Abstract
Background & Aims
The contribution of humoral immune responses to spontaneous control of Hepatitis C virus (HCV) infection remains unclear. We assessed nAb responses during acute HCV infection to determine whether infection outcome is associated with the neutralizing antibody (nAb) response, specifically its timing or breadth (neutralization of multiple genotype-matched variants).
Methods
A representative genotype 1 HCV pseudoparticle (HCVpp) library, consisting of 19 genetically-distinct genotype 1 HCVpp that comprise the natural variability of genotype 1 E1E2 sequences, was used to assess anti-genotype 1 nAb responses during acute infection in at-risk persons followed prospectively. Neutralization of individual library HCVpp by the last viremic plasma sample obtained before clearance was compared to either one-year post-initial viremia or clearance time-matched specimens obtained from subjects developing persistent infection.
Results
In persistently infected persons nAb responses were delayed then progressively broadened whereas in persons who controlled viremia broader responses were detected early and contracted after clearance of viremia. Surprisingly, the breadth of anti-genotype 1 nAb responses was not dependent upon subjects’ infection genotype. Also, individual library HCVpp neutralization sensitivity was not associated with any known E2 sequence determinants. Interestingly, two single nucleotide polymorphisms in the HLA-DQ locus were associated with nAb breadth.
Conclusions
Taken together, these data demonstrate that control of HCV infection is associated with more rapid development of a broad nAb response, independent of the infection viral genotype, providing further evidence for the role of nAb in controlling HCV infection and the potential benefit of generating broad anti-HCV nAb responses by vaccination.
Keywords: neutralizing antibody, HCV infection outcome, acute infection
A hepatitis C virus (HCV) vaccine that prevents infection remains elusive. Identification of immunological mechanisms of spontaneous resolution of HCV infection may inform rational vaccination strategies. While a broad and potent cellular immune response has been demonstrated to play an important role in spontaneous control of HCV infection, the contribution of humoral immune responses to spontaneous control of HCV infection remains unclear. Prior experimental evidence suggests that humoral immunity, specifically neutralizing antibodies (nAb), contributes to an effective immune response to HCV infection. Control of HCV infection was associated with an increased incidence and potency of nAb responses during the first six months of infection(1) and the presence of nAb has been shown to drive HCV envelope sequence evolution during acute infection(2) (3).
One of the obstacles to investigating the role of nAbs in HCV infection outcome is that the unique global and intrapersonal sequence variability of HCV complicates selection of a representative sequence to use in studies. Seven genotypes of HCV have been identified with extensive inter- and intragenotype envelope amino acid sequence diversity (up to 50% and 20%, respectively)(4). Additionally, each HCV infection comprises a quasispecies of HCV sequences consisting of genetically-distinct yet related sequences driven by immune selection and restricted by fitness constraints(3, 5). nAb studies using a single isolate may underestimate the incidence or magnitude of nAb responses due to this high level of sequence diversity.
We have begun to address this issue by constructing a novel library of HCV pseudoparticles (HCVpp) expressing 19 genetically-distinct, genotype 1, HCV envelope glycoproteins derived from primary human isolates. This library models the natural envelope sequence variability of the most prevalent and incident subtypes of genotype 1(6) and was used to analyze the breadth (capacity to neutralize multiple isolates of a single genotype) of nAb responses in individuals with HCV infection. We used this model to study nAb responses in a cohort of persons with acute HCV infection. We demonstrated that earlier appearance of broader nAb responses was associated with spontaneous control of HCV infection compared to individuals who progress to persistent infection, independent of infection genotype. Interestingly, we found that the neutralization sensitivity of library HCVpp was not associated with any known E2 sequence determinants and two single nucleotide polymorphisms (SNP) in the HLA-DQ locus were associated with nAb breadth. Taken together, these data demonstrate that control of HCV infection is associated with more rapid development of a broad nAb response, providing further evidence for the role of nAb in control of HCV infection.
Methods
Subject selection
Subjects were selected from the Baltimore Before and After Acute Study of Hepatitis (BBAASH) in which the incidence, immunology and virology of HCV infection in young injection drug users is prospectively monitored, as previously described(7). The study was approved by the Institutional Review Board at the Johns Hopkins School of Medicine(7).
Determination of infection outcome
Subjects were assigned to Clearance and Persistence groups based on infection outcome. Clearance was defined as undetectable HCV RNA assessed by the COBAS Taqman RT-PCR quantitative assay for a period of at least 60 days in individuals with detectable anti-HCV antibodies in the setting of incident infection. Persistence was defined as viremia for more than one year with the same virus as determined by Core-E1 phylogenetic analysis(8). The midpoint between sample collection dates was used to estimate date of onset and resolution of viremia. Clearance and Persistence subject samples were selected using two sets of selection criteria, one-year and time-matched.
Specimen selection
One-year analysis
Plasma samples at 365 days (± 60 days) post-detection of initial viremia were selected for analysis. For HCV infections that were controlled in less than 365 days, the last sample in which viremia was detectable (± 60 days) was selected for analysis.
Time-matched analysis
Persistence and Clearance subjects were randomized and two Persistence subjects were matched with one clearance subject based on rank order. For Clearance subjects, the last viremic specimen (viremia duration less than 365 days) or a specimen obtained at 365 days (± 60 days) post-initial viremia detection was selected for analysis of neutralization. Persistence subject visits were selected by matching viremia duration (± 60 days) to the Clearance subject.
Genotype 1 HCVpp library
Source of E1E2 genes
Plasma samples obtained from HCV infected subjects in the BBAASH cohort(7), Irish Anti-D cohort(9), and Swan Project(10) were used to construct a library of genotype 1 E1E2-expressing lentiviral pseudoparticles using a high-throughput production and screening approach.
HCV E1E2 expression plasmids
The E1E2 region was PCR amplified from cDNA reverse transcribed from viral RNA purified from subject plasma and cloned into the expression vector pcDNA3.2/V5/Dest (Invitrogen, USA) using Gateway technology in a one-tube BP/LR reaction. Details are described in Supplementary Methods.
High-throughput HCVpp production and infectivity screening
HCVpp were produced from purified cDNA clones by lipofectamine-mediated transfection of HCV E1E2 and pNL4-3.Luc.R-E- plasmids into HEK293T cells in a 96-well plate as described in Supplementary Methods.
Selection of HCVpp for inclusion in library
Infectious constructs were sequenced, aligned using ClustalX(11), and a neighbor-joining amino acid phylogenetic tree with pairwise deletion was constructed using Mega. Unique infectious sequences were identified based on phylogeny and the most ancestral sequence from each clade was selected for inclusion in the library. Protein sequence divergence was determined using the Protdist Phylip program included in the BioEdit software package(12). Novel E1E2 sequences have been submitted to GenBank, accession numbers XXX through YYY.
Comparison of library and global E1E2 sequence diversity
Diversity plots were generated using VarPlot version 1.2 (described in Ray, et al(13) and available from the author (http://sray.med.som.jhmi.edu/scroftware/VarPlot)) and VisSPA v1.6 (http://sray.med.som.jhmi.edu/SCRoftware/VisSPA/).
