Abstract
Study Objectives:
To examine associations of objectively and subjectively measured sleep with subsequent cognitive decline.
Design:
A population-based longitudinal study.
Setting:
Six centers in the United States.
Participants:
Participants were 2,822 cognitively intact community-dwelling older men (mean age 76.0 ± 5.3 y) followed over 3.4 ± 0.5 y.
Interventions:
None.
Measurements and Results:
Objectively measured sleep predictors from wrist actigraphy: total sleep time (TST), sleep efficiency (SE), wake after sleep onset (WASO), number of long wake episodes (LWEP). Self-reported sleep predictors: sleep quality (Pittsburgh Sleep Quality Index [PSQI]), daytime sleepiness (Epworth Sleepiness Scale [ESS]), TST. Clinically significant cognitive decline: five-point decline on the Modified Mini-Mental State examination (3MS), change score for the Trails B test time in the worse decile. Associations of sleep predictors and cognitive decline were examined with logistic regression and linear mixed models. After multivariable adjustment, higher levels of WASO and LWEP and lower SE were associated with an 1.4 to 1.5-fold increase in odds of clinically significant decline (odds ratio 95% confidence interval) Trails B test: SE < 70% versus SE ≥ 70%: 1.53 (1.07, 2.18); WASO ≥ 90 min versus WASO < 90 min: 1.47 (1.09, 1.98); eight or more LWEP versus fewer than eight: 1.38 (1.02, 1.86). 3MS: eight or more LWEP versus fewer than eight: 1.36 (1.09, 1.71), with modest relationships to linear change in cognition over time. PSQI was related to decline in Trails B performance (3 sec/y per standard deviation increase).
Conclusions:
Among older community-dwelling men, reduced sleep efficiency, greater nighttime wakefulness, greater number of long wake episodes, and poor self-reported sleep quality were associated with subsequent cognitive decline.
Citation:
Blackwell T; Yaffe K; Laffan A; Ancoli-Israel S; Redline S; Ensrud KE; Song Y; Stone KL. Associations of objectively and subjectively measured sleep quality with subsequent cognitive decline in older community-dwelling men: the MrOS sleep study. SLEEP 2014;37(4):655-663.
Keywords: Aging, cognitive function, disturbed sleep, total sleep time
INTRODUCTION
As many as 50% of older adults report habitual sleep problems, including chronic insomnia.1 At least 10% of people 65 y old or older will develop cognitive impairment, with the rate rising exponentially with advancing age.2,3 With the rate of cognitive impairment increasing and the high prevalence of sleep problems in the elderly, it is important to determine prospective associations with sleep and cognitive decline.
Cognitive impairment has been shown to be associated with sleep quality, but most studies have been cross-sectional in nature, preventing conclusions on the direction of associations.4–8 Of the few studies examining the longitudinal association of sleep quality and cognitive decline, most have been based on self-reported9–15 rather than objectively measured16–18 sleep parameters.
To test the hypothesis that subjectively and objectively measured sleep disturbances are associated with an increased risk of cognitive decline in older men, we measured sleep parameters in a cohort of 2,822 cognitively intact men aged 67 y and older enrolled in the multicenter Outcomes of Sleep Disorders in Men (MrOS Sleep) Study. Data were gathered for two measures of cognition at the start of follow-up and at two subsequent time points an average of 1.4 and 3.4 y after assessment of sleep parameters. The MrOS Sleep Study provides a unique opportunity to study this question in a large cohort of community-dwelling older men who are well characterized for sleep parameters as well as for potentially important confounding factors such as medication use, depression, education level, physical function, and comorbidities. Comprehensive sleep measurements allow for assessment of the independent relative contribution of objectively measured sleep parameters and self-reported sleep quality to risk of cognitive decline.
METHODS
Participants
During the Osteoporotic Fractures in Men Study (MrOS) baseline examination from the years 2000 to 2002, 5,994 community-dwelling men 65 y or older were enrolled at six clinical centers in the United States: Birmingham, Alabama; Minneapolis, Minnesota; Palo Alto, California; the Monongahela Valley near Pittsburgh, Pennsylvania; Portland, Oregon; and San Diego, California.19,20 In order to participate, men needed to be able to walk without assistance and must not have had a bilateral hip replacement.
The MrOS Sleep Study, an ancillary study of the parent MrOS cohort, recruited 3,135 participants for a comprehensive sleep assessment. Men were screened for nightly use of mechanical devices during sleep, including pressure mask for sleep apnea (continuous positive airway pressure or bilevel positive airway pressure), oral appliances, or nocturnal oxygen therapy and were excluded if they could not forgo use of these devices during a polysomnography (PSG) recording. Of the 2,859 men who did not participate in this ancillary study, 349 died before the sleep visit, 39 had already left the study, 324 were not asked because recruitment goals had already been met, 150 were ineligible, and 1,997 refused participation.
This analysis used data collected at the Sleep Visit (2003-2005), MrOS Visit 2 (2005-2006), and MrOS Visit 3 (2007-2009) (Figure 1). To be included in this analysis, men had to have data on cognitive change from the Sleep Visit to one or both of the follow-up time points, and had not been classified as having “probable dementia” at the Sleep Visit (Modified Mini-Mental State examination [3MS] score < 80 or on a medication for dementia).
Figure 1.
