Abstract
Regionalized trauma care has been widely implemented in the United States, with field triage by emergency medical services (EMS) playing an important role in identifying seriously injured patients for transport to major trauma centers. In this study we estimated hospital-level differences in the adjusted cost of acute care for injured patients transported by 94 EMS agencies to 122 hospitals in 7 regions, overall and by injury severity. Among 301,214 patients, the average adjusted per episode cost of care was $5,590 higher in a level 1 trauma center than in a nontrauma hospital. We found hospital-level differences in cost among patients with minor, moderate, and serious injuries. Of the 248,342 low-risk patients—those who did not meet field triage guidelines for transport to trauma centers—85,155 (34.3 percent) were still transported to major trauma centers, accounting for up to 40 percent of acute injury costs. Adhering to field triage guidelines that minimize the overtriage of low-risk injured patients to major trauma centers could save up to $136.7 million annually in the seven regions we studied.
Trauma care ranks second as a contributor to total US health care spending, exceeded only by heart disease.1 The annual cost of treating seriously injured adults in the United States is estimated to be $30 billion (in 2008 dollars),2 and the estimated cost of treating all injured patients is $163 billion (in 2008 dollars)—which represents approximately 10 percent of the total US medical expenditures.3
Developing more-efficient models for injury care is increasingly important because of the common occurrence of injury, finite trauma center resources, the continued escalation of US health care costs, and persistent financial threats facing trauma centers.4 However, there has been relatively little research that describes and evaluates the drivers of acute injury costs and methods for providing high-value trauma care while minimizing unnecessary expenditures.
Regionalized trauma care and trauma centers have been shown to improve survival among seriously injured adults5–9 and children.10–12 The cost of providing care at major trauma centers is higher than at nontrauma hospitals.13–15 However, these specialized centers have been shown to be cost-effective, particularly for young patients with severe injuries.13
Less is known about the cost implications of treating patients without serious injuries at major trauma centers. Because the number of patients without serious injuries is vastly larger than the number of those with serious injuries, and because the benefit of major trauma centers is limited to seriously injured patients,5–12 efficiently matching patients’ needs to hospitals’ resources and capability is vital to improving the value of trauma care.
Emergency medical services (EMS) serve a large number of injured patients and play a critical role in directing seriously injured patients to major trauma centers. Because serious injuries may not be immediately apparent, and because transporting all injured patients to major trauma centers would quickly overwhelm trauma resources, most US EMS and trauma systems use national field triage guidelines to identify seriously injured patients for transport to major trauma centers. Originally developed in 1987, the triage guidelines have been periodically revised based on new research16,17 and are widely implemented by EMS agencies throughout the United States.
Undertriage (transporting seriously injured patients to nontrauma centers) and overtriage (transporting patients without serious injuries to major trauma centers) represent mismatches between need and capability and are important problems in trauma systems that must be addressed.18 Because it is not realistic to markedly reduce both under- and overtriage,19 the prevailing philosophy in the United States has been to minimize undertriage (with the goal of subjecting no more than 5 percent of cases to undertriage) instead of overtriage (the current goal is no more than 50 percent of cases).18 Nonetheless, the development and implementation of field triage guidelines are modifiable aspects of the health care delivery system.
In this study we sought to compare the adjusted total cost of acute injury care—that is, EMS, emergency department (ED), and hospital admission costs—by hospital type and injury severity among a broad cohort of injured patients transported by EMS to acute care hospitals in seven regions of the western United States. We also evaluated the potential cost savings that would accrue from eliminating overtriage—transporting low-risk injured patients to major trauma centers.
Study Data And Methods
DESIGN
This was a multiregion, population-based, retrospective cohort study. Sixteen Institutional Review Boards in the seven regions involved approved this protocol and waived the requirement for informed consent.
SETTING
The study included injured children and adults evaluated by ninety-four EMS agencies and transported to 122 hospitals (15 level 1 trauma centers, 8 level 2 trauma centers, and 99 nontrauma centers) in seven regions across the western United States from January 1, 2006, through December 31, 2008. The regions were Portland, Oregon, and Vancouver, Washington (four counties); King County, Washington; Sacramento, California (two counties); San Francisco, California; Santa Clara, California (two counties); Salt Lake City, Utah (four counties); and Denver County, Colorado. Each region had a predefined geographic “footprint,” including a central metropolitan area and surrounding suburban and rural areas defined by EMS agency service areas. All of the regions had established trauma systems with designated major trauma centers.
The process of field triage in these trauma systems is guided by the national guidelines and is intended to identify seriously injured patients in need of immediate transport to major trauma centers. The guidelines consist of twenty-four criteria organized into a four-step algorithm (physiologic, anatomic, mechanism, and special considerations “steps”).17
After responding to a 911 call about an injured patient, EMS providers typically make the triage decision based on criteria represented in the algorithm, including the use of their own judgment.20 When an EMS provider determines that an injured patient meets one or more of the field triage criteria (these cases are called field trauma activations in this article), the patient is triaged to the ED of a major (level 1 or 2) trauma center. Such centers provide tertiary trauma services—including twenty-four-hour availability of a trauma surgeon and specialists such as a neuro-surgeon, surgical critical care, and the use of trauma-specific quality assurance processes—that are all required to care effectively for patients with the most complex trauma conditions.18 Injured patients who do not meet triage criteria (cases called nonfield activations or triage-negative cases here) may be transported to an ED based on patient choice, proximity, ambulance diversion status, and other factors.20,21
PATIENT POPULATION
The study sample included all injured patients for whom the 911 EMS system was activated within the seven predefined geographic regions and for whom the call resulted in transport to an acute care hospital (either a trauma center or not). The sample included patients with minor, moderate, and serious injuries.
