Abstract
Recently, there has been a rapid increase in the number of hip arthroscopies performed. The increase in the number of primary surgeries has been associated with a similar increase in the number of revision procedures. The most frequent indications for revision hip arthroscopy are residual bony deformity (impingement), persistent labral pathology, and intra-articular adhesions. Our current understanding of capsulolabral adhesions is limited. Although adhesions between the capsule and labrum are common after hip arthroscopy, generally, they are mild and asymptomatic. However, in severe cases they may cause persistent synovitis and pain, and they may tether the labrum away from the femoral head, causing loss of the suction-seal effect. Such patients present with nonspecific symptoms such as persistent pain, giving way, catching, and pain in hip flexion. Magnetic resonance imaging can aid in the diagnosis by showing the absence of liquid in the capsulolabral recess, although the definitive diagnosis is based on dynamic arthroscopic evaluation. We present our approach to the lysis of capsulolabral adhesions with preservation of labral tissue and describe a technique that uses an iliotibial band allograft to prevent recurrence of such adhesions by maintaining space between the capsule and labrum.
In the past decade, there has been a large increase in the number of hip arthroscopies performed because of the recognition of femoroacetabular impingement (FAI) as a cause of hip pain in young adults. However, the increase in the number of primary surgeries comes with a similar increase in the number of revision surgeries. Diagnostic evaluation and surgical decision making in patients with persistent pain after hip arthroscopy are complex.1 The most frequent indications for revision hip arthroscopy are residual bony deformity (impingement), persistent labral pathology or insufficiency, and adhesions. Adhesions may occur between the capsule and the labrum or between the capsule and the femoral neck. In this article we will focus on the adhesions between the capsule and the labrum, which are commonly seen after arthroscopic hip surgery (Table 1).2,3
Table 1.
Key Points
| Adhesions are common at revision hip arthroscopy but are not always symptomatic. |
| Symptomatic adhesions can be removed through careful dissection of the capsulolabral recess. |
| The native labrum should be preserved whenever possible. |
| Aggressive adhesion debridement may inadvertently remove healthy labral tissue. |
| A capsulolabral spacer is made with a tubularized iliotibial band allograft. |
| The spacer may prevent recurrent adhesions by keeping an offset between the capsule and the labrum. |
Our current understanding of capsulolabral adhesions is limited. The hip capsulolabral recess has an abundant blood supply, which may contribute to adhesions after surgical intervention. Kelly et al.4 showed the predominance of vasculature on the capsular margin of the labrum and in the adjacent capsulolabral recess. Surgical exposure in this area during arthroscopy, as well as the presence of suture material from labral repair, may play a role in adhesion formation. Capsulolabral adhesions are frequently encountered in revision surgery.2 Often, they are mild and do not cause symptoms. However, in some cases severe adhesions can contribute to persistent synovitis and pain, as well as loss of the fluid seal due to tethering of the labrum. In these cases the labrum can be everted by the adhesions and lose contact with the femoral head during motion.
Diagnosis
Clinical symptoms in patients with capsulolabral adhesions may include decreased range of motion; persistent pain; and symptoms of microinstability, such as “giving way,” catching, and apprehension in extremes of motion. Some patients report pain with straight hip flexion (after around 85° of flexion) and not necessarily with adduction and internal rotation, differentiating it from the anterior impingement sign. A comprehensive physical examination is important in this population to confirm an intra-articular source of pain. Young female patients are particularly prone to capsulolabral adhesions after hip arthroscopy. Philippon et al.5 reported the outcomes of 60 surgeries performed in patients aged younger than 16 years. Among these patients, 8 needed revision procedures because of adhesions, all of whom were female patients. Hip circumduction exercises in the rehabilitation protocol seem to help to prevent this complication.6
It is important to obtain details regarding surgical treatment during the primary procedure, as well as the status of the labrum, cartilage, and capsule. The amount of acetabular rim exposure likely plays a role because of increased bleeding and subsequent scar formation. In our experience, capsulolabral adhesions will rarely develop in patients who undergo surgery for isolated cam FAI. The presence of suture material in the capsulolabral recess from prior repair may initiate a biologic response in some patients. Therefore we believe that it is important to recess the sutures inside the anchor hole as much as possible during labral repair.
