Abstract
Introduction
The purpose of this article is to present further longitudinal data for short-term and long-term stability, following up our previous article in the surgery literature with a larger sample and 2 years of stability data.
Methods
Data from 38 patients enrolled in this prospective study were collected before treatment, at maximum expansion, at removal of the expander 6 months later, before any second surgical phase, at the end of orthodontic treatment, and at the 2-year follow-up, by using posteroanterior cephalograms and dental casts.
Results
With surgically assisted rapid palatal expansion (SARPE), the mean maximum expansion at the first molar was 7.60 ± 1.57 mm, and the mean relapse was 1.83 ± 1.83 mm (24%). Modest relapse after completion of treatment was not statistically significant for all teeth except for the maxillary first molar (0.99 ± 1.1 mm). A significant relationship (P <0.0001) was observed between the amount of relapse after SARPE and the posttreatment observation. At maximum, a skeletal expansion of 3.58 ± 1.63 mm was obtained, and this was stable.
Conclusions
Skeletal changes with SARPE were modest but stable. Relapse in dental expansion was almost totally attributed to lingual movement of the posterior teeth; 64% of the patients had more than 2 mm of dental changes. Phase 2 surgery did not affect dental relapse.
Although a number of articles on the stability of surgically assisted rapid palatal expansion (SARPE) have been published, the reported stability varies considerably.1–8 It is apparent that most conclusions about the stability of SARPE depend on what was measured and when the measurements were made during the sequence of treatment. The goal of this article was to present further longitudinal data for short-term and long-term stability, following up our previous article in the surgery literature with a larger sample and 2 years of stability data.9
MATERIAL AND METHODS
Thirty-eight patients, 19 females and 19 males between 15 and 54 years of age, agreed to participate in a prospective, observational study of SARPE outcomes approved by the Ethics Committee of Laval University in Québec, Canada. All had dental casts and posteroanterior (PA) cephalograms immediately before SARPE (T1), at the completion of expansion (T2), and at the removal of the expander approximately 6 months later (T3). As of the end of January 2010, 32 had the same records before any second surgical phase (T4), 37 had records at the completion of orthodontic treatment (T5), and 23 had records 2 years after the end of orthodontic treatment (T6). Treatment characteristics are described in Table I.
Table I.
Treatment characteristics of the experimental sample
| Observation time point | n | Mean time (mo) | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| T1–T2 (distraction completed) | 38 | 0.68 | 0.23 | 0.46 | 1.81 |
| T2–T3 (expander retention) | 38 | 5.95 | 0.68 | 4.21 | 7.13 |
| T1–T4 (start to second surgery) | 32 | 15.27 | 3.99 | 9.40 | 24.28 |
| T2–T5 (end of expansion to deband) | 37 | 21.59 | 5.28 | 12.88 | 41.69 |
| T3–T5 (expander out to deband) | 37 | 15.64 | 5.09 | 7.79 | 35.19 |
| D1–T5 (total treatment time) | 37 | 23.57 | 5.27 | 15.41 | 43.07 |
| T5–T6 (postorthodontic treatment) | 23 | 25.35 | 4.49 | 20.96 | 39.49 |
D1, Treatment initiated in the mandibular arch; T(x)–T(y), observation between 2 time points.
A tooth-borne expansion device (Superscrew Super-spring, Highwood, 1ll), either banded (n = 21) or bonded with occlusal coverage (n = 17) was used (Fig 1).
Fig 1.
Superscrew for palatal expansion: A, with 2 molar bands and 2 bonded occlusal rests on the first premolars; B, with bonded occlusal coverage. The bonded version was used for patients with an open bite or a high mandibular plane angle to minimize downward-backward rotation of the mandible.
The surgical technique (described in detail previously) included separation of the pterygoid junction and the midpalatal suture between the incisors’ roots.9 All surgery was performed by the same surgeon.
After the surgery, a latency period of 7 days was observed, and then the patients were instructed to activate the screw by 0.25 mm twice a day. The patients were monitored twice a week until the planned expansion was achieved 14 to 21 days later. Active orthodontic treatment for the maxillary dentition began 2 months after expansion had stopped. The expansion device was kept in place for approximately 6 months. In the mandibular arch, orthodontic alignment of the teeth began 1 week to 2 months before SARPE.
After the removal of the expander, no other retention except the main archwire was used until the end of orthodontic treatment. When the braces were removed, a bonded lingual wire was placed from canine to canine in both arches. No removable retainers were used.
Of the 38 patients who completed the distraction phase, 32 had a second surgical phase planned (usually superior repositioning of the maxilla or mandibular advancement), but 4 of them did not need it after reassessment. One patient was overexpanded and needed constriction of the maxilla at the second surgical phase to achieve arch coordination. His data were removed at T5. Twenty-three patients so far have returned for records 2 years after the end of orthodontic treatment.