Injured patients arriving at hospitals by means other than EMS (such as walk-in patients and those who came by private automobile) were excluded from the sample, as were interhospital transfers without an initial presentation involving EMS. However, we did track subsequent interhospital transfers following the initial EMS transport for patients in the sample. We also excluded EMS calls with no patient contact and patients who were not transported—for example, those who refused transport or who died before they could be transported.
DATA PROCESSING AND DATABASE DEVELOPMENT
To construct the sample, each participating EMS agency transmitted its electronic patient care reports to a central data coordinating center. In regions where multiple EMS agencies (such as fire departments and private ambulance agencies) care for the same patients, we matched EMS records at the patient level. We then matched EMS records to hospital records in trauma registries, state hospital discharge databases (for admitted patients), and state ED databases (for patients not admitted to a hospital) through probabilistic linkage. We used LinkSolv software, version 8.2.
The development of our database has been previously described,22 including the validation of all-electronic data collection processes.23 The record linkage methodology has been validated for matching ambulance records to trauma registry data24 and rigorously evaluated in this database.22 In Appendix Exhibits 1 and 2, we detail how we constructed the database and sample.25
VARIABLES
We used a comprehensive approach to identify field trauma activations, including a specific mention of trauma triage criteria in the EMS patient care report; documentation of field trauma activation (or similar wording, depending on local terminology) by the EMS provider; an EMS-recorded trauma identification number (used in some regions as a mechanism for tracking injured patients who enter a trauma system); a matched record from the local trauma registry specifying EMS field trauma activation; and transcribed phone records from regions where EMS personnel must call ahead to the trauma center before arriving with field trauma activation patients. All other patients were considered triage negative. Trauma activation status was considered independent of the type of hospital to which the patient was transported.
We collected additional variables through EMS and hospital charts. These variables included patients’ demographic characteristics, insurance status, out-of-hospital physiologic measures, mechanism of injury, out-of-hospital procedures, transport mode (ground versus helicopter), injury severity measures (described below), surgical interventions, blood transfusions, hospital length-of-stay, in-hospital mortality, and cost (also described below). Additional variables were hospital type and whether or not there was an interhospital transfer.
Acute care hospitals were categorized by trauma center level (level 1, level 2, or nontrauma center), based on their American College of Surgeons accreditation status and state-level designations. For purposes of this analysis, we coded hospital type on the basis of final destination to represent the type of facility in which patients received the majority of their care.
Injury severity measures were not collected in state discharge or ED databases. Therefore, we used International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), codes and the ICDPIC mapping function in the statistical analysis software Stata, version 11,26 to convert diagnosis codes to Injury Severity Score27 (ISS) and ICD-9-CM-based Injury Severity Score (ICISS) values. Previous studies have validated the process of mapping administrative diagnosis codes to generate anatomic injury scores.28,29 In addition, we have previously validated ICDPIC-generated injury scores against chart-abstracted scores in our database.30 We defined injury severity categories using ISS27 as follows: serious injury is ISS =16; moderate injury is ISS 9–15; and minor injury is ISS 0–8.
OUTCOME
The primary outcome was total acute care cost. We evaluated the cost per patient based on the following four sources of acute care expenses: initial EMS transport from the scene of the injury; ED care; hospitalization (for admitted patients); and interhospital transfer, including the cost of initial ED evaluation and EMS interhospital transport. We estimated the per unit cost of ambulance transport from a separate sample of injured Medicare fee-for-service patients transported by EMS in Oregon and Washington. We obtained patient-level ED and in-hospital facility charges for all patients with linked hospital records.
ED and hospital charges were converted to costs using hospital- and year-specific cost-to-charge ratios.31,32 We estimated professional fees from facility costs by applying a conversion factor (1.27) that had previously been calculated for injured patients using the Truven Health Analytics MarketScan database.13 For patients requiring an interhospital transfer, we estimated the per unit cost of the initial ED evaluation and EMS interhospital transport, using the previously described Medicare fee-for-service sample.
We did not evaluate costs beyond the acute care period (for example, costs for postdischarge follow-up, outpatient visits, or rehabilitation) or costs related to loss of productivity or workdays. All costs were adjusted to 2008 US dollars using a region-specific medical Consumer Price Index.33
DATA ANALYSIS
The primary analysis included all injured patients transported by EMS in the seven regions, whether or not a hospital record could be linked to the EMS record. This strategy preserved the population-based sampling design and minimized bias in the analysis. We used multiple imputation34 through flexible chains regression models35 to handle missing values.
