Abstract
We describe the use of intraoperative ultrasound for the safe development of arthroscopic portals during hip arthroscopy without the requirement for fluoroscopy. We find this technique consistently accurate, allowing the safe introduction of arthroscopic instruments into the hip with a very low rate of iatrogenic injury. We have further developed the technique for application to both central- and peripheral-compartment procedures. We now have a total experience of more than 700 procedures to date. With the described technique of ultrasound guidance for portal placement, fluoroscopy is required in fewer than 2% of hip arthroscopy procedures at our institution.
Arthroscopic procedures of the hip are becoming increasingly popular for the management of early articular pathology and pre-arthritic disorders of the hip joint. Because of the deep location and highly constrained nature of the hip joint, safe passage of arthroscopic instrumentation to the hip joint routinely requires intraoperative imaging in the form of fluoroscopy. In the hands of an experienced surgeon, using appropriate techniques under fluoroscopic guidance, the rate of iatrogenic articular damage during hip arthroscopy to either the acetabular labrum or hyaline cartilage surfaces is very low. However, the use of fluoroscopy does have some disadvantages. Although the required fluoroscopic exposure time is usually limited to the development of the hip arthroscopic portals, radiation is applied not only to the patient but also to staff, who may be involved in large volumes of procedures over time. Protecting staff from radiation behind lead screens can increase the operative time under traction, and the use of lead gowns increases staff fatigue. There are also the practical implications with the use of fluoroscopy because lead screens and fluoroscopic equipment and monitors lead to congestion in operating theaters with limited space. Furthermore, the use of fluoroscopy usually requires coordination with radiology departments, and in some institutions with limited imaging resources, competing for intraoperative fluoroscopy assistance can lead to theater delays. In addition, there are sterility requirements for the fluoroscopy C-arm that may be of particular concern with the patient in a lateral decubitus arthroscopic position in which the arm needs to be swung either over or under the patient to obtain appropriate imaging.
Hua et al.1 described the use of ultrasound guidance in the establishment of hip arthroscopic portals in 18 patients in the supine position by use of a low-frequency (3- to 5-MHz) convex transducer. The described technique required arthroscopy to be undertaken with both a surgeon and radiologist in consultation during the procedure. The first arthroscopic portal was developed with the hip not distracted initially, which in part may explain the relatively high rate of chondrolabral injuries observed with this technique (4 of 18 patients).
We describe an alternative method of arthroscopic portal development with the hip distracted, using a sequence of instrumentation that would be familiar to hip arthroscopy surgeons. Furthermore, our technique is relatively easy to learn and can simply be conducted by the operating surgeon without radiologist or radiographer assistance. We have previously described the use of ultrasonography in the conduct of arthroscopic proximal iliotibial band release about the hip.2
Technique
At our institution, we prefer to conduct hip arthroscopy with the patient in a supine position, although the technique using ultrasound described earlier is equally valid and easy to conduct with the patient in the lateral decubitus position. The patient is placed supine with a well-padded perineal post; particular attention is given to the adequacy of binding and pressure area care to the foot. The patient is administered a general anesthetic with muscle paralysis. No antibiotics are administered. The contralateral leg is placed in slight traction to stabilize the pelvis. Traction to the operative leg is applied in the line of the femoral neck by a combination of adduction across the broad perineal post and longitudinal traction applied by the traction table in the line of the leg. While under traction, the hip is placed in slight flexion and approximately 10° of internal rotation. The ultrasound machine is placed on the operative side, beside the patient's head, ensuring accessibility and ease of vision for the surgeon. All other equipment required is placed on the nonoperative side of the patient (Fig 1).
Fig 1.
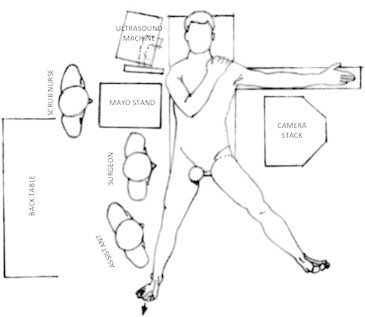
Basic theater layout.
