti D, Basu GK, Biswas BK, Chowdhury UK, Rahman MM, Paul K, et al. Characterization of arsenic bearing sediments in Gangetic Delta of West Bengal India. In: Chappell WR, Abernathy CO, Calderon RL, editors. In Arsenic Exposure and Health Effects. New York: Elsevier Science; 2001. pp. 27–52. [Google Scholar]
- Chakraborti D, Mukherjee SC, Pati S, Sengupta MK, Rahman MM, Chowdhury UK, Lodh D, Chanda CR, Chakraborti AK, Basu GK. Arsenic groundwater contamination in Middle Ganga Plain, Bihar, India: A future danger? Environmental Health Perspectives. 2003;111:1194–1201. doi: 10.1289/ehp.5966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, van Geen A, Graziano J, Pfaff A, Madajewicz M, Parvez F, et al. Reduction in urinary arsenic levels in response to arsenic mitigation in Araihazar, Bangladesh. Environmental Health Perspectives. 2007;115:917–923. doi: 10.1289/ehp.9833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Graziano JH, Parvez F, Liu M, Slavkovich V, Kalra T, et al. Arsenic exposure from drinking water and cardiovascular disease mortality: A prospective cohort study in Bangladesh. British Medical Journal. 2011;342:d243. doi: 10.1136/bmj.d2431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Z, Zheng Y, Mortlock R, van Geen A. Rapid multi-element analysis of groundwater by highresolution inductively coupled plasma mass spectrometry. Analytical and Bioanalytical Chemistry. 2004;379:513–518. doi: 10.1007/s00216-004-2618-x. [DOI] [PubMed] [Google Scholar]
- DPHE/UNICEF. Horizontal Learning Program Learning Note: Pay-for-Use Testing, Marking & Switching of Wells. 2011 [Google Scholar]
- Fendorf S, Michael H, van Geen A. Spatial and temporal variations of groundwater arsenic in South and Southeast Asia. Science. 2010;328:1123–1127. doi: 10.1126/science.1172974. [DOI] [PubMed] [Google Scholar]
- Flanagan SV, Johnston RB, Zheng Y. Arsenic in tube well water in Bangladesh: health and economic impacts and implications for arsenic mitigation. Bull WHO. 2012;90:839–846. doi: 10.2471/BLT.11.101253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George CM, Graziano JH, Mey JL, van Geen A. Impact on arsenic exposure of a growing proportion of untested wells in Bangladesh. Environmental Health. 2012a;11:7. doi: 10.1186/1476-069X-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George CM, Zheng Y, Graziano JH, Rasul SB, Mey JL, van Geen A. Evaluation of an arsenic test kit for rapid well screening in Bangladesh. Environmental Science and Technology. 2012b;46:11213–11219. doi: 10.1021/es300253p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George CM, van Geen A, Slavkovich V, Singha A, Levy D, Islam T, et al. A cluster-based randomized controlled trial promoting community participation in arsenic mitigation efforts in Bangladesh. Environmental Health. 2012c;11:41. doi: 10.1186/1476-069X-11-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George CM, Inauen J, Rahman SM, Zheng Y. The effectiveness of educational interventions to enhance the adoption of fee-based arsenic testing in Bangladesh: A cluster randomized controlled trial. Am. J. Trop. Med. Hyg. 2013;89:138–144. doi: 10.4269/ajtmh.12-0664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inauen J, Hossain MM, Johnston RB, Mosler HJ. Acceptance and use of eight arsenic-safe drinking water options in Bangladesh. PLoS ONE. 2013;8:e53640. doi: 10.1371/journal.pone.0053640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakariya M, Vahter M, Rahman M, Wahed MA, Hore SK, Bhattacharya P, Jacks G, Persson LA. Screening of arsenic in tubewell water with field test kits: Evaluation of the method from public health perspective. Science of the Total Environment. 2007;379:167–175. doi: 10.1016/j.scitotenv.2006.11.053. [DOI] [PubMed] [Google Scholar]
- DPHE/JICA (Dept. of Public Health Engineering, Bangladesh, Japan International Cooperation Agency) Report on Situation Analysis of Arsenic Mitigation, 2009 (Local Government Division, Government of Bangladesh, DPHE, JICA. 2010
- Madajewicz M, Pfaff A, van Geen A, Graziano J, Hussein I, Momotaj H, et al. Can information alone both improve awareness and change behavior? Response to arsenic contamination of groundwater in Bangladesh. Journal of Development Economics. 2007;84:731–754. [Google Scholar]
- McArthur JM, Banerjee DM, Hudson-Edwards KA, Mishra R, Purohit R, Ravenscroft P, et al. Natural organic matter in sedimentary basins and its relation to arsenic in anoxic ground water: the example of West Bengal and its worldwide implications. Appl Geochem. 2004;19:1255–1293. [Google Scholar]