Adjusted estimates for total costs were generated using multivariable generalized linear models with a gamma distribution and log link function to fit the positively skewed distribution of costs.36–38 To assess the robustness of our findings, we compared our primary results with sensitivity analyses using the nonimputed data set (the complete case analysis) and truncated versus nontruncated costs. Details regarding record linkage, imputation, and cost analyses are presented in Appendix Exhibit 3.25
LIMITATIONS
This study had important limitations. It was not designed as a cost-effectiveness analysis, and we did not evaluate patient outcomes. The cost-effectiveness of trauma care has previously been demonstrated.13
A central premise in this study is that only patients with serious injuries benefit from care in major trauma centers. Although this assumption is supported by many previous studies,5–12 most research demonstrating the benefit of trauma centers and trauma systems has focused on survival. There may be other benefits of major trauma centers for less seriously injured patients that are difficult to quantify (for example, fewer complications, missed diagnoses, and errors). Whether these potential benefits justify the increased costs of providing care in major trauma centers for patients without serious injuries remains unclear.
Other potential limitations include the characteristics of the study sample and unmeasured confounding. We did not include injured patients who did not use the 911 EMS system. Therefore, our findings apply only to injured patients transported by EMS and thus underestimate the total cost of acute injury care. Also, the use of a helicopter can increase costs in a trauma system.39 However, a relatively small proportion of patients in our sample were transported by helicopter.
If sicker patients tended to be transported to specific types of hospitals (such as level 1 trauma centers) and the observed variables did not completely explain that fact, such unmeasured confounding could have inflated the cost differences. We used several analytic strategies to account for confounding, and we used sensitivity analyses to assess the robustness of our results. Our cost estimates were similar to15 or more conservative than13 those in previous studies.
The cost analyses involved several assumptions, including the accuracy of using cost-to-charge ratios, per unit cost estimates for EMS transport, and a ratio to calculate professional fees from facility costs. Although there is potential for error with each of these steps, inclusion of all of these costs presents a more representative picture of total costs.
Furthermore, our data did not produce direct insights into why costs are higher at major trauma centers. For example, it is not clear if the explanation is that such centers have greater fixed resources to maintain, use cost shifting to account for higher rates of uncompensated care, make greater use of diagnostic testing and technology, or support education and research missions.
Our estimates for cost savings also assumed that nontrauma hospitals could handle larger patient volumes and navigate the obstacles of providing the on-call coverage40 that would be required to care for a wider variety of injured patients. In addition, actualizing the cost savings assumed that modifying ambulance transport protocols would not keep EMS personnel and vehicles out of commission longer than they are at present, and that trauma centers could survive with less revenue.
Study Results
CHARACTERISTICS OF SAMPLE AND TRIAGE PROCESSES
During the three-year study period, 301,214 injured patients were transported by ninety-four EMS agencies to 122 hospitals in the seven regions, resulting in total estimated acute care costs of more than $1.01 billion. Of those patients, 12,382 (4.1 percent) had serious injuries, 31,170 (10.4 percent) had moderate injuries, and 257,662 (85.5 percent) had minor injuries (Exhibit 1).
Exhibit 1.
Characteristics Of Injured Patients In The Study Sample Transported By Emergency Medical Services (EMS)
| Characteristics | Number | Percent |
|---|---|---|
|
DEMOGRAPHIC CHARACTERISTICS
| ||
| Age (years)a | ||
| Under 18 | 35,385 | 11.8 |
| 18–54 | 163,020 | 54.1 |
| 55 or older | 102,809 | 34.1 |
| Female | 145,188 | 48.2 |
|
| ||
|
PREHOSPITAL PHYSIOLOGY AND PROCEDURES
| ||
| Initial SBP ≤90 mmHg | 8,536 | 2.8 |
| Initial GCS ≤8 | 4,988 | 1.7 |
| Intubation attempt | 2,136 | 0.7 |
| Intravenous line placement | 91,254 | 30.3 |
|
| ||
|
FIELD TRIAGE STATUS
| ||
| 1 or more field triage criteria | 52,872 | 17.6 |
|
| ||
|
MECHANISM OF INJURY
| ||
| Gunshot wound | 3,137 | 1.0 |
| Stabbing | 6,082 | 2.0 |
| Assault | 27,266 | 9.1 |
| Fall | 118,856 | 39.5 |
| Motor vehicle crash | 90,844 | 30.2 |
| Other | 55,029 | 18.3 |
|
| ||
|
EMS TRANSPORT
| ||
| Air medical scene transport | 1,247 | 0.4 |
| Interhospital transfer | 7,759 | 2.6 |
|
| ||
|
HOSPITAL TYPE (FINAL DESTINATION)
| ||
| Level 1 trauma center | 98,709 | 32.8 |
| Level 2 trauma center | 28,800 | 9.6 |
| Nontrauma center | 173,705 | 57.7 |
|
| ||
|
OUTCOME
| ||
| ISSb | ||
| 0–8 | 257,662 | 85.5 |
| 9–15 | 31,170 | 10.4 |
| ≥16 | 12,382 | 4.1 |
| Major nonorthopedic surgeryc | 12,020 | 4.0 |
| Orthopedic surgery | 65,470 | 21.7 |
| In-hospital mortality | 4,447 | 1.5 |
SOURCE Authors’ analysis of the study data.