Assessment of neutralization of library HCVpp
Library HCVpp were produced by lipofectamine-mediated transfection of E1E2 expression plasmids in HEK-293T cells as described in Supplementary Methods. Heat-inactivated plasma samples were tested for neutralization of library HCVpp at a single dilution as previously described(8), detailed in Supplementary Methods. HCVpp were tested undiluted if infectivity, in the absence of antibodies, was less than 1.5×106 relative light units (RLUs) or diluted to less than 1.5×106 RLUs with media. Positive detection of neutralizing antibodies was noted when neutralization was ≥50%.
Analysis of viral determinants of neutralization sensitivity in library HCVpp E2 sequences
Predicted N-linked glycosylation sites for each library HCVpp were determined using NetNGlyc 1.0 (http://www.cbs.dtu.dk/services/NetNGlyc/). Monoclonal antibody epitopes were determined based on previous studies(14, 15, 15–22). Epitopes that contain the same amino acid positions were counted as one (HC84.1 and HC84.2; HC84.22 and HC84.23; Fab e137 and Fab e20; AR3B and AR3D; and 95-2 and HCV1). An epitope was considered intact when the amino acid sequence matched the published sequence.
Single nucleotide polymorphism genotyping
Genomic DNA was extracted from peripheral blood mononuclear cells using the QIAamp DNA Blood Mini Kit (Qiagen Sciences, Germantown, MD). Single nucleotide polymorphisms (SNPs) were genotyped using custom TaqMan® SNP Genotyping Assays (Life Technologies, Carlsbad, CA).
Statistical Analysis
Wilcoxon rank-sum test, Wilcoxon signed rank-sum test, Kruskal-Wallis One Way ANOVA on Ranks and Fisher Exact test (where appropriate, based on descriptive statistics) were used to evaluate statistically significant differences between groups.
Results
Construction of a representative genotype 1 HCVpp library
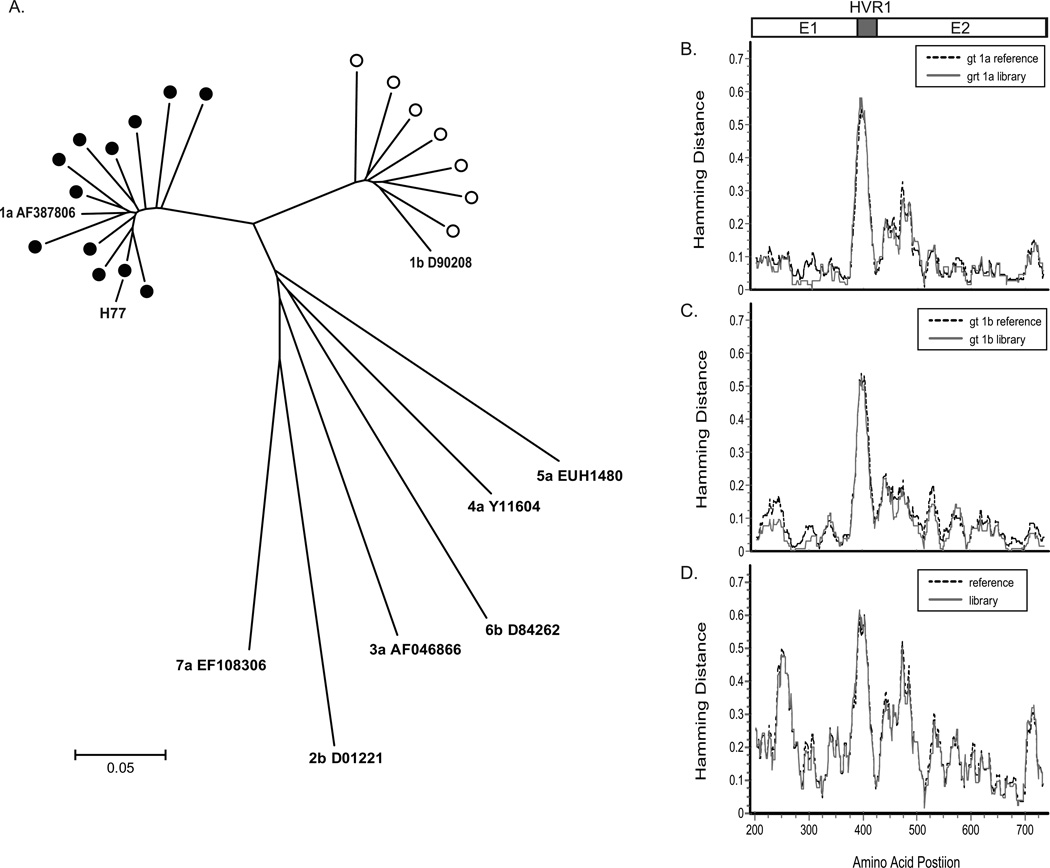
A total of 156 infectious HCVpp expressing unique E1E2 proteins (113 subtype 1a, 43 subtype 1b) derived from 33 different subjects (21 subtype 1a, 12 subtype 1b) were identified using a high-throughput production and screening approach. Phylogenetic analysis identified 12 distinct subtype 1a and 7 subtype 1b clades (Figure 1a). Amino acid distance analysis revealed median (IQR) distances of 0.14 (0.12 – 0.18) for ancestral subtype 1a HCVpp E1E2 sequences and 0.17 (0.16 – 0.19) for ancestral subtype 1b HCVpp E1E2 sequences included in the library.
Figure 1.
Representative genotype 1 HCVpp library. A) Neighbor-joining amino acid phylogenetic tree depicting amino acid diversity of distinct subtype 1a (closed circles) and subtype 1b (open circles) E1E2 sequences included in the genotype 1 HCVpp library. Reference sequences (text) were obtained from Genbank. Diversity plots depicting variability at each amino acid position of B) subtype 1a and C) subtype 1b HCVpp E1E2 sequences (grey line) compared to 374 subtype 1a or 260 subtype 1b reference sequences (black line) and D) divergence between subtype 1a and 1b reference sequences and subtype 1a and 1b library sequences. Amino acid position numbering is based on the H77 reference sequence.
In order to assess how accurately our HCVpp library represents genotype 1, we compared the E1E2 sequence diversity of the library to 374 subtype 1a and 260 subtype 1b reference sequences. The diversity profile of subtype 1a (Figure 1b, n=12) and subtype 1b (Figure 1c, n=7) HCVpp E1E2 sequences was strikingly similar to the diversity of reference sequences. Additionally, the divergence between subtype 1a and 1b reference sequences was equivalent to the divergence between subtype 1a and 1b library sequences (Figure 1d). These data strongly suggest that our genotype 1 HCVpp library accurately represents the natural diversity of E1E2 sequences.
Appearance of broad nAb responses is delayed in subjects who fail to control HCV infection
Initially, 31 subjects who developed persistent infection and 21 subjects who controlled infection were selected for analysis of nAb breadth in specimens collected during acute infection. Age, sex, race, follow-up interval, HCV infection genotype and IL28B-related rs12979860 allele frequencies were similar between these Persistence and Clearance groups (Table 1). The duration of infection in Clearance subjects was significantly shorter than Persistence subjects, since the infection duration in eight Clearance subjects was less than 230 days.
Table 1.