Surgical Technique
We perform hip arthroscopy with the patient in the supine position, using 2 working portals (mid anterior and anterolateral). Revision arthroscopy in this population is performed in a systematic fashion (Video 1): (1) After a diagnostic inspection, adhesions between the capsule and labrum are released. (2) All other pathology, such as persistent labral or chondral damage and cam or pincer lesions, is addressed. (3) The labral spacer allograft is prepared and positioned inside the joint. (4) Finally, the capsule is inspected and closed.
The release of capsulolabral adhesions without damage to the underlying labrum is challenging. It is important to use different instruments. A Beaver blade (Smith & Nephew, Andover, MA) is used for sharp dissection between the capsule and labrum and to create the initial plane of dissection. A Dyonics Platinum shaver (Smith & Nephew) is then used to remove loose and frayed tissue. Finally, a radiofrequency device (Dyonics RF; Smith & Nephew) is useful for cauterizing bleeding surfaces as necessary. Preservation of the native labral tissue is important during the removal of adhesions (Fig 1). In addition, any retained suture from previous repair should be removed. After lysis of adhesions, any residual pincer lesion, when present, is addressed. Precise and controlled rim trimming with an Abrader Burr (Smith & Nephew) is needed to avoid iatrogenic instability. The subspinal region should also be examined as a potential source of residual impingement.
Fig 1.
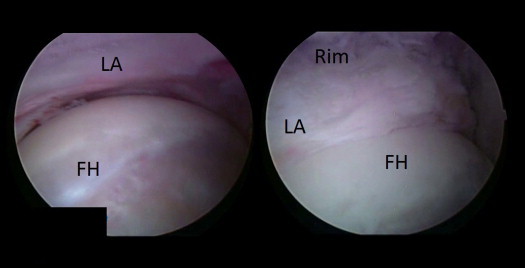
Left hip in supine position, viewed from mid-anterior portal. Before adhesion release (left), the LA is tethered to the capsule, limiting its contact with the FH. After release of adhesions (right), the area between the LA and the rim is visible and the labrum makes full contact with the FH. (FH, femoral head; LA, labrum.)
If, after lysis of adhesions, the remnant labrum is absent or severely insufficient, we recommend labral reconstruction with a tubularized iliotibial band autograft as previously described.7,8 When the native labrum is adequate, we use allograft spacer placement in the capsulolabral recess to attempt to decrease the formation of recurrent adhesions. The graft is positioned between the capsule and the labrum and is secured in position with suture anchors. We use an iliotibial band allograft for the capsulolabral spacer. The allograft tissue is trimmed to the appropriate width. It is tubularized to a diameter of 6 to 7 mm. The graft is cut to the same length as the extent of the adhesions observed during inspection. It is tubularized with No. 2-0 Vicryl (Ethicon, Somerville, NJ). We use 2 passes of a continuous suture to make sure the tubularization is tight and stable. At the lateral end of the graft, a loop suture is made to aid in intra-articular manipulation of the graft. The graft is first secured to the most medial suture anchor (Osteoraptor 2.3 mm; Smith & Nephew) right after the graft is pushed down a plastic cannula of sufficient diameter. We use a free needle to pass the first anchor's suture through the graft before passage down the cannula. Next, the grasper is used to position the graft evenly in the capsulolabral recess, at the same location at which the adhesions were released at the beginning of the procedure (Fig 2). The lateral end of the graft is secured with a second anchor at the lateral extent of the affected area. The loop suture aids in the manipulation of the graft because it is still very mobile inside the joint at this point. The lateral extent of the graft can be secured with this loop or with passage of a suture-passing device (NanoPass; Pivot Medical, Sunnyvale, CA) through the substance of the graft. In addition, suture can be passed through the substance of the labrum in a vertical mattress fashion to add additional stability without compromising the hip seal. Several other suture anchors are then used to secure the graft firmly in position. The exact number will vary depending on the size of the graft, while keeping a mean distance of 1 cm between anchors. It is important to make sure that all knots are placed on the capsular side of the labrum to avoid this as a potential cause of further adhesions.
Fig 2.