NOTES N = 301; 214 patients. SBP is systolic blood pressure. GCS is Glasgow Coma Scale. See Sternbach GL. The Glasgow coma scale. J Emerg Med. 2000;19(1):67–71.
Mean age is 45.7 years.
ISS is Injury Severity Score (see Note 27 in text). Mean ISS is 4.4. 0–8 is minor injury, 9–15 is moderate injury, and ≥16 is serious injury.
Brain, spine, neck, thorax, abdomen, interventional radiology, or vascular operative procedures during hospitalization.
Within the study population there were 52,872 (17.6 percent) field trauma activations. Field trauma activations identified 7,209 (58.2 percent) of the 12,382 seriously injured patients. In total, 7,686 (62.1 percent) patients with serious injuries were transported to major trauma centers—including patients identified by triage guidelines and those transported to trauma centers for other reasons—resulting in 37.9 percent undertriage.
Of the 288,832 patients with minor or moderate injuries, 119,823 (41.5 percent) received care at major trauma centers (92,016 patients at level 1 and 27,807 patients at level 2 centers). Although patients without serious injuries treated at major trauma centers are typically considered overtriaged, the extent and seriousness of injuries are generally not known at the time of EMS evaluation. To provide a more realistic perspective, there were 248,342 low-risk patients identified by field triage guidelines, of whom 85,155 (34.3 percent) were transported (overtriaged) to major trauma centers.
REGIONAL CHARACTERISTICS AND COSTS
Characteristics of the study regions and region-specific costs are detailed in Appendix Exhibit 4.25 The region-specific adjusted per patient cost of acute injury care ranged from $4,480 to $12,114, with an average cost of $9,651. Estimates of per capita injury costs—that is, the cost of acute injury care averaged across the population served—ranged from $29 to $283.
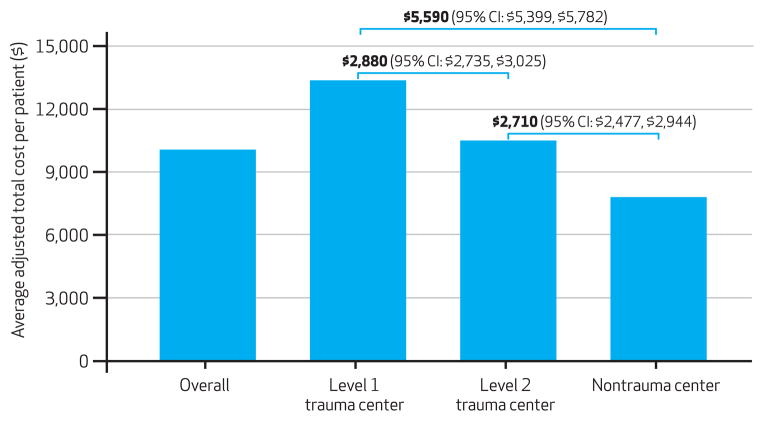
COST DIFFERENCES BY HOSPITAL TYPE
There were substantive differences in adjusted costs by hospital type, with patients who received care at level 1 trauma centers incurring the largest average cost (Exhibit 2). Detailed results from the regression analysis are provided in Appendix Exhibit 5.25
Exhibit 2.
Average Adjusted Total Cost Per Patient In The Study Sample, By Hospital Level
SOURCE Authors’ analysis of the study data. NOTES N = 301; 214 patients. Covariates in the multivariable generalized linear model were hospital type (level 1, level 2, or nontrauma center); age; sex; mechanism of injury (fifteen categories); field triage status (positive or negative); need for field ventilation (intubation or bag-valve mask ventilation); IV placement; Glasgow Coma Scale (see Exhibit 1 Notes); systolic blood pressure ≤90 mmHg; Injury Severity Score (see Note 27 in text); Injury Severity Score based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), codes; and need for major nonorthopedic surgery, orthopedic surgery, blood transfusion, or interhospital transfer. The numbers above the brackets represent the difference in adjusted estimated per patient cost between the levels of hospitals, including 95% confidence intervals (CI).
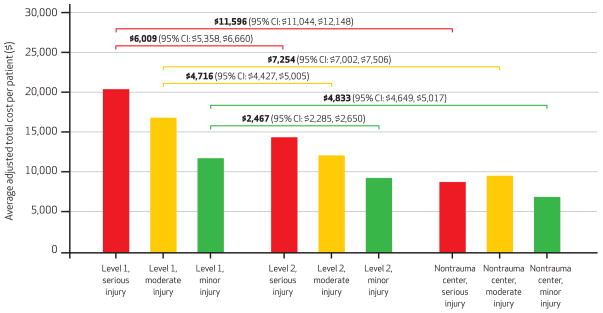
COST DIFFERENCES BY HOSPITAL TYPE AND INJURY SEVERITY
When patients were stratified by injury severity, the cost differences between different types of hospitals persisted (Exhibit 3). Level 1 trauma centers had the highest adjusted costs per patient across all injury strata. Among patients with minor injuries, for example, the adjusted cost of treatment at level 1 centers was $2,467 (95% confidence interval: $2,285, $2,650) higher than at level 2 centers and $4,833 (95% CI: $4,649, $5,017) higher than at nontrauma hospitals. Detailed results from the regression model are provided in Appendix Exhibit 6.25
Exhibit 3. Average Adjusted Total Cost Per Patient In The Study Sample, By Injury Severity.