Demographic and HCV infection data of Clearance subjects versus Persistence subjects of One-Year and Time-Matched visits.
| One-Year Analysis | Time-Matched Analysis | ||||
|---|---|---|---|---|---|
| Clearance | Persistence | P | Persistence | P | |
| N | 21 | 31 | 42 | ||
| Age1 | 25.7 (4.3) | 26.0 (4.0) | 0.85 | 26.8 (4.8) | 0.85 |
| % Female | 52% | 30% | 0.09 | 30% | 0.09 |
| % Caucasian | 100% | 91% | 0.28 | 85% | 0.16 |
| Infection duration2 | 275 (102, 338) | 344 (336, 355) | <0.01 | 238 (116, 342) | 0.73 |
| HCV subtype (%) | 0.71 | 0.63 | |||
| 1a | 76.2 | 74.2 | 83.3 | ||
| 1b | 9.5 | 3.2 | 2.4 | ||
| 2b | 4.8 | 9.7 | 7.1 | ||
| 3a | 9.5 | 12.9 | 9.5 | ||
| IL28B genotype (%)3 | 0.165 | 0.075 | |||
| CC | 66.7 | 45.2 | 40.5 | ||
| CT | 33.3 | 41.9 | 45.2 | ||
| TT | 0.0 | 12.9 | 14.0 | ||
at seroconversion, yr, Mean (SD);
days, Median (IQR);
IL28B gene SNP rs12979860;
% CC vs % CT/TT
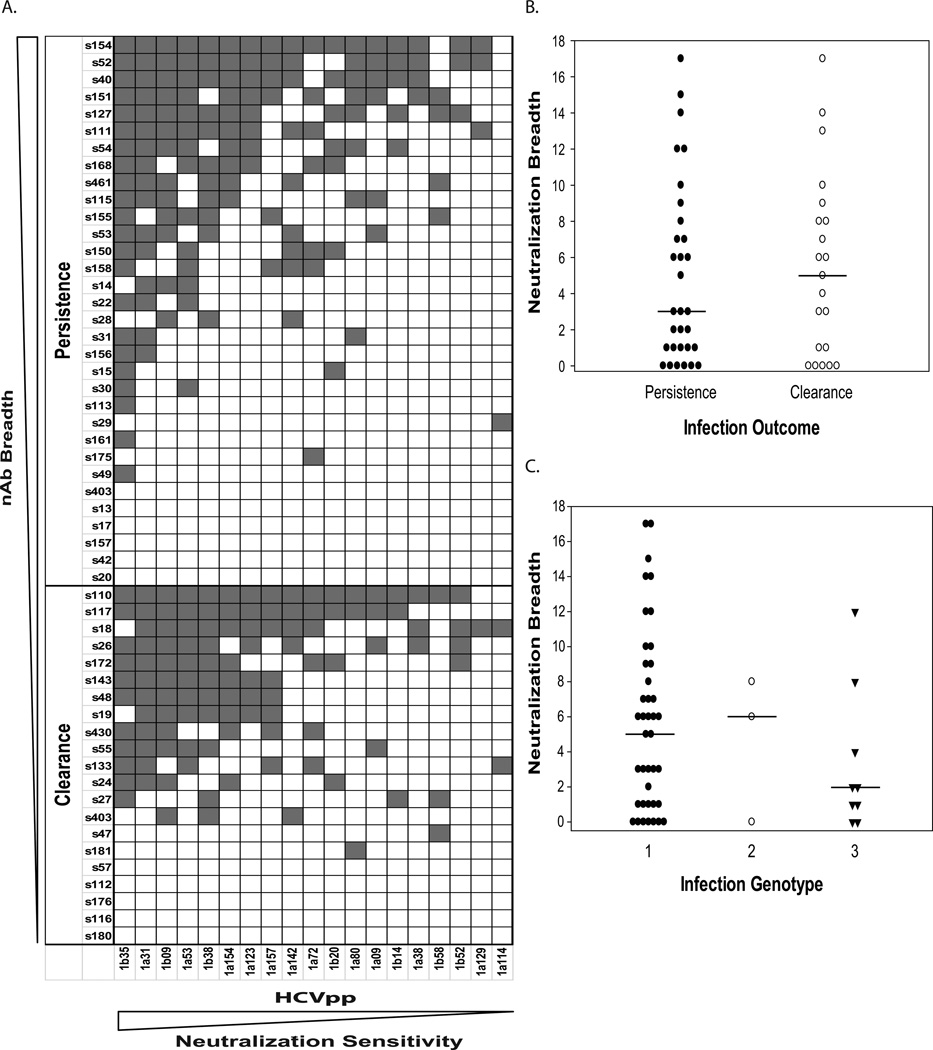
In order to examine whether the incidence and breadth of anti-genotype 1 nAb responses during acute infection is associated with infection outcome, we first compared neutralization of library HCVpp by Persistence subject plasma samples obtained one year following initial detection of to Clearance subject plasma samples obtained one year following initial detection of viremia or the last viremic sample (infection duration < one year. Neutralization of at least one HCVpp was observed in 76.2% of Clearance subjects and 80.6% of Persistence subjects (Figure 2a; P = 0.74). The median breadth of nAb responses at 12 mo of infection or last viremia (Figure 2b) in the Clearance group was similar to the median breadth of nAb responses at 12 months of infection in Persistence group (P = 0.757). However, in this analysis there was a 2-fold lower duration of infection in the Clearance group, because more than 50% of Clearance subjects experienced less than 6 months of viremia.
Figure 2.
The breadth of nAb responses was similar in Persistence subjects at one year of infection to Clearance subjects at last viremia or one year of infection. A) Heat map illustrating neutralization results against each HCVpp for Persistence and Clearance subjects. Each square represents negative (white) or positive neutralization (grey) of that particular HCVpp. HCVpp 1a154 denotes the H77 E1E2 clone included in the library. B) Breadth of anti-genotype 1 nAb responses in Persistence and Clearance subjects. Values represent the number of HCVpp neutralized by each subject. The median (line) breadth of nAb responses in Persistence subjects was similar to Clearance subjects (P = 0.757). C) Breadth of anti-genotype 1 nAb responses in subjects stratified by infection genotype. Values represent the number of HCVpp neutralized by each subject. The median breadth of nAb responses in each genotype was not different (P = 0.452).