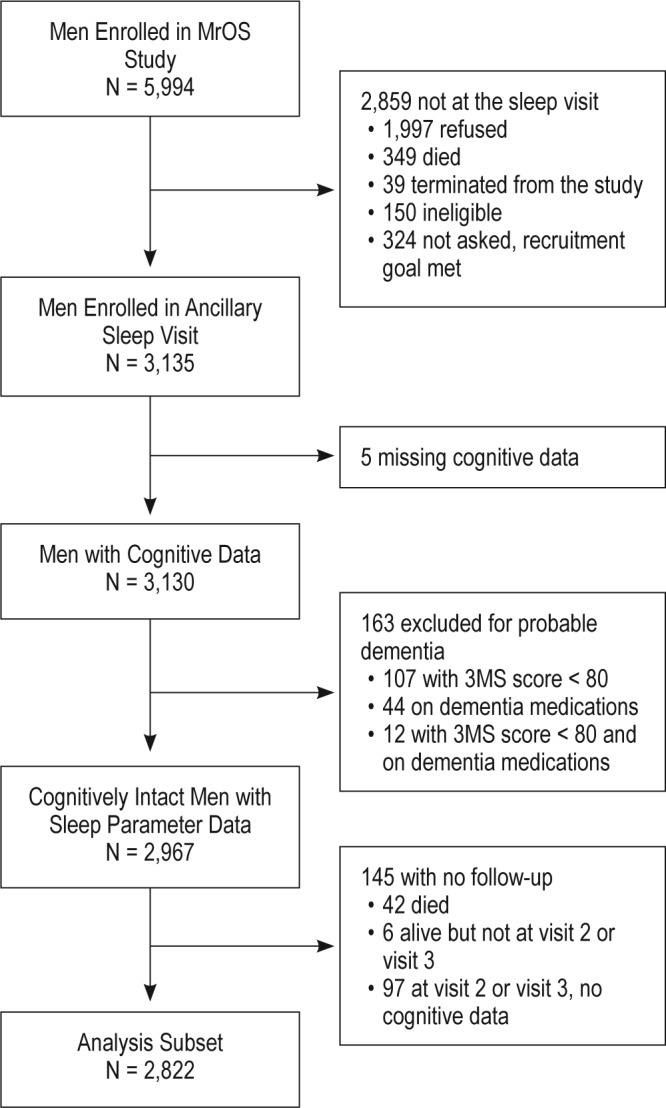
Progression of participants through the MrOS Study and the MrOS Sleep Study. 3MS, Modified Mini-Mental State examination.
Among these 3,135 participants of the MrOS Sleep Study, cognitive function data for either the Trail Making Test– Part B (Trails B) or the 3MS were available for 3,130 men. One hundred sixty-three men were not included because they had probable dementia. Of the remaining 2,967 men, all had Sleep Visit data on self-reported sleep (total sleep time [TST], Pittsburgh Sleep Quality Index [PSQI], Epworth Sleepiness Scale [ESS]) and 2,899 had actigraphy data.
No exclusion criteria were used for participation in Visit 2 or Visit 3. At both visits, most men completed the clinic visit and had cognitive function measured. Of the 2,967 cognitively intact men with Sleep Visit data, 2,822 provided data on cognition at either Visit 2 or Visit 3 (Visit 2: 2,757, 98% of survivors; Visit 3: 2,505, 94% of survivors) and comprise our analytic cohort.
All men provided written informed consent, and the study was approved by the Institutional Review Board at each clinic site.
Objective Actigraphic Parameters of Sleep-Wake Patterns
Objective characteristics of sleep-wake patterns were estimated using an actigraph (SleepWatch-O, Ambulatory Monitoring, Inc., Ardsley, NY). Our goal was to collect at least 5 nights of actigraphy data for each participant. The average number of nights was 5.2 ± 0.9 (range, 1 to 11), with 215 (7.8%) having less than 5 nights of data (eight with 1 night, six with 2 nights, 41 with 3 nights, 160 with 4 nights). Participants were instructed to wear the actigraph securely fastened around their nondominant wrist, and it was to be removed only when bathing or during water sports. The actigraph is similar in size and weight to a wristwatch, and movement is detected via a piezoelectric bimorph-ceramic cantilever beam that generates a voltage each time the actigraph is moved. These voltages are gathered continuously and summarized over 1-min intervals. Actigraphy has been shown to provide a reliable estimate of sleep-wake patterns.21 Data were collected in three modes but are reported here based on digital integration mode (also known as proportional integration mode).22 ActionW-2 software (Ambulatory Monitoring, Inc., Ardsley, NY) was used to analyze the actigraphy data.23 Details of the actigraphy scoring algorithms used in the study have been published elsewhere.24,25
Participants completed sleep diaries for the time period they wore the actigraph. The diaries included time into and time out of bed and times the actigraph was removed. This information was used in editing the actigraphy data files to set intervals when the participant was in bed trying to sleep (after “lights off”), and to delete time when the actigraph was removed. Interscorer reliability for editing the actigraphy data files has been previously found to be high in our group (intraclass coefficient = 0.95), and actigraphy has been shown to have good concordance with TST from PSG (intraclass coefficient = 0.57).24,26
Parameters estimated from actigraphy used in this analysis included TST: the hours per night spent sleeping while in bed after “lights off”; sleep efficiency (SE): the percentage of time in bed after “lights off” spent sleeping; wake after sleep onset (WASO): min of wake after sleep onset during the in-bed interval, with sleep onset defined as the point when the participant achieved a 20-min continuous block of sleep after “lights off”; and number of long wake episodes (LWEP): number of awakenings 5 min or longer in duration while in bed. All parameters from actigraphy reflect data averaged over all nights the device was worn in order to obtain a more representative characterization of usual sleep patterns.
Subjective Self-Reported Sleep Parameters
Participants completed the PSQI, a validated measure of subjective sleep quality and sleep disturbances over a 1-mo time period. Global PSQI scores range from 0 to 21 and a score of > 5 is indicative of poor sleep.27 The ESS, a self-administered questionnaire, was used to classify subjective daytime sleepiness. Scores on the ESS range from 0 to 24, with a score of > 10 indicating excessive daytime sleepiness.28,29 In addition, participants were asked about TST with the question “On most nights, how many hours do you sleep each night?”, with data collected rounded to the nearest hour.
Ascertainment of Cognitive Function
Two tests of cognitive function were administered at the clinic visits by trained staff: the Trails B and the 3MS.
The Trails B is a timed test that measures attention, sequencing, visual scanning, and executive function. Executive function is a measure of the ability for planning or decision making, error correction or trouble shooting, and abstract thinking. The Trails B test requires the participant to continuously scan a page to identify numbers and letters in a specified sequence while shifting from number to letter sets.30 The participant is given 300 sec to complete the test. A lower time for completion (in sec) represents better cognitive functioning. A positive change in completion time represents cognitive decline (took longer to complete the test at the follow-up time point).
The 3MS is a global measurement of cognitive function, with components for orientation, concentration, language, praxis, and immediate and delayed memory. The 3MS test is a broad sampling of cognitive domains. Scores range from 0 to 100, with higher scores representing better cognitive functioning.31 A negative change in 3MS score represents cognitive decline (score was lower at the follow-up time point).