SOURCE Authors’ analysis of the study data. NOTES N = 301; 214 patients. Covariates in the multivariable generalized linear model were combined Injury Severity Score (see Note 27 in text) and hospital type (nine categories); age; sex; mechanism of injury (fifteen categories); need for field ventilation (intubation or bag-valve mask ventilation); IV placement; Glasgow Coma Scale (see Exhibit 1 Notes); systolic blood pressure ≤90 mmHg; Injury Severity Score based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), codes; and need for major nonorthopedic surgery, orthopedic surgery, blood transfusion, or interhospital transfer. The numbers above the brackets represent the difference in adjusted estimated per patient cost between the levels of hospitals, including 95% confidence intervals (CI).
COSTS FOR PATIENTS NOT MEETING FIELD TRAUMA TRIAGE CRITERIA
Of the 248,342 patients identified as low risk by field triage guidelines, 243,169 (97.9 percent) were not seriously injured. However, 85,155 of the patients identified as low risk (34.3 percent) were overtriaged (64,382 being transported to level 1 trauma centers and 20,773 to level 2 centers).
We estimated the cost savings that could be achieved by using five different scenarios for redirecting such overtriaged patients to lower-level centers (Exhibit 4). To test the robustness of these estimates, we recalculated cost savings using only nonfield activations. Under the five scenarios, estimated cost savings ranged from 3.8 percent to 40.6 percent of total acute care costs. Redirecting all nonfield activations previously transported to level 1 and level 2 trauma centers to nontrauma centers instead was associated with the largest cost savings.
Exhibit 4.
Estimated Annual Cost Savings, By Scenarios Of Changes In Emergency Medical Services (EMS) Transport Patterns For Patients Not Meeting National Field Triage Guidelines
| Scenario | Annual savings in study regions
|
|||
|---|---|---|---|---|
| Using full study sample for estimates
|
Using only nonfield activations for estimates
|
|||
| Dollars | % of acute care costs | Dollars | % of acute care costs | |
| 1: All nonfield activations transported to nontrauma centers | 136,718,910 | 40.6 | 113,365,667 | 33.7 |
|
| ||||
| 2: Nonfield activations previously transported to level 1 trauma centers transported to level 2 centers | 60,075,703 | 17.8 | 60,118,625 | 17.8 |
|
| ||||
| 3: Nonfield activations previously transported to level 1 trauma centers transported to nontrauma centers | 118,234,110 | 35.1 | 100,593,442 | 29.9 |
|
| ||||
| 4: Nonfield activations previously transported to level 2 trauma centers transported to nontrauma centers | 18,484,800 | 5.5 | 12,772,225 | 3.8 |
|
| ||||
| 5: 50% of nonfield activations previously transported to level 1 or 2 trauma centers transported to nontrauma centers | 67,353,875 | 20.0 | 55,677,254 | 16.5 |
SOURCE Authors’ analysis of the study data.
NOTES “Nonfield activations” are injured patients who do not meet the criteria in the national field triage guidelines (see Note 17 in text). Cost savings were estimated from average adjusted cost differences by trauma center type (level 1, level 2, and nontrauma centers) after costs of interhospital transfer (including initial emergency department evaluation) for undertriaged patients (those with severe injuries originally transported to nontrauma centers) were accounted for.
SENSITIVITY ANALYSES
To test the validity and robustness of our models, we conducted several sensitivity analyses. To assess model fit, we compared actual costs to predicted costs, which yielded similar values ($9,651 versus $10,090, respectively). Across the majority of comparisons, estimated cost savings were lower when we used multiple imputation in comparison to a nonimputed sample (Appendix Exhibit 7).25
Cost data were more likely to be missing for patients not admitted to a hospital (a population with both less severe injuries and lower expected costs), compared to admitted patients. Thus, the sensitivity analyses suggested that results from the multiply imputed data set were preferred, and we retained them for our primary results.
Discussion
This study demonstrates that among injured patients transported by EMS, the cost of acute care differs substantially by the type of hospital to which a patient is transported. This finding remained consistent after we accounted for severity of injury and multiple important confounders. We also found that the downstream costs of transporting low-risk patients to major trauma centers—such as the costs of inpatient hospital services—are substantial, particularly for level 1 centers. These results suggest that EMS field triage decisions have large cost implications. If health systems matched patients’ needs more appropriately to hospitals’ capabilities, costs could be reduced. Our study also demonstrates variability in per patient and per capita injury costs across regions, which may further contribute to excess acute care costs.
