Abstract
Background
Patient recruitment is one of the most difficult aspects of clinical trials, especially for research involving elderly subjects. In this paper, we describe our experience with patient recruitment for the behavioral intervention randomized trial, "The relaxation response intervention for chronic heart failure (RRCHF)." Particularly, we identify factors that, according to patient reports, motivated study participation.
Methods
The RRCHF was a three-armed, randomized controlled trial designed to evaluate the efficacy and cost of a 15-week relaxation response intervention on veterans with chronic heart failure. Patients from the Veterans Affairs (VA) Boston Healthcare System in the United States were recruited in the clinic and by telephone. Patients' reasons for rejecting the study participation were recorded during the screening. A qualitative sub-study in the trial consisted of telephone interviews of participating patients about their experiences in the study. The qualitative study included the first 57 patients who completed the intervention and/or the first follow-up outcome measures. Factors that distinguished patients who consented from those who refused study participation were identified using a t-test or a chi-square test. The reason for study participation was abstracted from the qualitative interview.
Results
We successfully consented 134 patients, slightly more than our target number, in 27 months. Ninety-five of the consented patients enrolled in the study. The enrollment rate among the patients approached was 18% through clinic and 6% through telephone recruitment. The most commonly cited reason for declining study participation given by patients recruited in the clinic was 'Lives Too Far Away'; for patients recruited by telephone it was 'Not Interested in the Study'. One factor that significantly distinguished patients who consented from patients who declined was the distance between their residence and the study site (t-test: p < .001). The most frequently reported reason for study participation was some benefit to the patient him/herself. Other reasons included helping others, being grateful to the VA, positive comments by trusted professionals, certain characteristics of the recruiter, and monetary compensation.
Conclusions
The enrollment rate was low primarily because of travel considerations, but we were able to identify and highlight valuable information for planning recruitment for future similar studies.
Background
Patient recruitment in clinical trials is recognized as one of the most difficult aspects of the study process [1,2]. Recruitment among elderly patients who have chronic diseases poses particular challenges [3-7]. Studies have identified that transportation is a specific issue in recruitment of the elderly [1,8]. A trial that requires frequent travel for a behavioral intervention at a study site, which can be a long distance away from the patient's residence, adds difficulties to recruitment among the elderly [7]. These two complicating factors increased the recruitment challenges in the clinical trial, "The relaxation response intervention for chronic heart failure (RRCHF)."
The RRCHF was a three-armed, randomized controlled trial designed to evaluate the efficacy and cost of a 15-week relaxation response intervention conducted on veterans with chronic heart failure (CHF). The relaxation response is a state in which individuals evoke a bodily calm that has the opposite effect of the fight-or-flight response, with concomitant favorable physiological changes. Studies have shown that the relaxation response is effective in managing various medical conditions including hypertension, insomnia, anxiety, and depression [9-14].
The primary aim of the RRCHF was to evaluate the efficacy of the relaxation response in the improvement of the cardiac function and quality of life of CHF patients. Two control groups were used: a 15-week cardiac education group and a usual care group. The original plan was to recruit a total of 120 patients in 14 months to be randomized into the three study groups with equal numbers in each group. A number of factors contributed to the challenge in patient recruitment for this study: 1. strict inclusion criteria in cardiac function status limiting the number of potentially eligible patients; 2. high comorbidity among Veterans Affairs (VA) patients increasing the burden to patients of time spent receiving care or participating in a study; 3. the age of VA patients with CHF making travel to the hospital for the intervention an issue due to either the lack of the means of transportation or an inability to drive; 4. the large catchment areas of the VA acute care hospital at which we were conducting the study, potentially requiring study subjects to travel long distances to the study site; 5. study protocol requiring 15 weeks of group attendance in the hospital, which can be a burden for the elderly with numerous comorbidities; and 6. one of the study outcomes requiring a bike test, which is not possible for some patients due to disability or certain heart conditions.
Despite the challenges we faced in patient recruitment for this behavioral intervention trial, we successfully recruited the target number of patients. In this article we describe the experience in patient recruitment for this trial, including the steps we took to modify the recruitment strategies. We document reasons patients gave for refusing to participate in the study, and we discuss factors that are associated with agreeing to participate. We also identify factors that motivated participation in the study based on a qualitative sub-study. What we learned in this study is helpful for planning future studies with similar features.