Development of clinically significant cognitive decline from the Sleep Visit to Visit 3 (a mean of 3.4 ± 0.5 y later) was defined separately for each test as follows: having a decline in five points on the 3MS,32 or being in the worst decile of change scores for Trails B (Visit 3-Sleep Visit change score ≥ 65 sec).33
Other Measurements
All participants completed questionnaires at the time of the Sleep Visit, which included items about demographics, medical history, self-reported health status, physical activity, smoking, caffeine intake, and alcohol use. The number of prior medical conditions was calculated as the summed total of self-reported prior diagnoses of common chronic illnesses (hypertension, stroke or transient ischemic attack, diabetes mellitus, Parkinson disease, chronic obstructive pulmonary disease, coronary heart disease). The chronic illness of depression was assessed using the number of depressive symptoms from the Geriatric Depression Scale,with higher scores corresponding to higher levels of depression.34 Participants were asked to bring in all medications used within the preceding 30 days. All prescription and nonprescription medications were entered into an electronic database and each medication was matched to its ingredient(s) based on the Iowa Drug Information Service Drug Vocabulary (College of Pharmacy, University of Iowa, Iowa City, IA).35 The use of antidepressants, benzodiazepines, and prescription sleep medications (nonbenzodiazepine, nonbarbiturate sedative hypnotics) were categorized. The level of physical activity was assessed using the Physical Activity Scale for the Elderly.36 Functional status was assessed by collecting information on five instrumental activities of daily living (IADL), which included walking two to three blocks on level ground, climbing up to 10 steps, preparing meals, doing heavy housework, and shopping for groceries or clothing.37,38 Self-reported caffeine intake was calculated based on answers to questions regarding intake of caffeinated coffee, tea, and soda.39
A comprehensive examination included measurements of body weight and height. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters.
Statistical Analysis
For the primary analyses, the sleep parameters were expressed as categorical variables that were defined similarly to previous publications for comparability (TST: ≤ 5 h, > 5 to 7 h, > 7 to 8 h, > 8 h; SE: < 70% versus ≥ 70%; WASO: ≥ 90 min versus < 90 min; number of LWEP: eight or more versus fewer than eight)4,5,14,15 or used standard cutpoints (PSQI five or greater versus five or less; ESS < 10 versus ≥ 10).27–29 Analyses were also performed to evaluate the linear relationship of the sleep parameters and cognition, with the sleep parameters expressed as continuous variables.
Characteristics of participants were compared by categories of SE using chi-square tests for categorical variables, t-tests for normally distributed continuous variables, and Wilcoxon rank sum tests for continuous variables with skewed distributions. Similar comparisons were performed across categories of the other sleep parameters (data not shown).
Random-effects models were used to study the association between sleep parameters and changes in cognition over time. These models account for between-participant variation and within-participant correlation of repeated outcomes.40 The random-effect terms included both the intercept and the slope of the cognitive measurements over time, allowing for individual time trends for each participant. Variances and covariances were estimated using the restricted maximum likelihood method. Time was modeled as a continuous covariate, measured as years from the Sleep Visit. A quadratic term for time was considered to account for a nonlinear time trend; in all models the interaction of the quadratic term for time and the sleep parameters were not significant so time was modeled linearly. All models were minimally adjusted for age, race, and clinic site. Additional covariates (fixed effects) were selected for inclusion in a multivariable model by examining both the univariate association of the covariate and the sleep parameters and the association with the 3MS and Trails B outcomes in unadjusted random-effects models. Age, race, clinic site, BMI, and those covariates associated with both a sleep parameter and an outcome at P < 0.10 were kept in all multivariable models, which included education, number of depressive symptoms, number of comorbidities, presence of an IADL impairment, benzodiazepine use, antidepressant use, self-reported health status, physical activity, alcohol use, and smoking status. All continuous covariates were centered (value-mean) for use in the models. Change in cognition is presented as average change per year, calculated using the coefficients derived from the random-effects models. The continuous cognitive scores were transformed to meet model requirements (log- transformation for Trails B, cube transformation for 3MS) and back-transformed for display of results. The results for models with sleep parameters used as continuous variables are presented as a 1 standard deviation decrease for SE (11.68), a 30-min increase for WASO, a 1-unit increase for number of LWEP, a 1-h decrease for TST, and a 1 standard deviation increase for the PSQI (3.18) and ESS (3.62).
The association of the sleep parameters with clinically significant cognitive decline was assessed using logistic regression models. Minimally and multivariable adjusted models were performed as described previously. Results are presented as odds ratios and 95% confidence intervals (OR, 95% CI).
When significant associations were present, secondary analyses were performed, further adjusting multivariable models to include parameters of objectively measured sleep and self-reported sleep quality to determine if these associations with cognitive decline were independent.
All significance levels reported were two-sided and all analyses were conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC).
RESULTS
Characteristics of the Study Population
The analysis cohort was composed of 2,822 primarily Caucasian men (90.7%) with an average age of 76.0 ± 5.3 y at the Sleep Visit assessment. Almost half of the men (43%) had self-reported poor sleep quality (PSQI > 5) and 12% had self-reported excessive daytime sleepiness (ESS > 10). The average values of both self-reported and objectively measured TST were similar (self-reported 6.9 ± 1.2 h; objectively measured 6.4 ± 1.2 h), with approximately 11% of men with ≤ 5 h of sleep per night (self-reported 10.9%, objective 11.6%) and about 6% with a long sleep duration (> 8 h per night; self-reported 5.2%, objective 6.7%). Although mean values from objectively and subjectively measured TST were similar, correlation between the two measures was modest (rho = 0.30). Based on objective measures, men had an average SE of 79%, an average WASO of 76 min, and an average of seven LWEP. The men on average had high levels of cognitive function at the initial visit: 117.2 ± 50.7 sec for Trails B completion time, 93.6 ± 4.5 points for the 3MS.