Previous research has shown that adjusted costs are higher at major trauma centers than at nontrauma hospitals.13–15 However, past studies have primarily focused on patients with serious injuries. One exception is a recent study suggesting that implementing updated field triage guidelines could result in a national savings of $568 million annually by reducing over-triage.41 We found similar results among a broad, population-based sample of injured patients transported by EMS to acute care hospitals.
Focusing on patients served through the 911 EMS system is important because EMS plays an integral role both in concentrating seriously injured patients at major trauma centers (through field triage) and in selecting the location of hospital care. The benefit of major trauma centers appears limited to patients with serious injuries.5–12 Thus, the combination of higher costs and treating a large number of patients who are not seriously injured at major trauma centers results in an expensive mismatch of hospitals’ capabilities to patients’ needs without measurable benefit. Although it is possible that certain patients with minor to moderate injuries have improved outcomes in trauma centers, these benefits have not yet been demonstrated.
Our estimates for cost savings provide insights into aspects of trauma systems that could be modified to save costs. Because it would be impossible to avoid all overtriage—transporting to major trauma centers those patients identified as high risk by the criteria in the field triage guidelines but ultimately found not to have serious injuries—we focused our estimates on patients identified as low risk by the criteria but who are still transported to major trauma centers. For low-risk patients, the EMS process of selecting a destination hospital is driven largely by patient choice and hospital proximity.20,21
The traditional perception has been that triage-negative patients—those not identified as high risk by the criteria in the guidelines—are transported to nontrauma centers. Our findings refute this assumption and suggest that up to 40 percent of acute injury costs are incurred by patients without serious injuries who are cared for at resource-heavy hospitals. This phenomenon may represent an unintended consequence of regionalized care systems.
Although redirecting triage-negative patients to nontrauma hospitals could reduce costs, such practices might encounter resistance and have unintended consequences. Changes in ambulance transport patterns might reduce patients’ autonomy in hospital selection, disrupt the continuity of care for certain patients, increase the number of interhospital transfers, and reduce the availability of EMS vehicles for other 911 calls if transport times were increased.
Furthermore, redirecting patients to non-trauma hospitals might result in lost revenue for major trauma centers, adding to concerns about the financial viability of trauma systems.4 Shifting a larger volume of ambulance transports to nontrauma hospitals could also overwhelm those hospitals. Even in the case of patients without serious injuries, there were concerns during the development of trauma systems about providing initial trauma care in nontrauma hospitals. The majority of urban and suburban hospitals are now staffed with emergency physicians trained in the initial evaluation and management of trauma. Nonetheless, these concerns would need to be addressed, with care in nontrauma hospitals measured and tracked.
This study highlights the importance of accurate field triage processes so that patients’ needs can be matched with hospitals’ capabilities and excess costs in trauma systems can be minimized. Patients who are identified as high risk by the criteria in the field triage guidelines have more severe injuries that generally require care at major trauma centers. Some seriously injured patients are undertriaged—that is, they are missed by the guidelines and transported to nontrauma hospitals—which is one form of system inefficiency that may result in worse patient outcomes. Overtriage—transporting patients without serious injuries to major trauma centers—is another form of system inefficiency and a major contributor to excess costs.
Because under- and overtriage are inversely related,19 health policy makers must balance the competing priorities of addressing both factors. However, our results suggest that in systems using standard field triage guidelines, stricter adherence to transporting low-risk patients to nontrauma hospitals would reduce health care costs.
Conclusion
The cost of acute injury care for patients transported by EMS is highest in major trauma centers, even among patients with minor injuries. A substantive portion of acute care costs can be attributed to transporting low-risk patients to high-resource hospitals. Strict adherence to field triage guidelines, including the transport of low-risk patients to nontrauma centers, might reduce unnecessary health care costs and improve trauma systems in a cost-constrained environment.
Supplementary Material
Acknowledgments
The authors acknowledge and thank all of the participating emergency medical service agencies and medical directors, trauma registrars, and state offices that supported this project and helped provide data for it. A brief version of these results was presented at the annual meeting of the Society for Academic Emergency Medicine, Boston, Massachusetts, June 5, 2011. This project was supported by the Robert Wood Johnson Foundation Physician Faculty Scholars Program and the National Center for Research Resources at the National Institutes of Health (NIH) and the NIH Roadmap for Medical Research, through the Oregon Clinical and Translational Research Institute (Grant No. UL1 RR024140); University of California, Davis, Clinical and Translational Science Center (Grant No. UL1 RR024146); Stanford Center for Clinical and Translational Education and Research (Grant No. 1UL1 RR025744); University of Utah Center for Clinical and Translational Science (Grant Nos. UL1-RR025764 and C06-RR11234); and University of California, San Francisco, Clinical and Translational Science Institute (Grant Nos. UL1 RR024131 and KL2 RR024130).
Contributor Information
Craig D. Newgard, Email: newgardc@ohsu.edu, Associate professor of emergency medicine at Oregon Health and Science University, in Portland
Kristan Staudenmayer, Assistant professor of surgery at Stanford University, in Palo Alto, California.