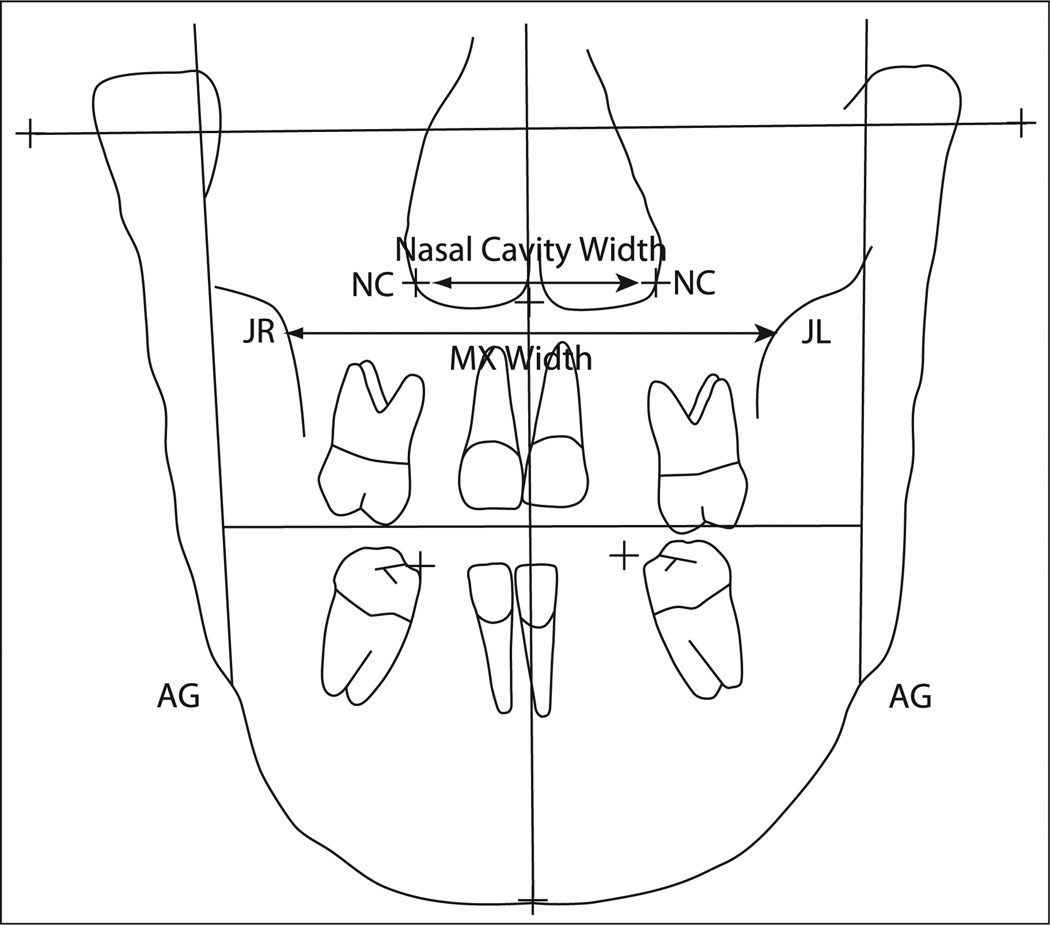
On the PA cephalograms, posterior maxillary width was measured as the distance between the bilateral jugula points, and nasal width was measured across the lowest wide part of the nasal cavity (Fig 2). The enlargement factor was assessed by using the width of the screw in situ and compared with the width of the screw on the PA cephalogram. On the dental casts, maxillary intercanine, interpremolar, and intermolar widths were measured as the distances between the cusp tips of the canines, mesial fossae of the premolars, and central fossae of the molars. Mandibular inter-first molar width was measured in the central fossae.
Fig 2.
Width measurements on PA cephalometric radiographs used in this study. Maxillary (MX) width was measured between jugula left (JL) and right (JR), with jugula defined as the point on the jugal process at the intersection of the outline of maxillary tuberosity and the zygomatic process. Nasal cavity (NC) width was measured between the left and right points at the lowest part of the maximum concavity of the piriform rim.
The statistical significance of changes between baseline and posttreatment data was assessed by using paired 2-sample t tests and repeated measures analysis of variance (ANOVA). The first test was used as a micro-investigation of any significant changes between 2 specific times, and the last test was used as a macroinvestigation of the global evolution of the measurements through more than 2 times. Since there were 6 t tests for dental changes, the level of significance was corrected by the Bonferroni adjustment (α = 0.05/6) to prevent type 1 error. Moreover, unpaired 2-sample t tests were used to compared the means of dental or skeletal changes between the 2 types of appliance (bonded, banded) or between the 2 subgroups for the mandibular arch (extraction, nonextraction). ANOVA models were also used to measure the effect of phase 2 surgery. After a significant effect, protected least significant difference multiple comparisons were used to test the differences between all pairs of surgery. Finally, the association between dental and skeletal changes was investigated by using Pearson correlation coefficients. The method error was also evaluated on dental changes at T6 for which the measurements were taken twice. To do so, the Shrout and Fleiss intra-class correlations were used as a coefficient of fidelity; these were all greater than 0.99, indicating a small method error.
RESULTS
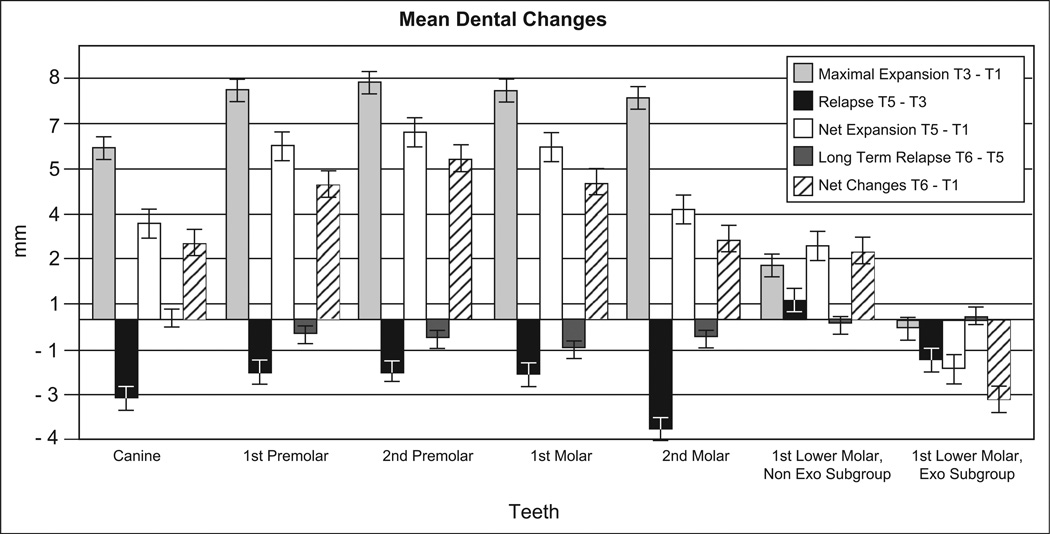
Dental changes, as measured on the dental casts obtained at each time point, are shown in Figure 3 and Appendix. The changes in the maxillary arch during expansion (T3-T1) and after expansion (T5-T3) were significantly different from zero (P <0.001), as were the net expansion amounts at debonding (T5-T1) and the 2-year recall (T6-T1). The amount of expansion at the second molars (7.36 mm) was similar to that at the first premolars (7.61 mm), showing the parallelism of maxillary expansion anteroposteriorly viewed from the occlusal aspect. Greater relapse was noted across the second molars; therefore, the net expansion at the second molar was significantly less than across the first premolars (P = 0.0013). This can be explained by arch-form coordination during treatment.