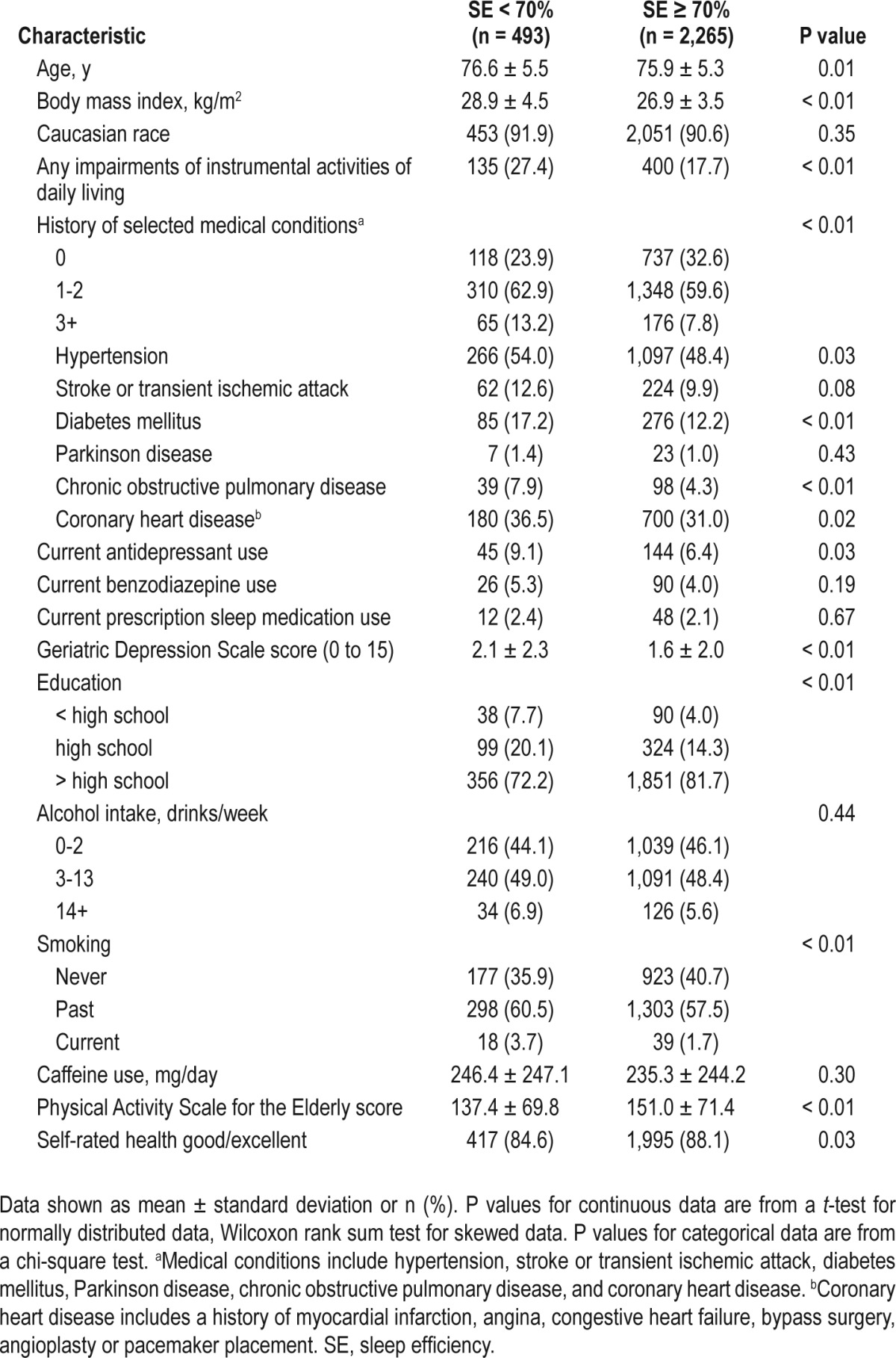
Many participant characteristics differed significantly across categories of sleep efficiency (Table 1). Compared to those with higher SE (≥ 70%), those men with lower SE (< 70%) on average were older, had higher BMI, had more depressive symptoms, and had lower levels of physical activity. Men with SE < 70% were also more likely to have an IADL impairment or have one or more medical conditions. They were more likely to take antidepressants, had lower levels of education, were more likely to smoke, and less likely to report good or excellent self-reported health status.
Table 1.
Sleep visit characteristics by sleep efficiency
By Visit 3, an average of 3.4 ± 0.5 y later, on average the men declined on both cognitive tests. The unadjusted average increase in time to complete the Trails B test was 9.1 ± 49.2 sec and the 3MS score was lower by 1.3 ± 5.5 points. Of clinical significance, at Visit 3, 18.8% of men were considered to have cognitive decline based on the 3MS (five-point decline).
Association of Objectively Measured Sleep Parameters and Cognitive Decline
The adjusted annualized change in both Trails B completion time and 3MS score by objectively measured sleep parameters are summarized in Table 2. After multivariable adjustment, there was an association seen with the number of LWEP and Trails B, with an average annualized increase in test time of 2.3 sec for a 1-unit increase in the number of LWEP. For 3MS, the annualized decrease in test score was larger on average by half a point for those men with SE < 70%, compared to those with SE ≥ 70%. The association of clinically significant change in the two cognitive outcomes and objectively measured sleep is shown in Table 3. There was a consistent association seen between disturbed sleep and clinically significant worsening of Trails B test completion time. After multivariable adjustment, higher levels of WASO and LWEP and lower levels of SE were associated with an approximate 1.5-fold increase in odds of clinically significant decline as defined by the Trails B test (OR [95% CI]: SE < 70% versus SE ≥ 70%: 1.53 [1.07, 2.18]; WASO ≥ 90 min versus WASO < 90 min: 1.47 [1.09, 1.98]; eight or more LWEP versus fewer than eight: 1.38 [1.02, 1.86]). Having eight or more LWEP during the night compared to fewer than eight was related to a 1.4-fold increase in the odds of clinically significant decline of 3MS score (OR [95% CI]: eight or more LWEP versus fewer than eight: 1.36 [1.09, 1.71]). To help interpret these effect sizes, the associations of a 5 y increase in age and clinically significant cognitive decline from these multivariable models are presented (OR [95% CI]: Trails B: 1.44 [1.25, 1.66]; 3MS:1.36 [1.09, 1.71]). Therefore, higher levels of SE, WASO, and more LWEP were associated with an equivalent or slightly larger odds of clinically significant cognitive decline as a 5-y increase in age. No associations were seen with objectively measured TST and cognitive decline.
Table 2.
Adjusted annualized mean cognitive decline by objectively measured sleep parameters

Table 3.