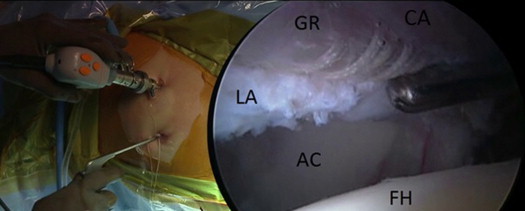
Left hip in supine position, viewed from mid-anterior portal. The GR is being positioned between the labrum and the CA with the use of a grasper. (AC, acetabulum; CA, capsule; FH, femoral head; GR, graft; LA, native labrum.)
The final construct shows the graft firmly secured between the labrum and the capsule (Fig 3). At this point, traction is released and a dynamic examination is performed to ensure that the labrum and graft are stable in position. Restoration of the suction seal is also confirmed on dynamic examination. The capsule is closed with No. 1 absorbable sutures (Vicryl)—generally, 2 to 3 sutures.
Fig 3.
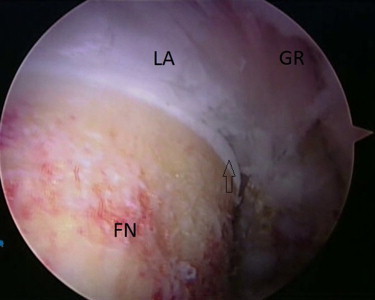
Left hip in supine position, viewed from mid-anterior portal. When the GR is in place, the labrum contacts the femoral head and the seal is re-established. The arrow indicates the head-neck junction (the head is not visible because traction was released). (FN, femoral neck; GR, graft; LA, native labrum.)
We emphasize the value of circumduction exercises during postoperative rehabilitation. Circumduction is performed with the hip extended and flexed. From day 1, this type of exercise is important to prevent adhesions from recurring while being a safe exercise that will not compromise the stability of the construct. We use continuous passive motion and early stationary bicycling in all patients. Three weeks of partial weight bearing with crutches is recommended.
Discussion
Revision hip arthroscopy often poses challenges that are not seen during primary cases, including the presence of symptomatic capsulolabral adhesions. Mild adhesions may not be a source of persistent pain in many cases, but severe capsulolabral adhesions can contribute to persistent symptoms by compromising the function of the acetabular labrum. Tethering of the capsule to the labrum leads to coupled motion of the capsule and labrum that may pull the labrum away from the femoral head. This phenomenon can lead to loss of the hip seal (Video 1) and lead to persistent symptoms of microinstability.
In 2007 Philippon et al.2 published their experience with revision hip arthroscopy. Adhesions were present in as many as 62% of the patients in their series, which suggested how much this phenomenon could contribute to persistent symptoms after hip arthroscopy. Beck and colleagues3,9 described intra-articular adhesions of the hip joint after surgical hip dislocation for the treatment of FAI. Although their studies reported on adhesions after an open procedure, we believe that the clinical presentation is similar to what is seen after arthroscopic surgery.
If extensive capsulolabral adhesions are observed during revision hip arthroscopy, the surgeon must determine whether the labral tissue is tethered to the capsule or whether it is hypoplastic/absent (possibly from previous labral debridement). If the labral tissue is hypotrophic, it is better to simply remove all the scar tissue and proceed with a full labral reconstruction (Table 2). Good clinical outcomes of patients undergoing labral reconstruction with an iliotibial band graft have been reported.7,8 When the labral tissue still has good firmness and thickness, it should be preserved. Lysis of adhesions can restore the sealing function of the labrum but, in the experience of the senior author, can be difficult to prevent from recurring in some patients. In these cases our technique aims to create an offset between the capsule and labrum to prevent recurrence of adhesions and keep the native labrum in constant contact with the femoral head, producing an effective hip fluid seal.
Table 2.
Indications and Contraindications
| Indications | Contraindications |
|---|---|
| Symptomatic adhesions | Minor/asymptomatic adhesions |
| Viable native labrum (7 mm in thickness) | Insufficient labral tissue (from previous debridement) |
| >2 mm of joint space | Narrowed joint space/hip arthritis |
The main advantage of our technique is that it reopens the space between the capsule and the labrum while preserving the original labral tissue and keeping its biomechanical properties. When the labrum still has sufficient firmness and thickness, it should provide an optimal fluid seal, as long as it is not tethered away from the femoral head because of adhesions.