Fig 3.
Changes in arch width with SARPE. All maxillary changes were statistically significant from zero. Changes for the mandibular first molars of subjects who did not have first premolar extractions (Non Exo Subgroup) are significantly different from zero. Changes for the mandibular first molars in the subgroup that had first premolar extractions (Exo Subgroup) showed moderate constriction, although it was nonsignificant. The brackets on each bar show the standard error. See Appendix for completed detailed changes.
The mandibular arch changes should be interpreted cautiously. Eight patients had the first premolars extracted in the mandibular arch for second stage surgery preparation. Therefore, 2 subgroups were assessed according to this variable. The nonextraction subgroup with records at T5 (n = 28) showed significant expansion of mandibular intermolar width at debonding (2.45 ± 2.18 mm; P <0.0001), whereas the extraction subgroup (n = 8) showed variable responses with a tendency toward decreased intermolar width.
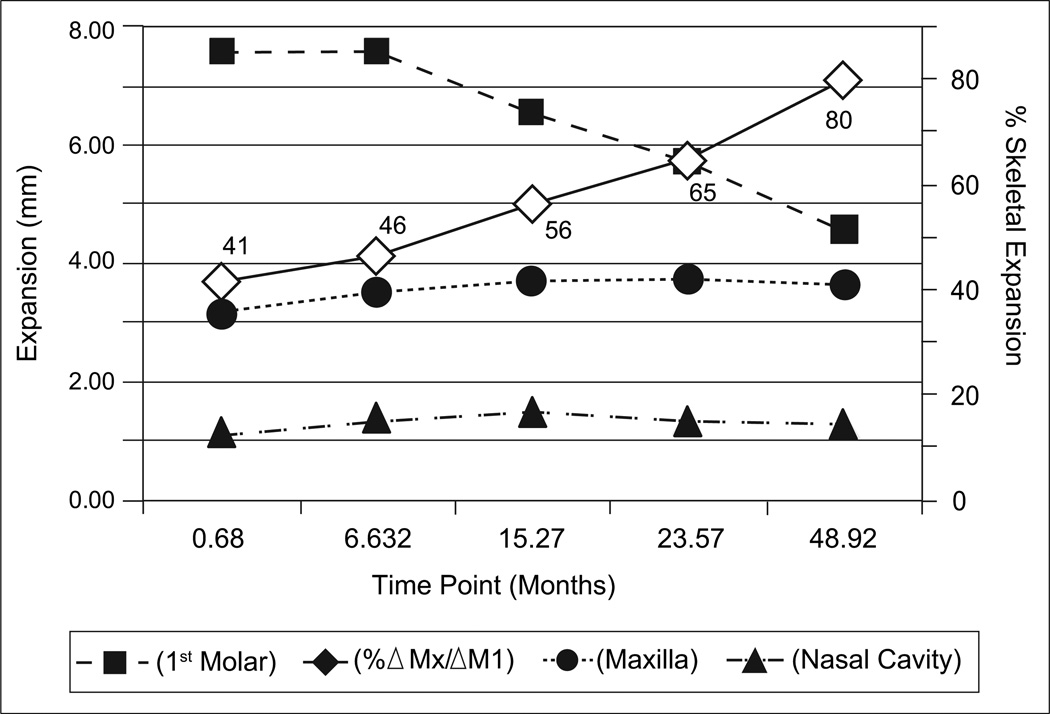
Figure 4 shows the changes over time in nasal cavity width and skeletal maxillary width (see Fig 2 for the points that were measured). In both locations, significant expansion was obtained (P <0.0001) and post-SARPE change was negligible (P = 0.1166). Therefore, the skeletal changes produced during SARPE can be considered to be quite stable.
Fig 4.
Changes over time after SARPE in the dental and skeletal dimensions, and in the percentages of skeletal expansion. Almost all relapse was dental rather than skeletal. Repeated-measures ANOVA confirmed a significant relationship between the amount of dental relapse and the time after surgery, when skeletal changes are stable and unaffected by time after surgery. Squares indicate expansion at the first molar. Diamonds indicate percentages of skeletal expansion at each time point. Circles indicate maxillary skeletal expansion. Triangles indicate expansion across the nasal cavity.
Table II shows that the 2 expansion devices had no significant difference in terms of expansion at the first molar (P = 0.2727), the skeletal level measured at jugula (P = 0.2735), or the nasal cavity (P = 0.3779).
Table II.
