Abstract
Purpose
The prevalence of lower urinary tract symptoms (LUTS) increases with age and impairs quality of life. Radical prostatectomy (RP) has been shown to relieve LUTS at short-term follow-up. The long-term effect of RP on LUTS is unclear.
Materials and Methods
We performed a prospective cohort study of 1788 men undergoing RP. Progression of scores from the self-administered American Urological Association Symptom Index (AUASS) preoperatively and at three, six, 12, 24, 48, 60, 84, 96, and 120 months were analyzed using models controlling for preoperative AUASS, age, PSA, Gleason score, pathologic stage, nerve sparing, race, and marital status. This model was also applied to patients stratified by baseline clinically significant (AUASS>7) and insignificant (AUASS≤7) LUTS.
Results
Men exhibited an immediate worsening of LUTS that improved between three months and two years post-RP. Overall, the difference between mean AUASS at baseline and 10 years were not statistically or clinically significant. Men with baseline clinically significant LUTS experienced immediate improvements in LUTS that lasted until 10 years post-RP (13.5 vs. 8.81, p<0.001). Men with baseline clinically insignificant LUTS experienced a statistically significant but clinically insignificant increase in mean AUASS (3.09 to 4.94, p<0.001). The percentage of men with clinically significant LUTS declined from baseline to 10 years post-RP (p = 0.02).
Conclusions
RP is the only treatment for prostate cancer shown to improve and prevent the development of LUTS at long-term follow-up. This previously unrecognized long-term benefit argues in favor of the prostate as the primary contributor to male LUTS.
Keywords: prostate cancer, prostatectomy, quality of life, lower urinary tract symptoms, outcomes
Introduction
The prevalence of clinically significant LUTS, most commonly caused by BPH,1 progressively increases in men beginning in the fifth decade of life, exceeding 40% by their seventies.2-7 BPH and LUTS have been shown to greatly increase healthcare resource utilization, work productivity loss, activity impairment, pain, anxiety, and depression.5,8-10 Medical and surgical treatments for BPH cost $4 billion per year,11 and cause potentially serious side effects.12,13
Prostate cancer is the most common non-cutaneous malignancy in men and second leading cause of cancer mortality in American males.14 Approximately 40% of the 240,000 men diagnosed annually with prostate cancer in the United States undergo RP.15,16 RP may diminish quality of life by causing short- and long-term urinary incontinence and erectile dysfunction.17,18 In contrast, RP improves short- to intermediate-term quality of life by relieving LUTS.17,19-22 Whether this benefit to quality of life is durable over the long-term has yet to be studied.
Our prospective, longitudinal outcomes study of men undergoing RP with up to 10 years of follow-up provides the unique opportunity to elucidate the natural history of LUTS in the absence of a prostate gland in the aging male population. We hypothesize that the prostate is the primary factor contributing to the development of LUTS in men, and that RP will both arrest the development of and promote durable improvements in LUTS. If this hypothesis is proven, it will demonstrate a previously unrecognized long-term benefit of RP.
Methods
Between October 2000 and September 2012, 1836 men underwent open RP by a single surgeon (HL). Of these men, 1788 (97%) signed informed consent to participate in our IRB-approved prospective longitudinal outcomes study. The AUASI23 was self-administered prior to surgery and at 3, 6, 12, 24, 48, 60, 84, 96, and 120 months after surgery. The AUASI scores three storage (frequency, urgency, and nocturia) and four voiding (sensation of bladder emptying, intermittent urinary stream, caliber of urinary stream, and straining to urinate) symptoms on a scale of 0 to 5, yielding a composite score between 0 and 35. Total AUASS of 0 to 7, 8 to 19, and 20 to 35 define mild, moderate, and severe LUTS, respectively.1,24,25 Clinically significant LUTS are widely defined as AUASS>7.1,24,25
AUASIs were completed during routine follow-up visits or mailed directly to a data manager responsible for maintaining the database. The operating surgeon was not involved in administering the AUASI, entering data into a database, retrieving data, or conducting statistical analyses.