Methods
Study design
The study design consisted of a randomized clinical trial that included three study groups: relaxation response, cardiac education, and usual care. The cardiac education group was used as a comparison intervention to the study intervention, relaxation response. The education group also served as a control group in order to eliminate possible effects associated with group meetings and for patients' expectations for improvement simply by participating in the intervention (Hawthorne Effect). This study was approved by the institutional review boards at the VA Boston Healthcare System and the VA New England Health Care Bedford division.
Study population inclusion and exclusion criteria
The targeted patient population in this study consisted of ambulatory CHF patients of either gender and any race who visited the VA Boston Health Care System at the campuses of either Jamaica Plain or West Roxbury during the study period and who met the following inclusion criteria: 1) moderate levels of symptom severity (a New York Heart Association classification of II or III); 2) left ventricular ejection fraction (LVEF) ≤ 40%; and 3) undergoing pharmacological treatments according to established clinical guidelines (i.e., ACE inhibitors and the more recently recommended drug treatment, β-blockers). However in the early stage of patient recruitment, we noticed that a substantial number of patients were not under the treatment of ACE inhibitors or β-blockers, we therefore dropped the inclusion criteria on medication treatment. The exclusion criteria were: 1) participation in a rehabilitation program that included exercise training and an education group; and 2) cognitive impairment as measured by the Mini Mental Status Examination (MMSE), a reliable and valid screening instrument for the detection of cognitive impairment. A commonly used cut-off point of 24 (<24) on the MMSE was used to identify patients as cognitively impaired.
Clinical sites
The CHF clinic in the VA Boston Healthcare System was the primary recruitment site. The chief of the clinic at the time during the study period was one of the co-investigators of the study. She facilitated study recruitment by helping to identify potentially eligible patients in her clinic and informing patients about the study. After a few months of recruitment, it became apparent that the recruitment rate was lower than expected and that the CHF clinic did not provide enough potentially eligible patients for the study. We therefore extended the recruitment sites, first to all the cardiology clinics and then to the primary care clinics to capture CHF patients who visited those clinics.
Recruitment methods
Clinic recruitment
We first identified patients with a CHF diagnosis (ICD-9 codes of 428, 428.0, 428.1, and 428.9) based on the diagnoses listed in the VA medical centers' outpatient database that contains all diagnostic and procedural information routinely collected in the VA hospitals. We then obtained the information on the LVEF from the computer files in the VA to screen patients for the eligibility criteria of LVEF ≤ 40%. The LVEF information was available only for those patients who took at least one of three tests: catheterization, echocardiogram and radionuclide ventriculogram. Referencing lists of potential study participants, the recruiters approached the patients when they came to the clinics for their regularly scheduled appointments. The physicians and nurses in the clinics, informed about the study, also assisted in referring patients for recruitment. Due to the budget constraints and the limited availability of the recruiters, not all the clinic days were covered for patient recruitment. Since there was no systematic pattern of choosing the days for recruitment, no selection bias was expected.
Telephone recruitment
Approximately one year after the clinic recruitment started, we added telephone recruitment to the protocol in an effort to increase the recruitment rate. The patients who were targeted for telephone recruitment were those with a CHF diagnosis and LVEF ≤ 40% who had visited the hospitals in the VA Boston Health Care System at least once in the past year and had not been screened in the clinic for the study. We sent letters to the targeted patients to inform them of the study and then followed-up with phone calls to recruit them into the study. Patients were given the option to return postcards if they did not want to receive the phone calls. Those patients who expressed interest in study participation over the phone were scheduled to come in to the clinic for further screening based on cognitive impairment. The Mini Mental Status Examination, requiring an in-person interview, was used to determine eligibility.
Flyers
Recruitment flyers were posted in the Jamaica Plain and West Roxbury campuses of the VA Boston Health Care System. We selected those two locations exclusively because we had access to the required LVEF data only for patients who visited those two hospitals. Patients who visited those two facilities were also more likely to participate in the study because they were the specified sites for the study.
Recruitment monitoring
The recruitment statistics were generated monthly and presented to the co-investigators of the study and to the recruiters. The statistics included the total number of appointments of CHF patients in the clinics, the number of patients to be screened (those with LVEF ≤ 40%), the number of "no show" patients, the number of patients screened, and the number of patients who consented and enrolled. Patients were defined as having consented to participate in the study when they signed the consent forms. "Enrolled" patients were those who consented and completed the baseline assessments. Enrolled patients were randomly assigned to one of the 3 study groups: relaxation response, cardiac education, and usual care groups.