Effect of the type of appliance on expansion
| Variable | Type of appliance | n | Mean (mm) | SD | Minimum | Maximum | P value |
|---|---|---|---|---|---|---|---|
| First molar expansion | Bonded | 17 | 7.91 | 1.29 | 5.48 | 10.99 | 0.2727 |
| Banded | 21 | 7.34 | 1.75 | 4.95 | 10.98 | ||
| Jugula expansion | Bonded | 17 | 3.88 | 1.98 | 2.00 | 8.90 | 0.2735 |
| Banded | 21 | 3.21 | 1.93 | −1.40 | 6.40 | ||
| Nasal cavity expansion | Bonded | 17 | 1.20 | 1.13 | −1.10 | 3.60 | 0.3779 |
| Banded | 21 | 1.56 | 1.33 | −1.10 | 4.20 |
Of the 36 subjects whose treatments were completed by January 2010, 10 underwent a second-stage maxillomandibular surgery for AP or vertical repositioning, 12 had mandibular advancement only, 5 had maxillary surgery only, and 9 did not need a second surgical phase. There was no significant effect of any phase 2 surgery on dental relapse (P = 0.6637).
The data available at T3 to T4 and T5 (Table III) were used to analyze the timing of dental relapse changes at the first molar. About 57% of the total relapse occurred during the first 9 months after expander removal, and 43% occurred in the next 6 months. There was a significant relationship (P <0.0001) between the amount of relapse seen after SARPE and when the post-treatment observation was made. Long-term data show that some relapse, although nonsignificant, continues to occur after orthodontic treatment. The exception was the maxillary first molar, which reached the level of significance. Thirty-nine percent of the patients with 2 years of follow-up had more than 1 mm of relapse across the first molars during those 2 years. For those 9 patients, the mean relapse was 2.2 mm.
Table III.
Effect of the time on relapse after expander removal
| Time-point comparison | Relapse (mm) | Error | T or F value | df | P value |
|---|---|---|---|---|---|
| T3 vs T4 vs T5 vs T6 | 28.98 (F) | 3, 125 | <0.0001 | ||
| T3 vs T4 (9.5 ± 3.2 mo) | −1.05 | 0.30 | 3.53 (T) | 125 | 0.0006 |
| T4 vs T5 (5.7 ± 1.5 mo) | −0.79 | 0.30 | 2.62 (T) | 125 | 0.0098 |
| T3 vs T5 (15.2 ± 5.1 mo) | −1.85 | 0.29 | 6.43 (T) | 125 | <0.0001 |
| T5 vs T6 (24.7 ± 3.1 mo) | −1.09 | 0.34 | 3.23 (T) | 125 | 0.0016 |
T(x) vs T(y), Difference between time point (x) and (y).
Table IV shows that, of the different independent and dependent variables assessed in this study, only 2 variables, the diastema at T2 and the change in length of the screw during expansion, were significantly correlated with the amount of first molar expansion at T3. There was no significant association between diastema width and net expansion, skeletal and dental changes, skeletal and screw length changes, relapse and molar expansion, or relapse and skeletal expansion.
Table IV.
Coefficient of correlation and determination between variables
| Variable | n | r | P value |
|---|---|---|---|
| Diastema at T2 vs first molar expansion at T3 | 38 | 0.640 | <0.0001 |
| Diastema at T2 vs first molar expansion at T5 | 36 | 0.355 | 0.0334 |
| Diastema at T2 vs skeletal changes at T3 | 38 | 0.217 | 0.1902 |
| Screw changes vs first molar expansion at T3 | 38 | 0.936 | <0.0001 |
| Skeletal changes at T3 vs dental changes at T3 | 38 | 0.338 | 0.0381 |
| Skeletal changes at T3 vs screw changes at T3 | 38 | 0.295 | 0.0719 |
| Relapse T5-T3 vs first molar expansion at T3 | 36 | −0.265 | 0.1186 |
| Relapse T5-T3 vs skeletal expansion at T3 | 36 | −0.259 | 0.1271 |
DISCUSSION
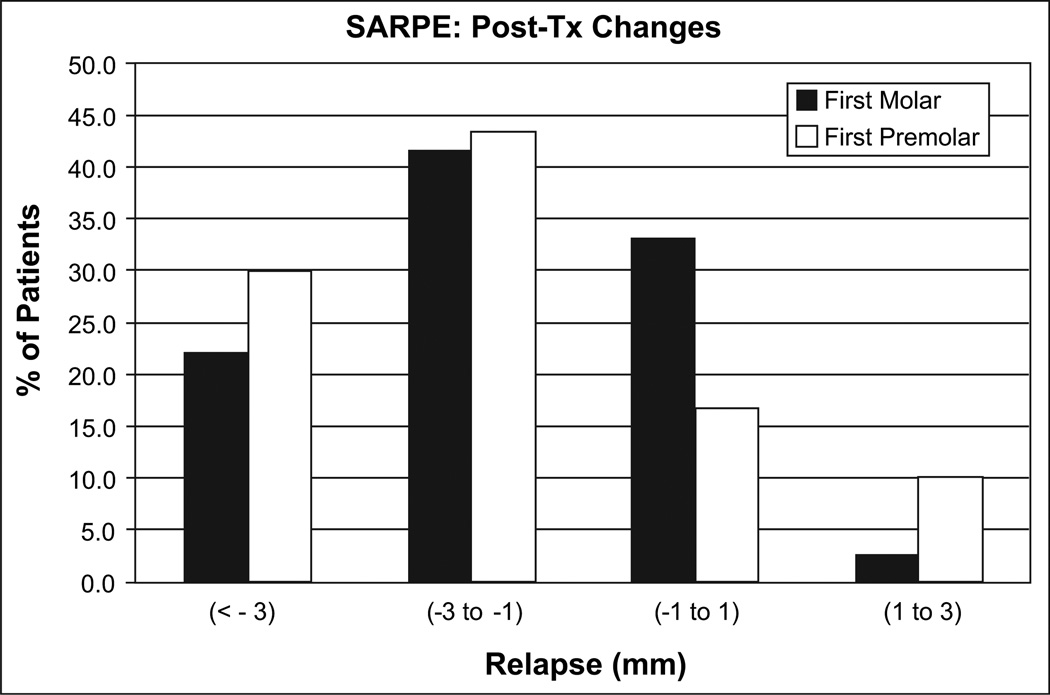
The amount of expansion across the first molars from the SARPE procedure was 7.60 ± 1.57 mm. This was similar to other reports with measurements to the maximum expansion point.5,6,8,10 We noted a mean relapse in width that was significant for all dental cast dimensions from the canine to the second molar, with a mean change of 1.83 ± 1.83 mm at the first molar. This is a loss of 24% of the maximum expansion. As the large standard deviation indicates, there was considerable variation in the amount of relapse, which is shown as the percentage of patients by amount of change in Figure 5.