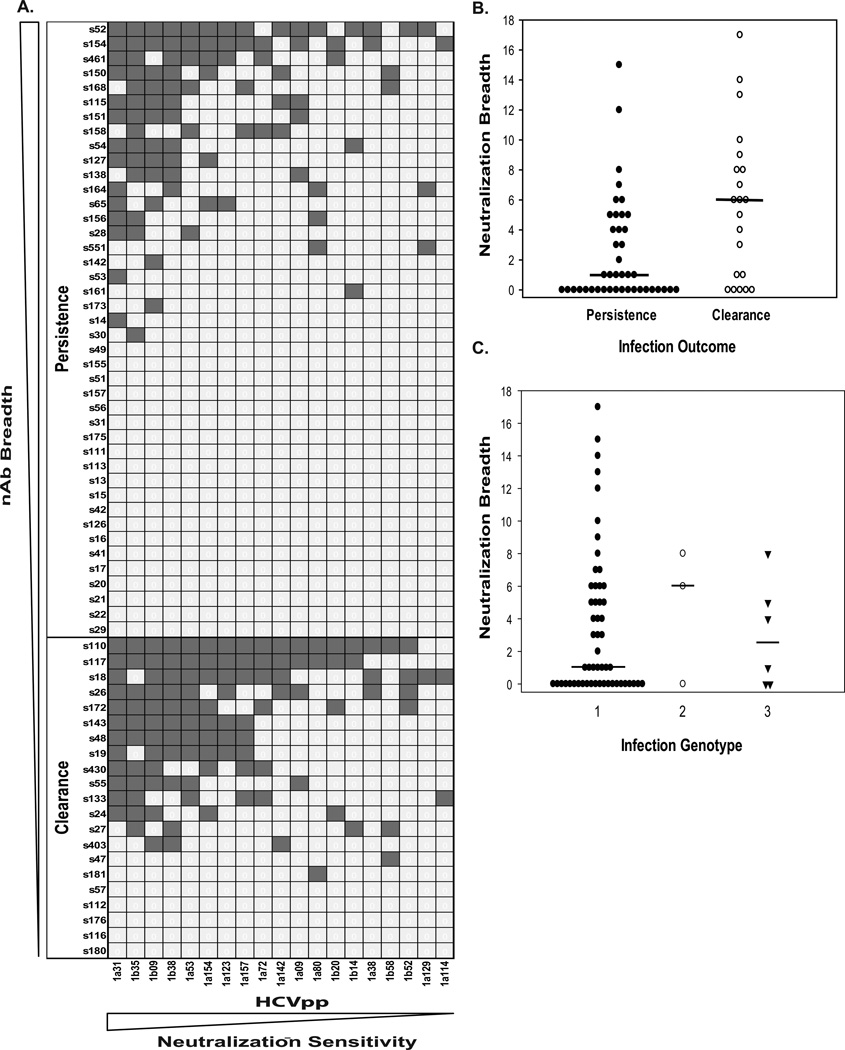
In order to control for the effect of infection duration, nAb breadth was also assessed in Clearance subjects at last viremia or one year of infection compared to time-matched Persistence subjects. Therefore, 21 Clearance subjects were matched with 42 Persistence subjects and samples from each of these Persistence subjects were time-matched based on infection duration (Table 1). As intended, the infection duration of Clearance and time-matched Persistence subjects was not different.
In this time-controlled analysis, there was a trend for a greater percentage of Clearance subjects neutralizing at least one HCVpp (76.2% versus 52.4%, P = 0.101; Figure 3a). In addition, the breadth of nAb responses was greater in Clearance subjects than in time-matched Persistence subjects (P = 0.007; Figure 3b). Taken together, these results suggest that the appearance of broad nAb responses is delayed in subjects who fail to control HCV infection. End-point plasma titers of nAb were similar between subjects with Clearance and Persistence in a subset of subjects representing the range of neutralization breadth (Supplementary Figure 3).
Figure 3.
Broader anti-genotype 1 nAb responses were observed in Clearance subjects compared to time-matched Persistence subjects. A) Heat map illustrating neutralization results against each HCVpp for Persistence and Clearance subjects. Each square represents negative (white) or positive neutralization (grey) of that HCVpp. HCVpp 1a154 denotes the H77 E1E2 clone included in the library. B) Breadth of anti-genotype 1 nAb responses in Persistence and Clearance subjects. Values represent the number of HCVpp neutralized by each subject. The median (line) breadth of nAb responses in Clearance subjects was greater than Persistence subjects (P = 0.007). C) Breadth of anti-genotype 1 nAb responses in subjects stratified by infection genotype. Values represent the number of HCVpp neutralized by each subject. The median breadth of nAb responses in each genotype was not different (P = 0.772).
Overall, 60.3% of plasma samples neutralized at least one HCVpp in the genotype 1 HCVpp library while the subtype 1a and subtype 1b HCVpp with the highest neutralization sensitivity was neutralized by only 41.3% and 39.7% of subjects, respectively, (subtype 1a, P = 0.05, subtype 1b, P = 0.03). These data indicate that the use of an HCVpp library for screening for nAb responses during acute infection is a more sensitive approach than screening with a single HCVpp.
Infection genotype does not affect neutralization breadth
To assess the influence of infection genotype on the breadth of nAb responses, neutralization data from the one-year and time-matched analysis was stratified by infection genotype, regardless of infection outcome, and breadth of nAb responses was compared between infection genotypes. The breadth of nAb responses was similar in both one-year (Figure 2c) and time-matched subjects (Figure 3c) infected with genotype 1, 2 or 3 viruses (one-year, P = 0.452; time-matched, P = 0.778). These data indicate that the breadth of anti-genotype 1 nAb responses is not influenced by infection genotype, and provide further evidence that HCV genotypes do not represent serotypes.
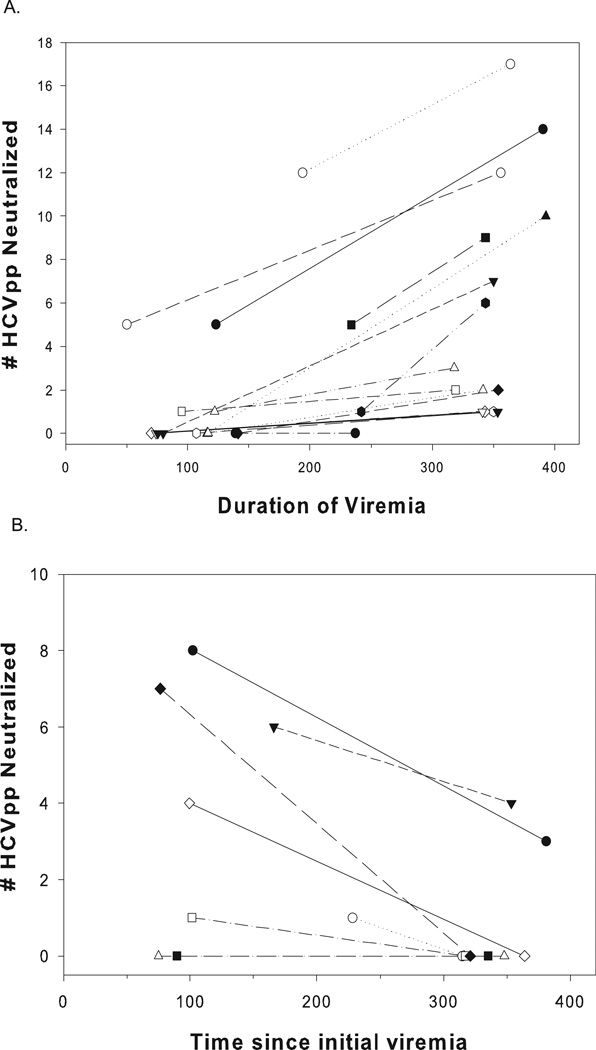
Stability of nAb responses during persistent infection and following viremia control
The breadth of nAb responses in Persistence subjects over time was compared in subjects who were included in both the one-year analysis and time-matched analysis in order to assess whether nAb responses broadened over time in Persistence subjects during acute infection. The breadth of nAb responses in the one-year analysis samples was significantly greater (P > 0.001) than the breadth of nAb responses in the time-matched analysis samples obtained 98 to 306 days earlier from the same subjects (Figure 4A). Conversely, we compared the breadth of nAb responses in Clearance subjects at last viremia with samples obtained from these same subjects one year following initial detection of viremia. The breadth of nAb responses in the last viremic samples was significantly greater (P = 0.03) than the breadth of nAb responses in the one year samples obtained 97 to 279 days later from the same subjects (Figure 4B). These data suggest that the breadth of nAb responses declines following control of viremia and increases during persistent infection.
