Abstract
Intra-articular osteoid osteoma (OO) is uncommon, especially in the hip joint. Delayed treatment may cause early osteoarthritis; however, diagnosis and complete excision are often challenging. We describe the feasibility of the combination of T2 mapping magnetic resonance imaging evaluation and arthroscopic excision of OO in the acetabulum. A 12-year-old boy presented with a 6-month history of hip pain. An undifferentiated tumor of the medial wall of the acetabulum was suspected on radiographs and computed tomography. T2 mapping showed joint effusion, and the T2 value of the acetabular cartilage just above the tumor was significantly high. These findings suggested OO in the acetabulum. An arthroscopic excision was performed for biopsy and excision of the tumor to avoid damage to the normal cartilage and growth plate. Histologic examination confirmed the OO. At 16 months' follow-up, there was no evidence of recurrence. This is the first report to evaluate intra-articular OO by T2 mapping and to treat it arthroscopically. Arthroscopic treatment assisted by T2 mapping has excellent potential as a minimally invasive technique to enable us to approach the tumor from the area of discriminative abnormal cartilage with minimal damage to the normal cartilage and surrounding tissue.
Osteoid osteoma (OO) is a benign osteoblastic tumor, representing 13% of all benign tumors, and was described by Jaffé1 in 1935. It occurs mostly in children and young adults and commonly arises in the lower extremity. Intra-articular OO is less frequent (10%), and only 1% to 3% of all cases are located in the pelvic area. Delayed treatment of intra-articular OO is known to damage the cartilage and cause osteoarthritis, so it is important to diagnose it in an early stage and to achieve complete excision of the nidus or cell death.2 The diagnosis of OO is usually possible from typical clinical and imaging findings; however, in intra-articular OO cases, these findings may be absent and the diagnosis is often delayed for months or years. Recently, T2 mapping magnetic resonance imaging has become a standard technique for evaluating articular cartilage, and recent reports support the use of T2 mapping as an early marker of cartilage degeneration.3
We report the arthroscopic excision of OO in the acetabulum in which T2 mapping was useful for diagnosis and treatment. An otherwise healthy 12-year-old boy presented with a 6-month history of persistent pain of the left hip. On the first visit, he had limped badly and physical examination showed limited range of motion. All tests for serologic workup were within the normal range. Radiographs and computed tomography (CT) showed subcortical thickening and lysis in the medial wall of the acetabulum (Figs 1A and 1B). Magnetic resonance imaging and T2 mapping showed that there was joint effusion, and the T2 value of the articular cartilage of the acetabulum just above the tumor was significantly high, which indicated edematous or degenerative changes of the cartilage (Figs 1C and 1D). These findings suggested OO in the acetabulum. The decision was made to perform an arthroscopic biopsy and excision of the tumor.
Fig 1.
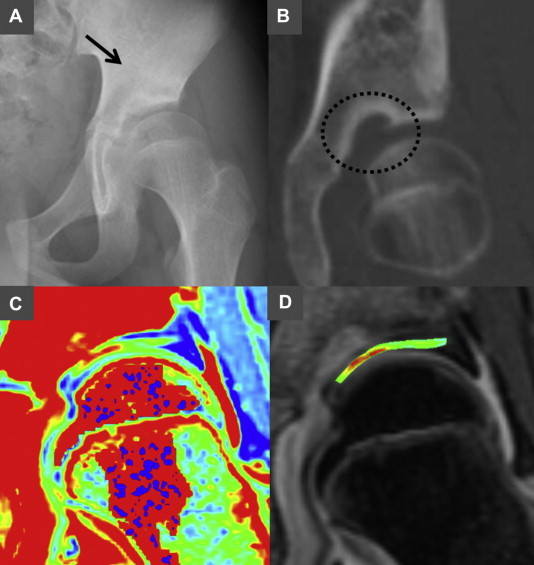
(A) A plain anteroposterior radiograph shows subcortical thickening and lysis in the medial wall of the acetabulum. The arrow indicates the lesion. (B) CT coronal view. The circle indicates the lesion, showing the features of OO: a subcortical oval lytic lesion with a nidus and 11-mm diameter in the medial acetabulum. (C) Preoperative coronal view on T2 mapping magnetic resonance imaging of the hip, colored by color-mapping software (BAUM, version 2D.1.16; Osaka University, Osaka, Japan) because of T2 value. Red indicates a high T2 value, and blue indicates a low T2 value. (D) The T2 value of the articular cartilage above the lesion was higher, which indicated the degenerative changes of the cartilage.