Association of sleep parameters and clinically significant cognitive decline
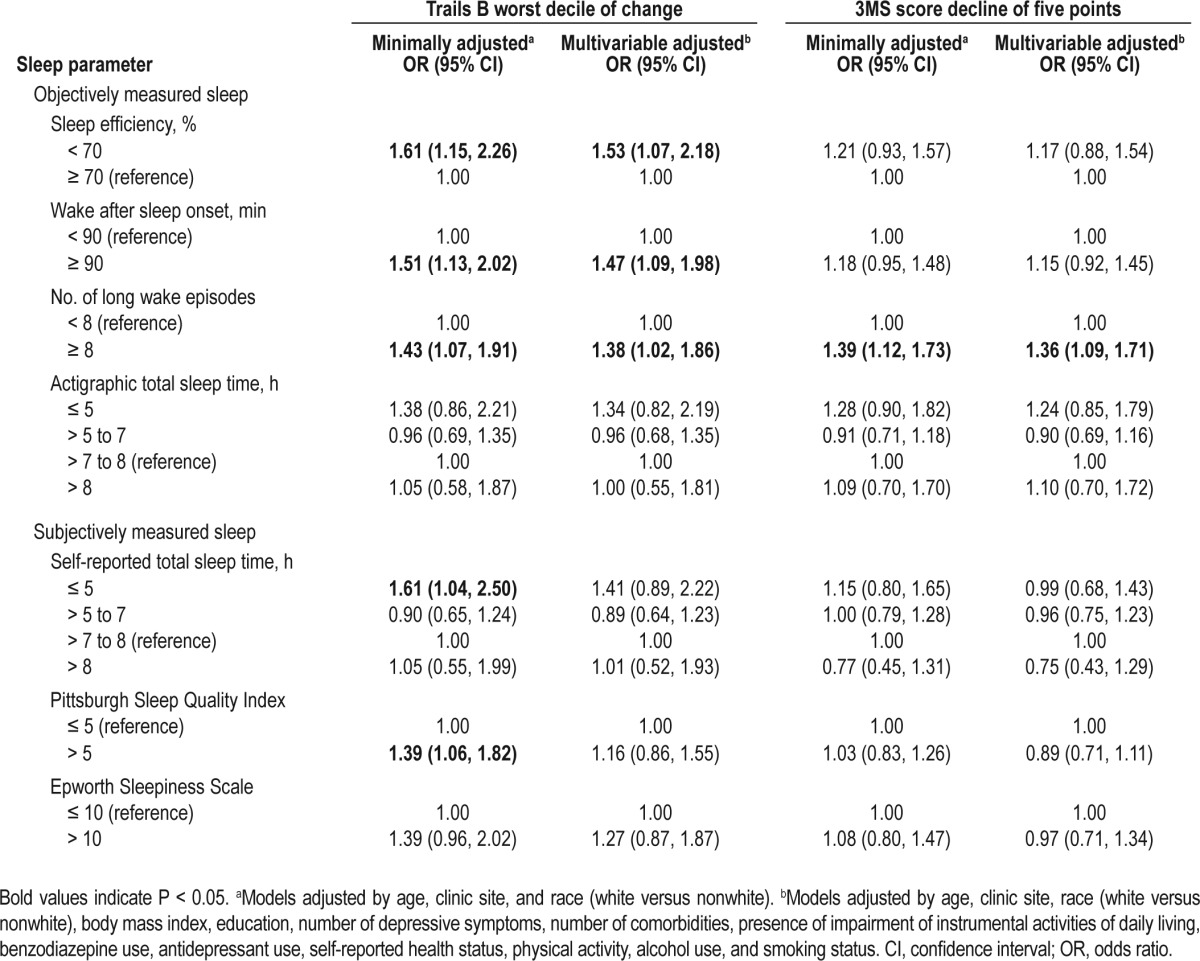
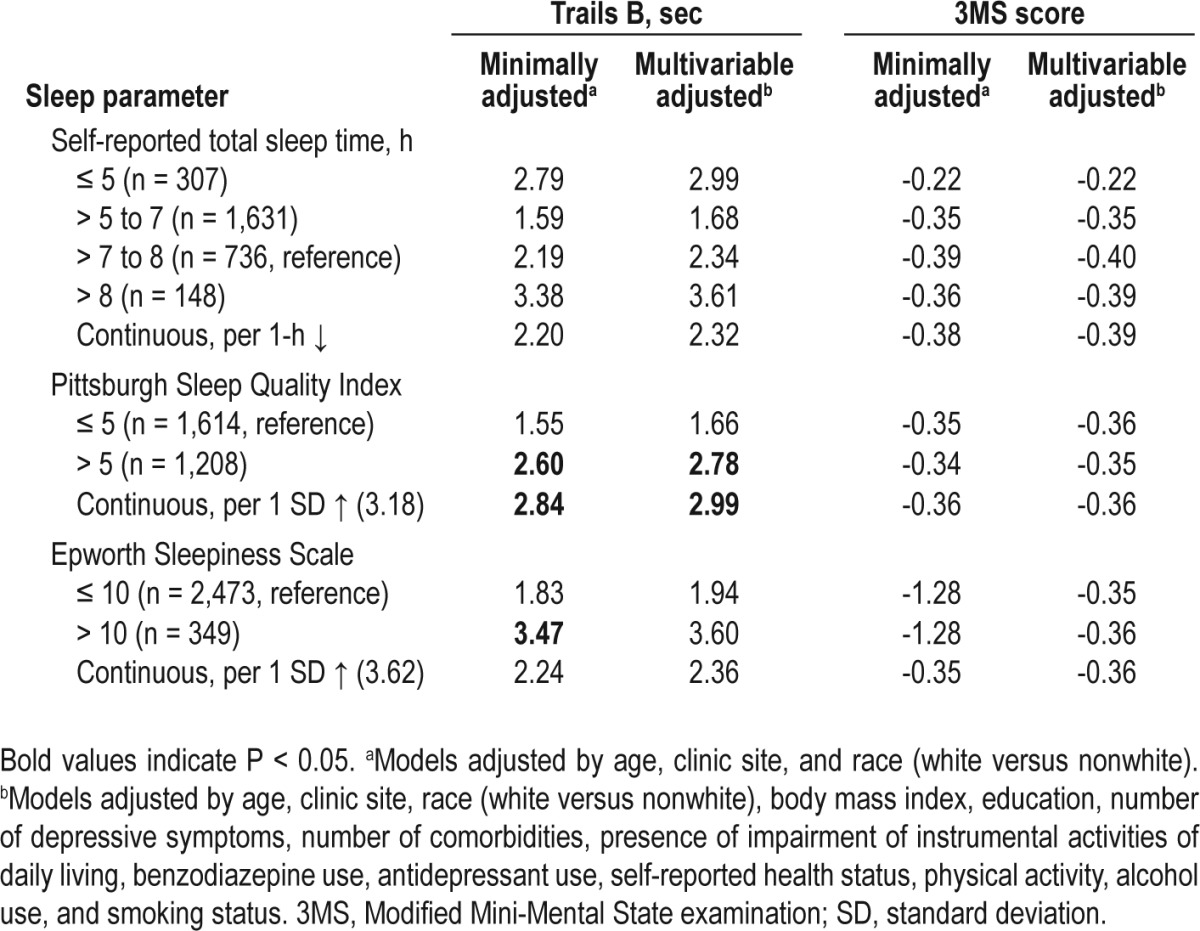
Association of Subjectively Measured Sleep Parameters and Cognitive Decline
No associations were seen with self-reported TST and cognitive decline (Table 4). After multivariable adjustment, an association between self-reported poor sleep quality and Trails B test completion time was seen, with an average annualized increase in test time of 2.8 sec more for those with PSQI > 5 than those with PSQI ≤ 5. In minimally adjusted models, men with excessive daytime sleepiness (ESS > 10) had a larger annualized increase in test completion time compared to those with ESS ≤ 10 (ESS > 10: 3.5 sec; ESS ≤ 10: 1.8 sec, P = 0.04). This association lost significance after further adjustment for multiple confounders. After adjustment for multiple confounders there were no significant associations seen between subjectively measured sleep and clinically significant cognitive decline (Table 3).