Figure 4.
nAb responses broaden in Persistence subjects during acute HCV infection and become more shallow in Clearance subjects following control of viremia. A) Increasing breadth of nAb responses in Persistence subjects over time. Values represent the number of HCVpp neutralized by each subject. The breadth of nAb response in each subject is connected by a line. The breadth of nAb responses was greater in the one-year samples than the time-matched subjects (P < 0.001). B) Decreasing breadth of detectable nAb responses in Clearance subjects following control of viremia. The breadth of nAb responses was greater in the last viremic samples than the one-year samples (P = 0.031).
Variation at viral sequence determinants is not associated with neutralization sensitivity
To explore mechanisms underlying variation in sensitivity to neutralization by plasma among HCVpp, we studied viral sequence determinants with respect to neutralization sensitivity. Since the degree of glycosylation of E2 may affect neutralization sensitivity(23), we examined whether the number of predicted N-linked glycosylation sites in the library HCVpp was associated with neutralization sensitivity. The number of N-linked glycosylation sites predicted was 11 in 83% of subtype 1a, and 10 in 86% of subtype 1b, HCVpp envelope sequences (Figure 5a). There were two subtype 1a HCVpp envelope sequences in which only 10 N-linked glycosylation sites were predicted, similarly, there was one genotype 1b HCVpp envelope sequence with only 9 predicted N-linked glycosylation sites. These data suggest that natural variation in the number of N-linked glycosylation sites does not appear to have a major impact on neutralization sensitivity.
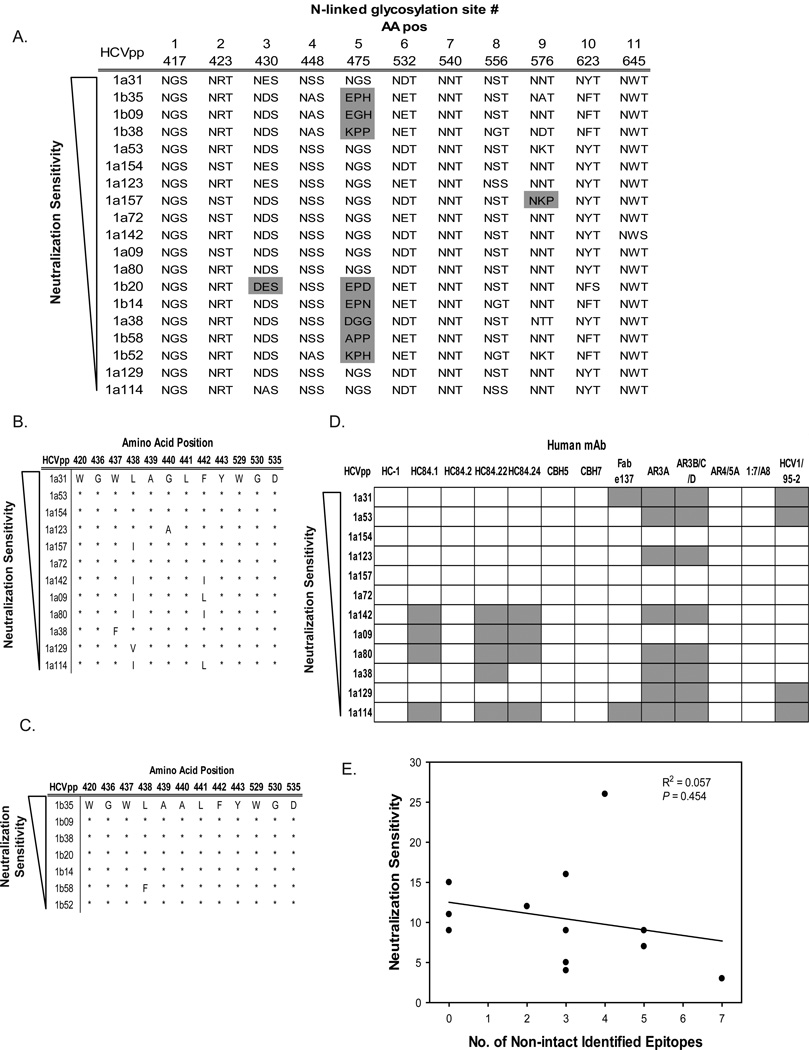
Figure 5.
E1E2 sequence variation versus neutralization sensitivity. A) Amino acid sequences of N-linked glycosylation sites in E2. Amino acid position numbering is based on the H77 reference sequence. CD81 binding residue amino acid sequences in B) subtype 1a and C) subtype 1b HCVpp E1E2 sequences. D) The presence of intact (white) or non-intact (grey) neutralizing epitopes in each HCVpp E1E2 sequence. E) Correlation between the number of non-intact epitopes and neutralization sensitivity. Values represent the number of non-intact epitopes in an HCVpp E1E2 sequence and the neutralization sensitivity of a HCVpp.
Specific amino acid positions in E2 have been shown to be important in HCV-CD81 interactions and disruption of this interaction is a mechanism of neutralization(17). In the current study, variant CD81 binding residues were observed in 67% of subtype 1a HCVpp E1E2 sequences (Figure 5B). While the CD81 binding residues appear to be more variable in the HCVpp with the lowest neutralization sensitivity, variability at CD81 binding residues were also observed in the HCVpp with the highest neutralization sensitivity. Conversely, variability at CD81 binding residues were observed in 86% of subtype 1b sequences across the spectrum of neutralization sensitivities (Figure 5C). These results suggest that the neutralization sensitivity is not strongly associated with natural variation in canonical CD81 binding residues.
Broadly neutralizing human anti-HCV mAbs have been isolated by multiple laboratories and the epitopes targeted by these mAbs have been mapped using alanine scanning(15, 17–19, 21, 22, 24, 25). Since mutation of amino acids in these epitopes may result in escape from nAbs, we investigated whether the presence of intact epitopes in our HCVpp sequences was associated with neutralization sensitivity. The amino acid sequences of each HCVpp at the described epitope positions are presented in Supplementary Figure 1. For all HCVpp, the number of epitopes in which the amino acid sequence was different from the published epitope sequence was not significantly correlated with neutralization sensitivity (R2 = 0.06, P = 0.5; Figure 5D and 5E). These results suggest that the observed natural (rather than alanine-mutagenesis) variation in known mAb epitopes is not associated with decreased neutralization sensitivity.