Renee Y. Hsia, Assistant professor of emergency medicine at the University of California, San Francisco
N. Clay Mann, Professor of pediatrics at the University of Utah, in Salt Lake City.
Eileen M. Bulger, Professor of surgery at the University of Washington, in Seattle
James F. Holmes, Professor of emergency medicine at the University of California, Davis
Ross Fleischman, Assistant professor of emergency medicine at Harbor-UCLA Medical Center, in Torrance, California.
Kyle Gorman, Executive officer of Clackamas County Fire District No. 1, in Milwaukee, Oregon.
Jason Haukoos, Associate professor of emergency medicine at Denver Health Medical Center, in Colorado.
K. John McConnell, Associate professor of emergency medicine at Oregon Health and Science University.
NOTES
- 1.Thorpe KE, Florence CS, Joski P. Which medical conditions account for the rise in health care spending? Health Aff (Millwood) 2004;23(4):w4-437-45. doi: 10.1377/hlthaff.w4.437. [DOI] [PubMed] [Google Scholar]
- 2.Weir S, Salkever DS, Rivara FP, Jurkovich GJ, Nathens AB, Mackenzie EJ. One-year treatment costs of trauma care in the USA. Expert Rev Pharmacoecon Outcomes Res. 2010;10(2):187–97. doi: 10.1586/erp.10.8. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Medical expenditures attributable to injuries—United States, 2000. MMWR Morb Mortal Wkly Rep. 2004;53(1):1–4. [PubMed] [Google Scholar]
- 4.Mann NC, Mackenzie E, Teitelbaum SD, Wright D, Anderson C. Trauma system structure and viability in the current healthcare environment: a state-by-state assessment. J Trauma. 2005;58(1):136–47. doi: 10.1097/01.ta.0000151181.44658.0a. [DOI] [PubMed] [Google Scholar]
- 5.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366–78. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 6.Mullins RJ, Veum-Stone J, Helfand M, Zimmer-Gembeck M, Hedges JR, Southard PA, et al. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA. 1994;271(24):1919–24. doi: 10.1001/jama.1994.03510480043032. [DOI] [PubMed] [Google Scholar]
- 7.Sampalis JS, Denis R, Lavoie A, Fréchette P, Boukas S, Nikolis A, et al. Trauma care regionalization: a process-outcome evaluation. J Trauma. 1999;46(4):565–79. doi: 10.1097/00005373-199904000-00004. discussion 579–81. [DOI] [PubMed] [Google Scholar]
- 8.Pracht EE, Tepas JJ, 3rd, Celso BG, Langland-Orban B, Flint L. Survival advantage associated with treatment of injury at designated trauma centers: a bivariate probit model with instrumental variables. Med Care Res Rev. 2007;64(1):83–97. doi: 10.1177/1077558706296241. [DOI] [PubMed] [Google Scholar]
- 9.Nathens AB, Jurkovich GJ, Rivara FP, Maier RV. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma. 2000;48:25–30. doi: 10.1097/00005373-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Cooper A, Barlow B, DiScala C, String D, Ray K, Mottley L. Efficacy of pediatric trauma care: results of a population-based study. J Pediatr Surg. 1993;28(3):299–303. doi: 10.1016/0022-3468(93)90221-6. [DOI] [PubMed] [Google Scholar]
- 11.Hulka F, Mullins RJ, Mann NC, Hedges JR, Rowland D, Worrall WH, et al. Influence of a statewide trauma system on pediatric hospitalization and outcome. J Trauma. 1997;42(3):514–9. doi: 10.1097/00005373-199703000-00020. [DOI] [PubMed] [Google Scholar]
- 12.Pracht EE, Tepas JJ, 3rd, Langland-Orban B, Simpson L, Pieper P, Flint LM. Do pediatric patients with trauma in Florida have reduced mortality rates when treated in designated trauma centers? J Pediatr Surg. 2008;43(1):212–21. doi: 10.1016/j.jpedsurg.2007.09.047. [DOI] [PubMed] [Google Scholar]
- 13.MacKenzie EJ, Weir S, Rivara FP, Jurkovich GJ, Nathens AB, Wang W, et al. The value of trauma center care. J Trauma. 2010;69:1–9. doi: 10.1097/TA.0b013e3181e03a21. [DOI] [PubMed] [Google Scholar]
- 14.Goldfarb MG, Bazzoli GJ, Coffey RM. Trauma systems and the costs of trauma care. Health Serv Res. 1996;31(1):71–95. [PMC free article] [PubMed] [Google Scholar]
- 15.Durham R, Pracht E, Orban B, Lottenburg L, Tepas J, Flint L. Evaluation of a mature trauma system. Ann Surg. 2006;243(6):775–83. doi: 10.1097/01.sla.0000219644.52926.f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mackersie RC. History of trauma field triage development and the American College of Surgeons criteria. Prehosp Emerg Care. 2006;10(3):287–94. doi: 10.1080/10903120600721636. [DOI] [PubMed] [Google Scholar]
- 17.Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T, et al. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012;61(RR-1):1–20. [PubMed] [Google Scholar]
- 18.American College of Surgeons. Resources for the optimal care of the injured patient. Chicago (IL): ACS; 2006. [Google Scholar]