Initial assessment of the adequacy of traction is made by use of real-time ultrasound while the traction is being applied. We use a LOGIQe ultrasound machine (GE Healthcare, Sydney, Australia) with a 4C-RS 2.0- to 5.5-MHz transducer (GE Healthcare). The transducer is placed longitudinal to the femur, approximately 3 cm above the greater trochanter (Fig 2). Traction is then applied to the patient before sterile preparation and draping are conducted to assess the adequacy of joint distraction. If inadequate distraction of the joint is observed at this stage, the reasons are identified and addressed. Traction is removed while the hip region is prepared with antiseptic solution and drapes are applied. The ultrasound transducer is prepared by placing unsterile gel on the transducer, which is then covered with a sterile plastic bag (Elastic Fluoro Cover, 91 × 76 cm; Bard Lifemed, North Ryde, Australia) (Fig 3). The sterile transducer bag is then placed and secured in the fluid collection pouch of a vertical isolation drape. Sterile urinary catheterization lubricant is applied to the operating area to allow conductivity of the ultrasound wave signal.
Fig 2.
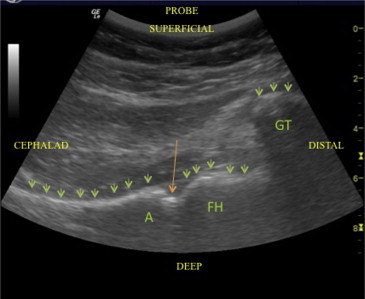
Ultrasound image of right hip (longitudinal view, no traction). The green arrows indicate the bony artifact, and the orange arrow indicates the joint space. (A, acetabulum; FH, femoral head; GT, greater trochanter.)
Fig 3.
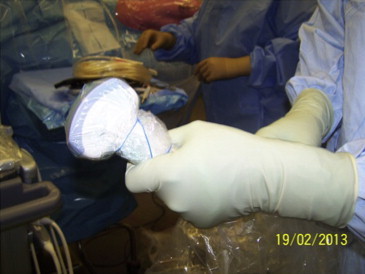
Sterile draping of ultrasound transducer.
The first portal developed is the posterior trochanteric portal, located 1 cm above the posterior one-third of the greater trochanter (Fig 4, Video 1). The greater trochanter is identified by direct palpation; however, its location can also be assisted by ultrasound if the patient is obese. Traction is applied with visualization of the degree of distraction by real-time ultrasound. Adequate distraction is judged to be on the order of 8 to 10 mm and can be judged by the evaluation of the femoral head excursion in relation to the acetabulum. Frequently, it is possible to see the acetabular labrum clearly, particularly in thinner patients. The initial portal needle is placed into the hip joint under direct ultrasound guidance. Usually, if an effusion is not present, an ultrasound artifact is observed at the interface between the air vacuum within the hip and the capsule of the joint. This will cast a linear echo shadow into the joint, which we have termed the “light-saber sign” (Fig 5). The most superficial portion of the light saber represents the interface between air and the intra-articular vacuum, and the needle is directed toward the center of this. Specific attention is taken to avoid the acetabular labrum, and particular attention is taken to avoid iatrogenic damage to the hyaline cartilage of the femoral head. After the initial portal needle has been placed, a standard cannulated instrument technique is used with passage of a nitinol wire, and subsequent development of the portal by use of cannulated instruments is conducted. Subsequent development of the portal after passage of the initial needle is conducted blind without the requirement for further imaging. This initial posterior trochanteric portal is used for placement of a 70° arthroscope (4.0 mm × 70° autoclavable videoarthroscope, 160-mm working length; Smith & Nephew, North Ryde, Australia), and initial evaluation of the hip joint surfaces can be conducted at this point under dry conditions without lavage fluid. Development of the anterior working portal is conducted by direct vision without the use of either ultrasound or fluoroscopy. After the working anterior portal has been developed, saline lavage fluid under pressure using an arthroscopic pump is delivered into the joint and joint assessment with corrective intervention can be conducted as necessary.