Study intervention
Enrolled patients who were randomized into the relaxation response group were required to attend a 90-minute group session each week for 15 weeks to learn various techniques to elicit the relaxation response. The techniques are breathing awareness, mental repetition of a word, sound, phrase, or prayer, mindfulness meditation, guided body scan, progressive muscle relaxation, and guided imagery. Three tapes with instructions on each of these techniques were used in the group sessions. Patients were also asked to practice the techniques at home for 15 to 20 minutes twice a day using these tapes.
Cardiac education program
Enrolled patients who were randomized into the cardiac education group were required to attend a 90-minute cardiac education lecture each week for 15 weeks. This education group was organized by the cardiac rehabilitation education program at the VA Boston Health Care System. The speakers of this ongoing education program are experts in each of the topic areas. The topics included medical, pharmaceutical, life style, nutrition, and psychosocial issues affecting people with heart disease and related conditions.
Usual care
Patients who were randomly assigned to the usual care group were not required to attend any group session. However, similar to patients in the relaxation response and education groups, they were expected to complete the questionnaires and undergo the exercise test at baseline, 15 week, 6 month and 12 month follow-up.
Patient compensation
To compensate the time and efforts patients spend for the study, patients were reimbursed with $50 for completing the first half of the study (baseline and first follow-up assessments) and again another $50 after the completion of the whole 12-month study. Participants were also reimbursed for the mileages traveled to the study sites for attending group sessions or bicycle exercise tests.
Data collection and data analysis
Patient demographic characteristics, address (used to calculate the distance between the patients' residence and the study clinical site), LVEF, and cardiac medication prescriptions were collected during screening and from the VA administrative database. A t-test and a chi-square test were used to compare between patients consented and refused as well as between patients enrolled and withdrawn after consenting.
A qualitative study was added approximately one year after the recruitment started. The first fifty-seven patients who finished the study intervention and/or the first follow-up outcome assessment were included in the qualitative study. Among these 57 patients, 21 were in the relaxation response group, 21 were in the education group and 15 were in the usual care group. These patients were interviewed by telephone about their experiences in the study. An open-ended question was included in the interview about the reasons for their participating in the study. All interviews were audio-taped, transcribed, and the data were analyzed. A content analysis was conducted by two study staff who independently coded and categorized the reasons for study participation. The two coders reached almost perfect agreement. The few instances of disagreement in coding were resolved in group discussions by the team.
Results
Enrollment rates
Clinic recruitment
The clinic recruitment period lasted for two years and three months, starting in April 2000 and ending in June 2002. This recruitment period was extended from the original planned 14 months due to the lower than expected recruitment rate.
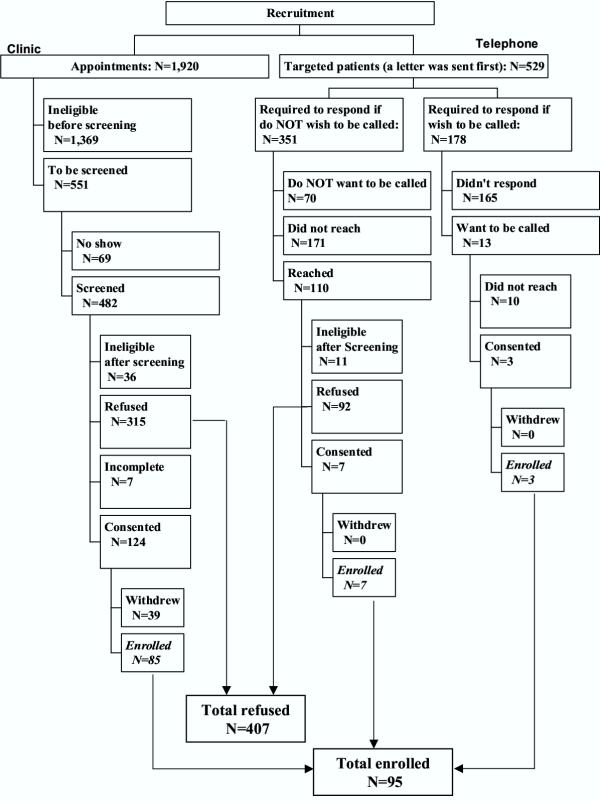
A total of 1,920 CHF patients had appointments on the recruitment days in the targeted study clinics (Figure 1). Among these patients, approximately 29% were eligible. A high LVEF and the unavailability of LVEF were the two main reasons for ineligibility (67% and 27%, respectively). These patients were classified as ineligible before screening. The total number of patients who remained eligible for clinic screening was 551. Of these patients, a total of 482 were screened; sixty-nine did not show up on any of the recruitment days. Among the screened patients, 315 (65%) declined, and 124 (26%) consented to participate in the study. A small percentage (N = 36, 7%) of patients were screened as ineligible for the following three main reasons: 1. New York Heart Association Classification of I or IV indicating mild and severe disease symptomatology (37%); 2. currently practicing relaxation response (18%); and 3. currently enrolled in a cardiac rehabilitation program (16%). Seven patients did not complete the screening and could not be reached afterward.