The primary dependent variable of interest was total AUASS at each follow-up period. Models controlled for preoperative AUASS, age (continuous, in years), preoperative PSA (continuous, in ng/mL), Gleason score (≤6, 3+4, 4+3, 7 [unspecified], ≥8, missing), pathologic stage (pT2a, pT2b, pT2c, pT3a, pT3b, pT3c, other or missing, based on American Joint Committee on Cancer staging classification), type of nerve sparing surgery (bilateral, unilateral, none, missing), race (Caucasian, African American, Hispanic, Asian, other, missing), and marital status (married, single, widowed, divorced or separated, other or missing).
We also included a random effect for each man to represent other distinguishing characteristics not controlled for by our independent covariates. This model was applied to all men and also stratified by baseline AUASS (clinically significant LUTS, AUASS >7 vs. clinically insignificant LUTS, AUASS≤7).
In men who responded to both baseline and either 3 month, 2 year, or 10 year post-RP surveys, McNemar's test and paired sample t-tests were used to assess whether the proportion of men with clinically significant LUTS or mean AUASS differed significantly between these assessments, respectively.
Analyses were conducted in SPSS 19.0.0.1 (SPSS, Inc, Chicago, IL) and STATA/SE 12.0 (College Station, TX). Differences were deemed to be significant at a two-sided p <0.05.
Results
Overall, 98% of the 1788 evaluable men completed the AUASI at baseline. This proportion progressively declined, reaching 43% at 10 years. There was no significant difference in age, race, marital status, nerve sparing status, pre-operative AUASS, or preoperative PSA between men who did and did not respond at 10 years (data not shown).
Thirty six percent of men exhibited moderate to severe LUTS at baseline (Table). The relationship between age and severity of LUTS is shown according to decade of life. The percentage of men with baseline clinically significant LUTS increased from 27% to 46% in men in their forties and seventies, respectively while mean AUASS increased from 5.42 to 7.95, respectively. Decade data for the five men and one man aged 30-39 and 80-89, respectively, is not displayed.
Table.
Pre- and peri-operative characteristics of a large longitudinal cohort undergoing RP for prostate cancer by a single surgeon.