HLA Class II SNPs are associated with nAb breadth
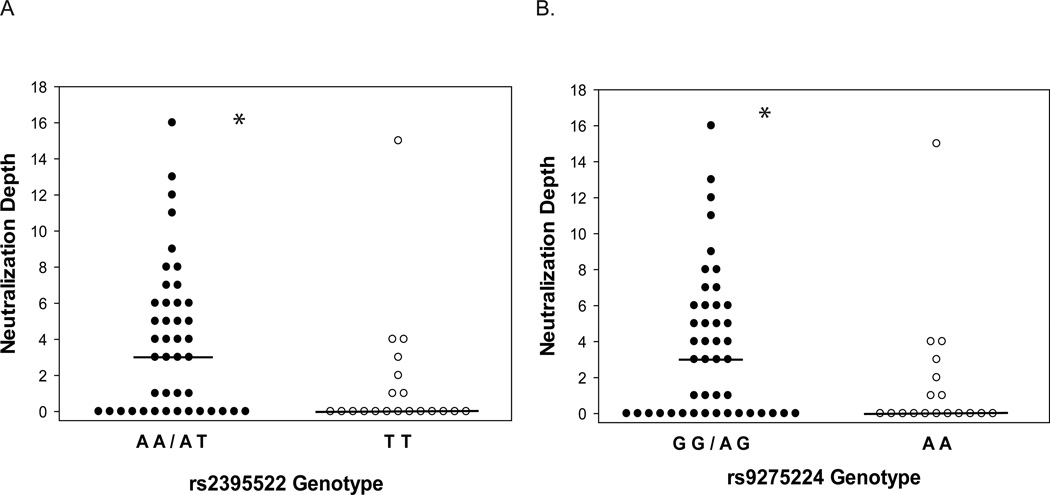
A previous genome-wide association study identified a number of SNPs that are associated with HCV infection outcome(26). Seven of these SNPs are located on chromosome 6, upstream of the HLA-DQB1 and HLA-DQA2 genes. Because one of these genes encodes a protein in the HLA-DQ heterodimer complex that is important in antigen presentation to CD4+ T helper cells, we investigated whether these SNPs were associated with differential breadth of nAb responses. All subjects included in the time-matched analysis were genotyped for each of these seven SNPs and nAb breadth was compared between SNP genotypes, regardless of outcome. The breadth of nAb responses was greater in subjects having the rs2395522 A allele (Figure 6A) or the rs9275224 G allele (Figure 6B). These two SNPs are genetically linked (D’ = 1.0, R2 = 1.0). No differences in nAb breadth were detected between genotypes of the remaining five SNPs (Supplementary Figure 2). These results suggest that HLA class II variation influences breadth of nAb responses during HCV infection.
Figure 6.
HLA-DQ A) rs2395522 and B) rs9275224 SNP genotypes are associated with an increased breadth of nAb responses. Values represent the number of HCVpp neutralized by each subject. * P < 0.05.
Discussion
Using a novel, representative library of genotype 1 HCV envelopes and a unique prospective cohort of persons infected with HCV, we performed the first complete assessment of HCV nAb breadth and control of HCV viremia in humans. In persons who cleared viremia, nAb responses were detected earlier and in greater breadth than in persons whose viremia persisted. In contrast, nAb responses contracted after viremia control while incrementally broadened in persons with persistent infection. These results provide further evidence for a role of nAb in control of HCV infection.
Previous studies have demonstrated that HCV infected individuals are able to generate cross-reactive nAb that target genotypes other than the infecting virus(8, 27). Building upon these studies, we show that the breadth of anti-genotype 1 nAb responses during acute infection was independent of the infection genotype. Therefore, nAb responses in subjects infected with genotype 1, 2 or 3 viruses, and possibly other genotypes, can be assessed using a genotype 1 HCVpp library. These results have implications for rational anti-HCV vaccine design, because the genotype of the E1E2 sequence selected for inclusion in the vaccine may not be important for generating antibodies with relevant neutralization activity.
Frequent sampling of study subjects allowed us to demonstrate that the similar breadth of nAb in the one-year analysis was because persons with persistent infection continued to mount new nAb responses. The differences between one-year and time-matched results can be explained by improved matching in the latter analysis, and reciprocal changes in nAb responses in the two groups. nAb responses rapidly waned after control of viremia while the breadth of nAb increased during the first year in those with Persistence. In contrast, as previously reported using a subset of the same subjects, new T cell responses are rarely detected more than 6 months after initial viremia(28). These kinetic changes agree with prior analyses of common-source outbreaks of HCV(1, 29), validating our HCVpp panel approach and highlighting the importance of accurately identifying infection start and control dates when studying anti-HCV nAb responses.
Interestingly, the percentage of subjects who neutralized at least one heterologous HCVpp was similar in Persistence and Clearance groups while the breadth of nAb responses was associated with infection outcome. This is in agreement with previous reports demonstrating the neutralization of a single heterologous HCV isolate during acute infection was not associated with outcome(30, 31). Therefore, the breadth but not simple presence of a heterologous nAb response may be an important immunological correlate of HCV infection control.
Previous studies have demonstrated that use of an autologous HCVpp results in greater detection of nAb responses than use of a heterologous HCVpp(1, 3, 32). However, the use of autologous HCVpp in studies examining nAb responses in the context of heterogeneous infection scenarios, such as intravenous drug use, is more challenging because a autologous HCVpp must be produced for each subject. We hypothesized that it would be feasible to study nAb responses during acute, non-single source HCV infection in large subject populations by using a HCVpp library that encompasses the genetic variability of E1E2 observed in nature. This study demonstrates that screening for nAb responses using a HCVpp library is more sensitive than using a single HCVpp, because detection of neutralization was observed in approximately 50% more subjects when screened using the panel than with the subtype 1a or 1b HCVpp with the highest neutralization sensitivity.
Using an HCVpp library that represents the natural diversity of genotype 1 E1E2 sequences reveals E1E2 sequence determinants that affect neutralization sensitivity. Variation in neutralization sensitivity was not explained by variation in predicted glycosylation state of library HCVpp, potentially reflecting a vital role for glycans in entry and maintenance of protein structure(33). Disruption of the interaction of HCV with any of the known entry factors is a possible neutralization mechanism for anti-HCV antibodies. CD81, a tetraspanin transmembrane protein, has been shown to facilitate HCV entry through an interaction between E2(34, 35) and the large extracellular loop of CD81(36), so variability of amino acids at these positions may alter neutralization sensitivity. While CD81 binding residues varied in some of the subtype 1a HCVpp E1E2 sequences with low neutralization sensitivity, these amino acids were essentially invariant in subtype 1b HCVpp across neutralization sensitivities.
Using hybridoma and antibody phage display technologies, human anti-HCV mAb that target conformational epitopes and neutralize HCV isolates of multiple genotypes have been isolated and characterized(14, 15, 15–22). We found that natural variability in our genotype 1 HCVpp library at amino acid sites in these conformational epitopes was not correlated with sensitivity to neutralization by plasma. Possible explanations for this finding include incomplete mapping of these epitopes, differential targeting of epitopes during persistent and cleared infection, and infrequent targeting of these epitopes during acute infection. Future mAb-subject plasma competition analyses may help address these discrepancies.