Figure 1.
Flow Diagram of Patient Recruitment
Of the 124 patients who signed the informed consent form at the time of recruitment, 31% (N = 39) did not come back for the baseline assessment. These patients were considered as withdrawing before enrollment. In follow-up calls, patients gave three main reasons for not continuing with the study: 1. health concerns/too sick; 2. too busy/schedule conflicts with the group meeting times; and 3. lost interest in the study. We calculated the enrollment rate as the number of patients who completed the baseline assessment (so called "enrolled patients") over the total number of patients screened in the clinic. The enrollment rate in the clinic was 18% (85/482).
Telephone recruitment
Most of the telephone recruitment was conducted during a three-month period from February through April, 2001. During this time period, letters were sent to 351 target patients inviting them to participate in the study. (See Methods section for the targeted patient criteria.) Seventy patients returned the postcard indicating they did not wish to be called. Telephone recruiters for the study were able to reach 110 patients by phone to invite them to join the study. Among them, only seven agreed to participate and were enrolled in the study. The enrolled rate was 6%, calculated as seven enrolled among 110 contacted by phone. Due to this low yield rate, the rest of the 178 target patients were mailed letters asking them to mail back the enclosed postcard if they were interested in receiving a phone call to learn about the study. Among them, only thirteen (7%) showed an interest by returning the postcard, and only three of those thirteen enrolled in the study. The enrollment rate was 2% when calculated as three patients enrolled among 178 patients who were mailed a letter.
Flyer
Only a small number of patients responded to the flyer. None of these patients was eligible due either to a high LVEF or not having a CHF diagnosis.
Reasons for refusing to participate in the study
We documented the reasons patients gave during recruitment for refusing to participate in the study. These reasons were given by patients unprompted. The reasons given by patients screened in the clinics were grouped into six general categories: 1. lives too far away (26%); 2. time constraints (22%), including too busy, too many appointments, and works on the day the study group meets; 3. not interested in the study (19%); 4. health problems (12%); 5. transportation problems (11%); and 6. others (10%). For patients screened by telephone, there were four main reasons: 1. not interested in the study (39%); 2. lives too far away (26%); 3. health problems (21%) and 4. too busy (7%).
Factors related to consent to the study
We compared patients who consented to participate in the study (N = 134) with those who refused to participate (N = 407) (Table 1). Patients who consented were younger (mean age of 70 vs. 73 years old) and were more likely to be non-white (mainly African American). The comparison by race was inconclusive however because of the high percentage of unknown race among patients who refused enrollment. The majority (99%) of both groups were male. Patients who consented and patients who refused had similar LVEF, indicating similar systolic function. Medication treatments for CHF were also comparable for the two groups of patients; a similar percentage (p value > .05) in each group received the two standard medications: β-blockers, and ACE inhibitors. A key factor in consenting to participate in the study was the distance between the patient's residence and the VA medical center where the study was conducted. Patients who consented lived an average of nine miles closer to the study site than patients who refused.
Table 1.
Characteristics of Patients Consented or Refused to Study Participation
| Consented Patients N = 134 | Refused Patients N = 407 | P-value* | |
| Patient Characteristics | |||
| Age (year) | |||
| Mean (SD) | 69.9 (9.6) | 73.0 (9.7) | 0.002 |
| Race | |||
| White | 83% | 84% | 0.001 |
| No-white (mainly African American) | 15% | 7% | |
| Unknown | 2% | 9% | |
| Cardiac Systolic Function | |||
| LVEF (%) | |||
| Mean (SD) | 31.3 (7.0) | 31.7 (7.9) | 0.56 |
| CHF Medication | |||
| ACE-Inhibitors | 82% | 75% | 0.08 |
| β-Blockers | 76% | 71% | 0.27 |
| Distance between Residence and Study Site (Mile) | |||
| Mean (SD) | 21.7 (21.4) | 31.3 (33.6) | 0.0002 |
*: P-value of statistical tests of t-test or chi-square test, comparing patients consented vs. refused to study participation.
