Abstract
Reconstruction of the medial patellofemoral ligament (MPFL) has recently become a popular procedure for children and adolescents with patellofemoral instability. Nevertheless, high complication rates of up to 26% have been reported. The traditionally used technique requires patellar bone tunnels that may place the proportionately smaller patella at higher risk of fracture. Because of the adjacent physis of the femoral insertion, anatomic reconstruction of the MPFL has the risk of injury to the growth plate. This technical report therefore presents a technique for anatomic reconstruction of the MPFL in a skeletally immature population using a pedicled superficial quadriceps tendon graft, hardware-free patellar graft attachment, and anatomic femoral fixation distal to the femoral physis. The advantages of this technique include avoidance of bony patellar complications, an anatomically truer reconstruction, a single incision, and sparing of the hamstring tendons for reconstruction of any future ligamentous injuries.
The medial patellofemoral ligament (MPFL) has been shown to be the primary medial static soft-tissue stabilizer of the patellofemoral joint. Reconstruction of this ligament has therefore become a popular procedure for the treatment of patellar instability in adults, with numerous methods described in the literature. Anecdotally, the most widespread method of MPFL reconstruction in Europe involves the harvesting of a free gracilis or semitendinosus graft, with bony patellar fixation. This method, though successful, has numerous documented complications, with an overall failure rate of up to 26%.1-3
Over recent years, however, a small number of technical reports have described the use of the ipsilateral quadriceps tendon in reconstruction of the MPFL in adults.4,5 Potential advantages of using the quadriceps tendon over the traditional approach include a single incision, avoidance of bony patellar complications, an anatomically truer reconstruction, cost savings, and sparing of the gracilis and semitendinosus tendons for reconstruction of any future ligamentous injuries.
The aforementioned advantages make a technique that uses the quadriceps tendon particularly attractive in a skeletally immature population in whom additional challenges are present. The open femoral physis poses a challenge for femoral fixation regardless of graft origin; however, a safe, growth-preserving technique is also possible using this pedicled quadriceps technique. The traditionally used technique requires patellar bone tunnels that may place the proportionately smaller patella at higher risk of fracture. In addition, the thick cord-like nature of a free hamstring graft may cause increased soft-tissue irritation in an immature population compared with the flatter aponeurotic quadriceps tendon.
This technical report presents a technique for anatomic reconstruction of the MPFL in a skeletally immature population using a pedicled superficial quadriceps tendon graft, hardware-free patellar graft attachment, and anatomic femoral fixation distal to the femoral physis.
Surgical Technique
Before surgery, every patient is examined under anesthesia, and a diagnostic arthroscopy is performed to evaluate and treat intra-articular pathology such as patellofemoral cartilage injuries. An additional superolateral arthroscopy portal is used to evaluate the patellofemoral joint throughout a full range of motion, which importantly may identify cases of trochlear dysplasia that were missed by magnetic resonance imaging or in which magnetic resonance imaging was not performed.
A longitudinal incision is made beginning inferiorly at the superomedial border of the patella (Fig 1). In our experience a modest incision length of 4 to 5 cm is adequate because the distance from the superior patellar pole to the myoaponeurotic junction of the quadriceps is 8 to 10 cm in adults.
Fig 1.

The skin incision is made at the superomedial border of the patella. In our experience a modest incision length of 4 to 5 cm is adequate.
The subcutaneous tissues are divided to expose the quadriceps fascia and tendon (Video 1). The 4 muscular elements of the quadriceps fuse to form the quadriceps tendon approximately 2 cm proximal to the patella.6 The initial superficial vertical incision is thus made 2 to 3 cm proximal to the superior patellar pole because the superficial slip of the tendon is easiest to differentiate at this level.6 In addition, the incision is made 2 to 4 mm lateral to the border of the vastus medialis, thus preserving a thin strip of the medial tendon (Fig 2A). The second vertical incision is made into the tendon approximately 12 to 15 mm lateral to the first, thus determining the width of the graft (Fig 2B).
Fig 2.