- McArthur JM, Banerjee DM, Sengupta S, Ravenscroft P, Klump S, Sarkar A, et al. Migration of As, and 3H/3He ages, in groundwater from West Bengal: Implications for monitoring. Water Research. 2010;44:4171–4185. doi: 10.1016/j.watres.2010.05.010. [DOI] [PubMed] [Google Scholar]
- Mukherjee A, Fryar AE, Scanlon BR, Bhattacharya P, Bhattacharya A. Elevated arsenic in deeper groundwater of the western Bengal basin, India: Extent and controls from regional to local scale. Appl Geochem. 2011;26:600–613. [Google Scholar]
- Nickson R, Sengupta C, Mitrai P, Fave SN, Banerjee AK, Bhattacharya A, et al. Current knowledge on the distribution of arsenic in groundwater in five states of India. Journal of Environmental Science and Health Part A. 2007;42:1707–1718. doi: 10.1080/10934520701564194. [DOI] [PubMed] [Google Scholar]
- Opar A, Pfaff A, Seddique AA, Ahmed KM, Graziano JH, van Geen A. Responses of 6500 households to arsenic mitigation in Araihazar, Bangladesh. Health & Place. 2007;13:164–172. doi: 10.1016/j.healthplace.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Parvez F, Wasserman GA, Factor-Litvak P, Liu X, Slavkovich V, Siddique AB, et al. Arsenic exposure and motor function among children in Bangladesh. Environmental Health Perspectives. 2011;119:1665–1670. doi: 10.1289/ehp.1103548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitt M, Rosenzweig MR, Hassan N. Identifying the hidden costs of a public health success: Arsenic well water contamination and productivity in Bangladesh, PSTC Working Paper Series 2012-02. http://brown.edu/academics/population-studies/sites/brown.edu.academics.population-studies/files/uploads/2012-02-PSTC-Working-Paper.pdf. [Google Scholar]
- Rahman A, Persson LA, Nermell B, Arifeen SE, Ekstrom EC, Smith AH, et al. Arsenic exposure and risk of spontaneous abortion, stillbirth, and infant mortality. Epidemiology. 2010;21:797–804. doi: 10.1097/EDE.0b013e3181f56a0d. [DOI] [PubMed] [Google Scholar]
- Ravenscroft P, Brammer H, Richards K. Arsenic Pollution: A Global Synthesis (RGS-IBG Book Series. Chichester, UK: Wiley-Blackwell; 2009. [Google Scholar]
- Smith AH, Lingas EO, Rahman M. Contamination of drinking-water by arsenic in Bangladesh: a public health emergency. Bulletin of the World Health Organization. 2000;78:1093–1103. [PMC free article] [PubMed] [Google Scholar]
- van Geen A, Ahsan H, Horneman AH, Dhar RK, Zheng Y, Hussain I, et al. Promotion of well-switching to mitigate the current arsenic crisis in Bangladesh. Bulletin of the World Health Organization. 2002;81:732–737. [PMC free article] [PubMed] [Google Scholar]
- van Geen A, Ahmed KM, Seddique AA, Shamsudduha M. Community wells to mitigate the current arsenic crisis in Bangladesh. Bulletin of the World Health Organization. 2003;82:632–638. [PMC free article] [PubMed] [Google Scholar]
- van Geen A, Zheng Y, Versteeg R, Stute M, Horneman A, Dhar R, et al. Spatial variability of arsenic in 6000 tube wells in a 25 km2 area of Bangladesh. Water Resources Research. 2003;39:1140. [Google Scholar]
- van Geen A, Cheng Z, Seddique AA, Hoque MA, Gelman A, Graziano JH, et al. Reliability of a commercial kit to test groundwater for arsenic in Bangladesh. Environmental Science and Technology. 2005;39:299–303. [PubMed] [Google Scholar]
- van Geen A, Trevisani M, Immel J, Jakariya M, Osman N, Cheng Z, et al. Targeting low-arsenic groundwater with mobile-phone technology in Araihazar. J. Health Population and Nutrition. 2006;24:282–297. [PMC free article] [PubMed] [Google Scholar]
- van Geen A, Cheng Z, Jia Q, Seddique AA, Rahman MW, Rahman MM, et al. Monitoring 51 deep community wells in Araihazar, Bangladesh, for up to 5 years: Implications for arsenic mitigation. Journal of Environmental Science and Health Part A. 2007;42:1729–1740. doi: 10.1080/10934520701564236. [DOI] [PubMed] [Google Scholar]
- von Brömssen M, Jakariya M, Bhattacharya P, Ahmed KM, Hasan MA, Sracek O, Jonsson L, Lundell L, Jacks G. Targeting low-arsenic aquifers in Matlab Upazila, Southeastern Bangladesh. Science of the Total Environment. 2007;379:121–132. doi: 10.1016/j.scitotenv.2006.06.028. [DOI] [PubMed] [Google Scholar]
- WASH Research Team. WASH programme of BRAC: Towards attaining the MDG targets: Baseline findings. Dhaka, Bangladesh: BRAC; 2008. [Google Scholar]
- Wasserman GA, Liu X, Parvez F, Ahsan H, Levy D, Factor-Litvak P, et al. Arsenic and manganese exposure and children’s intellectual function. NeuroToxicology. 2011;32:450–457. doi: 10.1016/j.neuro.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]