| Characteristic | Number of Men (n=1788) | |
|---|---|---|
| Age (Mean ±SEM) | 58.9 ± 0.17 | |
| Race | African-American: 72 (4%) | |
| Asian: 36 (2%) | ||
| Caucasian: 1608 (90%) | ||
| Hispanic: 29 (2%) | ||
| Other: 28 (2%) | ||
| No Response: 15 (1%) | ||
| Marital Status | Divorced: 73 (4%) | |
| Married: 1537 (86%) | ||
| Separated: 16 (1%) | ||
| Single: 113 (6%) | ||
| Widowed: 27 (2%) | ||
| No Response: 22 (1%) | ||
| PSA (Mean ±SEM) | 6.26 ± 0.127 | |
| Pathologic Gleason Score | 0-6: 867 (48%) | |
| 7: 791 (44%) | ||
| 8-10: 114 (6%) | ||
| Missing: 16 (1%) | ||
| Pathologic Stage | 0-2: 1352 (76%) | |
| 3-4: 420 (23%) | ||
| Missing: 16 (1%) | ||
| Nerve Sparing Status | Bilateral: 1369 (77%) | |
| Unilateral: 270 (15%) | ||
| None (or Blank): 149 (8%) | ||
| Pre-operative AUASS (Mean ±SEM) | 6.87 ± 0.14 | |
| LUTS Severity (all men, 1749 valid) | Mild (0-7): 1114 (64%) | |
| Mod (8-19): 556 (32%) | ||
| Severe (20-35): 79 (5%) | ||
| Pre-RP LUTS | % with AUASS>7 | Mean AUASS |
| 40-49 (n=151) | 27% | 5.42 ± 0.51 |
| 50-59 (n=765) | 31% | 6.24 ± 0.21 |
| 60-69 (n=727) | 42% | 7.71 ± 0.22 |
| 70-79 (n=107) | 46% | 7.95 ± 0.61 |
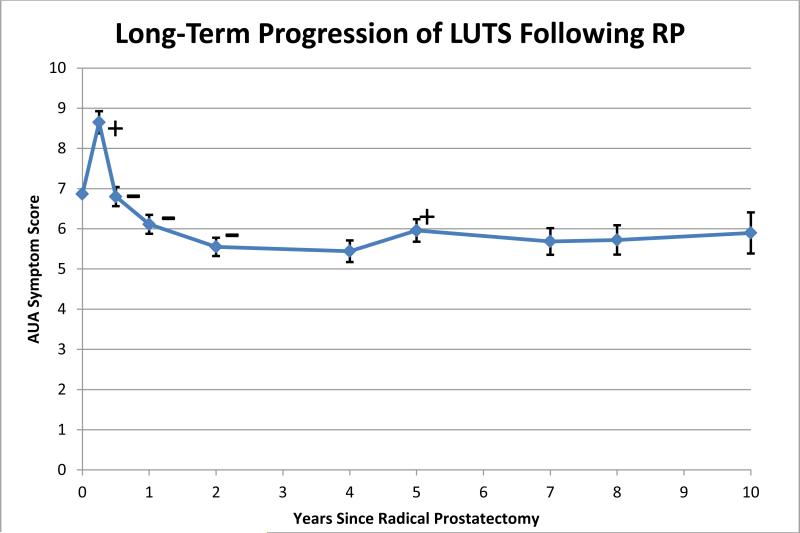
The adjusted time-dependent mean AUASS significantly increased by 1.74 points from baseline to the first post-operative assessment of LUTS at 3 months (6.88 vs. 8.62, p<0.001) (Figure 1). Thereafter, mean AUASS sequentially and significantly declined through two years. Mean AUASS did not change thereafter until 10 years, although there was a slight (0.52 point), yet statistically significant, increase between four and five years. Amongst the 242 men completing the AUASI at baseline and 10 years, the mean AUASS decrease of 0.48 was not statistically significant (p=0.24).
Figure 1.
Adjusted mean AUASS following RP. Error bars represent 95% confidence intervals. +/- indicates a significant increase/decrease in mean AUASS from previous follow-up interval.
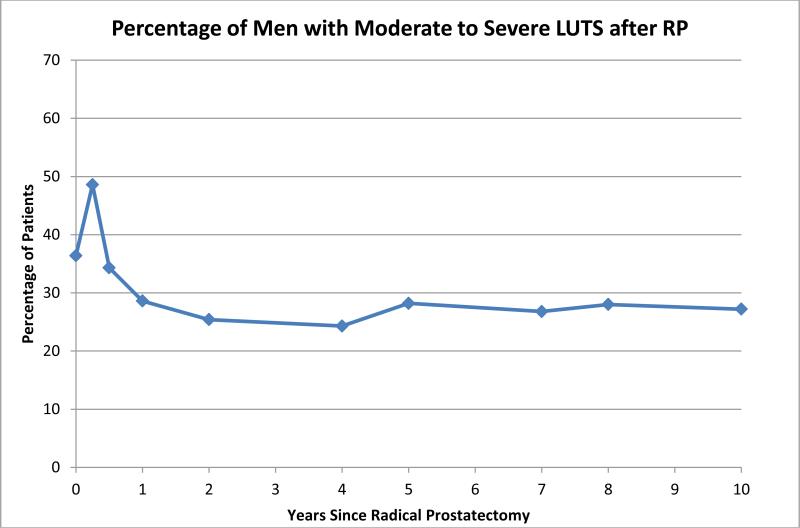
Over 10 years of follow-up, RP decreases the likelihood that men will have clinically significant LUTS (AUASS>7) at all evaluable time points with the exception of the three month assessment (Figure 2). Of the 242 men completing the AUASI at baseline and 10 years, 35.5% and 26.9% (p = 0.02) exhibited clinically significant LUTS, respectively.