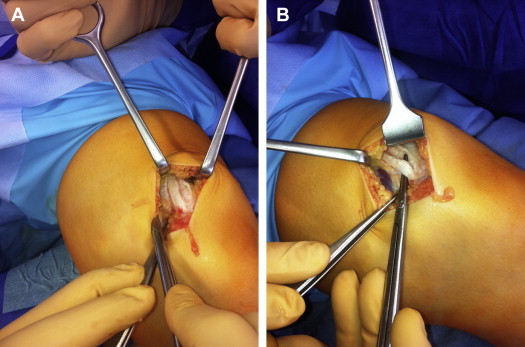
(A) The incision is made 2 to 4 mm lateral to the border of the vastus medialis, thus preserving a thin strip of the medial tendon. The superficial slip of the quadriceps tendon is elevated from the deeper tendon. (B) Staying in the same plane, the graft is then carefully dissected superiorly, keeping the middle and deep laminae intact.
By use of forceps and scissors, the most superficial layer of the quadriceps tendon is elevated from the deeper tendon (Fig 2B). Staying in the same plane, the graft is then carefully dissected superiorly, as far as the musculotendinous junction of the rectus femoris if possible. Occasionally, small fibers between the layers have to be dissected. During superior dissection of the graft, the assistant uses Langenbeck retractors to provide adequate superior exposure despite the conservative skin incision.
The graft is divided at its superior end and reflected to expose the posterior surface. Harvesting of the graft then continues distally to a point over the proximal patellar third. The superficial slip of the quadriceps tendon inserts into the anterior portion of the base and the superior third of the anterior surface of the patella. Dissection continues slightly further on the lateral side to a distance approximating the graft width. This creates a diagonal axis around which the pedicled graft may be reflected 180° and rotated 90° toward medial (Fig 3). Care is taken not to accidentally divide the graft at its inferior attachment to the patella during dissection. The total length of the graft should not be less than 9 cm to allow enough length for the femoral fixation with an interference screw (Fig 4).
Fig 3.

The pedicled graft is reflected 180° and rotated 90° toward medial. Care is taken not to accidentally divide the graft at its inferior attachment to the patella during dissection. The free end of the graft is prepared with a Vicryl suture.
Fig 4.

The graft matches the native MPFL, which is a thin, broad, sheet-like ligament. The length of the graft measures approximately 9 cm. The width of the graft is approximately 10 mm, which resembles the width of the original MPFL.
The free end of the graft is prepared with a nonabsorbable suture (No. 2 Sulene; Serag-Wiessner, Naila, Germany) by use of a baseball-suture technique (Fig 3). By blunt dissection, the interval between the capsule and the vastus medialis obliquus is developed to the femoral insertion of the MPFL. By use of the indirect radiographic method described by Schöttle et al.,7 the anatomic femoral insertion of the MPFL is identified under fluoroscopic control. Because of the concave curvature of the distal femoral physis, the lateral radiograph alone can be misleading for the determination of the relation between the distal femoral physis and the MPFL.8 The cross reference onto an anteroposterior view shows that the same point that is projected on or proximal to the physis on the lateral view is distal to the physis on the anteroposterior view.8
A guidewire is placed at the femoral insertion. After verification of the entry point in both the anteroposterior and true lateral planes, the guide pin is drilled to the lateral condyle. The guidewire is aimed toward an exit point on the anterolateral femur to avoid the neurovascular structures of the popliteal groove or popliteal fossa. A blind-ending tunnel (size, 6 mm) is then drilled into the medial femur along the guidewire (size, 2.4 mm) to a depth that will allow sufficient pull of the free end of the graft.
For additional soft-tissue support, the graft can usually be tunneled under a thin section of the medial retinaculum before the entry point of the medial capsular tunnel. The graft is then pulled between the second and third medial layers to the femoral insertion point. The reflected graft surface should remain outward facing to prevent twisting and preserve the flatness of the graft in line with the anatomic MPFL.
A locking suture (Biosure HA Interference Screw, 6 mm × 25 mm; Smith & Nephew, Andover, MA) is passed through the transepicondylar axis, pulling the graft into the medial tunnel. The knee is cycled several times from full flexion to full extension with the graft under tension, thus pre-stretching the graft. A controlled pull is kept on the graft using the contralateral side as a reference, and the graft is then secured within the medial condyle tunnel with a bioresorbable interference screw with the knee flexed to 30° (Fig 5).
Fig 5.