Surgical Technique
The patient underwent surgery in the supine position on a traction table. The operative hip was positioned in approximately 10° of flexion and abduction, with approximately 30° of internal rotation. Fluoroscopy was used preoperatively to locate the exact point for introduction of an arthroscope and location of the tumor. The 70° arthroscope and operating instruments were inserted through the anterolateral portal and midanterior portal, respectively, with Arthrogarde hip access cannulas (Smith & Nephew, Andover, MA). On initial visualization, the hip joint was filled with blood clots, and severe synovial proliferation was noted around the capsule and ligamentous teres (Fig 2A). Meticulous synovectomy was performed with an ablator (Dyonics Eflex monopolar radiofrequency probe; Smith & Nephew) to obtain good visualization of the acetabulum (Video 1). The articular cartilage above the tumor attached to the acetabular fossa had become discolored and thinned so that the location of the tumor could be found immediately and the cartilage was easily peeled off (Fig 2B). A dark cherry-red nidus was located just beneath the cartilage and carefully picked up with a grasper for pathologic examination, and the tumor was then completely resected with motorized instruments (Dyonics high-visibility sheath; Smith & Nephew) and various sizes of straight and angled curettes (Figs 2C and 2D). A meticulous synovectomy and re-examination of the location of the lesion were performed with further curettage of the perilesional bone under fluoroscopic guidance.
Fig 2.
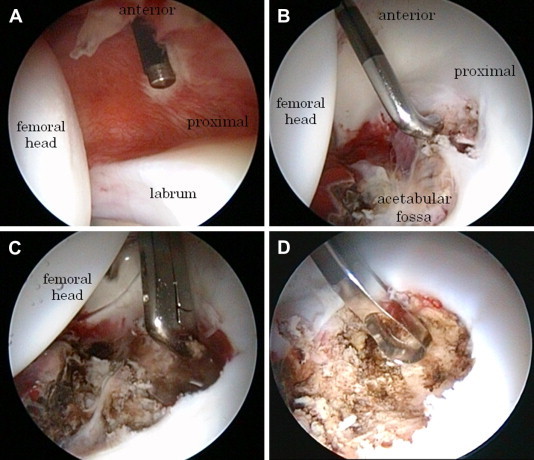
(A) Arthroscopic findings through the anterolateral portal with the patient in the supine position showed that there was severe synovial proliferation around the capsule. An intensive synovectomy was performed with an ablator. (B) Arthroscopic findings through the anterolateral portal showed that there was severe synovial proliferation around the ligamentous teres, and the articular cartilage above the tumor attached to the acetabular fossa had become thinned. (C) The nidus of the OO was located just beneath the articular cartilage. The fragile nidus was first carefully picked up with a grasper for pathologic examination, and the specimens were then completely resected. (D) The tumor was completely resected with an ablator, motorized instruments, and further curettage. The location of the treatment was then confirmed under fluoroscopic guidance.
No surgery-related complications were observed. Pathologic analysis confirmed the diagnosis of OO. Immediately after surgery, the patient had complete pain relief and rapid functional restoration. At 14 months after surgery, clinically, the patient was asymptomatic and had returned to full activities. Follow-up radiographs and CT examination findings showed successful complete excision of the tumor, partial ossification of the nidus, and no evidence of recurrence (Fig 3A). T2 mapping at 1 year after surgery showed that the T2 value of the articular cartilage of the acetabulum was decreased compared with that before surgery (Fig 3B).
Fig 3.