Figure 2.
Percentage of men with clinically significant LUTS (AUASS >7) who responded to the AUASI at each follow-up interval.
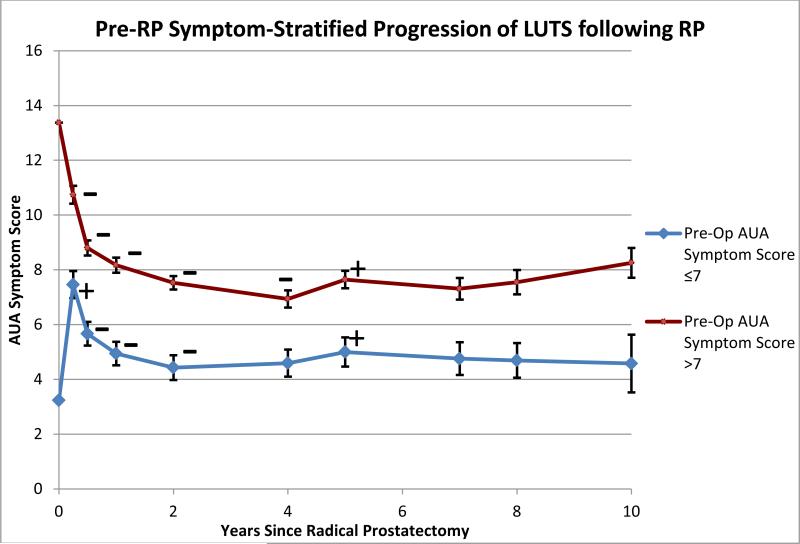
For men with baseline clinically significant LUTS (AUASS >7), there was an immediate and statistically significant 2.51 point decline in mean AUASS between the baseline and 3 month assessments (13.26 vs. 10.75, p<0.001) (Figure 3). Statistically significant and progressive declines in mean AUASS were observed between each sequential follow-up visit until the 4 year assessment. Mean AUASS increased by 0.50 points from four to five years (p=0.001), but was unchanged from five to 10 years. Overall, the long-term impact of RP on the 86 men with baseline clinically significant LUTS who completed the AUASI at baseline and 10 years was a significant 4.69 point decline in mean AUASS from 13.5 to 8.81 (p<0.001).
Figure 3.
Adjusted mean AUASS following RP, stratified by pre-operative LUTS score. Error bars represent 95% confidence intervals. +/- = significant increase/decrease in mean AUASS from previous time point.
For men with baseline clinically insignificant LUTS (AUASS ≤7), mean AUASS significantly increased by 4.17 points between the baseline and 3 month assessments (3.22 vs. 7.39, p<0.001) (Figure 3). Between 3 months and 2 years, mean AUASS progressively and significantly declined and reached a nadir at two years, remaining unchanged between 2 and 4 years. Between 4 and 5 years, mean AUASS significantly increased by 0.41 points (4.59 vs. 5.00, p<0.01). Between 5 and 10 years, there were no statistically significant interval changes in mean AUASS. Of the 156 men with baseline clinically insignificant LUTS who completed the AUASI at baseline and 10 years, mean AUASS increased by only 1.85 points from 3.09 to 4.94 (p<0.01).