A bioresorbable interference screw is used to secure the quadriceps graft within the medial condyle tunnel with the knee flexed to 30°. Reprinted with permission.12
The base of the graft is secured to the medial patella with additional subperiosteal Vicryl sutures (Ethicon, Somerville, NJ) to ensure that abnormal rotational forces on the anterior patella are avoided. Vicryl sutures may also be used to close or adapt the incised quadriceps tendon, which has the additional beneficial effect of slight medialization of the tendon.
The aponeurosis of the vastus medialis obliquus is sutured back to the patella with Vicryl, with further closure of the subcutaneous tissues and skin. Routine dressings and bandages are applied.
Rehabilitation
Postoperatively, partial weight bearing using crutches is allowed. Active and passive flexion and extension exercises, strengthening of the vastus medialis muscle, and straight-leg raise are prescribed. After 2 weeks, full weight bearing is allowed. Neuromuscular training is recommended, and return to sports is allowed after 3 months.
Discussion
For children with recurrent patellar instability, reconstruction of the MPFL is a valid and effective procedure. In a recent review, Vavken et al.9 found that in pediatric and adolescent patients with normal or restored knee anatomy, reconstruction of the MPFL is the most effective treatment option. The 2-bundle technique using a free gracilis tendon graft remains the standard of care in Europe. Although this technique has shown good results in adolescents and adults, its use in children remains controversial because of the requirement for both femoral and patellar bony fixation in patients with open growth plates.9,10
When the free hamstring graft approach is used, a method of attaching the graft to the medial patella is required. Numerous methods of graft fixation, both with hardware and hardware free, using variations in drill-hole techniques have been described in the literature.1-3 Regardless of the drill-tunnel technique, however, all of these methods have in common the necessity to breach the integrity of the patellar cortex, the reduction of the patellar bone substance, and the associated potential for subsequent bony complications.
In children, who have relatively smaller patellae compared with adults, the risk of fracturing the bone bridge between the 2 tunnels while drilling presents a significant challenge. In addition, violation of the chondral surface has also been reported when using a drill-hole fixation technique.1-3 In a systematic re view of the literature, Shah et al.3 found an overall cumulative complication rate of 26.1%, with patellar fracture being one of the major complications.
Therefore, one of the major advantages of a pedicled quadriceps technique, which keeps the patellar attachment of the quadriceps graft intact, is the removal of the need for drill holes or hardware insertion into the patella of the growing child, thus indirectly eliminating bony patellar complications. Whereas there are various techniques described in the literature using a free gracilis tendon graft, to our knowledge, this is the first study describing a technique for reconstruction of the MPFL using a pedicled quadriceps tendon graft in children.
There are numerous additional advantages that make the described technique a favorable alternative to the traditional free graft approach in children. Compared with the cord-like hamstring graft, the superficial quadriceps graft is a much closer approximation of the anatomy of the native MPFL, which is a thin, broad, sheet-like ligament.5,11 Several authors have emphasized that an ideal graft should be as similar in stiffness and strength to the native MPFL as possible to avoid overload and overstress on the patella.5 Using the technique described in this report, the surgeon creates a graft that is 12 to 15 mm in width and 90 to 100 mm in length and matches the thickness of the superficial quadriceps slip, which is 2 to 3 mm in our experience (Fig 4). These dimensions correspond well to those of the healthy MPFL as described by Baldwin.11 Namely, the patellar MPFL insertion is 28.2 ± 5.6 mm wide, the femoral MPFL insertion is 10.6 ± 2.9 mm wide, and as found in another study, the length of the ligament averages 10.6 ± 2.9 mm.11
Conversely, a hamstring graft is much stiffer and stronger than the native MPFL; thus even minimal malpositioning or overtensioning of the graft may lead to increased stress on the patellofemoral joint.1,2,9 Furthermore, embryologically, the MPFL and quadriceps tendon are from the ventral mesenchyme, as opposed to the hamstring tendons, which belong to the dorsal mesenchyme.5
Economically, the described technique is advantageous because there are no implants required for medial patellar fixation (Tables 1-3). Cosmetically, one less skin incision is required because the harvesting of the quadriceps tendon is carried out through the same longitudinal incision over the medial proximal two-thirds of the patella that is needed for reconstruction of the MPFL (Fig 6). Another theoretical advantage of this technique is that the ipsilateral gracilis and semitendinosus tendons are spared for potential use in the reconstruction of future ligamentous injuries.
Table 1.