Table 4.
Adjusted annualized mean cognitive decline by subjectively measured sleep parameters
Secondary Analyses
The association of SE and WASO with clinically significant change in Trails B remained significant after further adjusting the multivariable models by self-reported sleep quality (PSQI) (OR [95% CI]: SE < 70% versus SE ≥ 70%: 1.47 [1.02, 2.10]; WASO ≥ 90 min versus < 90 min: 1.42 [1.05, 1.92]). The association of LWEP with clinically significant change in Trails B remained similar in effect size but lost statistical significance after further adjusting the multivariable models by PSQI (OR [95% CI]: eight or more LWEP versus fewer than eight: 1.33 [0.99, 1.80], P = 0.06).
DISCUSSION
In this cohort of community-dwelling older men, there was a consistent relationship of disturbed sleep (lower SE, higher levels of WASO, and more LWEP) with decline in executive function as measured by an increase in time to complete the Trails B test that was similar in magnitude to the effect of a 5-y increase in age. Little association was seen with subjective sleep and cognitive decline, with the exception of an association seen between sleep quality as measured by the PSQI and a worsening of Trails B test completion time. The association of SE and WASO with decline in executive function was robust to further adjustment for self-reported sleep quality.
The consistent relationship seen with disturbed sleep and decline on the Trails B test and minimal associations seen with disturbed sleep and decline on the 3MS may be because the associations vary across specific domains of cognitive function. The Trails B test, a measure of attention and executive function, can be considered a test of prefrontal cortical function.41 It has been suggested that prefrontal cortex functioning is sensitive to sleep.42
Two previous studies explored the association of objectively measured sleep and development of mild cognitive impairment (MCI) or dementia in cognitively intact participants. One study of 737 older men and women found a positive association with sleep fragmentation and development of dementia after 3-6 y of follow-up.17 Another study of 298 older women did not note an association of WASO with development of MCI or dementia, although compared with those in the lowest tertile of objectively measured WASO, those in the highest tertile did have a suggestion of an elevated odds that did not reach statistical significance (OR, 95% CI 1.79 [0.97, 3.29]).18
The current study is largely confirmatory to prior studies finding no association of TST and cognitive decline, with TST measured both objectively16,18 and subjectively.15 Over 1 y of follow-up, one study did find an association with self-reported short sleep and development of cognitive impairment among men that was not replicated here or in other studies.14
A few studies did find an association with subjectively measured daytime sleepiness and cognitive decline that was not reproduced in this current study.10,11,13 One study found no association of daytime sleepiness and cognitive impairment after 2 y of follow-up, but did note an association after 10 y of follow-up.13 The other two studies had follow-up times of 3 and 10 y. Perhaps follow-up longer than the 3.4 y in this study is needed to observe an association. Because daytime sleepiness is easily measured by questionnaire, it could be a useful tool in assessing risk of future cognitive decline if other analyses confirm this association.
The underlying mechanisms relating disturbed sleep to cognitive decline remain unknown. One potential mechanism that might drive this association is lack of recuperation or restoration. During sleep the rate of anabolism is at a peak, with repair taking place in both the central nervous system and total body.43 Memory consolidation takes place during sleep, and disruption of sleep may affect this process.44 Recent animal research suggested that regardless of TST, a minimal amount of uninterrupted sleep was needed for memory consolidation.45 A small case control study in humans where TST and sleep architecture were similar between groups showed increased arousals from sleep predicted lack of overnight improvement in sleep-dependent memory processes.46 Other mechanisms may be the associations of inflammation or metabolic dysfunction with both sleep and cognitive decline.47–49
This study has several strengths. The study had a large population of cognitively intact community-dwelling older men who were not selected for inclusion based on sleep problems. There were a number of validated measures of sleep characteristics, including both subjective and objective measures. Adjustments for multiple potential confounding factors were made, suggesting these associations were not explained by other covariates including depression, comorbidities, medication use, education, or lifestyle.
This study also had limitations. The findings may not be generalizable to populations other than community-dwelling older men. Adjustment for numerous covariates was performed, but there may be unmeasured confounders that may affect the results. The cognitive battery of tests was somewhat limited and only included measures of global cognition and executive function.
In conclusion, among older community-dwelling men, reduced sleep efficiency, greater nighttime wakefulness, greater number of LWEP, and poor self-reported sleep quality were associated with subsequent cognitive decline. These associations were stronger for the cognitive domain of executive function than global cognition. Daytime sleepiness and sleep duration were not related to subsequent cognitive decline. Further study is needed to examine if these associations hold after longer follow-up and vary by specific cognitive domains. More studies with adjudication of events such as development of MCI or dementia would be beneficial. Exploration of possible underlying mechanisms of this potential association is also needed.
DISCLOSURE STATEMENT
This was not an industry supported study. The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Institute on Aging (NIA), the National Cancer Institute (NCI), the National Center for Research Resources (NCRR), and NIH Roadmap for Medical Research under the following grant numbers: U01 AR45580, U01 AR45614, U01 AR45632, U01 AR45647, U01 AR45654, U01 AR45583, U01 AG18197, U01-AG027810, and UL1 RR024140. The National Heart, Lung, and Blood Institute (NHLBI) provides funding for the MrOS Sleep ancillary study “Outcomes of Sleep Disorders in Older Men” under the following grant numbers: R01 HL071194, R01 HL070848, R01 HL070847, R01 HL070842, R01 HL070841, R01 HL070837, R01 HL070838, and R01 HL070839. Dr. Yaffe is supported by a grant from the NIA, K24 AG031155; serves on DSMB's for Takeda, Inc and a study sponsored by the NIH; is a member of the Beeson Advisory Committee; and is a consultant for Novartis and Eli Lilly. Dr. Ancoli-Israel is a consultant or on the advisory board for Astra Zeneca, Ferring Pharmaceuticals Inc, GaxoSmithKline, Hypnocore, Johnson & Johnson, Merck, NeuroVigil Inc, and Purdue Pharma LP. Dr. Redline's institution has received grant funding from ResMed, Inc, Philips Respironics, and ResMed Foundation and equipment from them for use in NIH studies. The other authors have indicated no financial conflicts of interest. The analysis was performed at California Pacific Medical Center Research Institute, San Francisco, CA.