Interestingly, the breadth of nAb responses was significantly associated with the presence of specific alleles of two SNPs located upstream of the HLA-DQB1 and HLA-DQA2 genes, outside of the protein coding regions. While the rs2395522 SNP has not been associated with any other disease outcome, the rs9275224 SNP has been associated with the development of systemic sclerosis(37) and rheumatoid arthritis(38). These SNPs are located outside of the protein coding regions so it is possible that they may be affecting regulation of gene transcription, or are linked to mechanism in some other way. Since HLA class II proteins are necessary for CD4+ helper T cell activation, it is possible that altered expression of these genes may contribute to increased nAb breadth. Further study is needed to clarify the mechanism by which these SNPs affect nAb responses.
Collectively, these results provide clear evidence for nAb responses in control of acute HCV infection, and identify early and broad nAb responses as an immunological correlate of protection against persistent HCV infection. This study also highlights the importance of controlling for duration of infection as well as the utility of using representative HCVpp libraries in assessing nAb responses during acute HCV infection. That control of viremia was associated with an earlier appearance of broader nAb responses and that nAb breadth was independent of infection genotype highlights the relevance of targeting envelope proteins in vaccination strategies to combat HCV-associated mortality and morbidity.
Supplementary Material
Acknowledgements
The authors would like to thank Barbara Rehermann and Elizabeth Kenny-Walsh for providing samples for inclusion in the HCVpp library and the BBAASH study subjects and coordinators.
This work was supported by: NIH grants U19 AI088791, R01013324 and R01 DA024565.
Abbreviations used
- nAb
neutralizing antibody
- mAb
monoclonal antibody
- HCVpp
HCV pseudoparticle
- RLU
relative light units
Footnotes
There are no conflicts of interest to disclose.
The authors contributed the following to the preparation of this manuscript:
W. O. – Study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript
A. S. – Acquisition of data
B. W. – Acquisition of data
R. L. – Acquisition of data
B. F. – Acquisition of data
J. B. – Study concept and design
D.T. – Critical revision of the manuscript for important intellectual content; obtained funding
A. C. – Critical revision of the manuscript for important intellectual content; obtained funding
S. R. – Obtained funding; study concept and design; critical revision of the manuscript for important intellectual content
Genbank accession numbers – XXX – YYY (to be provided upon acceptance)
References
- 1.Pestka JM, Zeisel MB, Blaser E, Schurmann P, Bartosch B, Cosset FL, et al. Rapid induction of virus-neutralizing antibodies and viral clearance in a single-source outbreak of hepatitis C. Proc Natl Acad Sci U S A. 2007 Apr 3;104(14):6025–6030. doi: 10.1073/pnas.0607026104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu L, Fisher BE, Thomas DL, Cox AL, Ray SC. Spontaneous clearance of primary acute hepatitis C virus infection correlated with high initial viral RNA level and rapid HVR1 evolution. Hepatology. 2012;55(6):1684–1691. doi: 10.1002/hep.25575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dowd KA, Netski DM, Wang XH, Cox AL, Ray SC. Selection Pressure from Neutralizing Antibodies Drives Sequence Evolution during Acute Infection with Hepatitis C Virus. Gastroenterology. 2009 Mar 17;136(7):2377–2386. doi: 10.1053/j.gastro.2009.02.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simmonds P. Genetic diversity and evolution of hepatitis C virus - 15 years on. J Gen Virol. 2004;85:3173–3188. doi: 10.1099/vir.0.80401-0. [DOI] [PubMed] [Google Scholar]
- 5.Mao Q, Ray SC, Laeyendecker O, Ticehurst JR, Strathdee SA, Vlahov D, et al. Human immunodeficiency virus seroconversion and evolution of the hepatitis C virus quasispecies. J Virol. 2001 Apr;75(7):3259–3267. doi: 10.1128/JVI.75.7.3259-3267.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pybus OG, Charleston MA, Gupta S, Rambaut A, Holmes EC, Harvey PH. The epidemic behavior of the hepatitis C virus. Science. 2001 Jun 22;292(5525):2323–2325. doi: 10.1126/science.1058321. [DOI] [PubMed] [Google Scholar]
- 7.Cox AL, Netski DM, Mosbruger T, Sherman SG, Strathdee S, Ompad D, et al. Prospective evaluation of community-acquired acute-phase hepatitis C virus infection. Clin Infect Dis. 2005 Apr 1;40(7):951–958. doi: 10.1086/428578. [DOI] [PubMed] [Google Scholar]
- 8.Osburn WO, Fisher BE, Dowd KA, Urban G, Liu L, Ray SC, et al. Spontaneous Control of Primary Hepatitis C Virus Infection and Immunity Against Persistent Reinfection. Gastroenterology. 2010 Jan;138(1):315–324. doi: 10.1053/j.gastro.2009.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kenny-Walsh E. Clinical outcomes after hepatitis C infection from contaminated anti-D immune globulin. Irish Hepatology Research Group. N Engl J Med. 1999 Apr 22;340(16):1228–1233. doi: 10.1056/NEJM199904223401602. [DOI] [PubMed] [Google Scholar]
- 10.Raghuraman S, Park H, Osburn WO, Winkelstein E, Edlin BR, Rehermann B. Spontaneous clearance of chronic hepatitis C virus infection is associated with appearance of neutralizing antibodies and reversal of T-cell exhaustion. J Infect Dis. 2012 Mar 1;205(5):763–771. doi: 10.1093/infdis/jir835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jeanmougin F, Thompson JD, Gouy M, Higgins DG, Gibson TJ. Multiple sequence alignment with Clustal X. Trends Biochem Sci. 1998 Oct;23(10):403–405. doi: 10.1016/s0968-0004(98)01285-7. [DOI] [PubMed] [Google Scholar]
- 12.Hall TA. BioEdit: Biological sequence alignment editor for Windows 95/98/NT version 7.1.3. [accessed 26 Mar 2012];software. 2001 Distributed by author: http://www.mbio.ncsu.edu/bioedit/bioedit.html. [Google Scholar]
- 13.Ray SC, Wang YM, Laeyendecker O, Ticehurst JR, Villano SA, Thomas DL. Acute hepatitis C virus structural gene sequences as predictors of persistent viremia: hypervariable region 1 as a decoy. J Virol. 1999 Apr;73(4):2938–2946. doi: 10.1128/jvi.73.4.2938-2946.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Broering TJ, Garrity KA, Boatright NK, Sloan SE, Sandor F, Thomas WD, Jr, et al. Identification and characterization of broadly neutralizing human monoclonal antibodies directed against the E2 envelope glycoprotein of hepatitis C virus. J Virol. 2009 Dec;83(23):12473–12482. doi: 10.1128/JVI.01138-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perotti M, Mancini N, Diotti RA, Tarr AW, Ball JK, Owsianka A, et al. Identification of a broadly cross-reacting and neutralizing human monoclonal antibody directed against the hepatitis C virus E2 protein. J Virol. 2008 Jan;82(2):1047–1052. doi: 10.1128/JVI.01986-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allander T, Drakenberg K, Beyene A, Rosa D, Abrignani S, Houghton M, et al. Recombinant human monoclonal antibodies against different conformational epitopes of the E2 envelope glycoprotein of hepatitis C virus that inhibit its interaction with CD81. J Gen Virol. 2000 Oct;81(Pt 10):2451–2459. doi: 10.1099/0022-1317-81-10-2451. [DOI] [PubMed] [Google Scholar]