Factors related to withdrawal after consenting to the study
Of the 134 patients who consented to the study either through the clinic or telephone recruitment, 95 finished the baseline assessments on the outcome measures. We compared these 95 patients with the 39 patients who withdrew from the study after signing the informed consent form. These two groups of patients were not statistically different in age, race, LVEF, or the distance from their residence to the VA hospital. Between the two groups of patients, similar (i.e., no statistical difference) percentages of patients received the β-blockers and ACE inhibitors.
Reasons for participating in the study – results from the qualitative study
Six general categories emerged in coding patients' responses to the question about the reasons for their study participation: 1. benefit to self; 2. benefit to others, including the VA; 3. gratitude to the VA; 4. positive comments by a trusted professional; 5. certain characteristics of the recruiter; and 6. monetary compensation.
Benefit to self
For the majority of patients (34 out of 57), the primary motivation for participation in the study appeared to be the desire to gain some benefit to themselves. These projected benefits ranged from learning more about the origin and manifestations of their condition, to learning additional ways to cope with their symptoms and limitations, to easing the boredom and inactivity brought about by their imposed lifestyles.
Many patients reported that it "couldn't hurt" or "might help" to gain more knowledge.
Well, I was looking for something.... I wanted to find out more about the heart, and I intended to learn more about it. Not only the heart, but every thing else, the dietician and so forth.
Some patients specifically joined to explore new ways, or learn new techniques to cope with their conditions.
Well, I felt as though when I said no about the whole thing, after I thought about it, I said, I might get some benefit out of it.... Because then I got to thinking, I said You know, to sit in on a meditating class is big bucks if I had to spin it out of my pocket. So I'm saying I'm getting this for nothing and getting a little incentive on top of that. So I says, Well, I have to go and see.
Some patients just thought that participation in the study would ease the burden of a restrictive and often inactive lifestyle imposed by their condition.
I guess just to get involved with something... just to have someplace to go and something to do.
Benefit to others
A large number of patients said that they participated in the study to help others, either other people with the same condition or health research in general.
If you can't do anything to help your fellow man, and you have the opportunity, and it's not painful, it's not costing you anything but a little time and you don't do that, I think there's something wrong with you.
Gratitude to the VA
Several patients emphasized that they agreed to participate because of their deep gratitude to the VA for the care given; they were happy to help the VA in its research and clinical efforts.
I figured anything that could help patients or the VA, I'm for it and I will do it again.
One man credited the VA with saving his life.
I am extremely grateful to the VA... for saving my life because a civilian hospital wouldn't do anything for me. And I feel that anything I can do to contribute to studies of this nature, I'm more than happy to do.
Another spoke of his positive relationship with the VA when asked why he joined the study.
And probably more my relationship with the VA. I get criticized at times, 'why are you a guinea pig for everything?' I said, I just feel that they've done so much good for me that if I can get involved in some program that maybe some new information will be developed or additional information that I'm more than willing and happy to do that.
Positive comments by trusted professional
Positive comments from their doctor or trusted clinician regarding the study appeared to be a very strong motivator in patient recruitment.
I thought it was just a good idea. I said, 'What the hell, they wouldn't have asked me to join the class if it wasn't going to help me... So I said, sure, why not? And uh, Dr. xxxx suggested it was a good idea and my lead nurse Mrs. XXXX said it's a good idea to follow these programs. So I said, what the hell, if they think it's good enough for them, why not?
Recruiter
The appearance, personality, manner, and gender of the recruiter emerged as an extremely important factor in the recruiting process. A number of patients in this study even stated that they joined specifically because they were impressed by the recruiter. A light-hearted flirtatious strain also appeared to enhance a positive response.
Because a young lady lassoed me down in the waiting room at West Roxbury and was very persuasive.
One man openly stated his attraction for the female recruiter.
The first interviewer that interviewed me was female... and very attractive, and I said, by golly, this can't hurt... I'd rather look at her or someone like her you know than a blank page, you know?... And then I wasn't disappointed because... I really had hopes that it might do something and it was pleasant.
Another expressed enjoyment at the meeting with the recruiter.
Well, I remember that day I talked to [the recruiter] in West Roxbury... Nice little girl, yes... It just was a pleasant meeting, and I enjoyed meeting her, and it seemed like a good sense thing to do.
One patient stressed that he was most impressed with the recruiter's competence and intelligence.
I think that when I was recruited, they talked about how it was good for the heart, and it relaxes. It just sounded like it would be good for me... It would help me; it relaxes me and could help my heart... I think the girl was a good recruiter. I was a field manager all my life. I owned my own company and trained my own sales people. And she was good.