Main Steps of MPFL Reconstruction Technique With Pedicled Quadriceps Tendon Graft
| 1. Diagnostic arthroscopy is performed to rule out intra-articular injuries. |
| 2. Exposure of the quadriceps tendon is performed with a skin incision length of 4 to 5 cm. |
| 3. A superficial vertical incision is made 2 to 3 cm superior to the proximal patellar pole. |
| 4. Harvesting of the superficial layer of the quadriceps tendon with a length of 9 cm is performed. |
| 5. The pedicled graft is reflected 180° and rotated 90° toward medial. |
| 6. The interval between the capsule and the vastus medialis obliquus is developed to the femoral insertion of the MPFL. |
| 7. The graft is pulled between the second and third medial layers to the femoral insertion point. |
| 8. The anatomic femoral insertion distal to the femoral physis is identified by fluoroscopy on a true lateral view of the knee for anatomic placement of the graft. |
| 9. The guide pin is drilled to the anterolateral condyle to avoid the neurovascular structures of the popliteal groove or popliteal fossa. |
| 10. A blind-ending tunnel is drilled into the medial femur along the guidewire. |
| 11. The knee is cycled several times from full flexion to full extension with the graft under tension, thus pre-stretching the graft. |
| 12. The graft is secured within the medial condyle with the knee flexed to 30°. |
Table 2.
Tips, Pearls, Contraindications, and Pitfalls
| Tips and pearls |
| Make the vertical incision 2 to 3 cm proximal to the superior patellar pole because the superficial slip of the tendon is easiest to differentiate at this level. |
| During superior dissection of the graft, provide adequate superior exposure to achieve an adequate length of graft. |
| Try to identify the femoral insertion under fluoroscopy; a true lateral view is necessary to accurately place the drill hole. |
| Aim the guidewire toward an exit point on the anterolateral femur to avoid the neurovascular structures of the popliteal groove. |
| Secure the graft within the medial condyle tunnel with the knee flexed to 30° to avoid overtensioning. |
| Contraindications |
| If additional risk factors such as torsional malalignment are not taken into consideration, the reconstruction is prone to failure. |
| MPFL reconstruction with the quadriceps tendon is more likely to fail in patients with severe trochlear dysplasia. |
| In patients with congenital dislocation of the patella, an additional soft-tissue release is necessary. |
| Pitfalls |
| Inadequate dissection can be performed, resulting in a graft that is too short. |
| In patients with severe trochlear dysplasia, secondary trochleoplasty after closure of the growth plate might be necessary. |
| Weakening of the graft at the patellar insertion is possible. |
| Overtensioning of the graft can occur. |
| Injury to the distal femoral physis with subsequent growth disturbance is possible. |
Table 3.
Advantages and Disadvantages
| Advantages |
| Avoidance of bony patellar complications |
| No violation of chondral surface |
| Anatomically truer reconstruction |
| Cost savings because of hardware-free patellar graft attachment |
| Sparing of gracilis and semitendinosus tendons for reconstruction of any future ligamentous injuries |
| Disadvantages |
| Meticulous dissection of the quadriceps tendon is necessary. |
| Intraoperative fluoroscopy is required. |
| In patients with severe trochlear dysplasia, secondary trochleoplasty after closure of the growth plate may be necessary. |
| Weakening of the graft at the patellar insertion is possible. |
| Overtensioning of the graft can occur. |
| Injury to the distal femoral physis with subsequent growth disturbance is possible. |
Fig 6.

Closure of wound, which typically has a length of 4 to 5 cm.
The challenge of femoral fixation of MPFL grafts in children and adolescents has been widely discussed in the literature. Because the distal femoral physis provides 70% of the growth of the femur, different dynamic femoral fixation techniques have been described that attempt to avoid iatrogenic violation of the physis. None of the described techniques is strictly anatomic, however, because they use the femoral insertion of the medial collateral ligament or of the adductor magnus tendon as a reference for the femoral insertion of the MPFL. Conversely, other authors have shown that the insertion of the MPFL is typically between 5 mm and 6.4 mm distal to the femoral physis.8,12 Thus there is enough room for secure and safe placement of a suture anchor or tunnel in an anatomic location, as described in this report, without jeopardizing growth.8,9
Whereas other authors have described the use of the quadriceps tendon in reconstruction of the MPFL, we believe that this report is the first to describe the use of the superficial quadriceps slip in combination with anatomic femoral fixation that respects open growth plates in a young population.