Fig 4.
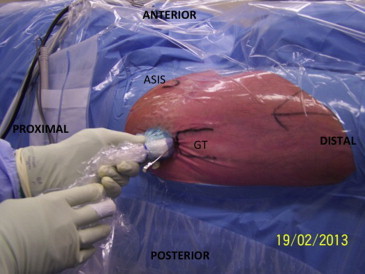
Position of transducer for initial (viewing) portal for central-compartment hip arthroscopy. (ASIS, anterior superior iliac spine; GT, greater trochanter.)
Fig 5.
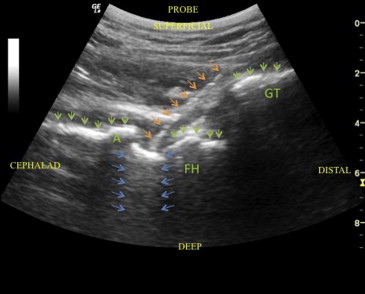
Ultrasound image showing air–intra-articular artifact (light-saber sign) and needle position for initial (viewing) portal placement. The green arrows indicate the bony artifact, the orange arrows indicate the needle, and the blue arrows indicate the light-saber artifact. (A, acetabulum; FH, femoral head; GT, greater trochanter.)
For peripheral-compartment procedures, we prefer to develop separate dedicated portals—all instruments used for establishment of the central-compartment procedure are removed from the hip joint, and traction is released. The foot is taken out of the traction device and is flexed to approximately 30°. The ultrasound transducer is placed on the anterior groin and aligned with the femoral neck (Fig 6). Movement of the ultrasound transducer is conducted to identify the superior and inferior portions of the femoral neck. The central to lower third of the femoral neck is selected for placement of the camera portal, and the femoral head-neck junction is identified by its curved contour. The initial portal needle is placed under ultrasound guidance into this location and developed using a cannulated instrument technique as in the central-compartment procedure (Fig 7, Video 1). A 70° arthroscope is introduced into the peripheral compartment, and the lens is rotated in a superior direction to allow clear visualization of the reduced hip and anterior surface of the femoral neck. The articular portion of the femoral head can be seen to curve underneath the labrum into the acetabulum. The peripheral-compartment working portal is placed at right angles to the line of the femoral neck, running from a superior direction, and is developed under direct vision, although ultrasound may be used to assist when necessary.
Fig 6.

Transducer position for peripheral-compartment initial portal placement—longitudinal view along femoral neck. (ASIS, anterior superior iliac spine; GT, greater trochanter.)
Fig 7.
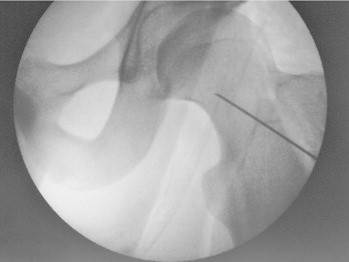
Fluroscopic image demonstrating location of initial (camera) portal placement for peripheral compartment procedures. We now rarely use fluroscopy for peripheral compartment procedures at our institution.