One patient was so impressed by the recruiter and the belief that she would be a part of the study that even though he could not immediately participate, he agreed to join at a future date. When he began the program and realized that the recruiter was not part of it, he expressed disappointment, but enjoyed the study nevertheless.
I was over at West Roxbury, and [the recruiter] came up to me and... I said I really can't do it, I don't have the time.... So I said if you wait till November, I'll do it.... So she's the one that talked me into it.... And then I find out she's gone!.... She spent about a half hour with me in there.... She says I really would love to have you in the class.... She said we really would love to have you come. I said I can't go until November when I have a few less appointments.... I started last November.
Monetary compensation
While some patients said that the monetary compensation was a nice feature and they were happy to get it, they stressed that they would have joined the study even without the money. Only one patient said he joined the study just for the money.
Discussion
Although a number of barriers made recruitment a challenge, this behavioral intervention trial was successful in obtaining a recruitment number beyond its original goal of 120 consenting patients. We attribute this success to the following two factors: close monitoring of the recruitment and a flexible protocol. By closely monitoring recruitment, we recognized in the early stages that the recruitment rate was lower than expected. We were then able to act in a timely manner to change our recruitment strategies and study protocol. The changes in recruitment strategies included: 1) extending recruitment clinics to include cardiology and primary care clinics in addition to the originally designated heart failure clinic; 2) extending the recruitment period from the originally planned one year and two months to two years and three months; 3) adding telephone recruitment. Although the yield rate was low, the ten patients recruited and enrolled from the telephone recruitment were, nevertheless, a valuable addition to the study. The changes in the study protocol consisted of the following: 1) allowing patients who could not do the exercise test using a bicycle (one of the two study outcomes) to enroll in the study; and 2) allowing patients who were not on the two major medications for treating CHF to enroll in the study. Twenty-two percent of the enrolled patients could not do the bike test. This change, therefore, proved very valuable. For those patients who could not do the bike test, the other study outcome, quality of life measures, was available for analysis. Around 20% of consenting patients were not receiving each of the two medications. We will control for medication use in the analysis when we evaluate the intervention effect to account for the possible confounding effect of medication on the study outcome.
Although the target number of patients agreed to participate, only 71% (N = 95) of those patients actually completed the baseline outcome assessments and enrolled in the study. Since it was necessary to schedule the bicycle exercise test some time after the recruitment, patients had time to change their minds about participation. This factor needed to be taken into account when we estimated the enrollment rate in the study planning stage. We had a higher enrollment rate using face-to-face recruitment in the clinic than using telephone recruitment. However, we were able to enroll only one patient per 5–6 patients approached in the clinic. With telephone recruitment, we only enrolled 6 patients per 100 patients contacted. The flyer was totally unsuccessful for recruitment because all the patients who called as a result of seeing it were not eligible due to a high LVEF or a lack of the CHF diagnosis. Our experiences indicate that for a behavioral intervention trial that requires patients to travel frequently to the intervention site and also requires laboratory data, face-to-face recruitment is the best choice. Even using a face-to-face recruitment approach, however, one should expect to have an enrollment rate that is much lower than the rate for studies that only require patients to fill out questionnaires.
Our recruitment experience also provided information on why patients declined to participate in the study. The top reasons given by patients who declined to participate in the study included living too far away, travel difficulties, and time constraints. These reasons were justified given the elderly study population with multiple comorbidities and the study requirement of frequent travel to the intervention site. These findings are consistent with other studies that also found that transportation, travel difficulties, and time commitment, are among the most common barriers for study participation, particularly for the elderly [1,15]. Our analysis comparing the patient characteristics between those who consented and refused to participate in the study confirmed that the distance between a patient's residence and the study site was a strong determining factor for study participation.
One important protocol change in this study was the addition of a qualitative piece consisting of telephone interviews with patients about their experiences in the study. As indicated in the literature, qualitative studies can provide valuable information about how and why intervention works [16,17]. This type of information is especially important for an intervention such as the relaxation response. The benefits that patients could obtain from the intervention might not be captured by the standard quality of life measures.
During the qualitative interview, for the purpose of helping with recruitment, we also asked patients why they decided to enroll in the study. The reason given by most of the study participants was for some benefit to self. Although patients were informed that no beneficial effect was to be expected, their decisions to participate in the study carried the expectation that they would benefit from it in some way. Patients defined benefits differently, ranging from learning more about their medical condition to helping them cope with imposed lifestyle changes. Other reported reasons for study participation included helping others, money, gratitude to the VA, or because of positive comments from a doctor, nurse, or clinician. The latter two motivations suggest the value of conducting a study within the VA health care system and the importance of informing relevant healthcare providers about planned clinical studies. Another important factor contributing to successful recruitment is the recruiter. Our experience with this study indicates that the personality, gender, confidence, competence, and attractiveness of the recruiter are extremely important factors in successful recruitment.