Discussion
The AUASI is a widely utilized, self-administered instrument for quantifying LUTS severity and the response of LUTS to interventions for BPH.23,26 The American Urological Association and European Association of Urology discourage interventions for men presenting with AUASS ≤7.24,25 Based on these guidelines, we stratified our cohort of men undergoing RP into two subgroups: baseline clinically insignificant LUTS (AUASS ≤7) and baseline clinically significant LUTS (AUASS >7). In addition, we considered a clinically significant change in AUASS to be 3, a number widely utilized in the literature and clinical practice.1,26 Overall, the short-term benefit of RP on relieving LUTS seems only to be relevant amongst men with baseline clinically significant LUTS. The long-term follow-up of AUASS following RP provides the unique opportunity to define the role of the prostate in the natural history of male LUTS and to determine the durability of LUTS improvement.
Strengths of this study include its prospective long-term follow-up of a large cohort of well-characterized men undergoing RP by a single surgeon, utilization of a validated questionnaire at baseline and multiple follow-up intervals, and data management and statistical analysis performed without involvement of the operating surgeon. At our institution, rigorous efforts are made to maximize response to surveys. Therefore, most men undergoing RP by the operating surgeon (97%) signed informed consent, minimizing selection bias. Additionally, preoperative characteristics of responders and nonresponders at 10 years were similar, suggesting that attrition was attributable to random events.
The only other large prospective assessment of long-term quality of life outcomes following RP was derived from the Prostate Cancer Outcomes Study (PCOS), which reported a response rate of 63% at 15 years.18 While this number appears to be higher than our response rate of 43%, the PCOS excluded and stopped sending surveys to patients who did not respond to earlier surveys. Thirty eight percent of the eligible men did not complete either 6 or 12 month surveys and another unspecified amount did not complete surveys at two or five years. Of the remaining cases, another 28% were censored due to mortality. In calculating our response rate, we did not exclude nonresponders or mortalities. Therefore, we believe our follow-up is more robust than the PCOS. Lastly, we employed a regression model which adjusted for key pre-operative variables and accounted for repeated observations by factoring in the interdependence between survey responses.
During the first three months following RP, we postulate that two opposing factors influence LUTS: the favorable effect of removing the prostate in men with clinically significant LUTS and the negative effects of urinary incontinence. Since only 36% of men in our study had baseline clinically significant LUTS, only these men could experience LUTS improvements attributable to extirpation of the prostate. We have recently reported our prospective, longitudinal assessment of continence rates for the 1788 men in the present study; continence rates prior to RP and at 3, 6, 12, and 24 months after RP were 99%, 72%, 88%, 93%, and 96%, respectively.27 Between baseline and three months, mean AUASS increased by 1.74 points in the total cohort, suggesting that incontinence was a factor influencing LUTS over this interval. By six months, mean AUASS returned to baseline, presumably due to recovery of urinary continence. From six months to 10 years, observed interval changes in AUASS fell between +0.52 and -1.8, none of which reached clinical significance. Men completing both baseline and 10 year AUASI showed a small but statistically insignificant decline in mean AUASS and a significant decline in the proportion of men with clinically significant LUTS. RP appears to interrupt the natural progressive course of LUTS, since a greater increase in the general population of men would have been anticipated.
Stratifying our results based upon severity of LUTS at baseline clarified the nature of LUTS progression. In men with baseline clinically insignificant LUTS, a statistically and clinically significant increase of 4.17 in mean AUASS was observed between baseline and three months. Since all men in this sub-group lacked significant baseline LUTS, the impact of early incontinence following RP was unopposed by the potential benefit of removal of the prostate. Over time, however, as a greater proportion of men regained continence, mean AUASS decreased to its lowest level at two years, corresponding to the time when maximal continence rates are achieved.17,28,29 The overall change in mean AUASS between baseline and 2 years was a statistically significant but clinically insignificant 1.08 points, confirming that removal of the prostate contributes little, if any, to short-term LUTS in men with baseline clinically insignificant LUTS. Between two and 10 years, in the absence of the prostate, the mean AUASS increase was only 0.16. This negligible absolute change over eight years suggests that in the absence of a prostate, men without clinically significant LUTS will rarely develop them.