Discussion
Ultrasound guidance for the development of hip arthroscopic portals is a relatively easy technique that we recommend to surgeons who perform hip arthroscopy on a regular basis (Table 1). We find this technique fast to conduct and very reliable. Since developing the technique, we have used fluoroscopy very seldom in our practice, although simultaneous fluoroscopic evaluation can easily be conducted when required. Our rate of iatrogenic arthroscopic injury to the femoral head or labrum is less than 1% to 2%. Even in hips in which it is difficult to achieve distraction, ultrasound guidance is accurate enough to be able to provide safe access to the joint. One of the advantages of ultrasound guidance is that the surgeon is able to visualize his or her portal placement in 3 dimensions such that the portals may be developed in a more posterior position, which would be somewhat more difficult with the use of fluoroscopy (Fig 8). This enables the surgeon to be able to identify the area of the joint that has the greatest gap for the passage of arthroscopic instruments, thereby reducing the risk of iatrogenic damage. This is particularly useful in patients with hips that are difficult to distract because of soft-tissue stiffness. A more posterior position for the arthroscope within the hip joint in central-compartment procedures also assists in visualizing the cartilage and labral disorders that are situated more superior in the joint at the 12-o'clock region.
Table 1.
Tips for Introducing Ultrasound into Hip Arthroscopy Practice
| The ultrasound and probe require clarity at 10 to 12 cm of depth. |
| Attend training in ultrasound prior. |
| Understand use of your specific ultrasound machine and transducer. |
| The surgeon should use combined ultrasound and fluoroscopy for his or her first 30 cases. |
| The light-saber sign is an accurately identifiable feature when the hip is under traction. |
Fig 8.
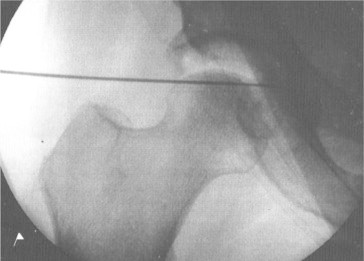
Fluroscopic image of posterior trochanteric central compartment (camera) portal, originally placed under ultrasound guidance. A more posterior position behind the femoral head is easy to obtain using ultrasound which may assist in treating superior acetabular cartilage lesions. We now rarely use fluroscopy for central compartment procedures at our institution.
Our initial experience with ultrasound-guided hip arthroscopy was undertaken without prior training specifically in the technique. We undertook a musculoskeletal ultrasound education course through a recognized ultrasound training facility (Australian Institute of Ultrasound, Queensland, Australia) before using ultrasound in the operating theater. We would recommend a sound understanding of the application and limitations of ultrasound before performing this technique. Furthermore, our initial 30 procedures were undertaken with combined ultrasound and fluoroscopic guidance to ensure patient safety, and we would recommend this staged introduction for surgeons first undertaking this technique. With greater experience, fluoroscopy can then be omitted.
The limitations of ultrasound for hip arthroscopy relate to the inability to obtain clear vision of the joint. This can be encountered in patients who are obese and in part relates to the adequacy of the ultrasound machine available. In our practice, with the equipment that we have available, a soft-tissue envelope of greater than 10 cm often presents poorer image quality. In addition, in situations in which a large effusion is seen, the radiographic landmark of the light-saber sign is not seen. In these situations, however, the femoral head usually can be seen more in its entirety because the fluid within the joint will transmit ultrasound echoes. Although the absence of the light-saber sign does not interfere with the accurate use of ultrasound in hip arthroscopy, the difference in the visual appearance of the joint must be taken into consideration. A further limitation of ultrasound is that when the initial needle is placed and the vacuum is released, the appearance of the hip joint air–capsule interface changes. This can make subsequent repositioning of the needle more difficult; however, we have found repositioning to be rarely necessary.
In summary, we describe a technique of ultrasound-assisted hip arthroscopy that is technically simple and very reproducible for the management of both central- and peripheral-compartment procedures.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Ultrasound Hip Arthroscopy
References
- 1.Hua Y., Yang Y., Chen S. Ultrasound-guided establishment of hip arthroscopy portals. Arthroscopy. 2009;25:1491–1495. doi: 10.1016/j.arthro.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Weinrauch P., Kermeci S. Ultrasonography-assisted proximal iliotibial band release and trochanteric bursectomy. Arthrosc Tech. 2013;2:e433–e435. doi: 10.1016/j.eats.2013.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Ultrasound Hip Arthroscopy