In general, the most effective recruitment involved a direct, personal approach. Patients appeared to enjoy being noticed and singled out for something presented to them as important and special ("I was asked to do it."); they responded to the implication that their participation was needed and appreciated ("I really would love to have you in the class.... We really would love to have you come."). Only one patient specified that he responded to a written notice. Implicit in this phenomenon is the patient's positive response to feeling needed or cared about; he feels special because he is singled out for his potential to help, whether it's himself, others, the VA in particular or humanity in general. Only one patient reported that money was his only motivation.
Based on our experiences in this study, we have learned a number of valuable lessons for successful patient recruitment: 1) Close monitoring of recruitment statistics is important; 2) Flexibility in protocol change is essential; 3) A successful recruiter requires certain specific characteristics; 4) Patient recruitment can be very time consuming and costly; and 5) Sufficient budget for recruitment personnel is necessary. Some of these lessons have been highlighted in other studies. For example one trial was successful in increasing recruitment rate through adopting flexible recruitment strategies based on the finding from a qualitative study within the trial [18]. With the experience we gained from this study, we recommend the following considerations for studies with similar features to this one: 1) Carefully evaluate the available transportation options in study planning; 2) Consider a multiple-site study; and 3) Adopt alternative intervention methods that allow patients to have the intervention at home, such as home study video tapes or Internet-based two-way video conferencing.
Conclusions
Although patient recruitment for clinical trials is a challenge, our experiences from the relaxation response intervention for chronic heart failure trial revealed factors that can contribute to recruitment success. Close monitoring of recruitment and flexibility in protocol change are the two keys for successful recruitment. Personal characteristics of the recruiters is also an important factor. Finally, careful planning including allocating a sufficient budget for recruitment is essential for success.
Competing interests
None declared.
Authors' contribution
BHC conceived of the study, and participated in its design, management and data analysis. AH participated in the study design and interpretation of analysis results. MS participated in the study design and facilitated patient recruitment. JSL participated in the study design. All authors read and approved the final manuscript.
Table 2.
Characteristics of Patients Enrolled or Withdrawn after Consenting
| Enrolled Patients N = 95 | Withdrawn Patients N = 39 | P-value* | |
| Patient Characteristics | |||
| Age (year) | |||
| Mean (SD) | 70.0 (9.7) | 69.8 (9.4) | 0.89 |
| Race | |||
| White | 86% | 82% | 0.65 |
| No-white (mainly African American) | 14% | 18% | |
| Cardiac Systolic Function | |||
| LVEF (%) | |||
| Mean (SD) | 31.2 (7.1) | 31.5 (6.7) | 0.78 |
| CHF Medication | |||
| ACE-Inhibitors | 82% | 81% | 0.85 |
| β-Blockers | 78% | 70% | 0.33 |
| Distance between Residence and Study Site (Mile) | |||
| Mean (SD) | 23.3 (23.6) | 17.5 (13.7) | 0.09 |
*: P-value of statistical tests of t-test or chi-square test, comparing patients enrolled vs. withdrawn after consenting.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
This research was supported by the Department of Veterans Affairs, Health Services Research and Development Grant (IIR 99–241). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. We are indebted to the veterans who volunteered to participate in the study. We also thank all the personnel who contributed their time to this project in recruitment, qualitative interviews and analysis, data management, and statistical analysis.
Contributor Information
Bei-Hung Chang, Email: bhchang@bu.edu.
Ann M Hendricks, Email: Ann.Hendricks@med.va.gov.
Mara T Slawsky, Email: Mara.Slawsky@bhs.org.
Joseph S Locastro, Email: Joseph.Locastro@med.va.gov.