ABBREVIATIONS
- MrOS Sleep Study
Outcomes of Sleep Disorders in Men Study
- MrOS
Osteoporotic Fractures in Men Study
- PSG
polysomnography
- 3MS
Modified Mini-Mental State examination
- Trails B Test
Trail Making Test–Part B
- TST
total sleep time
- PSQI
Pittsburgh Sleep Quality Index
- ESS
Epworth Sleepiness Scale
- SE
sleep efficiency
- WASO
wake after sleep onset
- LWEP
number of long wake episodes
- IADL
instrumental activities of daily living
- BMI
body mass index
- OR
odds ratio
- CI
confidence interval
- MCI
mild cognitive impairment
REFERENCES
- 1.Foley D, Ancoli-Israel S, Britz P, et al. Sleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America Survey. J Psychosom Res. 2004;56:497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 2.Ott A, Breteler MM, van Harskamp F, et al. Incidence and risk of dementia. The Rotterdam Study. Am J Epidemiol. 1998;147:574–80. doi: 10.1093/oxfordjournals.aje.a009489. [DOI] [PubMed] [Google Scholar]
- 3.Brookmeyer R, Gray S, Kawas C. Projections of Alzheimer's disease in the United States and the public health impact of delaying disease onset. Am J Public Health. 1998;88:1337–42. doi: 10.2105/ajph.88.9.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blackwell T, Yaffe K, Ancoli-Israel S, et al. Poor sleep is associated with impaired cognitive function in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci. 2006;61:405–10. doi: 10.1093/gerona/61.4.405. [DOI] [PubMed] [Google Scholar]
- 5.Blackwell T, Yaffe K, Ancoli-Israel S, et al. for the Osteoporotic Fractures in Men (MrOS) Study Group. Association of Sleep Characteristics and Cognition in Older Community-Dwelling Men: the MrOS Sleep Study. Sleep. 2011;34:1347–56. doi: 10.5665/SLEEP.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Foley DJ, Masaki K, White L, et al. Sleep-disordered breathing and cognitive impairment in elderly Japanese-American men. Sleep. 2003;26:596–9. doi: 10.1093/sleep/26.5.596. [DOI] [PubMed] [Google Scholar]
- 7.Ohayon MM, Vecchierini MF. Daytime sleepiness and cognitive impairment in the elderly population. Arch Intern Med. 2002;162:201–8. doi: 10.1001/archinte.162.2.201. [DOI] [PubMed] [Google Scholar]
- 8.Nebes RD, Buysse DJ, Halligan EM, Houck PR, Monk TH. Self-reported sleep quality predicts poor cognitive performance in healthy older adults. J Gerontol B Psychol Sci Soc Sci. 2009;64:180–7. doi: 10.1093/geronb/gbn037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cricco M, Simonsick EM, Foley DJ. The impact of insomnia on cognitive functioning in older adults. J Am Geriatr Soc. 2001;49:1185–9. doi: 10.1046/j.1532-5415.2001.49235.x. [DOI] [PubMed] [Google Scholar]
- 10.Elwood PC, Bayer AJ, Fish M, Pickering J, Mitchell C, Gallacher JE. Sleep disturbance and daytime sleepiness predict vascular dementia. J Epidemiol Community Health. 2011;65:820–4. doi: 10.1136/jech.2009.100503. [DOI] [PubMed] [Google Scholar]
- 11.Foley D, Monjan A, Masaki K, et al. Daytime sleepiness is associated with 3-year incident dementia and cognitive decline in older Japanese-American men. J Am Geriatr Soc. 2001;49:1628–32. doi: 10.1046/j.1532-5415.2001.t01-1-49271.x. [DOI] [PubMed] [Google Scholar]
- 12.Jelicic M, Bosma H, Ponds RW, Van Boxtel MP, Houx PJ, Jolles J. Subjective sleep problems in later life as predictors of cognitive decline. Report from the Maastricht Ageing Study (MAAS) Int J Geriatr Psychiatry. 2002;17:73–7. doi: 10.1002/gps.529. [DOI] [PubMed] [Google Scholar]
- 13.Keage HA, Banks S, Yang KL, Morgan K, Brayne C, Matthews FE. What sleep characteristics predict cognitive decline in the elderly? Sleep Med. 2012;13:886–92. doi: 10.1016/j.sleep.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Potvin O, Lorrain D, Forget H, et al. Sleep quality and 1-year incident cognitive impairment in community-dwelling older adults. Sleep. 2012;35:491–9. doi: 10.5665/sleep.1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tworoger SS, Lee S, Schernhammer ES, Grodstein F. The association of self-reported sleep duration, difficulty sleeping, and snoring with cognitive function in older women. Alzheimer Dis Assoc Disord. 2006;20:41–8. doi: 10.1097/01.wad.0000201850.52707.80. [DOI] [PubMed] [Google Scholar]
- 16.Cohen-Zion M, Stepnowsky C, Marler, Shochat T, Kripke DF, Ancoli-Israel S. Changes in cognitive function associated with sleep disordered breathing in older people. J Am Geriatr Soc. 2001;49:1622–7. doi: 10.1046/j.1532-5415.2001.t01-1-49270.x. [DOI] [PubMed] [Google Scholar]
- 17.Lim AS, Kowgier M, Yu L, Buchman AS, Bennett DA. Sleep fragmentation and the risk of incident Alzheimer's disease and cognitive decline in older persons. Sleep. 2013;36:1027–32. doi: 10.5665/sleep.2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yaffe K, Laffan AM, Harrison SL, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA. 2011;306:613–9. doi: 10.1001/jama.2011.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study--a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26:569–85. doi: 10.1016/j.cct.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Blank JB, Cawthon PM, Carrion-Petersen ML, et al. Overview of recruitment for the osteoporotic fractures in men study (MrOS) Contemp Clin Trials. 2005;26:557–68. doi: 10.1016/j.cct.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 21.Ancoli-Israel S, Cole R, Alessi C, et al. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26:342–92. doi: 10.1093/sleep/26.3.342. [DOI] [PubMed] [Google Scholar]