In men with baseline clinically significant LUTS, removal of the prostate has the potential to ameliorate LUTS by treating co-existing BPH. Between baseline and 3 months, the decrease in mean AUASS of 2.51 was statistically and nearly clinically significant. Mean AUASS continued to decline between three months and two years, presumably as continence was restored and the benefit of removing the prostate was fully realized. Overall, the decrease in mean AUASS from baseline to two years was 5.84 points, corresponding to moderate symptom improvement.26 From 2 to 10 years, sequential interval changes in mean AUASS ranged between +0.71 and -0.59, levels that do not approach clinical significance. Of those men with baseline clinically significant LUTS who completed baseline and 10 year assessments, the overall mean decline was 4.69 points. Our study provides compelling evidence that men with baseline clinically significant LUTS experience a clinically significant and durable decline in LUTS after RP.
Sarma et al have reported that the observed mean increase in AUASS for community-dwelling men in their forties, fifties, sixties, and seventies is 0.13, 0.30, 0.60, and 0.38 points per year, respectively.4 Extrapolating these findings to our 242 men who completed both baseline and 10 year assessments, the expected increase in mean AUASS is calculated to be an increase of 4.66 points. The actual change in mean AUASS over the 10 year interval in our cohort was a small decrease of 0.48 points, confirming the very favorable impact of RP on LUTS. Collectively, these observations provide compelling evidence that removal of the prostate interrupts the natural history of male LUTS, implying that the prostate is the major contributor to male LUTS.
Our hypothesis about the role of the prostate assumes that the LUTS prevalence in our cohort is due to the benign, and not the malignant, elements of the prostate. We have previously reported that over 45% of RP surgical specimen contain <10% cancer by volume.30 We assume that this low volume of cancer does not significantly contribute to LUTS. Additionally, available data shows that the percentage of men with clinically significant LUTS (AUASS>7) in the general population in their 40s, 50s, 60s, and 70s is 11-26%, 19-33%, 31-41%, and 40-49%, respectively.2,3,6,7 These findings are consistent with the decade-stratified LUTS in our cohort, suggesting that our results are generalizable to men without prostate cancer.
There are some limitations to our study. We did not assess whether men were on medical therapy for BPH prior to undergoing RP. However, all men were instructed to discontinue medical BPH therapies one week following RP. If therapy were terminated before RP, however, the baseline mean AUASS would have been higher and the RP-mediated improvement in LUTS would have been enhanced. Another benefit of RP in men with baseline clinically significant LUTS is the ability to discontinue a chronic medication. Our study also lacks a randomized control. However, LUTS progression has been well characterized in community-dwelling men. Finally, our results represent the experience of a single surgeon who has performed a high volume of RPs. Therefore, our results may not be generalizable to community urologists who perform a smaller number of cases per year.
Conclusions
Men contemplating the various treatment options for clinically localized prostate cancer should be counseled regarding the significant long-term benefit RP has on improving and preventing LUTS. This treatment-related benefit has not been reported for any other treatment option for prostate cancer. One should not underestimate the clinical relevance of relieving and preventing the development of LUTS, given that millions of men choose a lifetime commitment to medical therapy or surgical treatment of LUTS in order to improve their quality of life.
Acknowledgements
This study was supported in part by grant 5UL1RR029893 from the National Center for Research Resources, National Institutes of Health, and the United States Department of Veterans Affairs.