The described technique has its limitations: It is not capable of restoring the fluid seal if not enough labral tissue is viable. If this is the case, it is better to completely remove all scar tissue and remnant labrum, expose the acetabular rim, and perform a labral reconstruction. In addition, this technique is not indicated in patients with signs of arthritis and joint space narrowing. As a guideline, we recommend not performing this procedure in patients with less than 2 mm of joint space, for whom a total hip replacement should be considered.10
Footnotes
The authors report the following potential conflict of interest or source of funding: M.J.P. receives support from Steadman Philippon Research Institute, ISHA, Smith & Nephew, MIS, Ossur, Siemens, Vail Valley Medical Center, Arthrosurface, DonJoy, Slack, Elsevier, Linvatec, HIPCO. F.P.F. receives support from Smith & Nephew, Ossur, Siemens, Vail Valley Medical Center. J.J.N. receives support from Smith & Nephew, Ossur, Siemens, Vail Valley Medical Center.
Supplementary Data
Our technique is demonstrated in a left hip, in the supine position, with the arthroscope positioned in the mid-anterior portal. The capsulolabral adhesions are released. An iliotibial band allograft is tubularized so that it can be used as a spacer between the capsule and labrum. The graft is inserted in the correct position and secured in the capsulolabral recess by using suture anchors.
References
- 1.Lynch T.S., Terry M., Bedi A., Kelly B.T. Hip arthroscopic surgery: Patient evaluation, current indications, and outcomes. Am J Sports Med. 2013;41:1174–1189. doi: 10.1177/0363546513476281. [DOI] [PubMed] [Google Scholar]
- 2.Philippon M.J., Schenker M.L., Briggs K.K., Kuppersmith D.A., Maxwell R.B., Stubbs A.J. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 3.Beck M. Groin pain after open FAI surgery: The role of intraarticular adhesions. Clin Orthop Relat Res. 2009;467:769–774. doi: 10.1007/s11999-008-0653-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelly B.T., Shapiro G.S., Digiovanni C.W., Buly R.L., Potter H.G., Hannafin J.A. Vascularity of the hip labrum: A cadaveric investigation. Arthroscopy. 2005;21:3–11. doi: 10.1016/j.arthro.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 5.Philippon M.J., Ejnisman L., Ellis H.B., Briggs K.K. Outcomes 2 to 5 years following hip arthroscopy for femoroacetabular impingement in the patient aged 11 to 16 years. Arthroscopy. 2012;28:1255–1261. doi: 10.1016/j.arthro.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 6.Willimon S.C., Briggs K.K., Philippon M.J. Intra-articular adhesions following hip arthroscopy: A risk factor analysis. Knee Surg Sports Traumatol Arthrosc in press, available. 26 October, 2013 doi: 10.1007/s00167-013-2728-0. doi:10.1007/s00167-013-2728-0. [DOI] [PubMed] [Google Scholar]
- 7.Geyer M.R., Philippon M.J., Fagrelius T.S., Briggs K.K. Acetabular labral reconstruction with an iliotibial band autograft: Outcome and survivorship analysis at minimum 3-year follow-up. Am J Sports Med. 2013;41:1750–1756. doi: 10.1177/0363546513487311. [DOI] [PubMed] [Google Scholar]
- 8.Philippon M.J., Briggs K.K., Hay C.J., Kuppersmith D.A., Dewing C.B., Huang M.J. Arthroscopic labral reconstruction in the hip using iliotibial band autograft: Technique and early outcomes. Arthroscopy. 2010;26:750–756. doi: 10.1016/j.arthro.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 9.Dudda M., Mamisch T.C., Krueger A., Werlen S., Siebenrock K.A., Beck M. Hip arthroscopy after surgical hip dislocation: Is predictive imaging possible? Arthroscopy. 2011;27:486–492. doi: 10.1016/j.arthro.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Philippon M.J., Schroder E., Souza B.G., Briggs K.K. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy. 2012;28:59–65. doi: 10.1016/j.arthro.2011.07.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Our technique is demonstrated in a left hip, in the supine position, with the arthroscope positioned in the mid-anterior portal. The capsulolabral adhesions are released. An iliotibial band allograft is tubularized so that it can be used as a spacer between the capsule and labrum. The graft is inserted in the correct position and secured in the capsulolabral recess by using suture anchors.