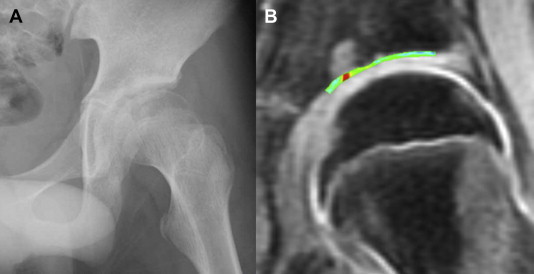
(A) Postoperative anteroposterior radiograph obtained 16 months after surgery. (B) The postoperative coronal view with T2 mapping 14 months after surgery showed that the T2 value of the articular cartilage of the acetabulum became lower compared with that before surgery.
Discussion
OO is characterized by typical imaging findings and local pain that is more frequent and severe at night, which is relieved by nonsteroidal anti-inflammatory drugs. On radiographs and CT, OO elicits an osteoblastic response in surrounding bone and shows sclerosis around the nidus. However, in some intra-articular cases, it may present with clinical features that mimic inflammatory synovitis and with atypical radiologic findings such as lack of both sclerosis and periosteal reaction. Given that Szendroi et al.4 reported that the degree of accuracy in the diagnosis of intra-articular lesions is 66%, it may be mistaken for other etiologies, causing the diagnosis to be delayed for months or years.
As for the pathophysiology, OO's relatively small size, self-limited nature, and intracellular viral particles may suggest an inflammatory process. Prostaglandins are thought to be implicated and linked to OO, and prostaglandins and other mediators are believed to provide a common pathway for pain generation. Besides, especially in intra-articular OO, Kawaguchi et al.5 reported that cyclooxygenase-2 protein produced by nidal osteoblasts released into the joint activates the arachidonic acid metabolism pathway and these changes are responsible for the development of osteoarthritis.
For the treatment of OO, surgery has remained the standard treatment in cases in which the nature of the lesion is in doubt, although less invasive methods such as CT-guided radiofrequency ablation (RFA) are gaining popularity.6 Especially in intra-articular cases, medical treatment may appear difficult because of the critical location of the tumor. Even with RFA, there is a possibility of thermal damage to the articular and triradiate cartilage, and the risk of recurrence increases if the patient is a child and the size of the tumor is over 10 mm.7
In our case the radiographs and CT findings could not provide accurate differentiation of the tumor; however, T2 mapping showed an inflammation or degenerative change of the cartilage just above the tumor, which suggested the diagnosis of OO in the acetabulum. Direct arthroscopic visualization allows histologic confirmation, synovectomy of concomitant synovitis for the prevention of joint degeneration, and complete excision of the tumor with minimal damage to the surrounding tissue.8 Furthermore, the major advantage of arthroscopy for OO is that synovectomy of concomitant synovitis and tumor excision can be performed together. Besides, T2 mapping enabled us to approach the tumor from the area of discriminative abnormal cartilage so that tumor resection could be performed with minimal disruption to the normal cartilage. At 14 months after surgery, follow-up radiographs and CT examination findings showed successful complete excision of the tumor without any evidence of recurrence. Furthermore, T2 mapping showed cartilage healing of the acetabulum.
This is the first report of the arthroscopic treatment and evaluation of intra-articular OO in the acetabulum by T2 mapping. There are some problems and limitations in this study. In our case it was easy to identify and excise the lesions because they were located in the medial wall. However, in some intramedullary cases, it may not always be possible to visualize the lesion through arthroscopic examination; therefore other treatment options such as CT-guided RFA should be considered (Table 1). Despite our limited experience, we believe that arthroscopic treatment assisted by T2 mapping comprises a minimally invasive technique that allows tumor excision with concomitant synovectomy that minimizes damage to the normal cartilage. The achieved result is encouraging, showing that T2 mapping may be a useful technique for diagnosis and treatment of this pathology.
Table 1.