- 22.Motionlogger® User's Guide. Act Millenium. Ardsley NY: Ambulatory Monitoring, Inc; [Google Scholar]
- 23.Action-W User's Guide, Version 2.0. Ardsley NY: Ambulatory Monitoring, Inc; [Google Scholar]
- 24.Blackwell T, Ancoli-Israel S, Gehrman PR, Schneider JL, Pedula KL, Stone KL. Actigraphy scoring reliability in the study of osteoporotic fractures. Sleep. 2005;28:1599–605. doi: 10.1093/sleep/28.12.1599. [DOI] [PubMed] [Google Scholar]
- 25.Jean-Louis G, Kripke DF, Mason WJ, Elliot JA, Youngstedt SD. Sleep estimation from wrist movement quantified by different actigraphic modalities. J Neurosci Methods. 2001;105:185–91. doi: 10.1016/s0165-0270(00)00364-2. [DOI] [PubMed] [Google Scholar]
- 26.Blackwell T, Ancoli-Israel S, Redline S, Stone KL for the Osteoporotic Fractures in Men (MrOS) Study Group. Factors that May Influence the Classification of Sleep-Wake by Wrist Actigraphy: The MrOS Sleep Study. J Clin Sleep Med. 2011;7:357–67. doi: 10.5664/JCSM.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buysse DJ, Reynolds CF, III, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 28.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 29.Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376–81. doi: 10.1093/sleep/15.4.376. [DOI] [PubMed] [Google Scholar]
- 30.Reitan R. Validity of the Trail Making Test as an indicator of organic brain damage. Percept Mot Skills. 1958;8:271–6. [Google Scholar]
- 31.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48:314–8. [PubMed] [Google Scholar]
- 32.Kuller LH, Lopez OL, Newman A, et al. Risk factors for dementia in the cardiovascular health cognition study. Neuroepidemiology. 2003;22:13–22. doi: 10.1159/000067109. [DOI] [PubMed] [Google Scholar]
- 33.Ganguli M, Belle S, Ratcliff G, et al. Sensitivity and specificity for dementia of population-based criteria for cognitive impairment: the MoVIES project. J Gerontol. 1993;48:M152–61. doi: 10.1093/geronj/48.4.m152. [DOI] [PubMed] [Google Scholar]
- 34.Sheikh J, Yesavage J. Clinical Gerontology: A Guide to Assessment and Intervention. New York: The Haworth Press; 1986. Geriatric Depression Scale: recent evidence and development of a shorter version; pp. 165–73. [Google Scholar]
- 35.Pahor M, Chrischilles EA, Guralnik JM, et al. Drug data coding and analysis in epidemiologic studies. Eur J Epidemiol. 1994;10:405–11. doi: 10.1007/BF01719664. [DOI] [PubMed] [Google Scholar]
- 36.Washburn RA, Smith KW, Jette AM, et al. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–62. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 37.National Center for Health Statistics, J. E. Fitti and M. G. Kovar: The Supplement on Aging to the 1984 National Health Interview Survey. Public Health Service. Washington. U.S: Government Printing Office; 1987. Oct, Vital and Health Statistics. Series 1, No. 21. DHHSPub. No. (PHS) 87-1323. [PubMed] [Google Scholar]
- 38.Pincus T, Summey JA, Soraci SA, Jr, et al. Assessment of patient satisfaction in activities of daily living using a modified Stanford Health Assessment Questionnaire. Arthritis Rheum. 1983;26:1346–53. doi: 10.1002/art.1780261107. [DOI] [PubMed] [Google Scholar]
- 39.Barone JJ, Roberts HR. Caffeine consumption. Food Chem Toxicol. 1996;34:119–29. doi: 10.1016/0278-6915(95)00093-3. [DOI] [PubMed] [Google Scholar]
- 40.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38:963–74. [PubMed] [Google Scholar]
- 41.Andrew MK, Fisk JD, Rockwood K. Social vulnerability and prefrontal cortical function in elderly people: a report from the Canadian Study of Health and Aging. Int Psychogeriatr. 2011;23:450–8. doi: 10.1017/S1041610210001195. [DOI] [PubMed] [Google Scholar]
- 42.Muzur A, Pace-Schott EF, Hobson JA. The prefrontal cortex in sleep. Trends Cogn Sci. 2002;6:475–81. doi: 10.1016/s1364-6613(02)01992-7. [DOI] [PubMed] [Google Scholar]
- 43.Shapiro CM, Flanigan MJ. ABC of sleep disorders. Function of sleep. BMJ. 1993;306:383–5. doi: 10.1136/bmj.306.6874.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rauchs G, Bertran F, Guillery-Girard B, et al. Consolidation of strictly episodic memories mainly requires rapid eye movement sleep. Sleep. 2004;27:395–401. doi: 10.1093/sleep/27.3.395. [DOI] [PubMed] [Google Scholar]
- 45.Rolls A, Colas D, Adamantidis A, et al. Optogenetic disruption of sleep continuity impairs memory consolidation. Proc Natl Acad Sci U S A. 2011;108:13305–10. doi: 10.1073/pnas.1015633108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Djonlagic I, Saboisky J, Carusona A, Stickgold R, Malhotra A. Increased sleep fragmentation leads to impaired off-line consolidation of motor memories in humans. PLoS One. 2012;7:e34106. doi: 10.1371/journal.pone.0034106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Craft S, Foster TC, Landfield PW, Maier SF, Resnick SM, Yaffe K. Session III: Mechanisms of age-related cognitive change and targets for intervention: inflammatory, oxidative, and metabolic processes. J Gerontol A Biol Sci Med Sci. 2012;67:754–9. doi: 10.1093/gerona/gls112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grandner MA, Buxton OM, Jackson N, Sands-Lincoln M, Pandey A, Jean-Louis G. Extreme sleep durations and increased C-reactive protein: effects of sex and ethnoracial group. Sleep. 2013;36:769–79. doi: 10.5665/sleep.2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Matthews KA, Dahl RE, Owens JF, Lee L, Hall M. Sleep duration and insulin resistance in healthy black and white adolescents. Sleep. 2012;35:1353–8. doi: 10.5665/sleep.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]