Fig 5.
Percentages of patients with major relapse (>3 mm), moderate relapse (1–3 mm), minimal changes (−1-1 mm), and posttreatment expansion.
Posttreatment retention is likely to be an important factor in any study of stability.7,10,11 In this study, the expansion device was maintained for 6 months after the distraction had stopped. Byloff and Mossaz,6 who maintained the expander for 3 months and then replaced it with a conventional removable retainer for another 3 months, had 36% of relapse at the first molar at the end of orthodontic treatment. Progel et al,5 Berger et al,7 Koudstaal et al,8 and de Freitas et al10 reported 0.88 mm (12%), 1.01 mm (17.5%), 0.5 mm (55%), and 1.48 mm (18%) of relapse, respectively, in a 12-month study period. They concluded that expansion obtained with SARPE is stable, but all their patients were still in orthodontic treatment. In our study, data at T4 were collected 15 months after SARPE, before the second surgical phase for those who needed it. At that point, we found a mean of 1.04 mm of relapse at the first molar; this was comparable with the above-mentioned studies. This relapse at T4 was only 57% of the total relapse we found. Therefore, any inferences about the stability of SARPE are questionable if arch form coordination or final AP or vertical relationships have not been achieved at the time of measurement.
Our data showed that 42% of the patients had a relapse of 2 mm, and 22% had a relapse greater than 3 mm at the first molar (Fig 5). This was similar to the stability reported with multi-segmented LeFort 1 osteotomy.9,12
Data at T6 were obtained 24.7 ± 3.1 months after the orthodontic treatment. Modest relapse after treatment was observed. This was not statistically significant for all teeth, except for the maxillary first molar (0.99 ± 1.1 mm; P = 0.0003), where it represents 17% of the net expansion at T5 and adds to the relapse from T3 to T5. This long-term relapse that was significant at the first molar only cannot be explained by a type 1 error, since the level of significance was adjusted by the Bonferroni method (α = 0.05/6). It also cannot be explained by the effect of a bonded vs banded appliance, since our result shows that the type of appliance had no effect on relapse. Posttreatment arch form adjustment might be the explanation, since on the average the mandibular intermolar distance was expanded and constricted modestly, and a large standard deviation was noted (−0.18 ± 1.5 mm).
The amounts of dental expansion and the percentages of relapse in this study are in keeping with other long-term studies of SARPE.1–3,13,14 Bays and Greco2 reported 0.45 ± 0.69 mm of relapse of the net expansion at the first molar (7.7%) 2.4 ± 1.3 years after treatment. Northway and Meade1 found 0.1 mm of relapse of the net expansion (6%) 5 years after treatment. Stromberg and Holm3 reported 1.2 ± 1.3 mm of relapse of the net expansion (8.3%) in a 3.5-year follow-up of a “selected sample.” Anttila et al4 reported an average relapse of 1.3 mm of the net expansion (22%) after 6 years.
In this study, immediately after SARPE, about half of the expansion (46%) was skeletal, as shown by significant widening of the maxilla and the nasal cavity. This was greater skeletal change than Byloff and Mossaz6 and Berger et al7 reported, perhaps because they removed the expander after 3 months instead of our 6 months. Hino et al15 reported greater skeletal expansion but used a landmark closer to the teeth than we did. Recent computed tomography studies found skeletal expansion from 5 to 7 mm with a tooth-borne device.16–19 Koudstaal et al,8 in a prospective randomized patient trial comparing bone-borne and tooth-borne devices, obtained 3.1 ± 2.0 mm of expansion at the alveolar crest and 2.6 ± 1.8 mm at the nasal level, and found no difference in the efficacy of the 2 devices.
If one looks at the stability of the skeletal changes with SARPE, it should rank high in the hierarchy of stability of orthognathic surgery, but if one looks at the dental changes, 64% of the patients had more than 2 mm of change and 22% had more than 3 mm of change (Fig 5). This could be attributed to several factors, such as the device itself, the surgical technique, or the timing of the observations, but for all other surgeries, presurgical orthodontic preparation is done, and few if any dental movements are needed after surgery. This is not the case for SARPE. Many dental movements, including correction of overexpansion, are done after the expander is removed to achieve arch-form coordination. With SARPE, as with other orthognathic surgical procedures, it is appropriate to focus on skeletal, not dental, stability—which has not been clearly reported previously because the appropriate PA cephalograms were not available at several time points.
The significant correlation between the width of the diastema at T2 and the amount of first molar expansion at T3 indicates that the development of a diastema is a predictor that adequate molar expansion is occurring. If no diastema appears, one might suspect that there is no separation of the hemimaxillae, and that the buccal segments are tipping.
We found that dental changes are not correlated with skeletal changes (r2 = 0.06); this is supported by the study of Goldenberg et al.18 This confirms that, in the frontal view, rotation of the hemimaxillae occurs, with teeth expanding more than bone8,9,17,20 and palatal depth decreasing.1,8 This means that the alveolar edges below the buccal corticotomy move inward, and the palatal processes move downward as the dentoalveolar process is expanding (Fig 6). One might expect that greater expansion during SARPE would mean greater relapse after removal of the expansion device. Our data show that there is no relationship between the amount of expansion and the amount of dental relapse (r2 = 0.07, P = 0.1186).