References
- Lovato LC, Hill K, Hertert S, Hunninghake DB, Probstfield JL. Recruitment for controlled clinical trials: literature summary and annotated bibliography. Controlled Clinical Trials. 1997;18:328–352. doi: 10.1016/S0197-2456(96)00236-X. [DOI] [PubMed] [Google Scholar]
- Ferland D, Fortin PR. Recruitment strategies in superiority trials in SLE: lessons from the study of methotrexate in lupus erythematosus (SMILE) Lupus. 1999;8:606–11. doi: 10.1191/096120399680411371. [DOI] [PubMed] [Google Scholar]
- McNeely EA, Clements SD. Recruitment and retention of the older adult into research studies. Journal of Neurosurgical Nursing. 1994;26:57–61. [PubMed] [Google Scholar]
- Ritchie CS, Dennis CS. Research challenges to recruitment and retention in a study of homebound older adults: lessons learned from the nutritional and dental screening program. Care Management Journals: Journal of Case Management; The Journal of Long Term Home Health Care. 1999;1:55–61. [PubMed] [Google Scholar]
- Porter EJ, Lanes TI. Targeting intermediaries to recruit older women for qualitative, longitudinal research. Journal of Women & Aging. 2000;12:63–75. doi: 10.1300/J074v12n01_05. [DOI] [PubMed] [Google Scholar]
- Harris R, Dyson E. Recruitment of frail older people to research: lessons learnt through experience. Journal of Advanced Nursing. 2001;36:643–51. doi: 10.1046/j.1365-2648.2001.02029.x. [DOI] [PubMed] [Google Scholar]
- Ory MG, Lipman PD, Karlen PL, Gerety MB, Stevens VJ, Singh MA, Buchner DM, Schechtman KB. Recruitment of older participants in frailty/injury prevention studies. Prevention Science. 2002;3:1–22. doi: 10.1023/A:1014610325059. [DOI] [PubMed] [Google Scholar]
- Petrovitch H, Byington R, Bailey G, Borhani P, Carmody S, Goodwin L, Harrington J, Johnson HA, Johnson P, Jones , et al. Systolic Hypertension in the Elderly Program (SHEP). Part 2: Screening and recruitment. Hypertension. 1991;17:II16–II23. doi: 10.1161/01.hyp.17.3_suppl.ii16. [DOI] [PubMed] [Google Scholar]
- Benson H, Caudill MA. Relaxation techniques for managing hypertension. Primary Cardiology. 1984;10:137–144. [Google Scholar]
- Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher KE, Pbert L, Lenderking WR, Santorelli SF. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry. 1992;149:936–43. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- Mason O, Hargreaves I. A qualitative study of mindfulness-based cognitive therapy for depression. British Journal of Medical Psychology. 2001;74:197–212. doi: 10.1348/000711201160911. [DOI] [PubMed] [Google Scholar]
- Jacobs GD. Clinical applications of the relaxation response and mind-body interventions. Journal of Alternative & Complementary Medicine. 2001;7:S93–101. doi: 10.1089/107555301753393850. [DOI] [PubMed] [Google Scholar]
- Mandle CL, Jacobs SC, Arcari PM, Domar AD. The efficacy of relaxation response interventions with adult patients: a review of the literature.[comment] Journal of Cardiovascular Nursing. 1996;10:4–26. doi: 10.1097/00005082-199604000-00003. [DOI] [PubMed] [Google Scholar]
- Fleischman J. Mind/Body Medicine: Using Your Mind for Better Health. Boston: Harvard Health Publications; 2001. [Google Scholar]
- Ross S, Grant A, Counsell C, Gillespie W, Russell I, Prescott R. Barriers to participation in randomised controlled trials: a systematic review.[see comment] Journal of Clinical Epidemiology. 1999;52:1143–56. doi: 10.1016/S0895-4356(99)00141-9. [DOI] [PubMed] [Google Scholar]
- Vuckovic N. Integrating qualitative methods in randomized controlled trials: the experience of the Oregon Center for Complementary and Alternative Medicine. Journal of Alternative & Complementary Medicine. 2002;8:225–7. doi: 10.1089/10755530260127916. [DOI] [PubMed] [Google Scholar]
- Verhoef MJ, Casebeer AL, Hilsden RJ. Assessing efficacy of complementary medicine: adding qualitative research methods to the "Gold Standard". Journal of Alternative & Complementary Medicine. 2002;8:275–81. doi: 10.1089/10755530260127961. [DOI] [PubMed] [Google Scholar]
- Donovan J, Mills N, Smith M, Brindle L, Jacoby A, Peters T, Frankel S, Neal D, Hamdy F. Quality improvement report: Improving design and conduct of randomised trials by embedding them in qualitative research: ProtecT (prostate testing for cancer and treatment) study. Commentary: presenting unbiased information to patients can be difficult [see comment] Bmj. 2002;325:766–70. doi: 10.1136/bmj.325.7367.766. [DOI] [PMC free article] [PubMed] [Google Scholar]