Indication, Contraindications, Pearls, and Pitfalls
| Indication | Contraindications | Pearls | Pitfalls |
|---|---|---|---|
| Intra-articular OO | Juxta-articular lesion | Use T2 mapping to approach from the area of discriminative abnormal cartilage. | Unless image evaluation is not used, damage to the normal and triradiate cartilage will occur. |
| Some intramedullary cases | An intensive synovectomy is needed to avoid osteoarthritis. | Capsulotomy before ablation of the capsule may cause bleeding from the synovium. | |
| Fluoroscopic guidance is helpful for detecting the lesion and further curettage. | There are some issues associated with hip arthroscopy: complications may be encountered, and the procedure is technically demanding. |
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
(1) After preparation of the anterolateral and midanterior portals, severe hemorrhagic proliferation of the synovium was observed. (2) After synovectomy around the portal with an ablator to avoid bleeding from the synovium, capsulotomy was performed to widen the portal. (3) An intensive synovectomy was performed around the capsule and ligamentous teres with an ablator. (4) The articular cartilage above the tumor attached to the acetabular fossa had become discolored and thinned so that the location of the tumor could be found immediately and the cartilage was easily peeled off. After the fragment of the articular cartilage was peeled off, a dark cherry-red nidus was seen and carefully picked up with a grasper for pathologic examination. (5) The tumor was then completely resected with an ablator, motorized instruments, and further curettage. (6) The wall of the tumor was burned with an ablator, and the location of the treatment was confirmed under fluoroscopic guidance.
References
- 1.Jaffé H.L. Osteoid osteoma. Arch Surg. 1935;31:709–728. [Google Scholar]
- 2.Norman A., Abdelwahab I.F., Buyon J., Matzkin E. Osteoid osteoma of the hip stimulating an early onset of osteoarthritis. Radiology. 1986;158:417–420. doi: 10.1148/radiology.158.2.3941866. [DOI] [PubMed] [Google Scholar]
- 3.Baum T., Stehling C., Joseph G.B. Changes in knee cartilage T2 values over 24 months in subjects with and without risk factors for knee osteoarthritis and their association with focal knee lesions at baseline: Data from the osteoarthritis initiative. J Magn Reson Imaging. 2012;35:370–378. doi: 10.1002/jmri.22834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Szendroi M., Killo K., Antal I. Intraarticular osteoid osteoma: Clinical features, imaging results, and comparison with extraarticular localization. J Rheumatol. 2004;31:957–964. [PubMed] [Google Scholar]
- 5.Kawaguchi Y., Sato C., Hasegawa T. Intraarticular osteoid osteoma associated with synovitis: A possible role of cyclooxygenase-2 expression by osteoblasts in the nidus. Mod Pathol. 2000;13:1086–1091. doi: 10.1038/modpathol.3880202. [DOI] [PubMed] [Google Scholar]
- 6.Rehnitz C., Sprengel S.D., Lehner B. CT-guided radiofrequency ablation of osteoid osteoma: Correlation of clinical outcome and imaging features. Diagn Interv Radiol. 2013;19:330–339. doi: 10.5152/dir.2013.096. [DOI] [PubMed] [Google Scholar]
- 7.Vanderschueren G.M., Tammiau A.H.M., Obermann W.R., Berg-Huysmans A.A., Bloem J.L. Osteoid osteoma: Factors for increased risk of unsuccessful thermal coagulation. Radiology. 2004;233:757–762. doi: 10.1148/radiol.2333031603. [DOI] [PubMed] [Google Scholar]
- 8.Adachi N, Shimose S, Nakamae A, Okuhara A, Kamei G, Ochi M. Intra-articular osteoid osteoma of the lateral tibial plateau treated with arthroscopically assisted removal and retrograde osteochondral grafting. Knee in press, available online 15 August, 2013. doi:10.1016/j.knee.2013.08.005. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(1) After preparation of the anterolateral and midanterior portals, severe hemorrhagic proliferation of the synovium was observed. (2) After synovectomy around the portal with an ablator to avoid bleeding from the synovium, capsulotomy was performed to widen the portal. (3) An intensive synovectomy was performed around the capsule and ligamentous teres with an ablator. (4) The articular cartilage above the tumor attached to the acetabular fossa had become discolored and thinned so that the location of the tumor could be found immediately and the cartilage was easily peeled off. After the fragment of the articular cartilage was peeled off, a dark cherry-red nidus was seen and carefully picked up with a grasper for pathologic examination. (5) The tumor was then completely resected with an ablator, motorized instruments, and further curettage. (6) The wall of the tumor was burned with an ablator, and the location of the treatment was confirmed under fluoroscopic guidance.