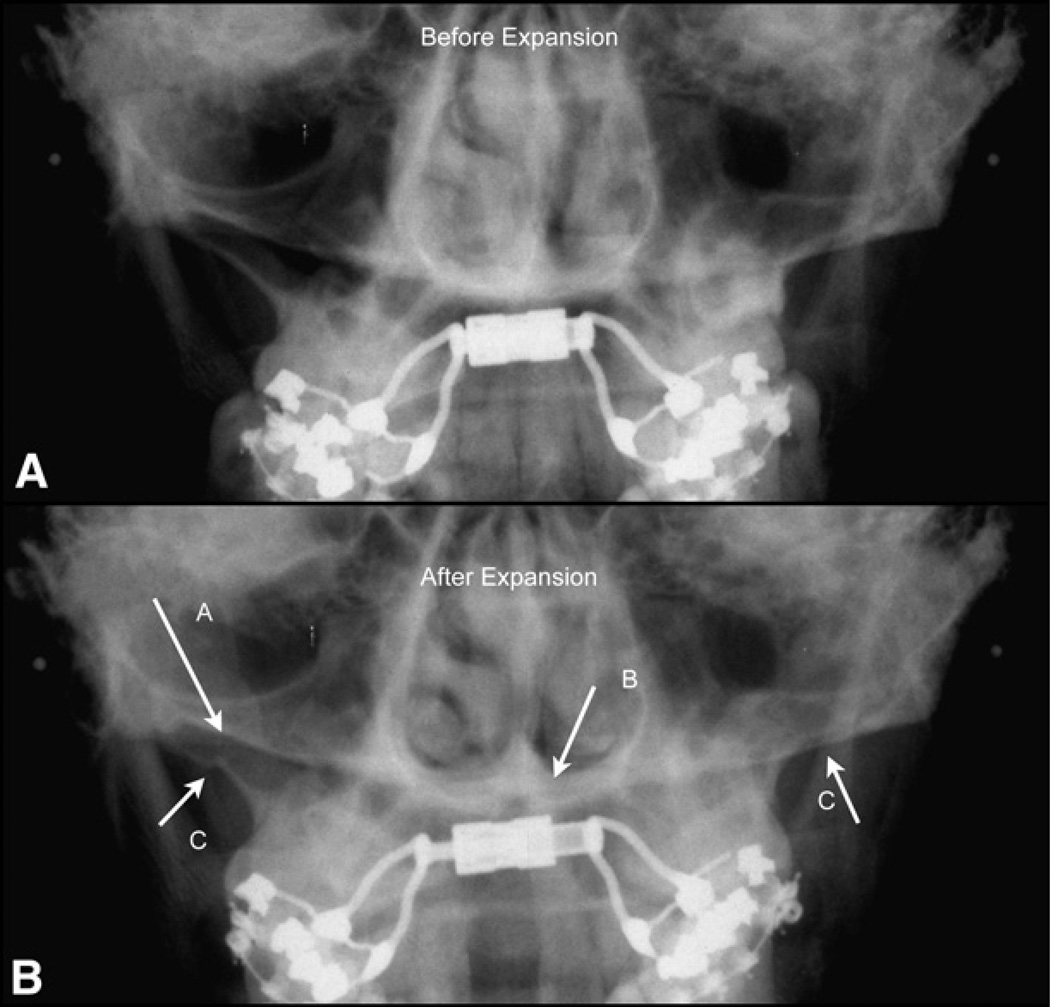
Fig 6.
PA cephalograms: A, before expansion; and B, after expansion. A, Inward movement of the alveolar edge below the buccal corticotomy (C); B, downward movement of the palatal process of the hemimaxillae.
The classic study of the stability of transverse expansion obtained with segmented LeFort 1 osteotomy reported that patients who had concurrent mandibular surgery had significantly greater relapse at the first and second molars.21 Our data showed no significant effect of any phase 2 surgery on dental relapse. This might be an important decision factor if large transverse changes are necessary along with vertical and AP changes.
CONCLUSIONS
In this study, transverse expansion of the maxilla was achieved through SARPE with pterygoid plate separation. Skeletal changes were modest (usually 3–4 mm) but stable. Relapse in dental expansion was almost totally attributed to lingual movement of the posterior teeth.
Phase 2 surgery did not affect dental relapse. The diastema at the end of distraction is a predictor that adequate molar expansion is occurring. Bonded expanders showed the same efficacy as banded expanders.
Acknowledgments
We thank Dany Morais for careful surgical treatment and Gaetan Daigle for statistical consultation and analysis.
Supported in part by NIH grant DE-05221 from the National Institute of Dental and Craniofacial Research.