Earlier accounts of quadriceps-based MPFL reconstruction describe the use of a full- or partial-thickness quadriceps tendon autograft, from the central one-third of the tendon. It is our opinion, in line with the findings of Goyal,5 that harvesting of only the medial superficial-most layer of the quadriceps tendon, preserving a thin strip of the insertion of the vastus medialis, is preferable because this is less likely to weaken the extensor mechanism and provides an ideal graft. Compared with the report by Goyal, we present a number of refinements to the technique including an emphasis on a conservative skin incision, the importance of securing the MPFL graft to the medial patella using supplementary periosteal sutures, and femoral anatomic fixation distal to the physis.
The described technique for MPFL reconstruction in children and adolescents with a pedicled superficial quadriceps tendon graft allows anatomic femoral and patellar fixation of the graft. A major advantage of the quadriceps technique is that no hardware fixation or bony procedure involving the patella is necessary, making it ideal for use in children with relatively underdeveloped patellae. The anatomic femoral aperture fixation respects the distal femoral physis and provides a safe fixation of the graft distal to the femoral physis. Pending long-term outcome studies, the pedicled superficial quadriceps technique offers an attractive alternative for MPFL reconstruction, especially in a skeletally immature patient population.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Anatomic reconstruction of MPFL using pedicled quadriceps tendon graft.
References
- 1.Bollier M., Fulkerson J., Cosgarea A., Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011;27:1153–1159. doi: 10.1016/j.arthro.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 2.Parikh S.N., Nathan S.T., Wall E.J., Eismann E.A. Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med. 2013;41:1030–1038. doi: 10.1177/0363546513482085. [DOI] [PubMed] [Google Scholar]
- 3.Shah J.N., Howard J.S., Flanigan D.C., Brophy R.H., Carey J.L., Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fulkerson J.P., Edgar C. Medial quadriceps tendon-femoral ligament: Surgical anatomy and reconstruction technique to prevent patella instability. Arthrosc Tech. 2013;12:e125–e128. doi: 10.1016/j.eats.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goyal D. Medial patellofemoral ligament reconstruction: The superficial quad technique. Am J Sports Med. 2013;41:1022–1029. doi: 10.1177/0363546513477828. [DOI] [PubMed] [Google Scholar]
- 6.Waligora A.C., Johanson N.A., Hirsch B.E. Clinical anatomy of the quadriceps femoris and extensor apparatus of the knee. Clin Orthop Relat Res. 2009;467:3297–3306. doi: 10.1007/s11999-009-1052-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schöttle P.B., Schmeling A., Rosenstiel N., Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 8.Nelitz M., Dornacher D., Dreyhaupt J., Reichel H., Lippacher S. The relation of the distal femoral physis and the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2011;19:2067–2071. doi: 10.1007/s00167-011-1548-3. [DOI] [PubMed] [Google Scholar]
- 9.Vavken P., Wimmer M.D., Camathias C., Quidde J., Valderrabano V., Pagenstert G. Treating patella instability in skeletally immature patients. Arthroscopy. 2013;29:1410–1422. doi: 10.1016/j.arthro.2013.03.075. [DOI] [PubMed] [Google Scholar]
- 10.Nelitz M., Dreyhaupt J., Reichel H., Woelfle J., Lippacher S. Anatomical reconstruction of the medial patellofemoral ligament in children and adolescents with open growth-plates: Surgical technique and clinical outcome. Am J Sports Med. 2013;41:58–63. doi: 10.1177/0363546512463683. [DOI] [PubMed] [Google Scholar]
- 11.Baldwin J.L. The anatomy of the medial patellofemoral ligament. Am J Sports Med. 2009;37:2355–2361. doi: 10.1177/0363546509339909. [DOI] [PubMed] [Google Scholar]
- 12.Kepler C.K., Bogner E.A., Hammoud S., Malcolmson G., Potter H.G., Green D.W. Zone of injury of the medial patellofemoral ligament after acute patellar dislocation in children and adolescents. Am J Sports Med. 2011;39:1444–1449. doi: 10.1177/0363546510397174. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Anatomic reconstruction of MPFL using pedicled quadriceps tendon graft.