- 17.Owsianka AM, Tarr AW, Keck ZY, Li TK, Witteveldt J, Adair R, et al. Broadly neutralizing human monoclonal antibodies to the hepatitis C virus E2 glycoprotein. J Gen Virol. 2008 Mar;89(Pt 3):653–659. doi: 10.1099/vir.0.83386-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keck ZY, Xia J, Wang Y, Wang W, Krey T, Prentoe J, et al. Human monoclonal antibodies to a novel cluster of conformational epitopes on HCV e2 with resistance to neutralization escape in a genotype 2a isolate. PLoS Pathog. 2012 Apr;8(4):e1002653. doi: 10.1371/journal.ppat.1002653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Giang E, Dorner M, Prentoe JC, Dreux M, Evans MJ, Bukh J, et al. Human broadly neutralizing antibodies to the envelope glycoprotein complex of hepatitis C virus. Proc Natl Acad Sci U S A. 2012 Apr 17;109(16):6205–6210. doi: 10.1073/pnas.1114927109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Law M, Maruyama T, Lewis J, Giang E, Tarr AW, Stamataki Z, et al. Broadly neutralizing antibodies protect against hepatitis C virus quasispecies challenge. Nat Med. 2008 Jan;14(1):25–27. doi: 10.1038/nm1698. [DOI] [PubMed] [Google Scholar]
- 21.Kong L, Giang E, Robbins JB, Stanfield RL, Burton DR, Wilson IA, et al. Structural basis of hepatitis C virus neutralization by broadly neutralizing antibody HCV1. Proc Natl Acad Sci U S A. 2012 Jun 12;109(24):9499–9504. doi: 10.1073/pnas.1202924109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tarr AW, Urbanowicz RA, Jayaraj D, Brown RJ, McKeating JA, Irving WL, et al. Naturally occurring antibodies that recognize linear epitopes in the amino terminus of the hepatitis C virus E2 protein confer noninterfering, additive neutralization. J Virol. 2012 Mar;86(5):2739–2749. doi: 10.1128/JVI.06492-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Helle F, Goffard A, Morel V, Duverlie G, McKeating J, Keck ZY, et al. The neutralizing activity of anti-hepatitis C virus antibodies is modulated by specific glycans on the E2 envelope protein. J Virol. 2007 Aug;81(15):8101–8111. doi: 10.1128/JVI.00127-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johansson DX, Voisset C, Tarr AW, Aung M, Ball JK, Dubuisson J, et al. Human combinatorial libraries yield rare antibodies that broadly neutralize hepatitis C virus. Proc Natl Acad Sci U S A. 2007 Oct 9;104(41):16269–16274. doi: 10.1073/pnas.0705522104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Law M, Maruyama T, Lewis J, Giang E, Tarr AW, Stamataki Z, et al. duplicate; use 9364 instead. Nature Medicine. 2008;14(1):25–27. doi: 10.1038/nm1698. [DOI] [PubMed] [Google Scholar]
- 26.Duggal P, Thio CL, Wojcik GL, Goedert JJ, Mangia A, Latanich R, et al. Genome-wide association study of spontaneous resolution of hepatitis C virus infection: data from multiple cohorts. Ann Intern Med. 2013 Feb 19;158(4):235–245. doi: 10.7326/0003-4819-158-4-201302190-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tarr AW, Urbanowicz RA, Hamed MR, Albecka A, McClure CP, Brown RJ, et al. Hepatitis C patient-derived glycoproteins exhibit marked differences in susceptibility to serum neutralizing antibodies: genetic subtype defines antigenic but not neutralization serotype. J Virol. 2011 May;85(9):4246–4257. doi: 10.1128/JVI.01332-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cox AL, Mosbruger T, Lauer GM, Pardoll D, Thomas DL, Ray SC. Comprehensive analyses of CD8+ T cell responses during longitudinal study of acute human hepatitis C. Hepatology. 2005 Jul;42(1):104–112. doi: 10.1002/hep.20749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Takaki A, Wiese M, Maertens G, Depla E, Seifert U, Liebetrau A, et al. Cellular immune responses persist and humoral responses decrease two decades after recovery from a single-source outbreak of hepatitis C. Nat Med. 2000 May;6(5):578–582. doi: 10.1038/75063. [DOI] [PubMed] [Google Scholar]
- 30.Steinmann D, Barth H, Gissler B, Schurmann P, Adah MI, Gerlach JT, et al. Inhibition of hepatitis C virus-like particle binding to target cells by antiviral antibodies in acute and chronic hepatitis C. J Virol. 2004 Sep;78(17):9030–9040. doi: 10.1128/JVI.78.17.9030-9040.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Logvinoff C, Major ME, Oldach D, Heyward S, Talal A, Balfe P, et al. Neutralizing antibody response during acute and chronic hepatitis C virus infection. Proc Natl Acad Sci U S A. 2004 Jul 6;101(27):10149–10154. doi: 10.1073/pnas.0403519101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lavillette D, Morice Y, Germanidis G, Donot P, Soulier A, Pagkalos E, et al. Human serum facilitates hepatitis C virus infection, and neutralizing responses inversely correlate with viral replication kinetics at the acute phase of hepatitis C virus infection. J Virol. 2005 May;79(10):6023–6034. doi: 10.1128/JVI.79.10.6023-6034.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brown RJ, Tarr AW, McClure CP, Juttla VS, Tagiuri N, Irving WL, et al. Cross-genotype characterization of genetic diversity and molecular adaptation in hepatitis C virus envelope glycoprotein genes. J Gen Virol. 2007 Feb;88(Pt 2):458–469. doi: 10.1099/vir.0.82357-0. [DOI] [PubMed] [Google Scholar]
- 34.Edwards V, Tarr AW, Urbanowicz R, Ball J. The role of neutralising antibodies in hepatitis C virus infection. J Gen Virol. 2011 Nov 2; doi: 10.1099/vir.0.035956-0. [DOI] [PubMed] [Google Scholar]
- 35.Wang Y, Keck ZY, Foung SK. Neutralizing antibody response to hepatitis C virus. Viruses. 2011 Nov;3(11):2127–2145. doi: 10.3390/v3112127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang J, Randall G, Higginbottom A, Monk P, Rice CM, McKeating JA. CD81 is required for hepatitis C virus glycoprotein-mediated viral infection. J Virol. 2004 Feb;78(3):1448–1455. doi: 10.1128/JVI.78.3.1448-1455.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Allanore Y, Saad M, Dieude P, Avouac J, Distler JH, Amouyel P, et al. Genome-wide scan identifies TNIP1, PSORS1C1, and RHOB as novel risk loci for systemic sclerosis. PLoS Genet. 2011 Jul;7(7):e1002091. doi: 10.1371/journal.pgen.1002091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Park J, Namkung J, Jhun M, Park T. Genome-wide analysis of haplotype interaction for the data from the North American Rheumatoid Arthritis Consortium. BMC Proc. 2009;3(Suppl 7):S34. doi: 10.1186/1753-6561-3-s7-s34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.