Key of Definitions for Abbreviations
- AUASI
American Urological Association Symptom Index
- AUASS
American Urological Association Symptom Score
- BPH
benign prostatic hyperplasia
- LUTS
lower urinary tract symptoms
- RP
radical prostatectomy
- PSA
prostate specific antigen
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sarma AV, Wei JT. Clinical practice. Benign prostatic hyperplasia and lower urinary tract symptoms. N Engl J Med. 2012;367:248–57. doi: 10.1056/NEJMcp1106637. [DOI] [PubMed] [Google Scholar]
- 2.Berges R, Oelke M. Age-stratified normal values for prostate volume, PSA, maximum urinary flow rate, IPSS, and other LUTS/BPH indicators in the German male community-dwelling population aged 50 years or older. World J Urol. 2011;29:171–8. doi: 10.1007/s00345-010-0638-z. [DOI] [PubMed] [Google Scholar]
- 3.Chute CG, Panser LA, Girman CJ, et al. The prevalence of prostatism: a population-based survey of urinary symptoms. J Urol. 1993;150:85–9. doi: 10.1016/s0022-5347(17)35405-8. [DOI] [PubMed] [Google Scholar]
- 4.Sarma AV, Jacobsen SJ, Girman CJ, et al. Concomitant longitudinal changes in frequency of and bother from lower urinary tract symptoms in community dwelling men. J Urol. 2002;168:1446–52. doi: 10.1016/S0022-5347(05)64471-0. [DOI] [PubMed] [Google Scholar]
- 5.Wu MP, Hsu YW, Weng SF, Ho CH, Wang JJ, Tong YC. Healthcare-seeking Prevalence of Lower Urinary Tract Symptoms Among National Health Insurance Enrollees in Taiwan, 2000-2009. Urology. 2012 doi: 10.1016/j.urology.2012.08.033. [DOI] [PubMed] [Google Scholar]
- 6.Terai A, Matsui Y, Ichioka K, Ohara H, Terada N, Yoshimura K. Comparative analysis of lower urinary tract symptoms and bother in both sexes. Urology. 2004;63:487–91. doi: 10.1016/j.urology.2003.09.070. [DOI] [PubMed] [Google Scholar]
- 7.Boyle P, Robertson C, Mazzetta C, et al. The prevalence of lower urinary tract symptoms in men and women in four centres. The UrEpik study. BJU Int. 2003;92:409–14. doi: 10.1046/j.1464-410x.2003.04369.x. [DOI] [PubMed] [Google Scholar]
- 8.Girman CJ, Jacobsen SJ, Tsukamoto T, et al. Health-related quality of life associated with lower urinary tract symptoms in four countries. Urology. 1998;51:428–36. doi: 10.1016/s0090-4295(97)00717-6. [DOI] [PubMed] [Google Scholar]
- 9.Coyne KS, Wein AJ, Tubaro A, et al. BJU Int. Vol. 103. Suppl 3: 2009. The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. pp. 4–11. [DOI] [PubMed] [Google Scholar]
- 10.Kannan H, Radican L, Turpin RS, Bolge SC. Burden of illness associated with lower urinary tract symptoms including overactive bladder/urinary incontinence. Urology. 2009;74:34–8. doi: 10.1016/j.urology.2008.12.077. [DOI] [PubMed] [Google Scholar]
- 11.Taub DA, Wei JT. The economics of benign prostatic hyperplasia and lower urinary tract symptoms in the United States. Curr Urol Rep. 2006;7:272–81. doi: 10.1007/s11934-996-0006-0. [DOI] [PubMed] [Google Scholar]
- 12.Carbone DJ, Jr., Hodges S. Medical therapy for benign prostatic hyperplasia: sexual dysfunction and impact on quality of life. Int J Impot Res. 2003;15:299–306. doi: 10.1038/sj.ijir.3901017. [DOI] [PubMed] [Google Scholar]
- 13.O'Leary MP. Treatment and pharmacologic management of BPH in the context of common comorbidities. Am J Manag Care. 2006;12:S129–40. [PubMed] [Google Scholar]
- 14.Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212–36. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- 15.Underwood W, 3rd, Jackson J, Wei JT, et al. Racial treatment trends in localized/regional prostate carcinoma: 1992-1999. Cancer. 2005;103:538–45. doi: 10.1002/cncr.20796. [DOI] [PubMed] [Google Scholar]