APPENDIX
Dental changes after SARPE
| Variable | n | Mean (mm) | SD | SE | Minimum | Maximum | P value |
|---|---|---|---|---|---|---|---|
| Canine T3-T1 | 37 | 5.689 | 2.030 | 0.334 | 0.570 | 9.560 | <0.0001 |
| Canine T4-T1 | 31 | 3.287 | 2.205 | 0.396 | −0.120 | 7.610 | <0.0001 |
| Canine T5-T1 | 35 | 3.179 | 2.275 | 0.385 | −1.140 | 8.240 | <0.0001 |
| Canine T5-T3 | 35 | −2.601 | 1.937 | 0.327 | −6.420 | 3.180 | <0.0001 |
| Canine T6-T5 | 22 | 0.060 | 0.683 | 0.146 | −1.470 | 1.390 | 0.6824 |
| Canine T6-T1 | 22 | 2.547 | 1.904 | 0.406 | −1.100 | 5.700 | <0.0001 |
| First premolar T3-T1 | 32 | 7.613 | 1.867 | 0.330 | 2.930 | 12.320 | <0.0001 |
| First premolar T4-T1 | 27 | 5.830 | 2.435 | 0.469 | 1.630 | 10.520 | <0.0001 |
| First premolar T5-T1 | 30 | 5.755 | 2.739 | 0.500 | 0.900 | 11.350 | <0.0001 |
| First premolar T5-T3 | 30 | −1.787 | 2.239 | 0.409 | −6.290 | 3.270 | 0.0001 |
| First premolar T6-T5 | 19 | −0.493 | 1.412 | 0.324 | −3.040 | 1.720 | 0.1456 |
| First premolar T6-T1 | 19 | 4.894 | 2.052 | 0.471 | 1.460 | 9.050 | <0.0001 |
| Second premolar T3-T1 | 38 | 7.865 | 1.865 | 0.302 | 3.830 | 12.290 | <0.0001 |
| Second premolar T4-T1 | 32 | 6.378 | 2.856 | 0.505 | 1.900 | 12.350 | <0.0001 |
| Second premolar T5-T1 | 36 | 6.214 | 2.747 | 0.458 | 1.020 | 13.170 | <0.0001 |
| Second premolar T5-T3 | 36 | −1.655 | 2.457 | 0.409 | −7.130 | 3.220 | 0.0003 |
| Second premolar T6-T5 | 23 | −0.642 | 1.351 | 0.282 | −2.850 | 1.980 | 0.0328 |
| Second premolar T6-T1 | 23 | 5.344 | 2.349 | 0.490 | 2.400 | 11.470 | <0.0001 |
| First molar T3-T1 | 38 | 7.598 | 1.566 | 0.254 | 4.950 | 10.990 | <0.0001 |
| First molar T4-T1 | 32 | 6.561 | 2.207 | 0.390 | 3.180 | 11.650 | <0.0001 |
| First molar T5-T1 | 36 | 5.732 | 2.088 | 0.348 | 1.780 | 12.400 | <0.0001 |
| First molar T5-T3 | 36 | −1.832 | 1.834 | 0.306 | −6.920 | 1.410 | <0.0001 |
| First molar T6-T5 | 23 | −0.987 | 1.110 | 0.231 | −3.570 | 0.590 | 0.0003 |
| First molar T6-T1 | 23 | 4.569 | 1.939 | 0.404 | 1.020 | 8.830 | <.0001 |
| Second molar T3-T1 | 34 | 7.360 | 1.850 | 0.317 | 3.440 | 11.120 | <0.0001 |
| Second molar T4-T1 | 29 | 5.359 | 2.268 | 0.421 | 1.660 | 10.030 | <0.0001 |
| Second molar T5-T1 | 32 | 3.659 | 1.891 | 0.334 | 1.030 | 7.930 | <0.0001 |
| Second molar T5-T3 | 32 | −3.640 | 1.986 | 0.351 | −7.710 | 0.540 | <0.0001 |
| Second molar T6-T5 | 21 | −0.636 | 1.238 | 0.270 | −3.250 | 2.820 | 0.0289 |
| Second molar T6-T1 | 20 | 2.684 | 1.494 | 0.334 | 0.290 | 6.130 | <0.0001 |
| Subgroup with mandibular premolar extractions | |||||||
| Mandibular first molar molar T3-T1 | 8 | −0.294 | 2.725 | 0.964 | −5.080 | 3.080 | 0.769 |
| Mandibular first molar molar T4-T1 | 7 | −1.766 | 3.218 | 1.216 | −5.800 | 3.120 | 0.197 |
| Mandibular first molar molar T5-T1 | 8 | −1.646 | 3.191 | 1.128 | −6.270 | 2.720 | 0.188 |
| Mandibular first molar T5-T3 | 8 | −1.352 | 2.260 | 0.799 | −4.480 | 1.100 | 0.134 |
| Mandibular first molar T6-T5 | 5 | 0.138 | 1.555 | 0.695 | −2.220 | 1.670 | 0.852 |
| Mandibular first molar T6-T1 | 5 | −2.648 | 1.385 | 0.619 | −4.600 | −1.550 | 0.013 |
| Subgroup without extractions | |||||||
| Mandibular first molar T3-T1 | 29 | 1.807 | 1.956 | 0.363 | −0.980 | 7.570 | <0.0001 |
| Mandibular first molar T4-T1 | 24 | 2.344 | 2.297 | 0.469 | −1.090 | 7.890 | <0.0001 |
| Mandibular first molar T5-T1 | 27 | 2.446 | 2.181 | 0.420 | −1.580 | 6.870 | <0.0001 |
| Mandibular first molar T5-T3 | 27 | 0.639 | 1.850 | 0.356 | −1.970 | 6.000 | 0.0843 |
| Mandibular first molar T6-T5 | 17 | −0.176 | 1.490 | 0.361 | −3.330 | 2.900 | 0.633 |
| Mandibular first molar T6-T1 | 17 | 2.283 | 1.955 | 0.474 | −0.380 | 8.090 | 0.0002 |
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
REFERENCES
- 1.Northway WM, Meade JB., Jr Surgically assisted rapid maxillary expansion: a comparison of technique, response, and stability. Angle Orthod. 1997;67:309–320. doi: 10.1043/0003-3219(1997)067<0309:SARMEA>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Bays RA, Greco JM. Surgically assisted rapid palatal expansion: an outpatient technique with long-term stability. J Oral Maxillofac Surg. 1992;50:110–115. doi: 10.1016/0278-2391(92)90352-z. [DOI] [PubMed] [Google Scholar]
- 3.Stromberg C, Holm J. Surgically assisted, rapid maxillary expansion in adults. A retrospective long-term follow-up study. J Craniomaxillofac Surg. 1995;23:222–227. doi: 10.1016/s1010-5182(05)80211-2. [DOI] [PubMed] [Google Scholar]
- 4.Anttila A, Finne K, Keski-Nisula K, Somppi M, Panula K, Peltomaki T. Feasibility and long-term stability of surgically assisted rapid maxillary expansion with lateral osteotomy. Eur J Orthod. 2004;26:391–395. doi: 10.1093/ejo/26.4.391. [DOI] [PubMed] [Google Scholar]