- 19.Newgard CD, Hsia RY, Mann NC, Schmidt T, Sahni R, Bulger EM, et al. The trade-offs in field trauma triage: a multiregion assessment of accuracy metrics and volume shifts associated with different triage strategies. J Trauma Acute Care Surg. 2013;74(5):1298–306. doi: 10.1097/TA.0b013e31828b7848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Newgard CD, Nelson MJ, Kampp M, Saha S, Zive D, Schmidt T, et al. Out-of-hospital decision making and factors influencing the regional distribution of injured patients in a trauma system. J Trauma. 2011;70(6):1345–53. doi: 10.1097/TA.0b013e3182191a1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Newgard CD, Mann NC, Hsia RY, Bulger EM, Ma OJ, Staudenmayer K, et al. Patient choice in the selection of hospitals by 911 emergency medical services providers in trauma systems. Acad Emerg Med. doi: 10.1111/acem.12213. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Newgard C, Malveau S, Staudenmayer K, Wang NE, Hsia RY, Mann NC, et al. Evaluating the use of existing data sources, probabilistic linkage, and multiple imputation to build population-based injury databases across phases of trauma care. Acad Emerg Med. 2012;19(4):469–80. doi: 10.1111/j.1553-2712.2012.01324.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Newgard CD, Zive D, Jui J, Weathers C, Daya M. Electronic versus manual data processing: evaluating the use of electronic health records in out-of-hospital clinical research. Acad Emerg Med. 2012;19(2):217–27. doi: 10.1111/j.1553-2712.2011.01275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Newgard CD. Validation of probabilistic linkage to match de-identified ambulance records to a state trauma registry. Acad Emerg Med. 2006;13:69–75. doi: 10.1197/j.aem.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 25.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 26.Clark DE, Osler TM, Hahn DR. ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. Boston (MA): Boston College Department of Economics; 2009. [Google Scholar]
- 27.Baker SP, O’Neill B, Haddon W, Jr, Long WB. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96. [PubMed] [Google Scholar]
- 28.MacKenzie EJ, Steinwachs DM, Shankar BS, Turney SZ. An ICD-9CM to AIS conversion table: development and application. Proc AAAM. 1986;30:135–51. [Google Scholar]
- 29.MacKenzie EJ, Steinwachs DM, Shankar B. Classifying trauma severity based on hospital discharge diagnoses. Validation of an ICD-9CM to AIS-85 conversion table. Med Care. 1989;27:412–22. doi: 10.1097/00005650-198904000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Fleischman RJ, Mann NC, Wang NE, Hsia RY, Rea TD, Liao M, et al. Society for Academic Emergency Medicine Annual Meeting Abstracts—2012: validating the use of ICD9 codes to generate injury severity score: the ICDPIC mapping procedure. Acad Emerg Med. 2012;19(Suppl 1):S4–393. [Google Scholar]
- 31.Bazzoli GJ, Kang R, Hasnain-Wynia R, Lindrooth RC. An update on safety-net hospitals: coping with the late 1990s and early 2000s. Health Aff (Millwood) 2005;24(4):1047–56. doi: 10.1377/hlthaff.24.4.1047. [DOI] [PubMed] [Google Scholar]
- 32.Corso P, Finkelstein E, Miller T, Fiebelkorn I, Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Inj Prev. 2006;12(4):212–8. doi: 10.1136/ip.2005.010983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bureau of Labor Statistics. Consumer Price Index [Internet] Washington (DC): Department of Labor; [cited 2013 Jul 19]. Available from: http://www.bls.gov/cpi/ [Google Scholar]
- 34.Rubin DB. Multiple imputation for nonresponse in surveys. New York (NY): John Wiley and Sons, Inc; 1987. [Google Scholar]
- 35.Raghunathan T, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001;27:85–95. [Google Scholar]
- 36.Manning WG. The logged dependent variable, heteroscedasticity, and the retransformation problem. J Health Econ. 1998;17:283–95. doi: 10.1016/s0167-6296(98)00025-3. [DOI] [PubMed] [Google Scholar]
- 37.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–94. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 38.Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24:465–88. doi: 10.1016/j.jhealeco.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 39.Taylor CB, Stevenson M, Jan S, Middleton PM, Fitzharris M, Myburgh JA. A systematic review of the costs and benefits of helicopter emergency medical services. Injury. 2010;41(1):10–20. doi: 10.1016/j.injury.2009.09.030. [DOI] [PubMed] [Google Scholar]
- 40.McConnell KJ, Johnson LA, Arab N, Richards CF, Newgard CD, Edlund T. The on-call crisis: a statewide assessment of the costs of providing on-call specialist coverage. Ann Emerg Med. 2007;49:727–33. doi: 10.1016/j.annemergmed.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 41.Faul M, Wald MM, Sullivent EE, Sasser SM, Kapil V, Lerner EB, et al. Large cost savings realized from the 2006 Field Triage Guideline: reduction in overtriage in U.S. trauma centers. Prehosp Emerg Care. 2012;16(2):222–9. doi: 10.3109/10903127.2011.615013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.