- 16.Cooperberg MR, Broering JM, Carroll PR. Time trends and local variation in primary treatment of localized prostate cancer. J Clin Oncol. 2010;28:1117–23. doi: 10.1200/JCO.2009.26.0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanda MG, Dunn RL, Michalski J, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008;358:1250–61. doi: 10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]
- 18.Resnick MJ, Koyama T, Fan KH, et al. Long-term functional outcomes after treatment for localized prostate cancer. N Engl J Med. 2013;368:436–45. doi: 10.1056/NEJMoa1209978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Namiki S, Ishidoya S, Saito S, et al. Natural history of voiding function after radical retropubic prostatectomy. Urology. 2006;68:142–7. doi: 10.1016/j.urology.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 20.Schwartz EJ, Lepor H. Radical retropubic prostatectomy reduces symptom scores and improves quality of life in men with moderate and severe lower urinary tract symptoms. J Urol. 1999;161:1185–8. [PubMed] [Google Scholar]
- 21.Lepor H, Kaci L. The impact of open radical retropubic prostatectomy on continence and lower urinary tract symptoms: a prospective assessment using validated self-administered outcome instruments. J Urol. 2004;171:1216–9. doi: 10.1097/01.ju.0000113964.68020.a7. [DOI] [PubMed] [Google Scholar]
- 22.Parker WR, Wang R, He C, Wood DP., Jr. Five year expanded prostate cancer index composite-based quality of life outcomes after prostatectomy for localized prostate cancer. BJU Int. 2011;107:585–90. doi: 10.1111/j.1464-410X.2010.09579.x. [DOI] [PubMed] [Google Scholar]
- 23.Barry MJ, Fowler FJ, Jr., O'Leary MP, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol. 1992;148:1549–57. doi: 10.1016/s0022-5347(17)36966-5. discussion 64. [DOI] [PubMed] [Google Scholar]
- 24.McVary KT, Roehrborn CG, Avins AL, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011;185:1793–803. doi: 10.1016/j.juro.2011.01.074. [DOI] [PubMed] [Google Scholar]
- 25.Madersbacher S, Alivizatos G, Nordling J, Sanz CR, Emberton M, de la Rosette JJ. EAU 2004 guidelines on assessment, therapy and follow-up of men with lower urinary tract symptoms suggestive of benign prostatic obstruction (BPH guidelines). Eur Urol. 2004;46:547–54. doi: 10.1016/j.eururo.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 26.Barry MJ, Williford WO, Chang Y, et al. Benign prostatic hyperplasia specific health status measures in clinical research: how much change in the American Urological Association symptom index and the benign prostatic hyperplasia impact index is perceptible to patients? J Urol. 1995;154:1770–4. doi: 10.1016/s0022-5347(01)66780-6. [DOI] [PubMed] [Google Scholar]
- 27.Prabhu V, Sivarajan G, Taksler GB, Laze J, Lepor H. Long-term Continence Outcomes in Men Undergoing Radical Prostatectomy for Clinically Localized Prostate Cancer. Eur Urol. 2013 doi: 10.1016/j.eururo.2013.08.006. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lepor H, Kaci L, Xue X. Continence following radical retropubic prostatectomy using self-reporting instruments. J Urol. 2004;171:1212–5. doi: 10.1097/01.ju.0000110631.81774.9c. [DOI] [PubMed] [Google Scholar]
- 29.Walsh PC, Marschke P, Ricker D, Burnett AL. Patient-reported urinary continence and sexual function after anatomic radical prostatectomy. Urology. 2000;55:58–61. doi: 10.1016/s0090-4295(99)00397-0. [DOI] [PubMed] [Google Scholar]
- 30.Shah O, Robbins DA, Melamed J, Lepor H. The New York University nerve sparing algorithm decreases the rate of positive surgical margins following radical retropubic prostatectomy. J Urol. 2003;169:2147–52. doi: 10.1097/01.ju.0000057496.49676.5a. [DOI] [PubMed] [Google Scholar]