- 5.Pogrel MA, Kaban LB, Vargervik K, Baumrind S. Surgically assisted rapid maxillary expansion in adults. Int J Adult Orthod Orthognath Surg. 1992;7:37–41. [PubMed] [Google Scholar]
- 6.Byloff FK, Mossaz CF. Skeletal and dental changes following surgically assisted rapid palatal expansion. Eur J Orthod. 2004;26:403–409. doi: 10.1093/ejo/26.4.403. [DOI] [PubMed] [Google Scholar]
- 7.Berger JL, Pangrazio-Kulbersh V, Borgula T, Kaczynski R. Stability of orthopedic and surgically assisted rapid palatal expansion over time. Am J Orthod Dentofacial Orthop. 1998;114:638–645. doi: 10.1016/s0889-5406(98)70195-7. [DOI] [PubMed] [Google Scholar]
- 8.Koudstaal MJ, Smeets JB, Kleinrensink GJ, Schulten AJ, van der Wal KG. Relapse and stability of surgically assisted rapid maxillary expansion: an anatomic biomechanical study. J Oral Maxillofac Surg. 2009;67:10–14. doi: 10.1016/j.joms.2007.11.026. [DOI] [PubMed] [Google Scholar]
- 9.Chamberland S, Proffit WR. Closer look at the stability of surgically assisted rapid palatal expansion. J Oral Maxillofac Surg. 2008;66:1895–1900. doi: 10.1016/j.joms.2008.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Freitas RR, Goncalves AJ, Moniz NJ, Maciel FA. Surgically assisted maxillary expansion in adults: prospective study. Int J Oral Maxillofac Surg. 2008;37:797–804. doi: 10.1016/j.ijom.2008.04.019. [DOI] [PubMed] [Google Scholar]
- 11.Zimring JF, Isaacson RJ. Forces produced by rapid maxillary expansion. 3. Forces present during retention. Angle Orthod. 1965;35:178–186. doi: 10.1043/0003-3219(1965)035<0178:FPBRME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Proffit WR, Turvey TA, Phillips C. The hierarchy of stability and predictability in orthognathic surgery with rigid fixation: an update and extension. Head Face Med. 2007;3:21. doi: 10.1186/1746-160X-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marchetti C, Pironi M, Bianchi A, Musci A. Surgically assisted rapid palatal expansion vs. segmental Le Fort I osteotomy: transverse stability over a 2-year period. J Craniomaxillofac Surg. 2009;37:74–78. doi: 10.1016/j.jcms.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 14.Sokucu O, Kosger HH, Bicakci AA, Babacan H. Stability in dental changes in RME and SARME: a 2-year follow-up. Angle Orthod. 2009;79:207–213. doi: 10.2319/031808-155.1. [DOI] [PubMed] [Google Scholar]
- 15.Hino CT, Pereira MD, Sobral CS, Kreniski TM, Ferreira LM. Transverse effects of surgically assisted rapid maxillary expansion: a comparative study using Haas and Hyrax. J Craniofac Surg. 2008;19:718–725. doi: 10.1097/SCS.0b013e31816aaa91. [DOI] [PubMed] [Google Scholar]
- 16.Loddi PP, Pereira MD, Wolosker AB, Hino CT, Kreniski TM, Ferreira LM. Transverse effects after surgically assisted rapid maxillary expansion in the midpalatal suture using computed tomography. J Craniofac Surg. 2008;19:433–438. doi: 10.1097/SCS.0b013e318163e2f5. [DOI] [PubMed] [Google Scholar]
- 17.Landes CA, Laudemann K, Schubel F, Petruchin O, Mack M, Kopp S, et al. Comparison of tooth- and bone-borne devices in surgically assisted rapid maxillary expansion by three-dimensional computed tomography monitoring: transverse dental and skeletal maxillary expansion, segmental inclination, dental tipping, and vestibular bone resorption. J Craniofac Surg. 2009;20:1132–1141. doi: 10.1097/scs.0b013e3181abb430. [DOI] [PubMed] [Google Scholar]
- 18.Goldenberg DC, Goldenberg FC, Alonso N, Gebrin ES, Amaral TS, Scanavini MA, et al. Hyrax appliance opening and pattern of skeletal maxillary expansion after surgically assisted rapid palatal expansion: a computed tomography evaluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:812–819. doi: 10.1016/j.tripleo.2008.02.034. [DOI] [PubMed] [Google Scholar]
- 19.Tausche E, Deeb W, Hansen L, Hietschold V, Harzer W, Schneider M. CT analysis of nasal volume changes after surgically-assisted rapid maxillary expansion. J Orofac Orthop. 2009;70:306–317. doi: 10.1007/s00056-009-9910-5. [DOI] [PubMed] [Google Scholar]
- 20.Zemann W, Schanbacher M, Feichtinger M, Linecker A, Karcher H. Dentoalveolar changes after surgically assisted maxillary expansion: a three-dimensional evaluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:36–42. doi: 10.1016/j.tripleo.2008.05.044. [DOI] [PubMed] [Google Scholar]
- 21.Phillips C, Medland WH, Fields HW, Jr, Proffit WR, White RP., Jr Stability of surgical maxillary expansion. Int J Adult Orthod Orthognath Surg. 1992;7:139–146. [PubMed] [Google Scholar]